Abstract
Rotatory atlantoaxial instability can manifest as an acute episode following subtle or minor injury or even following a gentle tap on head in young children and can manifest as a painless deformity of the head. Goel technique of direct surgical opening of the atlantoaxial facet joint, manual manipulation of the facets can lead to reduction of rotatory atlantoaxial dislocation and recovery from torticollis. Torticollis can be a protective natural phenomenon in response to atlantoaxial instability and related basilar invagination. Only atlantoaxial fixation can lead to immediate postoperative reduction of torticollis. Spasmodic torticollis related to muscle hyperactivity is unrelated to atlantoaxial instability.
Keywords: Atlantoaxial instability, basilar invagination, facetal locking, rotatory dislocation
INTRODUCTION
Atlantoaxial joint is the most mobile joint of the body. To facilitate circumferential movements, the joint is designed flat and round and has no restrictive edges like that seen in hinge or ball and socket joints. The joint caters to extensive movements that are orchestrated by the design of circumferential arch of atlas, peg-like odontoid process, strong and stubby spinous process of axis, and the masterly crafted facets of atlas and axis. The string of muscles attached to the spinous process and transverse processes of axis, thin but strong muscles attached to the large transverse process of the atlas, fan-like muscles attached to arch of atlas and suboccipital bone, and a host of ligaments traversing in multiple directions provide the possibility of lifetime free movements of the head and neck. Considering the size, in relative terms, the spinous process of axis and transverse process of atlas are largest and strongest of all spinal vertebrae. We had speculated earlier that all movements at the atlantoaxial joint occur in the facet joints and are powered by the muscles of the nape of the neck. The odontoid process has a role in directing and controlling the movements. The odontoid process in the craniovertebral junction and the discs in the subaxial spine are the brain of the movements, brawn of movements being the muscles of the nape of the neck that focus their activity on the facets that form the fulcrum of movements.[1]
BIOMECHANICS
The occipitoatlantoaxial joints are the most complex joints of the axial skeleton. This joint complex forms a part of the primary pillar of spine that provides stability and mobility to the head. While occipitoatlantal joint is the center of stability, atlantoaxial joint is the center for mobility. While atlantoaxial joint is the center for mobility, it is also the center for instability.
The review of literature on the subject suggests that the geometry of the atlantoaxial articular surfaces is such that they are convex with horizontal orientation, thus suitable to permit rotation. The maximum rotation between the atlas and axis is approximately 45°.[2] When rotation exceeds 45°, the inferior facet of atlas interlocks over the superior facet of axis. If the transverse ligament is unusually lax or weak, this facet interlock may occur even with rotation of <45°. It has been identified that if the transverse ligament remains intact, anterior arch of atlas will not subluxate over axis unless there is over 65° of rotation.
RANGE OF MOTION AT THE OCCIPITOATLANTOAXIAL JOINTS (REPRESENTATIVE VALUES)[2]
-
Occipitoatlantal joint
- Combined flexion and extension 25°
- One-side lateral bending 5°
- One-side axial rotation 5°.
-
Atlantoaxial joint
- Combined flexion and extension 20°
- One-side lateral bending 5°
- One-side axial rotation 40°–45°.
The alar ligaments limit axial rotation and side bending of the C0–C1–C2 complex. The left alar ligament limits rotation of C1 and the head to the right and the right alar ligament limits rotation to the left. The vertebral arteries located in the foramen transversarium are not affected by the extremes of normal rotation but they can be severely compromised by excessive rotation, especially if combined with anterior displacement.[3,4] The fact that the vertebral artery has a dynamic relationship with the bones during rotational movements was first discussed by us.[4] The laxity of the vertebral artery in the region assists in facilitating a range of neck movements.
ATLANTOAXIAL INSTABILITY
This extensively mobile region in the presence of round plate like articular surfaces of atlas and axis makes atlantoaxial joint most prone to instability. Our recent analysis suggests that atlantoaxial joint instability is the most common joint instability of the entire body. It seems that atlantoaxial instability is underrecognized and undertreated clinical entity. While in the elderly, the instability is related to weakness of the muscles that conduct the movements; in younger children, the design of flat bone surface and significantly more smooth articular cartilage make it liable to slip and dislocate. Rotatory dislocations are more common in children.
Atlantoaxial dislocations are divided into anterior, posterior, lateral, vertical, and rotational types.[5,6,7] Recently, we discussed an alternative classification of atlantoaxial instability that was based on facetal alignments.[8] We identified “central” or “axial” atlantoaxial dislocation, wherein there was instability of the atlantoaxial joint despite the fact that there was no abnormality of atlantodental interval and no dural or neural compression at the craniovertebral junction. The atlantoaxial instability was identified on the basis of facetal instability as observed by direct manual manipulation of the facets and on radiological observation of posterior dislocation of the facet of atlas in relationship with the facet of axis in lateral profile imaging in neutral head position. Destructive, infective, traumatic, or degenerative involvement of the craniovertebral region can rarely result in lateral dislocation of the facet of atlas over axis. In this review, we will discuss the rotatory types of atlantoaxial dislocations.
TORTICOLLIS
Torticollis is a manifestation of abnormal physical neck rotation. Three types of torticollis have been identified. Understanding each one of them is crucial as the pathology is discrete and the treatment protocol will depend on the factors that initiate the progress of torticollis.
Type 1 - Protective or secondary torticollis
This type of torticollis has similarities to scoliosis that results after an acute disc herniation. Chronic or long-standing atlantoaxial dislocation results in a number of musculoskeletal and neural-protective natural maneuvering by the body, torticollis being one of them. Eccentric indentation of the odontoid process into the cervicomedullary cord results in torticollis [Figures 1 and 2]. Such an indentation is seen in cases with both Group A and Group B basilar invagination. The torticollis seen in cases with basilar invagination is present in varying degrees and depends on the extent and direction of odontoid process indentation. The long-standing torticollis seen in such cases appear to be a part of protective physical alteration that occurs as an attempt to accommodate the spinal cord in a relentlessly and progressively reducing spinal canal. Our observations suggest that such a torticollis (and even short neck) is reversible following stabilization of the craniovertebral junction.[9]
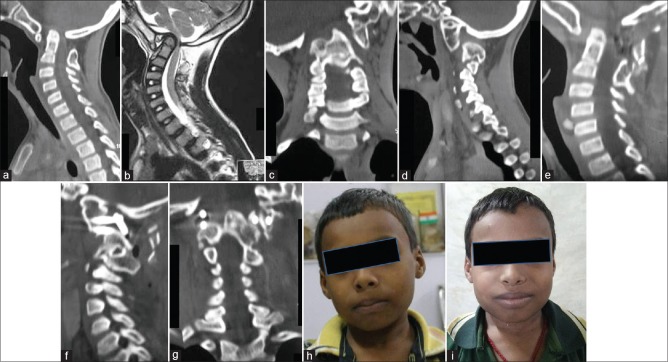
Figure 1.
Images of a 9-year-old boy. (a) Sagittal computed tomography scan shows basilar invagination, assimilation of atlas, and C2–C3 fusion. (b) T2-weighted magnetic resonance imaging shows neural compression. External syringomyelia and external syringobulbia can be seen. (c) Coronal computed tomography scan shows marked craniovertebral junction deformity. (d) Sagittal scan shows Goel Type 1 atlantoaxial instability. (e) Postoperative computed tomography scan shows reduction of basilar invagination and craniovertebral fixation. (f) Computed tomography showing the implant. (g) Coronal computed tomography scan showing the implant. (h) Preoperative clinical image. (i) Postoperative clinical image showing reduction of torticollis
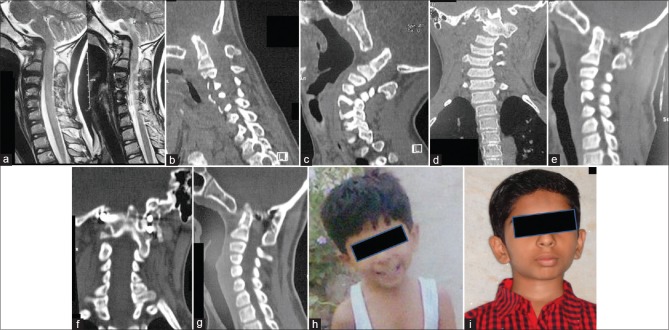
Figure 2.
Images of a 6-year-old boy. (a) T2-weighted magnetic resonance imaging shows basilar invagination, assimilation of atlas, and C2–C3 fusion. (b) Sagittal computed tomography scan in flexion shows basilar invagination, assimilation of atlas, and C2–C3 fusion. (c) Sagittal computed tomography in extension shows no significant reduction in basilar invagination. (d) Preoperative coronal computed tomography showing the deformity and torticollis. (e) Postoperative computed tomography showing reduction of basilar invagination and craniovertebral realignment. (f) Postoperative coronal computed tomography shows intra-articular implant on the right side and plate and screw fixation on the left side. (g) Delayed postoperative computed tomography scan shows craniovertebral fusion. (h) Preoperative clinical image. (i) Postoperative image showing reduction of torticollis
Treatment
Direct manipulation of the atlantoaxial joint, distraction of facets with bone graft, with or without introduction of titanium metal spacers, and fixation arthrodesis of the atlantoaxial joint has been shown by us to result in reduction of basilar invagination and of atlantoaxial dislocation [Figures 1 and 2]. Torticollis can recover in the immediate postoperative period [Figures 1 and 2]. Torticollis can recover after atlantoaxial fixation without any special or direct attempt toward reduction of torticollis. Differential distraction of the facets can also be done in selected cases, and this can result in reduction of torticollis.
Type 2 - Spasmodic torticollis
The torticollis in this group is related to sternocleidomastoid muscle spasm. The pathology in these cases and the treatment remain controversial. Botulinum injections in the spasmodic muscles have been identified to be a satisfactory temporary treatment modality in resistant cases.
Type 3 - Facetal rotatory torticollis
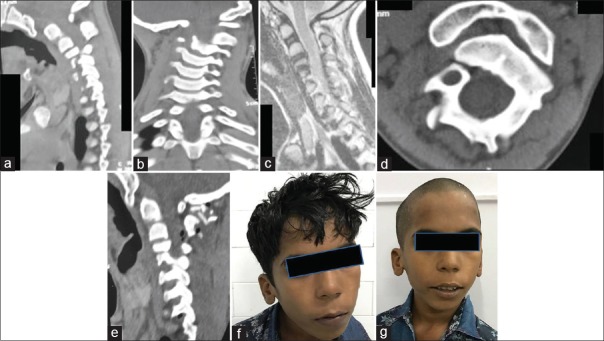
Torticollis in this group is related to “rotatory” atlantoaxial dislocation secondary to rotatory dislocation of the facet of the atlas over the facet of the axis[7] [Figures 3 and 4]. This group forms a discrete entity.
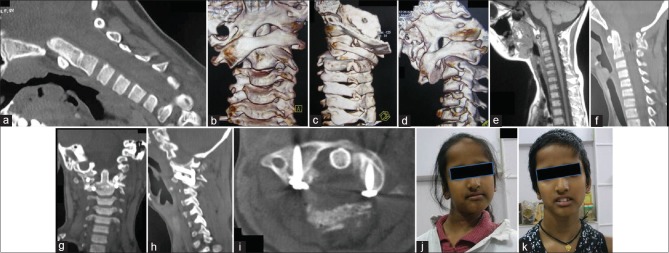
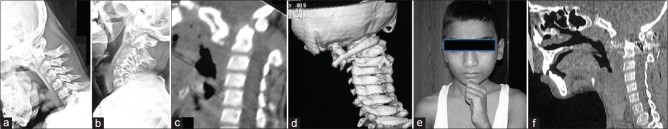
Figure 3.
Images of a 9-year-old female. (a) Computed tomography scan shows marked basilar invagination. (b) Three-dimensional computed tomography scan shows complete rotatory atlantoaxial dislocation. (c) Posterior view showing the rotatory dislocation. (d) Oblique view of three-dimensional computed tomography scan shows the rotatory abnormality. (e) T1-weighted magnetic resonance imaging shows basilar invagination. (f) Postoperative computed tomography shows reduction of basilar invagination. (g) Coronal computed tomography scan shows reduction of the facetal malalignment. (h) Computed tomography showing the implant and the facets in alignment. (i) Axial computed tomography scan shows screws in the facets of atlas. (j) Preoperative clinical image of the patient. (k) Postoperative image showing reduction of the torticollis
Figure 4.
Images of a 9-year-old male child. (a) Computed tomography scan shows rotatory atlantoaxial dislocation. (b) Coronal computed tomography scan showing the rotation. (c) T2-weighted magnetic resonance imaging shows no significant cord compression. (d) Axial computed tomography shows rotation. (e) Postoperative computed tomography scan showing craniovertebral fixation. (f) Preoperative picture of the patient showing torticollis. (g) Postoperative image showing reduction of torticollis
HISTORICAL BACKGROUND AND NOMENCLATURE
Rotatory dislocation of the atlantoaxial joint was first described by Bell in 1830[10] and Corner in 1907.[11] Wortzman and Dewar introduced the term atlantoaxial rotatory fixation in 1968.[12]
Rotatory atlantoaxial dislocation occurs usually in otherwise healthy children. Minor or insignificant trauma initiates the process. The torticollis is painless, and often, there are no neurological symptoms. Rotatory atlantoaxial dislocation can be subdivided into reducible or irreducible types. Reducible type rotatory atlantoaxial dislocation is classified as one where the dislocation reduces on dynamic images or after institution of cervical traction. Reducible rotatory atlantoaxial dislocation is usually of incomplete type, when some part of the facet of the atlas is in contact with the facet of the axis. Complete rotatory dislocation can also reduce on traction, but the possibilities of its reduction are relatively less. Mobile and reducible rotatory dislocation can be treated by conservative observation for about 3 months using halo traction or cervical collar. If during the period, the rotatory dislocation reduces and remains reduced on dynamic imaging, there is no need for surgery. Or else, surgical fixation of the rotatory dislocation in reduced position should be carried out. In cases with “irreducible” rotatory dislocation, an attempt can be made to reduce the dislocation by surgical distraction and reduction by manual realignment of facets.
ETIOPATHOGENESIS
Rotatory atlantoaxial dislocation or locking of atlantoaxial facets
Locking of the atlantoaxial facet joints has been identified to result in rotatory atlantoaxial dislocation. Such a dislocation has been identified more commonly in young children. Although several pathogenetic factors have been considered, the exact cause of the phenomenon is unclear. The dislocation is an acute event that is usually triggered by an episode of relatively minor trauma. Some patients have been identified as having throat and paranasal sinus infections or tonsillitis at the time of event. However, an exact correlation among possible infection, trauma, and atlantoaxial dislocation is only speculative. None of the patients in our series had any evidence of significant focus of infection. Several other seemingly insignificant events have been associated with initiation of the dislocation. Rheumatoid arthritis, Down syndrome, Morquio disease, and various congenital cervical anomalies have also been associated with rotatory dislocation. The higher incidence of rotatory atlantoaxial dislocation in children may be attributed to the shallower and more horizontally oriented joint surface, the relative elasticity of the ligaments, the not yet fully developed neck muscles, and a relatively large head.[3] The acuity of the neck deformity in an otherwise healthy and neurologically normal child are the hallmarks of the problem. Pain is not a prominent presenting symptom. Patients present with the head tilted toward one side and rotated toward the other and in slight flexion. In the case of right unilateral anterior rotatory subluxation, one observes lateral bending of the head and neck to the right and rotation of the head to the left. Rotation of the head contralateral to the direction it faces is difficult; however, rotating it further in the direction toward which it faces is possible.[11] In the acute setting, it is important to distinguish between rotatory locking and muscular torticollis. In rotatory dislocation, the sternomastoid spasm is on the side of the chin, whereas in muscular torticollis, the spasm is on the contralateral side.
The cause of fixation
The cause of the facet dislocation and its fixation in an abnormal position remains unknown because no anatomical or autopsy evidence bearing on this question is available. Trauma or infection of the ligaments leading to laxity or a tear has been implicated as the most possible pathogenetic factor. Obstruction of movements related to impingement of fragments of articular capsule or ligaments on the joint cavity has been speculated. However, with our surgical technique, which involved opening up of the joint and allowing for direct inspection, we found no actual tear or a broken fragment of ligament or bone within the joint cavity. We did identify alteration in texture and an unusually gray hue of the ligaments possibly related to inflammation in at least 25% cases. In the case involving translatory dislocation, extreme laxity or a tear of transverse ligament was possible. However, our investigations did not show this ligament clearly, and operative procedure did not provide an opportunity for direct inspection of this ligament.
Pathogenesis
A number of possible etiological factors have been posited in the literature. Wittek[13] suggested that there is an effusion in the synovial joints that produces stretching of the ligaments. Coutts[14] proposed the theory that synovial fringes, when inflamed or adherent, may block reduction, whereas Fiorrani-Gallotta et al.[15] indicated that the deformity is due to rupture of one or both alar ligaments and the transverse ligament. Jones[16] postulated the presence of a hyperemic decalcification with loosening of the ligaments. Grisel[17] suggested that muscle contracture might follow an upper respiratory tract infection and be a factor. Hess et al.[18] concluded that there is a combination of factors, including muscle spasm that prevents reduction in the early stages. Wortzman and Dewar[12] postulated that there is damage to the atlantoaxial articular processes of an unknown nature. Fielding and Hawkins[3] suggested that reduction of the dislocation is probably obstructed in the early stages by swollen capsular and synovial tissues and by associated muscle spasm. If the abnormal position persists due to a failure to achieve reduction, ligament and capsular contractures develop and cause fixation.
RADIOGRAPHIC FEATURES AND INVESTIGATIONS
Three-dimensional (3-D) computed tomography (CT) scans are useful for diagnosing facet locking, as the atlas, axis, and their positions can be accurately seen. Although it is possible to determine the degree of neck angulation based on CT scans, the exact parameters necessary have not been clearly described in the literature. Moreover, a uniform CT scan pattern is necessary for validity of such an evaluation. Dynamic scans have been advocated for analyzing the abnormality in relative motion between the atlas and axis, but this investigation was not performed. The basic diagnostic criterion for this condition is a persistent asymmetrical relationship between the dens and the articular masses of the atlas not correctable by rotation.
3-D model construction or 3-D CT scanning is the latest advance in the investigative modality and can be most effective to diagnose and confirm rotational atlantoaxial dislocation.[19] The exact alignment of the facets and their displacement can be evaluated. Dynamic CT scan, with the head and neck in flexed and extended positions, clearly delineates the pathology and assists in determining the appropriate surgical treatment modality.
Magnetic resonance imaging (MRI) assists in confirming the findings of CT scan and demonstrates features that would suggest compression and displacement of the neural and vascular structures.
The plain X-ray investigations have now become less relevant with the increasing and popular use of CT scanning and MRI.
The degree of neck rotation or tilt in patients having rotatory dislocation was measured as an angle between a line that coursed from the nasion, tip of the nose, and symphysis menti to the horizontal. The angle was then expressed as the degree of tilt from the vertical.
ROTATORY DISLOCATION AND VERTEBRAL ARTERY
Both rotatory and translatory dislocations result in an alteration in the course of the vertebral artery.[4] Theoretically, acuity of the event can lead to abnormal stretching or even vertebral artery occlusion. However, the suppleness of tissues in children probably allows space for accommodation. Apart from the alteration in the vertebral artery course due to deformity, we did not identify any structural variation in the arterial foramen or any abnormality in the artery's dimensions. The technique of distraction-induced realigning the osseous structures provided an opportunity of return of the vertebral artery into its normal course.
CLINICAL FEATURES
Because of the rarity of the pathology and lack of pain or any other significant neurological symptom, the diagnosis may be delayed. With minimal amounts of subluxation, patients may complain of only neck pain. With more severe degrees of subluxation or dislocation, torticollis may be noted and the patient may present with the typical “cock robin” posture with the head tilted toward one side and turned (rotated) toward the other and in slight flexion. For example, in a right-sided unilateral anterior rotatory subluxation (right-sided atlas lateral mass subluxated anteriorly), there is lateral bending of the head and neck to the right and rotation of the head to the left. When an attempt is made to turn the head opposite to the direction it faces, it is found to be difficult; however, rotating it further in the direction in which it faces is possible. On palpation, the C2 spinous process may be prominent and deviated to the side to which the chin is pointed, as a result of the lateral tilt of the head or from counterrotation of C2; this is done in an attempt to realign the head.[3]
In the acute setting, it is important to distinguish between true rotatory atlantoaxial dislocation and muscular torticollis. In rotatory atlantoaxial dislocation, the sternomastoid spasm is on the side of the chin whereas in muscular torticollis, the spasm is on the contralateral side. In rotatory dislocation, the sternomastoid spasm on the side of the chin is secondary or reflexive, as if the muscle is attempting to correct the deformity.[3]
Neurologic involvement is uncommon; however, occipital neuralgia may occur because the greater occipital nerve runs in close proximity to the C1–C2 facet capsule.[3]
CLASSIFICATION
Fielding and Hawkins classification
Fielding and Hawkins classified rotatory atlantoaxial dislocation into four types.[3]
-
Type I: Rotatory atlantoaxial dislocation with no anterior displacement of the atlas (atlantodental interval of 3 mm or less)
The transverse ligament is intact and the dens acts like a pivot. The rotation of the atlas on the axis is >45°. This is the most common type of rotatory atlantoaxial dislocation
-
Type II: Rotatory atlantoaxial dislocation with anterior displacement of the atlas by 3–5 mm
This type is associated with deficiency of the transverse ligament and unilateral anterior displacement of one lateral mass of the atlas while the opposite joint is intact and acts as the pivot. In these patients, there is abnormal anterior displacement of the atlas on the axis, and the amount of fixed rotation is in excess of normal maximum rotation. The rotation usually exceeds 40°
-
Type III: Rotatory atlantoaxial dislocation with anterior displacement of atlas by more than 5 mm
This type is associated with disruption of both the transverse and alar ligaments. Both lateral masses of the atlas are displaced anteriorly, one more than the other, thus producing the rotated position. The rotation is more than 40°, and the atlas is displaced forward from the odontoid by more than 5 mm
-
Type IV: Rotatory atlantoaxial dislocation with posterior displacement of atlas
This type is rare and occurs when the odontoid process is deficient or fractured. There is a posterior shift of one or both lateral masses of the atlas, one of them shifting more than the other thus causing rotation
Levine and Edwards[20] added to this classification by describing the extreme injury pattern of rotatory dislocation
Type V: Frank rotatory atlantoaxial dislocation.
Goel and Shah classification
The facetal locking was divided into two types: rotatory and translatory.[7]
Rotatory locking: Rotatory locking was when the head was in torticollis or “rotated” position. Rotatory locking was “partial” when the facet of atlas of only one side was dislocated anteriorly over the facet of axis. The facet on the contralateral side was not abnormally positioned and acted as a pivot for the dislocation. Rotatory locking was complete when the facets of atlas on both sides were dislocated over the facets of axis in a rotatory fashion. The process resulted in facet of atlas being positioned anterior to facet of axis on one side and posterior to it on the other side [Figure 3]
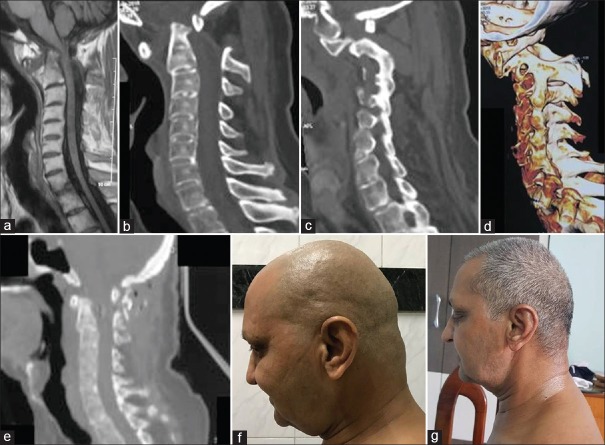
Translatory dislocation: Translatory dislocation was described as a condition when facets of atlas on both sides were dislocated anterior to the facets of axis. Such a dislocation resulted in a fixed flexion neck deformity [Figures 5 and 6]. Although a posterior translation is also technically possible, such cases were not encountered.
Figure 5.
Images of a 12-year-old boy. (a) Lateral radiograph with the head in flexion showing translatory dislocation. The C1 vertebra is dislocated anteriorly. (b) Lateral radiograph with the head in extension showing no reduction of the dislocation. (c) Sagittal computed tomography scan showing the atlantoaxial dislocation. (d) Three-dimensional computed tomography reconstruction revealing the translatory dislocation of C1 over C2. (e) Photograph of the boy holding his head with thumb over the chin to look ahead. (f) Postoperative computed tomography scan showing reduction of the dislocation
Figure 6.
Images of a 51-year-old male patient. (a) T1-weighted magnetic resonance imaging showing the craniovertebral junction and atlantoaxial instability. (b) Computed tomography scan showing the atlantoaxial dislocation. (c) Computed tomography scan of the facets showing Type 1 atlantoaxial facetal instability. (d) Three-dimensional computed tomography scan shows anterior translation of both facets of atlas over facets of axis. (e) Postoperative computed tomography scan shows craniovertebral fixation. (f) Preoperative clinical picture shows fixed flexion deformity of the head. (g) Postoperative clinical image shows normalization of head posture
TREATMENT
It is important to recognize atlantoaxial rotatory fixation as there maybe an underlying compromised atlantoaxial complex with the potential to cause neurological damage or even sudden death.
Traditional treatment guidelines based on the classification of Fielding and Hawkins[3] are as follows:
Type I lesion, which is the most benign may be treated with cervical spine immobilization after reduction
For Type II lesions, if reduction is achieved within 14 days of luxation in children, subsequent immobilization with halo was recommended. For Type II lesions associated with occipitoatlantal dislocation and/or when the diagnosis was delayed for more than 14 days, a posterior atlantoaxial or occipitoatlantoaxial arthrodesis was recommended
Type III and IV lesions were all treated with posterior arthrodesis after reduction.
Fielding and Hawkins[3] described children in whom the diagnosis of rotatory atlantoaxial subluxation was not made for months and in whom traction was unsuccessful in achieving a satisfactory reduction or relief of the symptoms. They performed an arthrodesis of atlas and axis in these patients and achieved resolution of the torticollis. They made no attempt intraoperatively to realign the atlas on the axis. Manipulative reduction of rotatory atlantoaxial subluxation may be indicated in selected patients with recent onset of torticollis; but, there is less risk when reduction is achieved by bed rest or by traction without manipulation.
Various authors have performed atlantoaxial facet joint manipulation in rotatory atlantoaxial dislocation and effected a reduction of the dislocation. Schmidek et al.[21] used a transoral route, Crockard and Rogers[22] employed an extreme lateral approach, and Goto et al.[23] released the atlantoaxial lateral facet joint by a transoral surgery and followed it up by a posterior fixation using interlaminar clamps. Goel et al.[24] achieved a reduction of the fixation with direct joint manipulation and subsequent fixation. Continuous monitoring of the neurological status of the patient is essential during any manipulative reduction. After reduction, some form of cervical immobilization is used to prevent recurrent subluxation. Immobilization presumably allows the stretched or edematous ligaments to heal and to return to their normal length. Full, pain-free motion of the neck should be restored before external immobilization is discontinued.
Phillips and Hensinger[25] recommended a treatment plan that is based on the duration of the torticollis. Patients who have had a rotatory subluxation of <1-week duration can be treated with immobilization in a soft collar and bed rest for a week. Close follow-up is essential. If reduction fails to occur spontaneously, then the patient should be hospitalized and given traction. In patients with rotatory subluxation of more than 1-week duration but <1-month duration, hospitalization and cervical traction are indicated. After reduction, immobilization for 4–6 weeks is recommended. In patients with subluxation of more than one month's duration, cervical traction can be attempted for up to 3 weeks. If reduction does not occur, an arthrodesis should be performed.
Treatment protocol
The patients can first be treated with attempts at closed reduction using cervical halter traction or a halo cervical traction for a period of about 3–4 weeks. In case the deformity reduced significantly, an attempt toward conservative observation can be made. The traction can then be removed, and the patient is placed on firm cervical collar for a period of 2 months. If the neck tilt is reduced or treated, the patient can be further observed. Otherwise, it is in the short- and long-term interest of the patient that atlantoaxial fixation is done.
Nonoperative treatment
A number of cases of reducible atlantoaxial facet subluxation can be treated nonoperatively using closed reduction. The patient must undergo a trial of conservative treatment. Due to the relative rarity of the dislocation and only limited reports in the literature, it is not possible to provide an approximate incidence of the event or describe which cases with which injury will recover after conservative or nonoperative treatment. On the basis of reducibility of the dislocation, facet locking can be subdivided into reducible or irreducible types. Some authors advise the use of direct cervical traction or progressive halo brace traction for varying periods. An analysis of the result of traction and modifying the surgical strategy is accordingly carried out. If during the period of conservative therapy, the rotatory dislocation diminishes and remains reduced on dynamic imaging, there is no need for surgery. Immobilization presumably allows the stretched or edematous ligaments to heal and to return to their normal length and function. Full, pain-free motion of the neck should be restored before external immobilization is discontinued. However, we observed that most children tolerated traction poorly, and in none of the cases in the present series did traction result in a permanent repositioning of the facet joints to a normal alignment. Based on our experience, we found that failure of a 2-month period of conservative treatment to restore normal neck stature arguably indicates that surgical realignment should be considered, as proposed. It appears that too much delay can result in local bone fusion that can affect surgery. In all of our patients, closed reduction or a conservative observation had already failed. Although the long-term outcome of untreated rotatory atlantoaxial dislocation has not been elaborately described in the literature, one can expect to find fusion to have occurred in the dislocated position. Delayed lower and midspinal deformities are possible, which will contribute to a patient's head facing straight ahead.
Goel technique of opening of the atlantoaxial joint and direct manipulation of the facets for reduction of rotatory atlantoaxial dislocation
We employed the technique of opening of the joint, distraction and manipulation of the facets, and reduction of rotatory atlantoaxial dislocation.[7] The technique is relatively complex and tedious, particularly so in the presence of intact neurological condition of the patient. However, reduction of the rotatory dislocation is possible by this technique [Figures 3 and 4]. Holding and manipulation of the spinous process of axis, posterior arch of atlas, and the facets of atlas and axis can result in reduction of the rotatory dislocation. We believe that our modality of treatment has revolutionized the management of rotatory atlantoaxial instability.
Surgical technique
After induction of anesthesia, the patient is placed under cervical traction, the weights ranging from 3 to 6 kg. The head end of the table is raised approximately 35° to provide countertraction by the body. This position assists in reducing the venous congestion in the operative field, particularly in the vein-rich region of the lateral masses. The exposure of the atlantoaxial joint in cases of facet joint malalignment is significantly more difficult and technically challenging than a normally aligned atlantoaxial joint encountered during the treatment of posttraumatic instability. However, we did observe that, in all cases, intraoperative traction resulted in an improvement in the alignment of the facets compared with their preoperative alignment. The atlantoaxial facet joints are widely exposed on both sides after sectioning of the large C2 ganglion. Such a wide exposure provides an opportunity to observe the status of the facets and direct manipulation. The joint capsule is excised, and the articular cartilage is widely removed using a microdrill. The joints on both sides are distracted using an osteotome. The flat edge of the osteotome is introduced into the joint, and it is then turned vertically to effect distraction and further manipulation. The sizes of the osteotomes can be varied depending on the local situation. The sequence of facet manipulation varies, but in general, the more easily approachable facetal articulation is treated first. When necessary, the distraction is done simultaneously on both sides. Although visualization of the region is possible with high-definition radiography or intraoperative CT scanning, such investigations were not performed. Direct observation of the position and alignment of the articular surfaces of the atlantal and axial facets is the key to facet realignment. Another indicator of successful realignment is the location of the tip of the C2 spinous process in relationship to the midline of the arch of atlas. Sectioning of the C2 ganglion can be done to achieve wide exposure and also provides an opportunity for identifying the most appropriate site for placement of C2 screws, as we have previously discussed. Wherever possible, C2 screw placement can even be transarticular. Such a screw placement provides additional stability to the joint. We labeled this method of fixation as “double-insurance” fixation.[26] The use of neuronavigation can assist in screw insertion and avoiding the course of the vertebral artery. Such additional precautions are more relevant in cases with rotatory dislocation because the location of the vertebral artery can be altered due to rotation. Exact preoperative evaluation of the status of vertebral artery is mandatory. Corticocancellous bone graft material harvested from the iliac crest is packed into the joint in small pieces. Subsequent fixation of the joint, with the help of interarticular screws and a metal plate, provides a biomechanically firm fixation as well as sustained distraction and realignment. In cases in which the facet of atlas was dislocated anteriorly and manual realignment was incomplete, the screw (with the plate) was first inserted into the lateral mass of the axis and was tightened. The atlantal screw was then tightened over the fixed plate. This variation resulted in posterior movement of the facet of atlas. A similar technique of reduction has been described in the treatment of spondylolisthesis. Larger pieces of corticocancellous bone graft were placed in the midline over the arch of atlas and lamina of axis after appropriately preparing host bone. Postoperatively, traction is discontinued, and the patient is placed in a 4-posthard cervical collar for 3 months, and all physical activities involving the neck are restrained during the period. After a 4-month period, all activities, including sports, were permitted in an unrestrictive manner in our patients.
Course of surgery
In no case did we observe any ligament tear or any bone fracture that could be identified as a reason for preventing the normal joint movements. In some cases, the ligaments in the region appeared to have an unusually gray hue and were swollen. Histological examination of the tissue was not carried out. There were no operative complications. There were no cases of infection, hardware failure, or need for reexploration.
Follow-up
Improvement or recovery from torticollis can be expected in the immediate postoperative and sustained resolution of positional neck abnormality [Figures 1–6]. The degree of neck deformity recovery is measured by the angle described earlier (angle between a line that coursed from the nasion, tip of the nose, and symphysis menti to the horizontal).[7] All neck movements, particularly rotation, are marginally limited in all cases, but they were significantly improved compared with the preoperative status. Arthrodesis was assumed if the neck retained its normal alignment after a period of 6 months. Based on this parameter, successful fusion was achieved in all patients.
Our encouraging experience suggests the validity of our procedure and its positive effects on clinical outcome. Our long-term experience with opening of the atlantoaxial joint and with facet manipulation in the treatment of atlantoaxial dislocation and basilar invagination assisted in the overall operation. Although technically challenging and anatomically precise, the procedure results in excellent restoration of the facet joint alignment and neck shape and satisfactory neck movements. Because the fixation of the craniovertebral junction was segmental at atlantoaxial joint, the rest of the neck and even the occipitoaxial joint provided an avenue for neck movements. Although quantitative assessments were not possible, we did note restriction of neck flexion and rotation compared with healthy children. The restriction of neck movements appeared more pronounced than in patients treated with the same technique for mobile and reducible atlantoaxial dislocations. The exact cause of this variation is unclear, but structural alterations in cases involving facet dislocation appear to be one possibility.
CONCLUSIONS
Rotatory atlantoaxial dislocation and related neck torticollis can be a physically crippling disorder. The difficulties associated with exposure and manipulation of the atlantoaxial joint for reduction of the rotatory dislocation, particularly in neurologically intact patients, make surgery for this problem a difficult therapeutic issue. The proposed operation of atlantoaxial facetal manipulation and reduction necessitates fixation of the joint. A technique that will reduce dislocation and permit movements of the atlantoaxial joint needs to be identified.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Goel A. Treatment of odontoid fractures. Neurol India. 2015;63:7–8. doi: 10.4103/0028-3886.152657. [DOI] [PubMed] [Google Scholar]
- 2.White AA, Panjabi MM. Clinical Biomechanics of Spine. 2nd ed. Lippincott (Pub); 1990. [Google Scholar]
- 3.Fielding W, Hawkins RJ. Atlantoaxial rotatory fixation – Subluxation. J Bone Joint Surg Am. 1977;59:37–44. [PubMed] [Google Scholar]
- 4.Cacciola F, Phalke U, Goel A. Vertebral artery in relationship to C1-C2 vertebrae: An anatomical study. Neurol India. 2004;52:178–84. [PubMed] [Google Scholar]
- 5.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 6.Vertical mobile atlantoaxial dislocation. J Neurosurg Spine. 2009;11:9–14. doi: 10.3171/2009.3.SPINE08927. [DOI] [PubMed] [Google Scholar]
- 7.Goel A, Shah A. Atlantoaxial facet locking: Treatment by facet manipulation and fixation. Experience in 14 cases. J Neurosurg Spine. 2011;14:3–9. doi: 10.3171/2010.9.SPINE1010. [DOI] [PubMed] [Google Scholar]
- 8.Goel A. Goel's classification of atlantoaxial “facetal” dislocation. J Craniovertebr Junction Spine. 2014;5:3–8. doi: 10.4103/0974-8237.135206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goel A, Shah A. Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine. 2009;10:220–7. doi: 10.3171/2008.12.SPINE08499. [DOI] [PubMed] [Google Scholar]
- 10.Bell C. The nervous system of the human body. Embracing the papers delivered to the Royal Society on the subject of nerve. Case. 1830;143:403. [Google Scholar]
- 11.Corner EM. Rotary dislocations of the atlas. Ann Surg. 1907;45:9–26. doi: 10.1097/00000658-190701000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wortzman G, Dewar FP. Rotary fixation of the atlantoaxial joint: Rotational atlantoaxial subluxation. Radiology. 1968;90:479–87. doi: 10.1148/90.3.479. [DOI] [PubMed] [Google Scholar]
- 13.Wittek A. Ein fall von distensionsluxation im atlanto-epistropheal-gelenke. Muenchener Med Wochenschr. 1908;55:1836–7. [Google Scholar]
- 14.Coutts MB. Atlanto-epistropheal subluxations. Arch Surg. 1934;29:297–311. [Google Scholar]
- 15.Fiorrani-Gallotta, Giovanni, Luzzatti G. Sublussazione laterale e sublussazione rotatorie del l'atlante. Arch Ortop. 1957;70:467–84. [PubMed] [Google Scholar]
- 16.Jones RW. Spontaneous hyperaemic dislocation of the atlas. Proc R Soc Med. 1932;25:586–90. [PMC free article] [PubMed] [Google Scholar]
- 17.Grisel P. Enucleation de l'atlas et torticollisnaso-pharyngien. Presse Med. 1930;38:50–3. [Google Scholar]
- 18.Hess JH, Bronstein IP, Abelson SM. Atlanto-axial dislocations. Unassociated with trauma and secondary to inflammatory foci in the neck. Am J Dis Child. 1935;49:1137–47. [Google Scholar]
- 19.Goel A, Jankharia B, Shah A, Sathe P. Three-dimensional models: An emerging investigational revolution for craniovertebral junction surgery. J Neurosurg Spine. 2016;25:740–4. doi: 10.3171/2016.4.SPINE151268. [DOI] [PubMed] [Google Scholar]
- 20.Levine AM, Edwards CC. Treatment of injuries in the C1-C2 complex. Orthop Clin North Am. 1986;17:31–44. [PubMed] [Google Scholar]
- 21.Schmidek HH, Smith DA, Sofferman RA, Gomes FB. Transoral unilateral facetectomy in the management of unilateral anterior rotatory atlantoaxial fracture/dislocation: A case report. Neurosurgery. 1986;18:645–52. doi: 10.1227/00006123-198605000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Crockard HA, Rogers MA. Open reduction of traumatic atlanto-axial rotatory dislocation with use of the extreme lateral approach. A report of two cases. J Bone Joint Surg Am. 1996;78:431–6. doi: 10.2106/00004623-199603000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Goto S, Mochizuki M, Kita T, Murakami M, Nishigaki H, Moriya H, et al. Transoral joint release of the dislocated atlantoaxial joints combined with posterior reduction and fusion for a late infantile atlantoaxial rotatory fixation. A case report. Spine (Phila Pa 1976) 1998;23:1485–9. doi: 10.1097/00007632-199807010-00010. [DOI] [PubMed] [Google Scholar]
- 24.Goel A, Kulkarni AG, Sharma P. Reduction of fixed atlantoaxial dislocation in 24 cases: Technical note. J Neurosurg Spine. 2005;2:505–9. doi: 10.3171/spi.2005.2.4.0505. [DOI] [PubMed] [Google Scholar]
- 25.Phillips WA, Hensinger RN. The management of rotatory atlanto-axial subluxation in children. J Bone Joint Surg Am. 1989;71:664–8. [PubMed] [Google Scholar]
- 26.Goel A. Double insurance atlantoaxial fixation. Surg Neurol. 2007;67:135–9. doi: 10.1016/j.surneu.2006.05.059. [DOI] [PubMed] [Google Scholar]