Abstract
The authors explored the prevalence and impact of the cardiovascular risk factors (CVRFs) in patients presenting with acute coronary syndrome (ACS). During a five‐month period in 2007, six adjacent Middle Eastern countries participated in the Gulf Registry of acute coronary events. CVRFs were identified on admission. Patients' characteristics and in‐hospital outcomes were analyzed across the types of ACS. Among 6704 consecutive patients with ACS, 61% had non–ST elevation ACS (NSTEACS) and 39% had ST–elevation myocardial infarction (STEMI). Female sex, old age, diabetes mellitus, hypertension, dyslipidemia, and obesity were more prevalent in NSTEACS patients. STEMI patients were more likely to be smokers and less likely to be taking aspirin prior to the index admission. Chronic renal failure (CRF) and diabetes mellitus were independent predictors of in‐hospital heart failure in NSTEACS, while CRF and hypertension were predictors of STEMI. Female sex and CRF were independent predictors of mortality in STEMI (odds ratio, 2.0; 95% confidence interval, 1.19–3.13 and odds ratio, 5.0; 95% confidence interval, 3.47–7.73, respectively). Assessment of the prevalence of CVRF in the acute coronary presentation is of important prognostic value for in‐hospital morbidity and mortality. CVRF and its impact may differ according to ACS type, age, and sex.
Coronary heart disease (CHD) is the leading cause of mortality and morbidity worldwide. To achieve a significant reduction in the prevalence of CHD, it is essential to adopt effective preventive strategies with adequate awareness of the epidemiology of cardiovascular risk factors (CVRFs).1 CVRFs include traditional and nontraditional factors. However, the US Preventive Services Task Force concluded that the evidence is insufficient to assess the balance of benefits and harms of using nontraditional risk factors.2, 3 The World Health Organization has recognized obesity, hypertension, hypercholesterolemia, and smoking among the top10 traditional risk factors for premature death and morbidity.4 Since these risk factors are usually evident before developing CHD, knowledge of their prevalence in a given population allows the prediction of the likely burden of CHD.3 The American Heart Association has recognized many risk factors; some can be modified, treated, or controlled and some can not.5 The more risk factors present, the greater the likelihood of developing CHD. Currently, most reports for prevention of CHD are mainly derived from European centers and suggest that risk factors for CHD are varying from country to country.6 However, data from the Arab Middle East that evaluate the prevalence and impact of these risk factors in acute coronary events are scarce.4, 7, 8 We explore the prevalence of CVRFs in patients with acute coronary syndrome (ACS) who are living in the Arab Middle East and the impact of these factors on in‐hospital heart failure (HF) and mortality. Copyright © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Methods
Patients and Protocol
The data were collected from a prospective, multicenter, observational study of the Gulf Registry of Acute Coronary Events (Gulf RACE). For five months in 2007, Gulf RACE recruited 6704 consecutive ACS patients from 64 hospitals in six Middle Eastern countries (Bahrain, Kuwait, Qatar, Oman, United Arab Emirates, and Yemen). Full details of the methods have been previously published.9, 10 Diagnosis of the different types of ACSs (ST–elevation myocardial infarction [STEMI] and non‐ST elevation ACS [NSTEACS]) and definitions of data variables were based on the American College of Cardiology clinical data standards.10, 11 CVRFs, including traditional and nontraditional clinical risk factors, were identified on admission. Traditional CVRFs included age, sex, diabetes mellitus (DM), hypertension, dyslipidemia, obesity, smoking, and family history of coronary artery disease (CAD). Other possible nontraditional risk factors or risk factor equivalents included metabolic syndrome, chronic renal failure (CRF), history of prior CAD, coronary revascularization, and past aspirin use. All CVRFs were obtained by history taking and clinical examination on admission.
Definitions of Risk Factors
Traditional Risk Factors. DM, hypertension, and dyslipidemia were defined when patients were known to have the given risk factors prior to the index admission and were already were on treatment. Obesity was defined when patients had a body mass index 30 kg/m2. Smoking was defined as regularly smoking 1cigarette daily or stopping smoking only within the past 12 months. Family history of CAD was defined as any direct blood relatives (parents, siblings, and children) who have had any of the following at 55 years or younger: angina, myocardial infarction, or sudden cardiac death without obvious cause.
Potential Risk Factors
Prior revascularization included history of percutaneous coronary intervention or coronary artery bypass grafting before the index admission. CAD risk factor equivalents included peripheral vascular disease and stroke in addition to renal failure.
Cluster of Risk Factors
Risk factors often occur in clusters and may build on one another, and, when grouped together, certain risk factors put patients at an ever greater risk for CAD. For example, metabolic syndrome, a cluster of CVRFs, increases the risk of CAD. Metabolic syndrome was defined in the presence of at least three of the following abnormalities: abdominal obesity (waist circumference: 85 cm in men or 90 cm in women); hypertriglyceridemia; a serum triglyceride concentration 150 mg/dL; low high‐density lipoprotein cholesterolemia (serum high‐density lipoprotein cholesterol concentration <40 mg/dL); hypertension; systolic blood pressure 130 mm Hg, diastolic blood pressure 85 mm Hg, and/or having received antihypertensive medication; high fasting glucose; and serum glucose concentration should be >/ = 110 mg/dL.12 CRF was included either alone or in association with other traditional or non‐traditional risk factor(s). CRF staging was defined according to the published guidelines on the basis of estimated glomerular filtration rate.11
Nontraditional Risk Factors
Nontraditional risk factors not measured in the current study were high‐sensitivity C‐reactive protein, ankle‐brachial index, leukocyte count, fasting blood glucose level, periodontal disease, carotid intima media thickness, coronary artery calcification score, homocysteine level, and lipoprotein (a) level.2
Statistical Analysis
Patients' characteristics, CVRFs, and in‐hospital outcomes were analyzed across the types of ACS, age groups, sex, and among the six countries. Continuous data were presented as mean standard deviation as appropriate. Differences in categoric variables between respective comparison groups were analyzed using the chi‐square test. The association between CVRF and adverse hospital outcomes (HF and mortality) were examined using univariate and multivariate logistic regression models. Crude and multivariable adjusted odds ratios (ORs), with accompanying 95% confidence intervals, were reported. All P values were the result of two‐tailed tests, and values <.05 were considered significant. All data analyses were carried out using the Statistical Package for Social Sciences version 14 (SPSS Inc, Chicago, IL). The protocols of this study received ethical approval from the institutional ethical bodies in all participating countries. All patients gave informed consent to process their anonymous data.
Results
The Gulf RACE study recruited 6704 consecutive patients presenting with ACS. Of these patients, 4085 had NSEACS and 2619 had STEMI, with mean age of 56 12 years. Table 1 lists the prevalence of CVRFs among all ACS patients. Compared with patients with STEMI, patients presenting with NSTEACS were more often female, elder, diabetic, hypertensive, dyslipidemic, and obese and more likely to have prior history of CAD and coronary revascularization. STEMI patients were more often smokers and less likely to be taking aspirin prior to the index admission when compared with NSTEACS patients. Figure 1 shows that smokers were younger and less likely to be diabetic, hypertensive, and dyslipidemic compared with nonsmokers. Most of the CVRFs apart from smoking were more prevalent among women compared with men (Figure 2).
Table 1.
Prevalence of Cardiovascular Risk Factors Across the Acute Coronary Syndrome Spectrum
| ACS (n = 6704) | STEMI (n = 2619) | OR (95% CI) | NSTEACS (n = 4085) | P Valuea | |
|---|---|---|---|---|---|
| Age, y | 56+/−12 | 54+/−12 | 1.0 (1.001–1.011) | 57+/−12 | <.001 |
| Diabetes, % | 40 | 32 | 0.93 (0.82–1.05) | 46 | <.001 |
| Hypertension, % | 49 | 33 | 0.54 (0.47–0.61) | 60 | <.001 |
| Dyslipidemia, % | 32 | 18 | 0.65 (0.56–0.75) | 41 | <.001 |
| Smoking, % | 38 | 52 | 1.9 (1.65–2.12) | 29 | <.001 |
| Prior CAD, % | 46 | 26 | 0.37 (0.33–0.43) | 58 | <.001 |
| Past aspirin use, % | 42 | 21 | 0.53 (0.44–0.63) | 55 | <.001 |
| Prior revascularization, % | 16 | 7 | 0.65 (0.53–0.80) | 21 | <.001 |
| Renal insufficiency, %c | 69 | 67 | 1.5 (1.24–1.69) | 70 | .06 |
| Family with CAD, % | 14 | 13 | 0.98 (0.83–1.16) | 14 | .45 |
| Obesity, % | 27 | 21 | 0.85 (0.74–0.97) | 30 | <.001 |
| In‐hospital outcomes, % | |||||
| Heart failure | 16 | 17 | 16 | .09 | |
| Mortality | 4 | 7 | 2 | <.001 |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; NSTEACS, non–ST elevation acute coronary syndrome; OR, odds ratio; STEMI, ST–elevation myocardial infarction.
Comparing STEMI vs NSTEACS.
Male sex.
Mild, moderate, or severe renal insufficiency on admission using estimated glomerular filtration rate.
Figure 1.
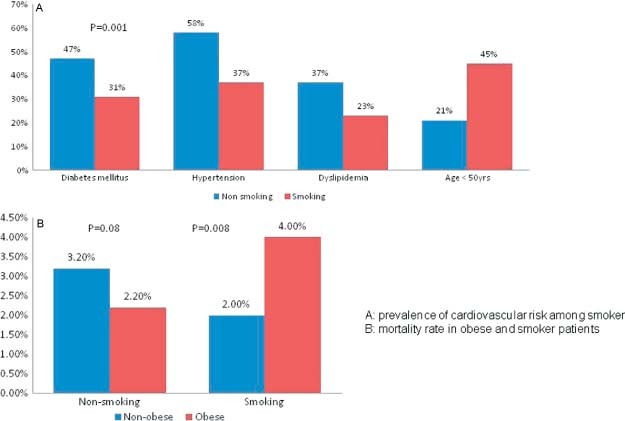
(A) Prevalence of cardiovascular risk factors among smokers. (B) Mortality rate in obese patients and smokers.
Figure 2.
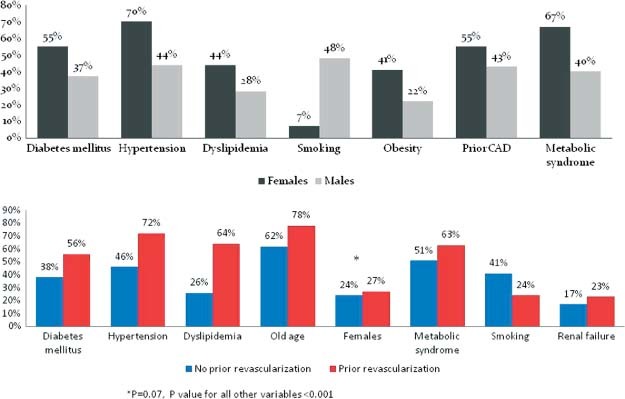
Prevalence of cardiovascular risk factors in men and women and those who had prior coronary revascularization. Abbreviation: CAD, coronary artery disease.
Table 2 summarizes the prevalence of the different CVRFs among the six Gulf countries. Figure 2 shows that patients with prior coronary revascularization were more likely to have greater number of CVRFs compared with patients without prior revascularization.
Table 2.
Prevalence of Cardiovascular Risk Factors in the Six Participating Counties from the Gulf Region
| Oman | United Arab Emirates | Qatar | Bahrain | Kuwait | Yemen | P Value | |
|---|---|---|---|---|---|---|---|
| No. | 1582 | 1335 | 359 | 230 | 2142 | 1054 | |
| Age, mean, y | 59+/−13 | 53+/−12 | 54+/−11 | 58+/−12 | 56+/−13 | 59+/−11 | .001 |
| Diabetes mellitus, % | 37 | 40 | 46 | 51 | 50 | 27 | <.001 |
| Hypertension, % | 53 | 50 | 49 | 60 | 56 | 33 | <.001 |
| Dyslipidemia, % | 35 | 36 | 29 | 45 | 37 | 12 | <.001 |
| Smoking, % | 18 | 49 | 37 | 32 | 40 | 53 | <.001 |
| Chronic renal insufficiency, % | 20 | 14 | 13 | 17 | 16 | 26 | <.001 |
| Obesity, % | 22 | 20 | 23 | 28 | 37 | 22 | <.001 |
| In‐hospital outcomes, % | |||||||
| Heart failure | 25 | 16 | 14 | 9 | 11 | 17 | <.001 |
| Mortality | 4.5 | 2.5 | 2.5 | 2.2 | 2 | 8 | <.001 |
In‐Hospital Outcomes
The overall incidence of HF (16%) was not significantly different across the types of ACS, while the mortality rate was three‐fold higher in STEMI compared with NSTEACS patients (7% vs 2%) (Table 1). HF was more evident among Omani (25%), Yemini (17%), and Emiratis (14%) patients. The mortality rate was higher among Yemeni (8%) and Omani (4.5%) patients compared with other Gulf states (2%–2.5%) (Table 2).
Table 3 demonstrates the prevalence and impact of risk factors among different age groups and stratified by sex. In the young group (<40 years), women were more likely to have DM, hypertension, obesity, metabolic syndrome, and prior history of CAD compared with men. In addition to these CVRFs, dyslipidemia was more prevalent among women in age groups 40 to 59 and 60 years and older. There was no significant difference in the incidence of HF and mortality between women and men up to age 59 years. Compared with men, women had a higher incidence of HF and mortality in the old age group (29% vs 23% and 7.3% vs 5.3%, respectively).
Table 3.
Cardiovascular Risk Factors in Women and Men Across Different Age Groups in Acute Coronary Syndrome Patients
| <40 y (n = 627) | 40–59 y (n = 3437) | 60 y (n = 2633) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Women, % | Men, % | P Value | Women, % | Men, % | P Value | Women, % | Men, % | P Value | |
| Diabetes mellitus | 37 | 17 | .001 | 54 | 37 | .001 | 56 | 42 | .001 |
| Hypertension | 50 | 21 | .001 | 67 | 41 | .001 | 74 | 56 | .001 |
| Dyslipidemia | 21 | 14 | .16 | 41 | 27 | .001 | 47 | 36 | .001 |
| Obesity | 48 | 21 | .001 | 48 | 23 | .001 | 37 | 22 | .001 |
| Smoking | 10 | 67 | .001 | 9 | 55 | .001 | 5 | 30 | .001 |
| Renal failure | 10 | 5 | .11 | 14 | 13 | .66 | 21 | 31 | .001 |
| Family history of coronary artery disease | 19 | 11 | .05 | 14 | 13 | .51 | 12 | 16 | .01 |
| Prior coronary artery disease | 34 | 22 | .02 | 49 | 39 | .001 | 60 | 57 | .10 |
| Prior revascularization | 10 | 7 | .49 | 15 | 13 | .26 | 19 | 21 | .15 |
| Outcomes | |||||||||
| Heart failure | 5 | 6 | .78 | 13 | 11 | .32 | 29 | 23 | .001 |
| Mortality | 1.6 | 0.4 | . 17 | 2.4 | 2.3 | . 95 | 7.3 | 5.3 | .03 |
Table 4 demonstrates the impact of different CVRFs on in‐hospital outcomes. In overall ACS, the mortality rates were significantly higher among elderly women with a history of CAD and patients with a family CAD. CRF was associated with a five‐fold increase in mortality rate compared with those who presented with normal renal function (10% vs 2%). There was a significantly higher mortality rate in the presence of DM, hypertension, dyslipidemia, and prior coronary revascularization in patients presenting with STEMI. Presence of family history of CAD was associated with higher mortality across NSTEACS and STEMI.
Table 4.
In‐Hospital Mortality Stratified by Cardiovascular Risk Factors in the Acute Coronary Syndrome Spectrum
| ACS (n = 6704), % | P Value | NSTACS (n = 4085), % | P Value | STEMI (n = 2619), % | P Value | |
|---|---|---|---|---|---|---|
| Age, y | ||||||
| 50 (n = 2384) | 1.6 | .001 | 1 | .005 | 2 | .001 |
| >50(n = 4313) | 4.5 | 2.1 | 9 | |||
| Sex | ||||||
| Female (n = 1632) | 5.3 | .001 | 2.5 | .02 | 14.7 | .001 |
| Male (n=5071) | 3.2 | 1.5 | 5.2 | |||
| Diabetes mellitus | ||||||
| No (n=3957) | 3.3 | .05 | 1.7 | .34 | 5.3 | .001 |
| Yes (n=2745) | 4.2 | 2.0 | 9.2 | |||
| Hypertension | ||||||
| No (n=3340) | 3.6 | .79 | 1.9 | .73 | 5.2 | .001 |
| Yes (n=3364) | 3.7 | 1.8 | 9.2 | |||
| Dyslipidemia | ||||||
| No (n=4552) | 3.8 | .55 | 2.1 | .16 | 5.7 | .001 |
| Yes (n=2150) | 3.5 | 1.5 | 10.7 | |||
| Smoking | ||||||
| No (n=4157) | 4.1 | .01 | 2.1 | .09 | 8.9 | .001 |
| Yes (n=2547) | 3.0 | 1.3 | 4.4 | |||
| Obesity | ||||||
| No (n=4756) | 2.7 | .91 | 1.3 | .79 | 4.7 | .12 |
| Yes (n=1694) | 2.8 | 1.2 | 6.3 | |||
| Family history of coronary artery disease | ||||||
| No (n=5798) | 3.2 | .001 | 1.6 | .02 | 5.7 | .001 |
| Yes (n=902) | 6.4 | 3 | 12 | |||
| Prior revascularization | ||||||
| No (n=5657) | 3.6 | .25 | 1.7 | .41 | 6 | .001 |
| Yes (n=1049) | 4.3 | 2.2 | 15 | |||
| Prior coronary artery disease | ||||||
| No (n=3636) | 3.2 | .03 | 1.2 | .01 | 5 | .001 |
| Yes (n=3068) | 4.2 | 2.3 | 11 | |||
| Chronic renal insufficiency | ||||||
| No (n=2041) | 2 | .001 | 1.5 | .001 | 4 | .001 |
| Yes (n=4477) | 10 | 5 | 18 |
Stepwise Logistic Regression Analysis
Table 1 shows the multivariate analysis of the different CVRFs to detect predictors of the ACS type. Smoking, CRF, and sex were strongly and independently associated with presenting with STEMI. Figure 3 demonstrates that CRF and DM were independent predictors of in‐hospital HF in NSTE‐ ACS (OR, 2.6; 95% confidence interval [CI], 2.09–3.18 and OR, 1.5; 95% CI, 1.19–1.78, respectively) while CRF (OR, 2.4; 95% CI, 1.88–3.11), hypertension (OR, 1.4; 95% CI, 1.12–1.85), and dyslipidemia (OR, 1.6; 95% CI, 1.25–2.19) were predictors of HF in STEMI. CRF was an independent predictor of mortality in STEMI (OR, 5.0; 95% CI, 3.47–7.73) and NSTEACS (OR, 5.0; 95% CI, 2.81–9.61). Female sex was an independent predictor of mortality in STEMI (OR, 2.0; 95% CI, 1.19–9.13).
Figure 3.
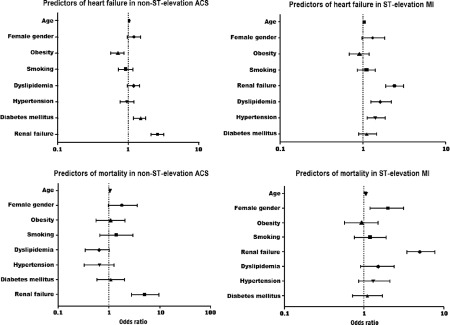
Predictors of heart failure and mortality across acute coronary syndrome (ACS) spectrum. MI indicates myocardial infarction.
Discussion
The current study explores the prevalence of CVRFs in patients presenting with ACS in the Arab Middle East. Moreover, it demonstrates the impact of these risk factors on in‐hospital HF and mortality rates. The key findings of this study include: first, the number and type of CVRF varied across the types of ACS, age groups, and sex. Second, the participating countries have higher prevalence of the CVRF in a unique fashion; however, the frequency and type of CVRF were not identical among these adjacent countries. This diversity may partly relate to the difference in the socioeconomic status, healthcare resources, and number of expatriates in each country. Third, the impact of CVRF on the occurrence of HF and mortality varied according to the type, number, and interaction of CVRFs. CRF emerges asan independent predictors of mortality and HF across ACS spectrum. Moreover, CRF in addition to DM, a traditional risk factor, were the only two CVRFs that independently predicted HF in patients with NSTEACS.
Among the few studies that evaluated the impact of CVRFs in patients presenting with ACS, the present study is the largest.13, 14 In a systematic review, Motlagh and colleagues3 revealed a high prevalence of obesity, DM, hypertension, and smoking in the Middle Eastern region, although there was considerable variation in the reported prevalence of risk factors. The overall prevalence of obesity in the Middle East was comparable with some of the rates reported from several high‐income and Western countries.3, 15, 16 Dietary habits in the Arabian Gulf region have markedly changed in the past few decades, with an increase in per capita energy and fat intake. It is probable that this high intake of fat‐rich foods and calories, in addition to the sedentary lifestyle in this region, played an important role in the rise of obesity and poor cardiovascular outcomes.17, 18
In the present study, DM, hypertension, and dyslipidemia were more prevalent among Bahraini and Kuwaiti patients. The prevalence of hypertension in the Middle East, which Motlagh and colleagues3 reported, was similar to rates observed in North America (28%) but lower than in Europe (44%) and the current study (40%). Overall, hypertension was more prevalent in women than men. The prevalence of smoking was high in the Arab Middle East in men, but it was relatively uncommon in women (48% vs 7%, respectively).
In the present study, there was no mortality difference between obese and non‐obese patients; however, when obesity was added to smoking, it was associated with a significantly greater mortality rate in STEMI patients compared with obese nonsmoking patients (Figure 1).
CVRFs encourage CAD in either sex at all ages but on different levels. Our study demonstrated that female sex was an independent predictor of mortality in patients with STEMI. Family history of CAD is a significant independent risk factor for CAD.19 This factor was evident in 14% of our study population and was associated with a two‐fold increase in mortality compared with those who had no family history of CAD (6.4% vs 3.2%, respectively; P = .001). In a population‐based study from Albania, and after adjustment for covariates, family history of CAD was found to be a strong predictor of ACS in men and women.20 Interestingly, in the present study prior coronary revascularization was associated with higher mortality and this was, in part, explained by the presence of many risk factors among the population with prior revascularization.
CRF alone is an independent risk factor for the development of CAD and is associated with increased mortality after ACS. Moreover, CRF is considered a CAD risk equivalent.10, 21, 22, 23 Previous data show that there is a high prevalence of CHD in CRF patients and that mortality due to CHD is 10 to 30 times higher in dialysis patients than in the general population.21 Most of the traditional CVRFs are highly prevalent in CRF. Other factors (nontraditional risk factors) that are not included in Framingham risk equations may play an important role in promoting CHD in patients with CRF.21 In the present study, CRF and DM were independent predictors of in‐hospital HF in NSTEACS, while CRF and hypertension were the predictors of HF in STEMI. Modifiable risk factors were unchanged in patients with prior MI, as these patients continued to have a higher prevalence of DM, hypertension, and dyslipidemia. In the current study, prior MI was associated with higher HF and mortality rates compared with patients who presented with their first MI (23% vs 14%, P = .001 and 5% vs 3%, P=.002, respectively). The severity and type of CAD disease is highly correlated with CVRF number and type and assumed different characteristics according to clinical presentation.24 In a large study from Europe and the Mediterranean area, presenting with STEMI was strongly associated with smoking but inversely related to obesity and hypertension.25 Prior history of CAD was associated with less ST elevation. In the present study, smoking, CRF, male sex, and old age were strong predictors of STEMI, whereas hypertension, obesity, prior CAD, dyslipidemia, and past aspirin use were predictors of NSTEACS. Therefore, shifts in coronary risk factor pattern may be contributing to a shift in the clinical presentation in ACS.25, 26
Study Limitations
Our data were collected from an observational study, which is a limitation. However, well‐designed observational studies provide valid results and do not systematically overestimate the results compared with the results of randomized controlled trials. Although data from the Gulf region suggested that high prevalence of physical inactivity represents a major public health concern, the current study did not evaluate the effect of physical inactivity and dietary habits in ACS patients.27 The third limitation is that the mean age in our study population was between 55 and 56 years, suggesting possible exclusion of elderly patients. Also, the study did not measure any of the laboratory nontraditional risk factors; however, measuring CV risk factors only by history taking is simpler, cost‐effective, and well studied. Moreover, the US Preventive Services Task Force reported no sufficient evidence to assess the balance of benefits and harms of using the nontraditional risk factors studied to screen asymptomatic men and women with no history of CHD to prevent CV events.2 Many CAD risk factor equivalents, such as peripheral vascular disease and stroke in addition to renal failure, need to be studied in more detail.
Conclusions
Assessment of the prevalence of the traditional CVRF in the acute coronary presentation is cost‐effective and of important prognostic value for in‐hospital morbidity and mortality. CVRF and its impact may differ according to ACS type, age, and sex. Most of the important risk factors for CAD are modifiable and therefore its early identification is vital to set the strategy for prevention. Lastly, not only the traditional CVRFs but also other clinical risk factors should be included in the risk stratification in patients with ACS.
Acknowledgements
We would like to thank all of the staff in all participating centers for their invaluable cooperation. Gulf RACE is a Gulf Heart Association project and was financially supported by Sanofi Aventis and Qatar Telecommunications Company. The sponsors had no role in the study design, data collection, or data analysis. The sponsors had no role in the writing of the report and submission of the manuscript. The study received ethical approval from the institutional ethical bodies in all participating countries. All patients gave informed consent to process their anonymous data. The authors have no conflict of interest to report.
References
- 1. Bener A, Al Suwaidi J, El‐Menyar A, et al. The effect of hypertension as a predictor of risk for congestive heart failure patients over a 10‐year period in a newly developed country. Blood Press. 2004;13:41–46. [DOI] [PubMed] [Google Scholar]
- 2. U.S. Preventive Services Task Force . Using nontraditional risk factors in coronary heart disease risk assessment: U.S. Preventive ServicesTask Force Recommendation Statement. U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:474–482. [DOI] [PubMed] [Google Scholar]
- 3. Motlagh B, O'Donnell M, Yusuf S. Prevalence of cardiovascular risk factors in the Middle East: a systematic review. Eur J Cardiovasc Prev Rehabil. 2009;16(3):268–280. [DOI] [PubMed] [Google Scholar]
- 4. El‐Menyar A, Amin H, Rashdan I, et al. Ankle‐brachial index and extent of atherosclerosis in patients from the Middle East (the AGATHA‐ME study): a cross‐sectional multicenter study. Angiology. 2009;60(3):329–334. [DOI] [PubMed] [Google Scholar]
- 5. Mihalopoulos NL, Berenson GS. Cardiovascular risk factors among internal medicine residents. Prev Cardiol. 2008;11(2):76–81. [DOI] [PubMed] [Google Scholar]
- 6. Yusuf S, Hawken S, Ounpuu S, et al; INTERHEART Study Investigators . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364(9438):937–952. [DOI] [PubMed] [Google Scholar]
- 7. El‐Menyar AA, Albinali HA, Bener A et al. Prevalence and impact of diabetes mellitus in patients with acute myocardial infarction: a 10‐year experience. Angiology. 2009. December–2010 January; 60(6):683–688. [DOI] [PubMed] [Google Scholar]
- 8. Al Suwaidi J, Bener A, Al Binali HA, et al. Mortality caused by acute myocardial infarction in Qatari women. Heart. 2004;90(6):693–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zubaid M, Rashed WA, Almahmeed W, et al. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the gulf registry of acute coronary events (Gulf RACE). Acta Cardiol. 2009;64(4):439–446. [DOI] [PubMed] [Google Scholar]
- 10. El‐Menyar A, Zubaid A, Rashed W, et al. Comparison of men and women with acute coronary syndrome in six Middle Eastern countries. Am J Cardiol. 2009;104(8):1018–1022. [DOI] [PubMed] [Google Scholar]
- 11. El‐Menyar A, Zubaid M, Sulaiman K, et al. In‐hospital major clinical outcomes in patients with chronic renal insufficiency presenting with acute coronary syndrome: data from a registry of 8176 patients. Mayo Clin Proc. 2010;85(4):332–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. [DOI] [PubMed] [Google Scholar]
- 13. Kurtulmus N, Bos S, Arslan S, et al. Differences in risk factors for acute coronary syndromes between men and women. Acta Cardiol. 2007;62(3):251–255. [DOI] [PubMed] [Google Scholar]
- 14. Esteghamati A, Abbasi M, Nakhjavani M, et al. Prevalence of diabetes and other cardiovascular risk factors in an Iranian population with acute coronary syndrome. Cardiovasc Diabetol. July 17 2006;(5):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. [DOI] [PubMed] [Google Scholar]
- 16. Hadi HA, Zubaid M, Al Mahmeed W, et al. The prevalence and outcome of excess body weight among Middle Eastern patients presenting with acute coronary syndrome. Angiology. 2010;61(5):456–464. [DOI] [PubMed] [Google Scholar]
- 17. Musaiger AO. Overweight and obesity in the Eastern Mediterranean region: Can we control it? East Mediterr Health J. November 2004;10(6):789–793. [PubMed] [Google Scholar]
- 18. Kokkinos P, Myers J, Kokkinos JP, et al. Exercise capacity and mortality in African‐American and Caucasian men. Circulation. 2008;117:614–622. [DOI] [PubMed] [Google Scholar]
- 19. Andresdottir MB, Sigurdsson G, Sigvaldason H, et al. Fifteen percent of myocardial infarctions and coronary revascularizations explained by family history unrelated to conventional risk factors. The Reykjavik Cohort Study. Eur Heart J. 2002;23:1655–1663. [DOI] [PubMed] [Google Scholar]
- 20. Burazeri G, Goda A, Sulo G, et al. Conventional risk factors and acute coronary syndrome during a period of socioeconomic transition: population‐based case–control study in Tirana, Albania. Croat Med J. 2007;48(2):225–233. [PMC free article] [PubMed] [Google Scholar]
- 21. Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–2169. [DOI] [PubMed] [Google Scholar]
- 22. Al Suwaidi J, Reddan DN, Williams K, et al. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation. 2002;106(8):974–980. [DOI] [PubMed] [Google Scholar]
- 23. El‐Menyar AA, Al Suwaidi J, Holmes DR Jr. Use of drug‐eluting stents in patients with coronary artery disease and renal insufficiency. Mayo Clin Proc. 2010;85(2):165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cademartiri F, Romano M, Seitun S, et al. Prevalence and characteristics of coronary artery disease in a population with suspected ischemic heart disease using CT coronary angiography: correlations with cardiovascular risk factors and clinical presentation. Radiol Med. 2008;113(3):363–367. [DOI] [PubMed] [Google Scholar]
- 25. Rosengren A, Wallentin L, Simoons M, et al. Cardiovascular risk factors and clinical presentation in acute coronary syndromes. Heart. 2005;91(9):1141–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saab F, Mukherjee D, Gurm H, et al. Risk factors in first presentation acute coronary syndromes (ACS): how do we move from population to individualized risk prediction? Angiology. 2009;60(6):663–667. [DOI] [PubMed] [Google Scholar]
- 27. Al‐Nozha MM, Al‐Hazzaa HM, Arafah MR, et al. Prevalence of physical activity and inactivity among Saudis aged 30–70 years: a population‐based cross‐sectional study. Saudi Med J. 2007;28(4): 559–568. [PubMed] [Google Scholar]


