Abstract
Medication error (ME) is an adverse preventable event which happens due to the inappropriate use of medication that leads to patient harm. Such events may be related to professional practice, health-care products, procedures, and systems including prescribing, communication, product labeling, packaging, and nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use. A major ME is the one, which results in either permanent harm or transfer to the intensive care units or death. When an error is identified, it shall be reported immediately. It must also be nonpunitive so that staff does not have to be afraid of repercussions. An error shall be reported to the concerned consultant immediately. Continuous monitoring and frequent assessments shall be done for the patient. A root cause analysis shall be done for all serious MEs.
Keywords: Administration, dispensing education, medication errors, monitoring
Introduction
The health-care system in India is evolving with the rapid increase in population. The health-care system is a complicated and complex system that involves the interaction between multiple professionals, institutions, and significantly depends on the revolutionized and improvised technology. The complexity of the health-care system may increase the risk to the health of the population in the country, which in turn may worsen or deteriorate the complication arising from these mistakes. It is the utmost duty of the government and health-care governing body throughout the world to provide infrastructure and health-care professionals to provide health care for all.[1] Primary care services or primary health centers are the core of the health-care system in the country that are the initial steps which integrate people in the health-care systems. It is the entry point of the health-care system of the country which focuses on coordination of care and has a targeted approach toward people and their families. Compromised primary health care may lead to unavoidable illness, and increases morbidity and mortality. Medications are the primary intervention in the health-care setups provided by health services in all the countries. In the modern world, there is an increasing trend of the use of medication for early relief that may substantially increase medication error (ME) and increase the risk to the general population.
The National Coordinating Council for ME Reporting and Prevention has defined MEs as, “Any preventable event that may cause or lead to inappropriate medication use or patient harm, while the medication is in the control of the health-care professional, patient, or consumer.”[2] The American Society of Hospital Pharmacists guidelines for MEs stated that the incidence of MEs cannot be exactly ascertained as different organizations have different definitions and methods to calculate MEs.[3] MEs have a significant impact on the patient and health-care system monetary due to increase in morbidity or mortality.
Incidence and Prevalence of Medication Error
MEs, worldwide, are not reported unless they cause significant causality. These issues may be reflected in the varying error prevalence rates worldwide.[4] It is estimated by the Institute of Medicine that the health-care cost due to MEs in the US is approximately $37.6 billion/year out of which nearly about $17 billion is spent for preventable errors.[5] It has been estimated worldwide, MEs form a prominent component of the adverse events and mortality cases. In the study done by Avery et al. in the United Kingdom, it was found that nearly 38% of the patients in the age group of above 75 years had either prescription or monitoring error which accounts for nearly one-tenth of primary care patients. MEs were found more in patients (30%) who were on polypharmacy.[6] Claesson et al. found a high rate of MEs (42%) in a study in Sweden. Most of these errors were prescriptions error, and others were due to an incorrect dose taken by the patient.[7] In a study done in Saudi Arabia, Khoja et al. found that nearly one-fifth of primary care prescriptions led to MEs, but few were serious.[8] Zavaleta-Bustos et al., done a study in Mexico, he found that most of the prescription errors in his study were related to dosage regimen, and it was approximately 28%.[9] It is really difficult to estimate the prevalence of MEs in the health-care system, as there are various definitions and classification systems. It normally depends on the denominator used, i.e., patient, prescription, or a specific medication.
In India, incidences of ME were as reported by the state government of Uttarakhand (26%) and Karnataka (14%).[10,11] It showed that our system was not concrete to prevent the avoidable harm of ME in the country.
Impact of Medication Errors on Health-Care System
MEs have an unfavorable impact on individuals as well as health-care economics. It includes undesirable adverse drug reactions, drug-drug interactions, decrease the efficacy of drugs, no adherence to management, which leads to a decrease in the quality of life and experience of the patient. These adverse events may, in turn, have significant consequences on the health of individuals and deteriorate the economic conditions of health care. These adverse events may increase the use of health-care services, increase in medication-related hospital admissions and some cases may lead to death.[12] It may contribute to approximately 6%–7% of admissions in some countries which are mostly avoidable and preventable cases.[13,14] These MEs related problems are more prevalent in the elderly as they are on risk to polypharmacy and related multiple factors.[15]
Types and Causes of Medication Errors
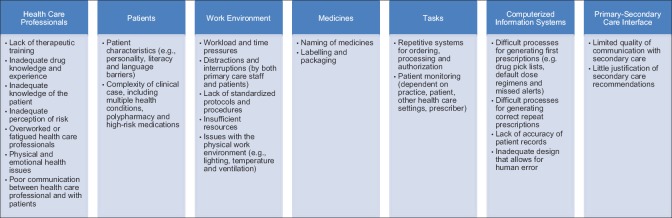
MEs can be understood better if we consider their classification based on contextual, modal, or psychological. In our text, we will consider psychological classification as it explains the real events. One of the disadvantages of this classification is that it data concentrates more on human than the systems which generate the errors. The following psychological classification is based on the work of reason on errors in general.[16] There are four broad types of MEs [Figure 1].[17]
Figure 1.
Types and causes of medication errors
Knowledge-based errors (through lack of knowledge), for example, giving penicillin, without having established whether the patient is allergic. In an Australian study, communication problems with senior staff and difficulty in accessing appropriate drug-dosing information contributed to knowledge-based prescription errors.[18] Knowledge-based errors are better avoided by updating the information about the prescribed drug and knowing the identity of the patient for whom the drug is prescribed. Computerized prescribing systems, bar-coded medication systems, cross-checking by others (e.g., pharmacists and nurses) and education can help to intercept such errors[19,20]
Rule-based errors (using a bad rule or misapplying a good rule), for example, injecting diclofenac into the lateral thigh rather than the buttock. The basic knowledge to avoid these types of errors is proper training, education, and implementation of rules for the health-care workers
Action-based errors (called slips), for example, picking up a bottle containing diazepam from the pharmacy shelf when intending to take one containing diltiazem. These errors are mostly due to the carelessness and ignorance occurred during routine prescribing, dispensing, or drug administration. These can be minimized by creating conditions in which they are unlikely (e.g., by avoiding distractions, by cross-checking, by labeling medicines clearly, and using identifiers, such as bar-codes);[21] so-called “Tall Man” lettering (mixing upper- and lower-case letters in the same word) has been proposed as a way to avoid misreading of labels,[22] but this method has not been tested in real conditions. Technical error is a subset of action-based errors that can be prevented by the use of checklists, fail-safe systems, and computerized reminders.[23] The example of a technical error is like putting the wrong amount of potassium chloride into an infusion bottle
Memory-based errors (called lapses), for example, giving penicillin, knowing the patient to be allergic, but forgetting. Computerized prescribing systems and by cross-checking of patient's drug allergy can intercept and prevent these type of error.
Causes of Medication Errors
ME can be defined as “a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient.”[17] The “treatment process” involves all medications, as defined above. The causes of MEs are described in Figure 1.
Choosing a medicine – irrational, inappropriate, and ineffective prescribing, underprescribing and overprescribing
Writing the prescription – prescription errors, including illegibility
manufacturing the formulation to be used – wrong strength, contaminants or adulterants, wrong or misleading packaging
Dispensing the formulation – wrong drug, wrong formulation, wrong label
Administering or taking the drug – wrong dose, wrong route, wrong frequency, wrong duration
Monitoring therapy – failing to alter therapy when required, erroneous alteration.
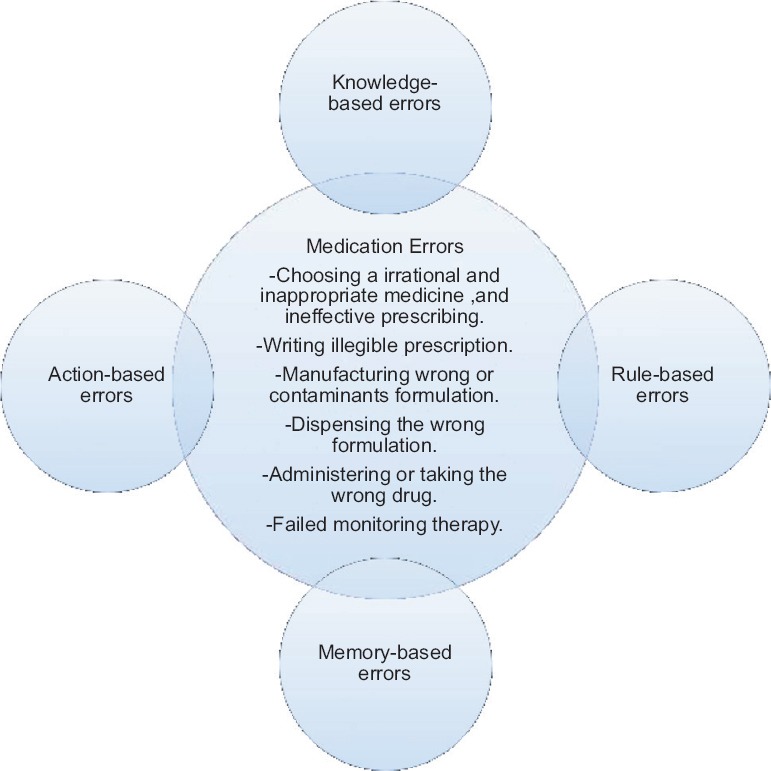
Factors Associated With Medication Errors
The important factors which lead to ME are as follows and given in Figure 2.[10,24]
Figure 2.
Factors affecting medication errors
Vulnerable patient's populations are more prone to MEs. The factors which lead to MEs in these patients are due to their personality, literacy, language barriers, complicated case, multiple comorbid conditions, polypharmacy, and high-risk medications (chemotherapy and opioids)
The working environment is an important area of health-care systems. Ineffective and insufficient working environment may lead to disruption of the health-care system, which in turn may lead to MEs, one of its consequences. The factors involved are an increase in workload or time pressures of the health-care professionals, disruptions in the workplace by the health-care staff and patients, no implementation of standardized protocols, no standard procedures, lack of resources and improper lighting, temperature, and ventilation issues in the working area
Information Technology: One of the important barriers is the communication between the primary and secondary care system. One of the important causes of MEs in the modern world is the adaptability of the health-care professionals with the use of computerized information systems. MEs are due to happen when there is a lack of skills to work with computers which may generate wrong prescriptions. The information system of the hospital should be updated with the correct drug lists; treatment-based dose regimens, missed alerts for the staff, maintenance of patient records and improved the flaws in the design of the system to correct human error. In the area of medicines, naming and packaging of drugs are the most important factors.
Prevention of Medication Errors
MEs and drug-related adverse events have an important impact on the health-care system as it increases the length of hospital stay and leads to discomfort and disability or increased mortality.[25,26] A complex series of system problems lead to MEs. It requires a multidisciplinary approach to pacify the systemic nature of the problems. In the medical literature, many solutions are proposed to fight the menace of MEs. Clinical pharmacologists, clinical pharmacists, and information technology are the core requirements of a multidisciplinary approach for improving the problem of MEs in the society. It has been proposed to consider two approaches for considering errors and accidents.[27] It is foremost important to identify individual problems, and deficiencies that lead to ME and second, the systems at fault should be analyzed.[28] If both the approaches are at faults, then it would lead to most accidents.[29] These approaches should focus on the special population, such as children and the elderly. It should target-specific clinical areas and diseases. These interventions lead to reduce hospital admission and death.
There are various tools which can be applied during prescribing, transcribing, dispensing, administering, and monitoring patient medications to prevent MEs. These are computerized physician order entry (CPOE); clinical decision support systems (CDSS); computerized monitoring of adverse drug events; pharmacist-assisted rounds; high-risk drug protocols; and verbal order verification. The application of these tools will significantly reduce MEs, improved the quality of health care and patient management.
Prescribing
Computerized physician order entry
Computerized provider order entry (CPOE) is the electronic process to strengthen the electronic prescription with alert systems. It is inbuilt with decision support that may be useful to target the potentially inappropriate prescriptions errors or wrong medications and alert the health-care professionals on clinically relevant warnings. In-patient setting has substantial proof to support the use of CPOE in health-care systems as it decreases the frequency of MEs.[30] CPOE helps the physician to order medications, tests, and procedures directly into the hospital computer system, thereby eliminating errors related to illegible handwriting. The errors related to prescribing such as dose, route, and frequency of administration are avoided with the use of CPOE. Several studies have demonstrated CPOE's ability to decrease the rate of MEs and increase compliance with recommended prescribing regimens.[31,32,33,34]
There is a significant investment required in CPOE, but the return is quite significant not only monetarily but also improvements in resource utilization and reductions in testing and imaging.[35] Improved data collection with the help of accurate coding enable the hospitals to increase physician reimbursements and also decrease the physician liability insurance premiums.[36,37]
CPOE will particularly improve communication efforts during the transfer of care of the patients. Decrease communication and lack of care during hospitalization have been associated with increased risk of adverse events, such as MEs.[38,39] CPOE has the potential to reduce the prevalence of preventable adverse drug events (pADEs) inpatient. CPOE has a major role to play for the benefit for patient health.
Computerized decision support systems
Computerized provider order entry (CPOE) with clinical decision support systems (CDSS) are used regularly in the hospital to review of orders as they are written, comparing new and existing orders, set-up to check for allergies, drug-drug interactions, appropriate dosing schedules, and alerting the physician to pertinent laboratory results, all of which impact the physician's decisions and the plan of care for the patient.[40] It enhances the clinical practices of prescribing. This system has the capability to identify and prevent duplications related to medications, testing, and imaging.
Clinical pharmacologist-assisted rounds
Clinical pharmacologist is the most easily accessed tools in making medication decisions. Clinical pharmacologist should update the list and consistently review prescriptions written by clinicians, as they are familiar with the institution's formulary, can assist physicians in selecting medications from among those drugs that are stocked for the patient during the hospital stay as well as when he gets discharged by addressing the discrepancies of medications in the discharge papers, addressing polypharmacy and focusing on the rational use of drugs to minimize the threat to patient health.[30] Formulary medications often have a lower cost and a higher reimbursement rate than nonformulary medications. Clinical pharmacologists should review order sets for compliance with formulary drug list and reduce the intake of inappropriate medications.
In the multidisciplinary interventions, nursing staff plays an important role as they intercept the prescription errors before it reaches to the patient. Ambiguous information, duplicate medications, and errors due to incorrect information added in the computer system are the common prescribing errors encountered at the nursing stations.
Handwriting
CPOE and standardized order protocol in the hospital will help to eradicate handwriting errors that lead to MEs and adverse patient events.[41] The hospitals are implementing and displaying a predetermined set of abbreviations according to health-care standards to minimize dual interpretations of the same abbreviations. The handwritten orders should be legible, complete, and reviewed at the nursing station by the pharmacist or appropriate staff to ensure the intended interpretation and transcription. Medication name, dosage form, dose, route, and frequency should be checked thoroughly in the prescription. It should contain the legible signatures of the physician accompanied by his/her printed name. All instructions should be written rather than abbreviated.
Abbreviations
MEs associated with units of measure, for example, using milligrams instead of milliliters are the common mistakes seen in the health-care system. The Institute for Safe Medication Practices (ISMP) has compiled a list of dangerous abbreviations, acronyms, and symbols for handwritten, patient-specific communications as described in Table 1. Although electronic prescription of medication is accepted worldwide for the rational and safe use of medications, they eliminate the possibility of MEs related to abbreviations if not used properly.
Table 1.
List of dangerous abbreviations, acronyms, and symbols for handwritten, patient-specific communications
| Abbreviation | Intended meaning | Possible Mis-interpretation |
|---|---|---|
| U | Units | Mistaken as a zero or a four resulting in overdose |
| Ug | Micrograms | Mistaken for “milligram resulting in a 1000-fold overdose |
| QD | Every day | The period after the “Q” has sometimes been mistaken for an “I” and the drug has been given QIID rather than daily |
| QOD | Every other day | Misinterpreted as “QD” or “QID” If the “O” is poorly written, it looks like a period or an “I” |
| SC or SQ | Subcutaneous | Mistaken as “SL” (sublingual) when poorly written. |
| AZT | Zidovudine (retrovir) | Mistaken as azathioprine or aztreonam |
| MTX | Methotrexate | Mistaken as mitoxantrone |
| Norflox | Norfloxacin | Mistaken as norflex |
According to ISMP. ISMP: Institute for Safe Medication Practices
Decimal points
Physicians should use a zero to the left of a dose < 1 (e.g., use 0.1 rather than 0.1) and avoid the use of a terminal zero to the right of the decimal point (e.g., use 5 rather than 5.0) to minimize ten-fold dosing errors.
Transcribing
The speed and accuracy of transcription are improved with electronic order transcription like CPOE. This methods further results in fewer MEs. The use of standardized order is also seen to expedite the transcription of orders.
Verbal order verification
Verbal orders should be avoided, if possible. It is the policy that appropriately licensed and credentialed health-care practitioners may issue verbal and telephone orders within their scope of practice. Only in urgent situations, verbal orders related to medication orders and test is feasible. To ensure safety, verbal orders require a “repeat-back” or “read-back” verification of the complete order by the person receiving the order. The receiving person will repeat the verbal order back to the ordering clinician, and the person giving the order verbally confirms that the repeated order is correct. For example, “one five” should be pronounced instead of “15” by both the parties. The recipients of verbal orders will sign, date, time, and note the order. Prescribers will verify, sign, and date orders within 24 h or as early as possible.
Dispensing
Automated dispensing
Institute for Safe Medication Practices in 2007, along with stakeholders convened a national forum for the development of automated dispensing cabinets for updated medication safe-use guidelines. The use of this technology will apparently decrease MEs.[30] The automated dispensing device will reduce human factors errors, such as “look-alike” and “sound-alike” drugs as given in Tables 2 and 3.
Table 2.
List of look- alike drugs
| Drug | Look- alike drug |
|---|---|
| Magnex Forte 1.5 g | Magnex Forte 3 g |
| Solumedrol 1 g | Solumedrol 500 mg |
| Alex Syrup | Alex Sugar-Free Syrup |
| Rosullin 500 mg | Reflin 1 g |
| Tropine | Pyrolate |
| Cutenox 40 mg | Cutenox 60 mg |
| Kenadion 1 mg | Kenadion 10 mg |
| Dulcoflux 5 mg | Dulcoflux 10 mg |
| Dapomedrol 1 ml | Dapomedrol 2 ml |
| Dytor 40 mg | Dytor 100 mg |
| Avil 25 mg | Lasix 40 mg |
| Haloxan 1 g | Haloxan 2 g |
| Dextrose 5% 500 ml (glass) | DNS (5% dextrosed and 0.2% sodium chloride) 500 ml (glass) |
| Gelofusine 500 ml | Gelaspan 500 ml |
| Kabiven central 2000 ml | Kabiven peripheral 1500 ml |
| Nephrosteril | Aminoven |
| Visipaque | Omnipaque |
Table 3.
List of sound- alike drugs
| Drug | Sound- alike drug |
|---|---|
| ANGlzaar | AMLOzaar |
| budeCORT | budeSAL |
| carCA | carDACE |
| cipLAR tab | cipLOX tab |
| DACTINOmycin | DAPTOmycin |
| DAUNOrubicin | DOXOrubicin |
| DOBUTAmine | DOPamine |
| DoxyCYCLINE | DoxoPHYLLINE |
| Dytor | dytor PLUS |
| ipraVENt | ipraZESt |
| Lignocaine | Lignocaine + ADRENALINE |
| MetoLAR tab | MetoPAR tab |
| NeLCium | NeKSium |
| PAri | PYri |
| Pan | pan D |
| PLAgerine | PLAgerine A |
| quiETAL | quTIPIN |
| R CIN cap | R cinEX |
| ROScillin | REFlin |
| SILOfast | SILdura |
| soLET | soLITEN |
| STALOpam plus | SYNDopa plus |
| TEGRItal | TRENtal |
| vinBLAST | inevinCRIStine |
| VlSlpaque | OMNIpaque |
High-risk drug protocols/policies
Majority of MEs result in death or serious injury to the patient. All efforts, including a focus on high-risk drugs, which cause sentinel events, are worthy goals. Medications that have the highest risk of causing injury when misused are known as high alert/high-risk medications. The high-alert medications are opiates; injectable potassium chloride concentrate; sodium chloride solutions 3%; heparin 25000 International Units; insulin, sedatives, and hypnotics, antipsychotic, antidepressants, neuromuscular blockers; and injectable anticancer drugs as given in Table 4. These drugs to be stored under lock and key with label of high-risk medications and inventory shall be maintained.
Table 4.
List of high risk medicine (according to Institute for Safe Medication Practices)
| 1. Narcotics (controlled drugs, stored under double lock): Morphine, fentanyl and pethidine |
| 2. Opiates: Pentazocine, tramadol |
| 3. Sedatives and hypnotics: Alprazolam, chlordiazepoxide, clonazepam, diazepam, lorazepam, midazolam, zolpidem, phenobarbitone, dexmedetomidine |
| 4. Neuromuscular blocking agents: Atracurium, pancuronium, rocuronium, vecuronium and succinylcholine |
| 5. Intravenous anaesthetic drugs: Ketamine and propofol |
| 6. Chemotherapeutic drugs (anti-cancer): All the drugs: Parental and oral |
| 7. Antithrombotic agents: Warfarin, LMW heparin, fondaparinux, apixaban, rivaroxaban, alteplase, reteplase, tenecteplase and eptifibatide |
| 8. Specific medications: |
| Insulin, injection potassium chloride, injection magnesium sulfate |
| Injection nitroprusside, injection potassium phosphates, injection |
| Vasopressin, injection oxytocin, sodium chloride-hypertonic >0.9% |
| Concentration, methotrexate (oral non-oncologic use). Epoprostenol IV |
| 9. Adrenergic agonist: Epinephrine, norepinephrine and phenylephrine |
| 10. Antiarrhythmics lV: Amiodarone and lidocaine |
| 11. Inotropic medications: Digoxin and milrinone |
| 12. Radiocontrast agents |
| 13. Dialysis solutions, peritoneal and hemodialysis |
| 14. Oral hypoglycemics |
Bar coding
The U. S. Food and Drug Administration (FDA) in 2006 mandated that hospitals use bar codes for medication.[41] Systems are required to phase in the use of bar code technologies. Barcode systems is an automatic identification systems which improves scheduling of medications, doses of medications missed are few, enables efficient drug monitoring, improved medication records, and facilitate better communication. This system helps to identify the right patient, the right drug, and the right dosage.
Administering/monitoring
The administration phase of medication delivery is a significant step to intervene to eliminate the sources of medical error. The use of technology such as automated drug dispensing, unit dose packaging, and the barcoding of drugs will help to eliminate errors in the administration phase of drug delivery.
The identification to detect potential MEs and its solutions can be managed by computerized order entry system or with a decision support system. These systems record the data related to MEs and the near misses, which can be used to analyze the indicators that contribute to MEs and also acts as valuable tools for education and training. Routine audits of patient charts can also be done in hospitals, which also help to identify the flawed practices of medication management in hospital and provide procedures to effectively reduce errors and increase safety. The patient education can also decrease MEs.
Medication administration record
The practice of recording the time, date, and route of ordered drug administration is known as medication administration records (MARs). MAR can function as both a prevention and intervention tool for the management of MEs. Incorporating the MAR into a computerized system results in typed orders and administration information which decreases the potential for errors. The system can also be programmed to require a cosigner for high-risk medications to double-check measure. A computerized MAR can also record data of the administrative drug delivery processes to prevent confusion over whether a dose was administered when it was administered, and other details of administration.
Environmental factors
It is known that working conditions contribute to MEs such as fatigue, poor lighting, an environment full of interruptions, noise, and an excessive workload. Hospitals and ambulatory surgical centers should evaluate and monitor environmental factors to ensure that distractions are kept to a minimum. MEs should be analyzed to determine trends and systems should be rectified if determined to be problematic.
Medication Reconciliation
Reconciliation of medication reduces adverse drug events and optimizes drug therapy across the continuum of care. Technological advances will assist with accomplishing this goal. It is always advisable to track the patient's current medications and those prescribed during discharge. This practice will help for the rational use of medications. According to the Joint Commission, the list of home medications should be handed over to the hospital staff within 24 h of admission for the initial assessment.
Electronic Medical Records
Major arguments in favor of electronic medical records (EMRs) state that its implementation will potentially decrease medication adverse events, improve health, and provide cost savings to health care. EMRs are useful if the knowledge is properly input into the system. They provide easy accessibility of patient records and history to clinicians and different health-care suppliers.
Program on educating health-care providers is a key component in the safety of patients. The interventions involve to provide tools for practicing safe medication prescribing and usage; involving patients in their own medicine management and providing support to the patient to avoid nonadherence to medication management. These interventions, in turn, reduce MEs part of multicomponent interventions. Educational interventions for clinicians on MEs improve prescription practice and dispensing of antibiotics as seen in a review of 47 studies.[42]
These multidisciplinary approaches to medical practices have drastically reduced inappropriate prescribing pattern and bring down the number of adverse drug events.[43]
Medication Errors Scenarios in India
In India, the prevalence of MEs is mostly under-reported due to sparse data on ME apart from the few studies done in a few hospitals. Only a few hospitals in our country looking for health-care accreditation are practicing or have a system to look into ME problem in their hospitals. Even in those hospitals that are having a high standard of health-care practice, the health-care professionals are not trained to detect MEs. There are lacunae in the system of drug delivery from prescription to administration of drugs to the patients. A national program on MEs in the country will definitely improve the health-care scenarios on medications errors, which definitely constitute a major chunk of the submerged iceberg in the health-care fallacies.
Conclusion
Spontaneous reporting of ME requires a structured system in the institution to ensure the participation of all the partners in the multifaceted interventions. These MEs will improve the rational use of drugs by health-care professional, will improve the quality of health-care products, streamline the procedures and system, including prescribing, order communication, product labeling, packaging, and nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and its use.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Duerden M, Avery AJ, Payne RA. Polypharmacy and Medicines Optimisation: Making it Safe and Sound. London: King's Fund; 2013. [Google Scholar]
- 2.The National Coordinating Council for Medication Error and Prevention (NCCMERP) The Council: Moving into the Second Decade “Developing Recommendations and Offering Tools”. 2010 [Google Scholar]
- 3.ASHP guidelines on preventing medication errors in hospitals. Am J Hosp Pharm. 1993;50:305–14. [PubMed] [Google Scholar]
- 4.Gandhi TK, Weingart SN, Borus J, Seger AC, Peterson J, Burdick E, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 5.To Err is Human: Building a Safer Health System. 1st ed. Washington, DC: National Academy Press; 1999. Institute of Medicine. [Google Scholar]
- 6.Avery A, Barber N, Ghaleb M, Franklin BD, Armstrong S, Crowe S, et al. Investigating the Prevalence and Causes of Prescribing Errors in General Practice: The PRACtICe Study. London: General Medical Council; 2012. [Google Scholar]
- 7.Claesson CB, Burman K, Nilsson JL, Vinge E. Prescription errors detected by Swedish pharmacists. Int J Pharm Pract. 1995;3:151–6. [Google Scholar]
- 8.Khoja T, Neyaz Y, Qureshi NA, Magzoub MA, Haycox A, Walley T. Medication errors in primary care in Riyadh city, Saudi Arabia. East Mediterr Health J. 2011;17:156–9. [PubMed] [Google Scholar]
- 9.Zavaleta-Bustos M, Castro-Pastrana LI, Reyes-Hernandez I, Lopez-Luna MA, Bermudez-Camps IB. Prescription errors in a primary care university unit: Urgency of pharmaceutical care in Mexico. Rev Bras Cienc Farm. 2008;44:115–25. [Google Scholar]
- 10.Gaur S, Sinha A, Srivastava B. Medication errors in medicine wards in a tertiary care teaching hospital of a hill state in India. Asian J Pharm Life Sci. 2012;2:56–63. [Google Scholar]
- 11.Kumar KS, Venkateswarlu K, Ramesh A. A study of medication administration errors in a tertiary care hospital. Indian J Pharm Pract. 2011;4:37–42. [Google Scholar]
- 12.Masotti P, McColl MA, Green M. Adverse events experienced by homecare patients: A scoping review of the literature. Int J Qual Health Care. 2010;22:115–25. doi: 10.1093/intqhc/mzq003. [DOI] [PubMed] [Google Scholar]
- 13.Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: Prospective analysis of 18 820 patients. BMJ. 2004;329:15–9. doi: 10.1136/bmj.329.7456.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alexopoulou A, Dourakis SP, Mantzoukis D, Pitsariotis T, Kandyli A, Deutsch M, et al. Adverse drug reactions as a cause of hospital admissions: A 6-month experience in a single center in Greece. Eur J Intern Med. 2008;19:505–10. doi: 10.1016/j.ejim.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Chan M, Nicklason F, Vial JH. Adverse drug events as a cause of hospital admission in the elderly. Intern Med J. 2001;31:199–205. doi: 10.1046/j.1445-5994.2001.00044.x. [DOI] [PubMed] [Google Scholar]
- 16.Reason JT. Human Error. Cambridge: Cambridge University Press; 1990. [Google Scholar]
- 17.Ferner RE, Aronson JK. Clarification of terminology in medication errors: Definitions and classification. Drug Saf. 2006;29:1011–22. doi: 10.2165/00002018-200629110-00001. [DOI] [PubMed] [Google Scholar]
- 18.Nichols P, Copeland TS, Craib IA, Hopkins P, Bruce DG. Learning from error: Identifying contributory causes of medication errors in an Australian hospital. Med J Aust. 2008;188:276–9. doi: 10.5694/j.1326-5377.2008.tb01619.x. [DOI] [PubMed] [Google Scholar]
- 19.Agrawal A, Wu W, Khachewatsky I. Evaluation of an electronic medication reconciliation system in inpatient setting in an acute care hospital. Stud Health Technol Inform. 2007;129:1027–31. [PubMed] [Google Scholar]
- 20.Frush K, Hohenhaus S, Luo X, Gerardi M, Wiebe RA. Evaluation of a web-based education program on reducing medication dosing error: A multicenter, randomized controlled trial. Pediatr Emerg Care. 2006;22:62–70. doi: 10.1097/01.pec.0000195760.97199.7e. [DOI] [PubMed] [Google Scholar]
- 21.Aronson JK. Medication errors resulting from the confusion of drug names. Expert Opin Drug Saf. 2004;3:167–72. doi: 10.1517/eods.3.3.167.31069. [DOI] [PubMed] [Google Scholar]
- 22.Filik R, Purdy K, Gale A, Gerrett D. Labeling of medicines and patient safety: Evaluating methods of reducing drug name confusion. Hum Factors. 2006;48:39–47. doi: 10.1518/001872006776412199. [DOI] [PubMed] [Google Scholar]
- 23.Aronson JK. Medication errors: Definitions and classification. Br J Clin Pharmacol. 2009;67:599–604. doi: 10.1111/j.1365-2125.2009.03415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slight SP, Howard R, Ghaleb M, Barber N, Franklin BD, Avery AJ. The causes of prescribing errors in English general practices: A qualitative study. Br J Gen Pract. 2013;63:e713–20. doi: 10.3399/bjgp13X673739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE prevention study group. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 26.de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: A systematic review. Qual Saf Health Care. 2008;17:216–23. doi: 10.1136/qshc.2007.023622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reason JT. Clinical Risk Management: Enhancing Patient Safety. London: BMJ Publications; 2001. Understanding adverse events: Human factors; pp. 9–30. [Google Scholar]
- 28.Alldred DP, Raynor DK, Hughes C, Barber N, Chen TF, Spoor P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2013;2:CD009095. doi: 10.1002/14651858.CD009095.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Hu SH, Capezuti E, Foust JB, Boltz MP, Kim H. Medication discrepancy and potentially inappropriate medication in older Chinese-American home-care patients after hospital discharge. Am J Geriatr Pharmacother. 2012;10:284–95. doi: 10.1016/j.amjopharm.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 30.Lainer M, Mann E, Sönnichsen A. Information technology interventions to improve medication safety in primary care: A systematic review. Int J Qual Health Care. 2013;25:590–8. doi: 10.1093/intqhc/mzt043. [DOI] [PubMed] [Google Scholar]
- 31.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–6. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 32.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma'Luf N, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6:313–21. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuperman GJ, Gibson RF. Computer physician order entry: Benefits, costs, and issues. Ann Intern Med. 2003;139:31–9. doi: 10.7326/0003-4819-139-1-200307010-00010. [DOI] [PubMed] [Google Scholar]
- 34.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160:2741–7. doi: 10.1001/archinte.160.18.2741. [DOI] [PubMed] [Google Scholar]
- 35.The Leapfrog Group's Patient Safety Practices. The Potential Benefits of Universal Adoption. 2004 [Google Scholar]
- 36.Briggs B. CPOE order from chaos. Health Data Manag. 2003;11:44–8. [PubMed] [Google Scholar]
- 37.Choi JS, Lee WB, Rhee PL. Cost-benefit analysis of electronic medical record system at a tertiary care hospital. Healthc Inform Res. 2013;19:205–14. doi: 10.4258/hir.2013.19.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348:2526–34. doi: 10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- 39.Petersen LA, Brennan TA, O'Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72. doi: 10.7326/0003-4819-121-11-199412010-00008. [DOI] [PubMed] [Google Scholar]
- 40.Classen DC, Bates DW. Finding the meaning in meaningful use. N Engl J Med. 2011;365:855–8. doi: 10.1056/NEJMsb1103659. [DOI] [PubMed] [Google Scholar]
- 41.Kohn LT, Corrigan JM, Donaldson MD, editors. To Err is Human: Building a Safer Health System. Washington, D.C.: National Academy Press; 2000. [PubMed] [Google Scholar]
- 42.Roque F, Herdeiro MT, Soares S, Teixeira Rodrigues A, Breitenfeld L, Figueiras A. Educational interventions to improve prescription and dispensing of antibiotics: A systematic review. BMC Public Health. 2014;14:1276. doi: 10.1186/1471-2458-14-1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pedersen JS, Brereton L, Newbould J, Nolte E. The puzzle of changing relationships. Does Changing Relationships Between Healthcare Service Users and Providers Improve the Quality of Care. London: The Health Foundation; 2013. [Google Scholar]