Abstract
Background:
One disadvantage of current loop recorders is the long interval between recording an electrocardiogram (ECG), establishing a diagnosis, and taking appropriate medical measures. The Cardio R loop recorder transmits cardiac recordings by cellular communication at the push of a button. Users can concomitantly relay symptoms, thereby providing a symptom/cardio‐rhythm correlation.
Hypothesis:
The Cardio R is capable of early detection of cardio‐electrical events that could account for patients' symptoms.
Methods:
This observational study was designed to evaluate patients who were referred from community physicians/cardiologists for evaluation of various cardiac symptoms that were not observed by regular office ECGs or traditional 24‐hour Holter cardiac monitoring. Transmitted recordings were instantly displayed on a monitor for immediate diagnosis by the on‐duty medical team at SHL‐Telemedicine's call center. Abnormal tracings, especially when accompanied by symptoms selected from the prepared list, enabled the staff to instruct the subscriber, notify their physician, and/or dispatch a mobile intensive care unit to the scene.
Results:
Between January 2009 and August 2010, there were 17 622 ECG transmissions received from 604 patients (age range, 10–95 years) who completed a 1‐month trial with the Cardio R device. Palpitation, presyncope, and chest pain were the leading complaints. A disturbance in rhythm that could account for symptoms occurred during recording in 49% cases and was displayed within 7 minutes in 93% of them. No longer than 2 days elapsed from recording onset to diagnosis.
Conclusions:
The Cardio R device enables prompt ECG confirmation/exclusion of a probable arrhythmic cause of symptoms, enabling rapid intervention for cardiac‐relevant complaints. © 2011 Wiley Periodicals, Inc.
Dr. Arie Roth is a medical consultant for SHL‐Telemedicine.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
Conventional loop recorders allow ambulatory recording of cardiac rhythm in patients with suspected arrhythmias that had not occurred within the 24‐hour cardiac monitoring by a Holter recorder. They are especially suitable for undetected sources of a suspected cardiac syncope and/or when cardiac events are infrequent.1, 2 One disadvantage of current loop recorders that could have significant consequences is the time lag between the electrocardiographic (ECG) recording and the provision of appropriate therapeutic management. This delay results from the interval between the actual recording of the cardiac rhythm by the patient while he/she is sensing a cardiac‐related symptom and the interpretation of the ECG recording for establishing the diagnosis by an expert. Any delay is obviously counterproductive to achieving the goal of early detection of a life‐threatening arrhythmia.
The purpose of this paper was to report the accumulated experience of SHL‐Telemedicine with a new loop recording device for the early detection, rapid interpretation, and when indicated, therapeutic management of cardiac electrical events.
Methods
The System and the Technology
SHL‐Telemedicine provides round‐the‐clock medical assistance to its subscribers. The system has been described in detail elsewhere.3, 4, 5, 6, 7, 8 Briefly, it operates through a call center managed by medical staff. Each subscriber's complete medical file (including a full 12‐lead ECG) is stored, as are periodically updated details on numerous clinical parameters. All subscribers carry a cardiobeeper for transmitting a 3‐ or 12‐lead ECG via a regular or cellular telephone line. The Cardio R is a newly designed loop recorder that uses digital cellular technology to record and transmit 3‐lead cardiac recordings by cellular communication at the press of a button (Figure 1). This technology allows instant availability of the recorded rhythm to the highly trained personnel of the call center. They are registered nurses who completed an advanced course on intensive care and/or a special 180‐hour course on interpreting ECG tracings taught by board certified cardiologists. An incoming ECG transmission generates a signal on a dedicated screen, and the on‐call nurse analyzes it for “first glance” confirmation/exclusion of a significant arrhythmia. ECGs that demonstrate the latter are saved for detailed analysis by a more experienced nurse in under several hours. Her interpretation will be reviewed in less than 24 hours by a board certified cardiologist who will certify the final ECG analysis. The call center is manned 24/7, allowing for rapid interpretation of the 3‐lead tracing and provision of appropriate interventions in cases of life‐threatening arrhythmias.
Figure 1.
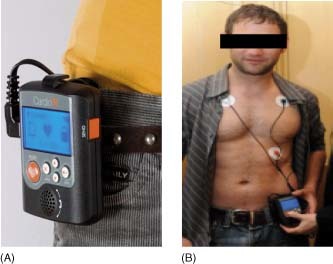
(A) The Cardio R cellular enhanced loop recorder. (B) Placement of electrodes and push‐button activation of the device.
The Cardio R loop recorder has a 90‐minute storage of the 3 leads. The patients were wired to the continuously recording device for whenever they chose within 1 month. They were instructed to push the recording button whenever they sensed what they believed to be a cardiac symptom and save the 2‐minute recording prior to and the 1‐minute recording following symptom occurrence. They could also select and transmit a description of the symptoms from a list of key words programmed within the device, such as palpitations, chest pain, and dizziness. The users could also receive messages that were displayed on the device's screen (eg, contact your doctor).
Patient Recruitment and Protocol for Device Use
Community physicians and cardiologists were informed of this observational study through flyers inviting their participation. The patients in the current study group were referred by them for monitoring to evaluate various cardiac symptoms that were not depicted by office ECGs or by 24‐hour Holter cardiac monitoring. The referring physicians were asked to complete a questionnaire on the patient's relevant demographic details and the reason(s) for referral, and which steps the monitor center was to take if the recording indicated any event of tachyarrhythmia (ventricular or tachycardia >140 bpm) or bradyarrhythmia (<40 bpm). Upon enrolling their patients into the program, the physicians received a code that accesses them to those patients' transmissions on the Internet. They also instructed the call center on the procedures to be followed for reporting to them the occurrence of an arrhythmia or any other specified symptom that their patients had transmitted. Based on well‐established protocols, computerized algorithms, and clinical judgment, the on‐call staff was prepared to directly contact the patient to provide advice on immediate treatment (ie, taking a tranquilizer), or to dispatch a mobile intensive care unit (MICU) staffed by a physician and a paramedic/driver to wherever the patient was located. False alarms or benign arrhythmias (eg, atrial premature contractions) would, of course, not justify contacting the patient at once. Nevertheless, because reassurance to confirm or rule out a meaningful arrhythmia was 1 of the primary reasons the patients received the device in the first place, they were notified that there had not been any cardiac event to cause alarm after 1 month of device use. The detailed interpretation of the transmitted ECG by trained personnel, with confirmation by an on‐call physician or cardiologist, was available within 24 hours. Referring physicians were able to follow a real‐time ECG “diary” by connecting to a password‐protected Internet site and could receive a CD with information relevant to the contact, the ECG tracing, and the details of the management of the event (cardiac or otherwise).
Data Collection
The data on selected parameters recorded for all consecutive patients who completed a 1‐month period of evaluation using the new loop recorder during the study period were analyzed. They are reported as percentage and actual number of patients, and presented as mean ± 1 standard deviation where appropriate.
Results
During the 20‐month study period (January 2009–August 2010), 604 patients were referred for monitoring and each completed the 1‐month follow‐up. Their mean age was 57 ± 19 years (range, 10–95 years), and 61% were females. The reason for referral was: palpitations (n = 418), episodes of presyncope (n = 161), and complaints of chest pain (n = 25). There were a total of 17 622 ECG transmissions of 18 698 events (some transmissions included more than 1 event of cardiac‐related symptoms, and some callers had more than 1 complaint). Each patient sent 29 ± 57 transmissions during the period of monitoring, but not all were motivated by the reason for which they were referred for monitoring (Table 1). There was a 2 ± 7‐day interval between affixing the Cardio R loop recorder and the transmission of the first symptomatic episode.
Table 1.
Selected Parameters of the 604 Study Patients
| Variable | Palpitations (418 Patients; 12 295 Transmissions) | Presyncope (161 patients; 4510 Transmissions) | Chest Pain (25 patients; 817 Transmissions) | Total (604 Patients; 17 622 Transmissions) |
|---|---|---|---|---|
| Age (mean ± 1 SD), y | 56 ± 18 | 59 ± 20 | 56 ± 22 | 57 ± 19 |
| Male gender, % | 36 | 74 | 40 | 39 |
| Average transmissions/patient | 29 ± 57 | 28 ± 58 | 33 ± 55 | 29 ± 57 |
| Notifications to physician, n (%) | 41 (0.33) | 45 (0.9) | 5 (0.61) | 91 (0.51) |
| MICU dispatches, n (%) | 11 (0.11) | 8 (0.17) | 0 | 22 (0.12) |
| Advice given to caller, n (%) | 128 (1.04) | 71 (1.57) | 14 (1.71) | 213 (1.21) |
| Relevant complaint,a n/total (%) | 7754/12 295 (63) | 436/4510 (10) | 438/817 (54) | 8628/17 622 (49) |
| Diagnostic real‐time ECG, n (% of relevant complaintsa) | 7443/7754 (96) | 253/436 (58) | 302/438 (69) | 7998/8628 (93) |
| Delay until transmission of 1st symptomatic episode, days | 2 ± 6 | 3 ± 8 | 1 ± 3 | 2 ± 7 |
Abbreviations: ECG, electrocardiogram; MICU, mobile intensive care unit, SD, standard deviation.
Relevant complaint refers to the complaint for which the patient was referred.
The median time between the transmission of a cardiac rhythm to the first viewing by the monitoring center's team was 7 minutes. The median time until the more detailed ECG interpretation by the trained staff was 5 hours, and the final interpretation and confirmation or refinement of the ECG interpretation by a qualified physician took place at a median of 16 hours from transmission.
The breakdown of demographics, number of transmission, and measures taken for the 604 patients according to the specific reasons for referral given by the referring physician are presented in the Table. Almost 2% of all the cardiac rhythm transmissions (n = 326) required instant medical attention, and 213 transmissions (1.21%) resulted in notifying the patient of the appropriate measures to take or instructions to be followed according to individual arrangements between the call center and the participating physician.
In 7754 (63%) of the 12 295 calls from patients referred for palpitations, the patients did in fact complain of palpitations, and the following ECG tracings that were associated with their complaints were recorded: atrial tachyarrhythmias (mostly multiple atrial premature contractions and atrial fibrillation with a heart rate >100 bpm) in 45% of the transmissions, ventricular arrhythmias consisting mostly of multiple ventricular premature complexes and repeated bouts of nonsustained ventricular tachycardia, accelerated idioventricular rhythm or normal transitions between pacemaker activity and spontaneous heart rate in 22%, sinus tachycardia (heart rate >100 bpm) in 31%, and sinus bradycardia in the remaining 2%. In 438 (54%) of the 817 calls from patients referred for chest pain, the patients did in fact complain of chest discomfort, and the following ECG tracings that were associated with complaints of chest pain were recorded: atrial tachyarrhythmias (mostly atrial fibrillation with a heart rate >100 beats/min) in 32% of the transmissions, ventricular arrhythmias consisting mostly of multiple ventricular premature complexes and repeated bouts of nonsustained ventricular tachycardia or accelerated idioventricular rhythm in 6%, and sinus tachycardia (heart rate >100 bpm) in 62%.
In contrast, only 436 (10%) of transmissions of the 4510 made by patients whose reason for referral was presyncope were done for lightheadedness/dizziness, and they were associated with the following complaints: atrial tachyarrhythmias (mostly atrial fibrillation with a heart rate >100 bpm) in 26% of the transmissions, ventricular arrhythmias consisting of events of nonsustained ventricular tachycardia in 21%, and bradyarrhythmias (including sinus arrhythmias or various degrees of atrioventricular blocks) in 53%. The Table also specifies the number of times the referring physician was informed about the event. Noteworthy, an MICU was dispatched in 22 cases of patients with arrhythmias who were judged as being at high risk (Figures 2 and 3).
Figure 2.
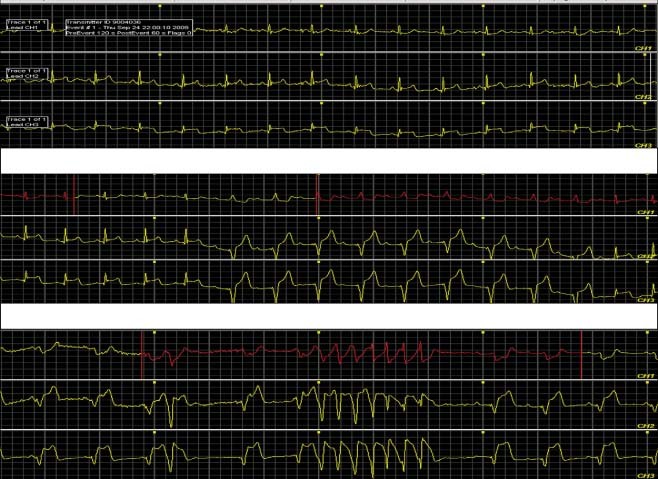
Consecutive recordings from a 64‐year‐old female who complained of chest pain, palpitations, and dizziness and for whom the aim of monitoring was to determine the order in which those symptoms appeared.
Figure 3.
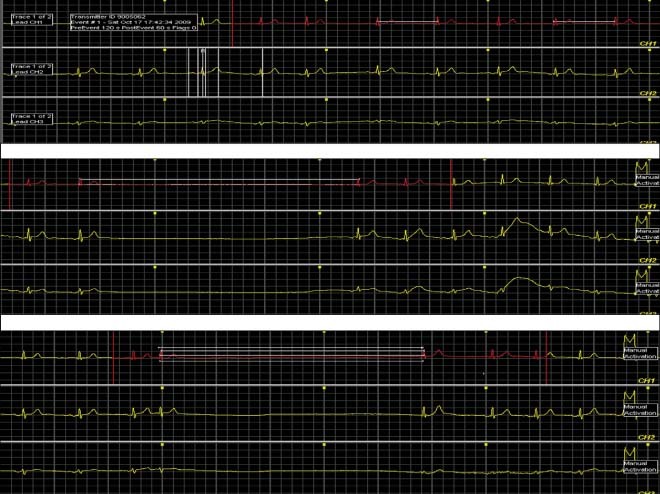
Consecutive recordings from a 76‐year‐old male with no neurological findings who was referred for monitoring because of 2 years of recurrent symptoms of presyncope. Pauses lasting 3 seconds each had been recorded on a Holter recording 2 weeks earlier.
Discussion
The objective of this study was to observe whether a new loop recorder could meaningfully shorten the time between performing an ECG recording of a suspected pathological cardiac rhythm, interpretation of the tracing, and provision of appropriate therapeutic management in symptomatic patients in the setting of a telemedicine system. This process could ordinarily take 1 week or longer for most cases compared to an average delay of only 3 days from the time the patient attached the Cardio R loop recorder to the appearance of the first symptom for which he/she initiated transmission. The first observation of the recorded rhythm took place within minutes of its being transmitted, the expert interpretation took a matter of hours, and the implementation of the established protocol for responding to the ECG findings was immediate. The longest gap was <12 hours.
Diagnosis of cardiac‐originated symptoms is challenging when a suspected arrhythmia or any other cardiac symptom is self‐limiting or occurs intermittently. Exclusion of arrhythmias as being responsible for symptoms is also critical for effective patient care, and commercially available means to measure and record them range from standard ECG units to surgically implanted devices. The office ECG is frequently normal because of being recorded in‐between events. A Holter monitor continuously records ECGs and provides 24 to 48 hours of full disclosure of heart rate, arrhythmia counts, and burden, but symptoms must occur during the limited time the monitor is operative, and consequently it rarely identifies relevant symptom‐related arrhythmias in patients with syncope.9 Event monitors that record for longer periods of time, mostly loop recorders, are used to overcome this obstacle. The patients activate the recording button only when they feel a symptom(s). If the recorded event is transmitted telephonically, the patients are required to dial the number of the call center, play back the event, and then erase that segment to reset the monitor for the next recording. Most models have a memory capacity of 6 minutes. Disadvantages of these devices include the delay in documenting symptoms from the moment of being aware of them until placement of the monitor to pushing the recording button, and the patient must have the presence of mind to correctly transmit the ECG. Finally, recordings with this model usually consist of only a 1‐lead ECG rhythm strip.
Event recorders have a looping memory, and pushing the buttons for describing symptoms captures 45 seconds of prememory and 15 seconds of the postsymptom ECG. One lead is routinely transmitted, but 2 leads are also optional. Loop recorders with 6 to 10 minutes of memory may record 1 to 6 events. They were shown to have a higher diagnostic yield than Holter monitors for patients with presyncope or syncope.10
Auto‐trigger event monitors comprise another tool for patients with infrequent symptoms, such as those suggestive of or being treated for paroxysmal atrial fibrillation (AF). They have a programmable memory of 10 to 20 minutes, and the patient must maintain enough calm to follow the required steps for transmitting the recorded events. Only 1 to 2 leads can be transmitted, and so some arrhythmic events are not well traced, whereas false negatives may occupy an appreciable amount of the low‐capacity storage memory, and artifacts may cause inappropriate algorithm triggering.
Outpatient telemetry is designed to be used at home for post‐coronary artery bypass grafting, AF, or drug management in patients with infrequent symptoms. An algorithm is installed in a home computer connected to a phone line, and the patient wears a module connected to the skin by electrodes. A major advantage is that ECG signals are transmitted through the computer automatically via the phone line to provide beat‐by‐beat analysis, 24 hours of stored ECG data, trends in heart rate, and the physician's daily reports. A disadvantage is that the patient must be homebound: monitoring a patient remote from a computer tower and without cellular telephone capabilities is impossible.
The auto‐activated Mobile Cardiac Outpatient Telemetry (MCOT) allows constant communication between the device carried by the patient and an in‐home base, or by cellular technology when away.11 Although patients cannot transmit a symptomatic cardiac rhythm, reporting consists of daily accounts and urgent information based on the physician's preset notification criteria.
The implantable loop recorder is surgically implanted (typically for up to 2 years) to detect and monitor cardiac arrhythmias. It is especially suitable when palpitations or syncope events are infrequent12 and when conventional noninvasive testing is negative or inconclusive. Its main advantage is the length of monitoring time. It provides a good symptom‐to‐rhythm correlation in cases of syncope and palpitations,13 because it can be interrogated even after the patient loses consciousness. The device has 21 to 42 minutes of memory, and events are downloaded via a pacemaker programmer. Disadvantages include the lack of remote transmission capabilities and the possibility of false positive results due to over/undersensing.
This study was not designed to assess the rate of diagnosis or the cost‐effectiveness of one modality over another. We focused solely on the parameters of time‐to‐diagnosis and time‐to‐treatment. The results of this observational study on a new loop monitor (Cardio R) integrated into a telemedicine system showed several advantages over other methods in current use. First, it significantly shortened the interval between the patient's sensing a cardiac‐related symptom and the interpretation of the almost real‐time ECG, allowing speedier application of appropriate therapeutic management. Second, it improved symptom‐rhythm correlation by allowing the patient to transmit the nature of the symptom(s) together with the ECG tracing, thus providing additional data on the cause of various cardiac symptoms (eg, changes in the ST segment during chest pain). Finally, it also allows clear‐cut exclusion of a cardiac origin of recurrent symptoms when no ECG abnormalities are evident.
Conclusion
We described a new loop recorder (Cardio R) device in the setting of a telemedicine system. This combination enabled prompt ECG interpretations and timely interventions for several different cardiac‐relevant complaints. It considerably shortened the lag time between the event, diagnosis, and treatment. It provided better symptom‐arrhythmia correlation by enabling the patient to report the symptom simultaneously with ECG transmission. Randomized prospective trials are needed to compare the Cardio R to other ambulatory monitoring systems to better determine its relative clinical utility and cost‐effectiveness.
Acknowledgements
Esther Eshkol is thanked for editorial assistance.
References
- 1. Brignole M, Alboni P, Benditt DG, et al. Task Force on Syncope, European Society of Cardiology: Guidelines on management (diagnosis and treatment) of syncope‐update 2004. Europace. 2004;6:467–537. [DOI] [PubMed] [Google Scholar]
- 2. Kabra R, Gopinathannair R, Sandesara C, et al. The dual role of implantable loop recorder in patients with potentially arrhythmic symptoms: a retrospective single‐center study. Pacing Clin Electrophysiol. 2009;32:908–912. [DOI] [PubMed] [Google Scholar]
- 3. Roth A, Herling M, Vishlitzki V. The impact of ‘Shahal’(a new cardiac emergency service) on subscribers'requests for medical assistance: characteristics and distribution of calls. Eur Heart J. 1995;16:129–133. [DOI] [PubMed] [Google Scholar]
- 4. Roth A, Bloch Y, Villa Y, et al. The CB‐12L: a new device for transtelephonic transmission of a 12‐lead electrocardiogram. Pacing Clin Electrophysiol. 1997;20:2243–2247. [DOI] [PubMed] [Google Scholar]
- 5. Viskin S, Golovner M, Malov N, et al. Circadian variation of symptomatic paroxysmal atrial fibrillation. Data from almost 10,000 episodes. Eur Heart J. 1999;20:1429–1434. [DOI] [PubMed] [Google Scholar]
- 6. Roth A, Elkayam I, Shapira I, et al. Effectiveness of pre‐hospital synchronous direct‐current cardioversion for supraventricular tachyarrhythmias causing unstable hemodynamic states. Am J Cardiol. 2003;91:489–491. [DOI] [PubMed] [Google Scholar]
- 7. Roth A, Rogowski O, Yanay Y, et al. Teleconsultation for cardiac patients: a comparison between nurses and physicians: the SHL experience in Israel. Telemed J E Health. 2006;12:528–534. [DOI] [PubMed] [Google Scholar]
- 8. Birati EY, Malov N, Kogan Y, et al. Vigilance, awareness and a phone line: 20 years of expediting CPR for enhancing survival after out‐of‐hospital cardiac arrest. The ‘SHL’‐Telemedicine experience in Israel. Resuscitation. 2008;79:438–443. [DOI] [PubMed] [Google Scholar]
- 9. Gibson TC, Heitzman MR. Diagnostic efficacy of 24 hour electrocardiographic testing for syncope. Am J Cardiol. 1984;53: 1013–1017. [DOI] [PubMed] [Google Scholar]
- 10. Sivakumaran S, Krahn AD, Klein GJ, et al. A prospective randomized comparison of loop recorders versus Holter monitors in patients with syncope or presyncope. Am J Med. 2003;115: 1–5. [DOI] [PubMed] [Google Scholar]
- 11. Brignole M, Vardas P, Hoffman E, et al. Indications for the use of diagnostic implantable and external ECG loop recorders. Europace. 2009;11:671–687. [DOI] [PubMed] [Google Scholar]
- 12. Krahn AD, Klein GJ, Skanes AC, et al. Insertable loop recorder use for detection of intermittent arrhythmias. Pacing Clin Electrophysiol. 2004;27:657–664. [DOI] [PubMed] [Google Scholar]
- 13. Ng E, Stafford PJ, Ng GA. Arrhythmia detection by patient and auto‐activation in implantable loop recorders. J Interv Card Electrophysiol. 2004;10:147–152. [DOI] [PubMed] [Google Scholar]


