Abstract
Background:
There is a paucity of data on the outcome of contemporary percutaneous coronary intervention (PCI) in the elderly. Accordingly, we assessed the impact of age on outcome of a large cohort of patients undergoing PCI in a regional collaborative registry.
Hypothesis:
Increasing age is associated with a higher incidence of procedural‐related complications.
Methods:
We evaluated the outcome of 152373 patients who underwent PCI from 2003 to 2008 in the 31 hospitals participating in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. The procedural outcomes of the cohort were compared by dividing patients into <70 years of age, 70 to 79 years, 80 to 84 years, 85 to 89 years, and ≥90 years.
Results:
Of the cohort, 64.64% were <70 years of age, 23.83% were 70 to 79 years, 7.85% were 80 to 84 years, 3.09% were 85 to 89 years, and 0.58% were 90 years or older. Increasing age was associated with an increase in all‐cause in‐hospital mortality, contrast‐induced nephropathy, transfusion, stroke/transient ischemic attack, and vascular complications. The overall in‐hospital mortality rate was 1.09% and increased from 0.67% in those younger than 70 years up to 5.44% in those 90 years old or greater. The mortality rate in patients over 80 years approached 12% to 15% for those with ST‐segment myocardial infarction and 39% in cardiogenic shock patients.
Conclusions:
The proportion of elderly patients referred for PCI is increasing. Procedural complications increase with age, and patients presenting with unstable symptoms are at the highest risk. © 2011 Wiley Periodicals, Inc.
This work was supported by Blue Cross Blue Shield of Michigan. The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
The elderly are the most rapidly growing segment of the population in the western world.1, 2 Coronary artery disease prevalence rises with age, and coronary revascularization is commonly performed in elderly patients for treatment.3 Prior studies have demonstrated a 2‐ to 4‐fold higher risk of mortality and major complications in elderly patients undergoing percutaneous coronary interventions (PCI).4 Most of these studies are almost a decade old and may not reflect contemporary outcomes. Advances in technology, optimization of pharmacotherapy, and better risk stratification are associated with a decline in procedural complications over the past decade.
There is a paucity of data on outcome of contemporary PCI in the elderly. Accordingly, we assessed the impact of age on outcome of a large cohort of patients undergoing PCI in a regional collaborative registry.
Methods
The study cohort included patients undergoing PCI between 2003 and 2008 in a regional PCI registry. The details of the Blue Cross Blue Shield of Michigan Cardiovascular Consortium registry and the data collection process have been described elsewhere.5, 6, 7, 8, 9 Briefly, procedural data on all patients undergoing PCI at the 31 participating hospitals were collected using standardized collection forms. Baseline data included clinical, demographic, procedural, and angiographic characteristics; as well as medications used before, during, and after the procedure; and in‐hospital outcome. All data elements had been prospectively defined and the local institutional review board approved the protocol. A dedicated staff member collected the data and forwarded it to the coordinating center. Medical records of all patients undergoing coronary artery bypass grafting (CABG), and of patients who died in the hospital were reviewed by auditors from the coordinating center to ensure accuracy. A further 2% of cases were randomly selected for audit. All procedures were performed using standard coronary intervention techniques. The choice of medications as well as equipment was at the discretion of the operating physician.
Procedural outcomes of the cohort were compared by dividing patients into <70 years of age, 70 to 79 years, 80 to 84 years, 85 to 89 years, and ≥90 years. The primary endpoint was in‐hospital death. Other endpoints included postprocedure transfusion, contrast‐induced nephropathy, stroke/transient ischemic attack (TIA), and vascular complications. In‐hospital death was defined as death from either cardiac or noncardiac cause. Blood transfusion was defined as any transfusion of product regardless of the number of units transfused. Vascular complication was defined as: pseudoaneurysm, arteriovenous fistula, femoral neuropathy, retroperitoneal hematoma, access site hematoma requiring transfusion/prolonged hospital stay or causing a drop in hemoglobin >3.0 gm/dL, or any access site complication requiring surgical repair. Because the risk of complications is influenced by procedural indications, we evaluated complications by key indications: cardiogenic shock, primary PCI for ST‐segment myocardial infarction (STEMI), and stable PCI. Stable patients were defined as those requiring nonurgent PCI, and excluded patients with presenting cardiogenic shock or cardiac arrest, those with a myocardial infarction (MI) within the preceding 7 days, and those who received intravenous heparin or nitrates, low‐molecular weight heparin, or a GP IIbIIIa inhibitor before the procedure.
Statistical Analysis
Continuous variables were expressed as mean ± standard deviation, and discrete variables were expressed as frequency counts and percentages. The difference in variable frequency between groups was evaluated by the Mantel‐Haenszel χ 2 test. Trends over age groups were evaluated by the Cochran‐Armitage test.
Results
Baseline Demographics
The baseline demographics of the 152373 patients are listed in the Table 1. Of the total cohort, 64.64% were <70 years of age, 23.83% were 70 to 79 years, 7.85% were 80 to 84 years, 3.09% were 85 to 89 years, and 0.58% were 90 years or greater. The proportion of patients in each age group remained stable throughout the study period. Stable patients accounted for 63876 patients, whereas 20220 underwent PCI for STEMI. Older patients were more likely to be female, lean (body mass index <25), and nonsmokers. Older patients were also more likely to suffer from medical comorbidities, but less likely to have diabetes, renal failure with dialysis, or to have sustained a previous cardiac arrest. There was no difference among the groups in having a prior PCI.
Table 1.
Baseline Demographics and Clinical Variables
| <70 | 70–79 | 80–84 | 85–89 | 90+ | Trend P | |
|---|---|---|---|---|---|---|
| N = 98500 | N = 36318 | N = 11966 | N = 4707 | N = 882 | ||
| Demographic | % | % | % | % | % | |
| Female | 28.83 | 41.64 | 47.97 | 53.28 | 58.62 | <0.0001 |
| Current smoking | 36.02 | 10.96 | 5.16 | 3.02 | 3.06 | <0.001 |
| Lean, BMI <25 | 14.3 | 21.82 | 33.5 | 43.54 | 53.33 | <0.0001 |
| Obese, BMI >30 | 52.17 | 38.45 | 25.09 | 17.32 | 12.86 | <0.0001 |
| Overweight, BMI 25–30 | 33.56 | 39.75 | 41.49 | 39.2 | 33.93 | <0.0001 |
| Historical | ||||||
| Hypertension | 78.27 | 86.75 | 88.52 | 88.95 | 87.76 | <0.0001 |
| MI | 33.99 | 35.97 | 36.18 | 37.01 | 37.87 | <0.0001 |
| Diabetes | 34.41 | 37.22 | 32 | 25.98 | 22.79 | <0.0001 |
| CHF | 10.69 | 18.59 | 23.59 | 27.62 | 30.95 | <0.0001 |
| Extracardiac vascular disease | 19.24 | 33.23 | 38.17 | 39.71 | 36.39 | <0.0001 |
| Renal failure w/dialysis | 2.04 | 2.03 | 1.86 | 1.1 | 0.57 | <0.0001 |
| Significant valve disease | 2.7 | 6.12 | 9.01 | 10.43 | 12.13 | <0.0001 |
| GI bleeding | 1.43 | 2.65 | 3.54 | 3.55 | 4.08 | <0.0001 |
| AFib | 5.36 | 14.57 | 19.71 | 23.18 | 22 | <0.0001 |
| Cardiac arrest | 1.35 | 1.23 | 1.06 | 1.27 | 0.45 | 0.002 |
| Prior PCI | 42.63 | 44.42 | 43.28 | 42.07 | 39.57 | 0.08 |
| CABG | 15.88 | 27 | 26.75 | 22.31 | 15.42 | <0.0001 |
| COPD | 16.78 | 21.49 | 20.09 | 19.38 | 15.76 | <0.0001 |
| Laboratory | ||||||
| Baseline Hgb, mean, g/dL (SD) | 13.9 (1.83) | 13.1 (1.79) | 12.6 (1.84) | 12.3 (1.70) | 12.1 (1.63) | <0.0001 |
| WHO anemia | 22.32 | 36 | 46.04 | 52.33 | 54.99 | <0.0001 |
| Baseline Cr, mean, mg/dL (SD) | 1.16 (1.05) | 1.24 (1.01) | 1.27 (1.19) | 1.27 (0.63) | 1.26 (0.42) | <0.0001 |
| Baseline Cr >1.5, mg/dL | 8.36 | 15.78 | 20.67 | 23.28 | 24.72 | <0.0001 |
| EF, mean (SD) | 52.0 (11.5) | 51.4 (12.2) | 49.7 (12.7) | 48.7 (12.8) | 47.6 (13.1) | <0.0001 |
| EF <50% | 28.31 | 31.54 | 39.02 | 43.85 | 46.49 | <0.0001 |
Abbreviations: AFib, atrial fibrillation; BMI, body mass index; CABG, coronary artery bypass grafting; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; Cr, creatinine; EF, ejection fraction; GI, gastrointestinal; Hgb, hemoglobin; MI, myocardial infarction; PCI, percutaneous coronary intervention; SD, standard deviation; WHO, World Health Organization.
Clinical Outcomes
All‐cause in‐hospital mortality rate was 1.09% and increased with age (P<0.0001). The overall mortality for PCI was 0.67% in those younger than 70 years, 1.43% in those 70 to 79 years, and increased to 5.44% in those 90 years or greater (Figure 1). Increasing age was also associated with higher rates of contrast‐induced nephropathy, transfusion, stroke/TIA, and vascular complications in all cases. In the cohort of patients, emergency coronary surgery was required in 565 (0.37%) patients. The rate of unplanned or emergency CABG was not related to age and occurred in 379 (0.38%) patients younger than 70 years, 124 (0.37%) patients 70 to 79 years, 43 (0.36%) patients 80 to 84 years, 14 (0.30%) patients 85 to 89 years, and 5 (0.57%) patients 90 years or greater (trend, P = 0.38). The overall rate of contrast‐induced nephropathy was 2.83% and as high as 9.33% in those 90 years or older (Figure 2). Transfusion was required in 4.96% of all patients in the study, with 3.54% in those younger than 70 years and increasing to 14.2% in those 90 years or greater (Figure 3). The rate of stroke/TIA increased from 0.23% in patients younger than 70 years, up to 0.91% in patients 90 years or greater (Figure 4). Increasing age was also associated with a higher rate of vascular complications. The overall rate of vascular complications in the cohort was 2.43% and increased from 2.05% in patients younger than 70 years, up to 4.08% in patients 90 years or greater (Figure 5).
Figure 1.
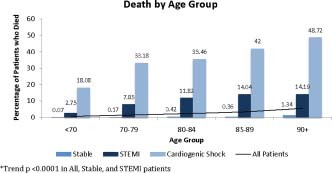
Death by age group. Abbreviation: STEMI, ST‐segment myocardial infarction.
Figure 2.
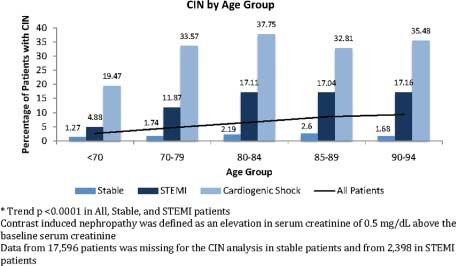
Contrast‐induced nephropathy (CIN) by age group. Abbreviation: STEMI, ST‐segment myocardial infarction.
Figure 3.
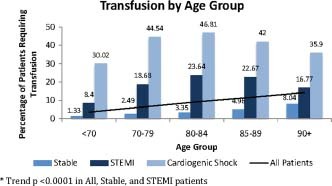
Transfusion by age group. Abbreviation: STEMI, ST‐segment myocardial infarction.
Figure 4.
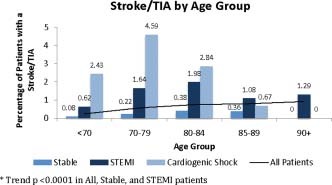
Stroke/transient ischemic attack (TIA) by age group. Abbreviation: STEMI, ST‐segment myocardial infarction.
Figure 5.
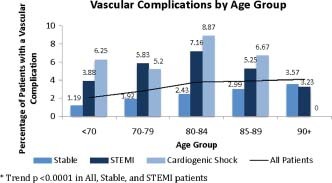
Vascular complications by age group. Abbreviation: STEMI, ST‐segment myocardial infarction.
Subgroup analysis of stable patients and patients with a STEMI demonstrated that increasing age was associated with higher rates of death, contrast‐induced nephropathy, transfusion, stroke/TIA, and vascular complications in both subgroups (Figures 1, 2, 3, 4, 5). In stable patients, the mortality rate increased from 0.07% in patients younger than 70 years to 1.34% in patients 90 years or greater, P < 0.0001 (Figure 1). Rates of contrast‐induced nephropathy, transfusion, stroke/TIA, and vascular complications in stable patients followed similar trends, P<0.0001 in all cases (Figures 2, 3, 4, 5). The overall mortality rate in STEMI patients was 4.50; with 2.75% in those younger than 70 years, 7.85% in those 70 to 79 yeras, 11.82% in those 80 to 84 years, 14.04% in those 85 to 89 years, and 14.19% in those 90 years or older (trend, P < 0.0001 [Figure 1]). Contrast‐induced nephropathy rates increased from 4.88% in patients younger than 70 years to 17.16% in 90 year olds or greater (trend, P < 0.0001 [Figure 2]). Transfusion rates, stroke/TIA rates, and vascular complication rates also followed similar trends (trend, P < 0.0001 in both cases [Figures 3, 4, 5]).
As expected, complication rates in patients presenting with cardiogenic shock was much higher than those without, with the mortality rate increasing from 33% in patients 70 to 79 years of age, with shock to nearly 50% in those 90 years old or greater (Figures 1, 2, 3, 4, 5).
Discussion
The elderly account for a large proportion of patients undergoing PCI. This population has been shown to have an increased incidence of PCI‐related complications. The present study supports these findings and demonstrates that the procedure can be performed with a reasonable degree of safety with relatively low associated morbidity and mortality in stable patients. However, the rate of complications increases in high‐risk groups. The current study offers a contemporary view of current practice and complication rates with patients having been treated from 2003 to 2008, and to our knowledge, includes the 3rd largest cohort of patients undergoing PCI over 80.10, 11
Poor outcomes among the elderly undergoing PCI were recognized in the early days of angioplasty. Studies prior to the development of intracoronary stenting demonstrated a mortality of approximately 8% to 20%,11, 12, 13, 14 with many being single‐center experiences enrolling less than 60 octogenarians.12, 13, 14 With the advent of stenting, mortality decreased.4, 15, 16 Two large multicenter registries examined PCI‐related complications in octogenarians between 1994 and 2000. Batchelor et al evaluated the outcomes of 7472 octogenarians from 1994 to 1997 in the National Cardiovascular Network (NCN) and observed an in‐hospital mortality rate of 3.8%, whereas a 3.77% in‐hospital mortality rate was observed in the 8828 octogenarians in the American College of Cardiology–National Cardiovascular Disease Registry (ACC‐NCDR) from 1998 to 2000.4, 15 Singh et al found an overall mortality of 3.16% in 155612 octogenarians in the NCDR registry from 2001 to 2006, with a temporal decline in mortality during the study period.10 The mortality rate of 2.75% in the 17555 patients 80 years or greater in our study is probably a reflection of the use of PCI in a slightly different population. In the NCN registry, 9.7% of octogenarians were experiencing an acute MI, whereas 68% of cases were elective, and similarly, in the ACC‐NCDR registry, 67.1% of octogenarians had not experienced an MI within the preceding 7 days.4, 15 In the NCDR registry, 65% of octogenarians were experiencing an acute coronary syndrome (34.89% unstable angina, 18.75% non‐STEMI, and 11.35% STEMI).10 In the current study, only 39.2% of the octogenarians were stable, whereas 10.9% were experiencing a STEMI. This may suggest that although we are taking a larger group of unstable/high‐risk octogenarians for cardiac catheterization and intervention, the mortality rates have remained acceptable.
Stroke and contrast‐induced nephropathy following PCI are associated with higher morbidity and mortality.15, 17, 18 Although the rate of stroke increased across all age groups in our study, the rate remained less than 1% for all patients (Figure 4). This is in agreement with previous studies that have documented a risk of 0% to 1.5% risk of stroke following PCI.10, 19, 20, 21, 22, 23, 24 We also found that the rates of contrast‐induced nephropathy increased with age. Given that the elderly inherently have a reduction in renal function, this calls attention to the importance of limiting contrast to elderly patients given the influence of contrast‐induced nephropathy on morbidity and mortality.
Vascular complication rates and need for postprocedure transfusion demonstrated similar trends. Over the past several years, there has been a change in antithrombotic regimens used during and after PCI. However, the rates observed in our study are similar to that of previous findings.4, 15, 19, 20 This may be secondary to the lack of adjustment for differing pharmacokinetics and the in‐ creased risk of vascular injury in elderly patients.
In stable patients, the risk of in‐hospital death did not exceed 1.5% across all age groups. Furthermore, the rates of all complications studied are lower in this group of patients. These low complications need to be balanced in the context of outcomes associated with alternate therapeutic strategies available, including medical therapy and CABG. The benefit of PCI in elderly patients vs medical therapy was evaluated in the Trial of Invasive versus Medical therapy in Elderly patients (TIME) trial, demonstrating that although an invasive approach was associated with procedural risk and no survival benefit, medical management was associated with a 50% chance of subsequent hospitalization and revascularization.25 Further, a meta‐analysis of revascularization strategies in octogenarians demonstrated that the 30‐day mortality for PCI was less than that for CABG (5.4% vs 7.2%, respectively), whereas 1‐year survival was nearly equal (87% in PCI and 86% in CABG).3 Furthermore, given the morbidity associated with CABG, PCI is often preferred by elderly patients. Therefore, based on the results of the current study and prior studies that documented the benefits of PCI vs optimized medical therapy or CABG, age alone should not be a contraindication to the consideration of cardiac catheterization with potential intervention in symptomatic elderly patients. Further research needs to be done to determine if revascularization vs contemporary medical therapy is the appropriate management of asymptomatic ischemia in elderly patients given the findings of Asymptomatic Cardiac Ischemia Pilot Study (ACIP) and Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE).26, 27
In STEMI patients, mortality approached 12% in patients 80 to 84 years old, and nearly 15% in patients age 85 years and greater (Figure 1). This is similar to the outcomes of PCI in octogenarians in the ACC‐NCDR, where the mortality rate was nearly 14% in those who presented with an acute MI within 24 hours, and less than the 27% observed in‐hospital mortality in nonagenarians in a retrospective analysis.15, 28 Despite the high mortality rate observed in this patient group, it is much less than those patients treated medically for STEMI or cardiogenic shock.29 Although in our registry, the STEMI and cardiogenic shock populations had the highest rate of mortality and other procedure‐related complications, we feel that this risk is appropriate given the morbidity and mortality associated with medical therapy alone.
Limitations
The limitations of this study are similar to other multicenter registries in that it offers observational data on nonrandomized patients. In a PCI study of elderly and very elderly patients, there may be a referral bias in that healthier older patients are being referred to PCI. As PCI complications and success are related to operator volume, the study did not analyze the relationship of volume to the rate of complications. Finally, the study does not include patients who received medical or surgical (CABG) therapies.
Conclusion
The proportion of elderly patients referred for PCI is increasing as this segment of the population continues to grow. The complication rates from PCI increase with age, and those with unstable symptoms have worse outcomes. However, we feel these rates are acceptable given higher complication rates with alternative strategies, and patient selection for PCI is important. Therefore, age alone should not be a contraindication to PCI.
Supporting information
Supporting information may be found in the online version of this article
References
- 1. Manton KG, Lowrimore GR, Ullian AD, et al. Labor force participation and human capital increases in an aging population and implications for U.S. research investment. Proc Natl Acad Sci U S A. 2007;104:10802–10807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long‐term changes in function and health in the U.S. elderly population. Proc Natl Acad Sci U S A. 2006;103:18374–18379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McKellar SH, Brown ML, Frye RL, et al. Comparison of coronary revascularization procedures in octogenarians: a systematic review and meta‐analysis. Nat Clin Pract Cardiovasc Med. 2008;5:738–746. [DOI] [PubMed] [Google Scholar]
- 4. Batchelor WB, Anstrom KJ, Muhlbaier LH, et al. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: results in 7,472 octogenarians. National Cardiovascular Network Collaboration. J Am Coll Cardiol. 2000;36:723–730. [DOI] [PubMed] [Google Scholar]
- 5. Kline‐Rogers E, Share D, Bondie D, et al. Development of a multicenter interventional cardiology database: the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) experience. J Interv Cardiol. 2002;15:387–392. [DOI] [PubMed] [Google Scholar]
- 6. Moscucci M, Eagle KA, Share D, et al. Public reporting and case selection for percutaneous coronary interventions: an analysis from two large multicenter percutaneous coronary intervention databases. J Am Coll Cardiol. 2005;45:1759–1765. [DOI] [PubMed] [Google Scholar]
- 7. Moscucci M, Kline‐Rogers E, Share D, et al. Simple bedside additive tool for prediction of in‐hospital mortality after percutaneous coronary interventions. Circulation. 2001;104: 263–268. [DOI] [PubMed] [Google Scholar]
- 8. Moscucci M, O'Connor GT, Ellis SG, et al. Validation of risk adjustment models for in‐hospital percutaneous transluminal coronary angioplasty mortality on an independent data set. J Am Coll Cardiol. 1999;34:692–697. [DOI] [PubMed] [Google Scholar]
- 9. Moscucci M, Rogers EK, Montoye C, et al. Association of a continuous quality improvement initiative with practice and outcome variations of contemporary percutaneous coronary interventions. Circulation. 2006;113:814–822. [DOI] [PubMed] [Google Scholar]
- 10. Singh M, Peterson ED, Roe MT, et al. Trends in the association between age and in‐hospital mortality after percutaneous coronary intervention: National Cardiovascular Data Registry experience. Circ Cardiovasc Interv. 2009;2:20–26. [DOI] [PubMed] [Google Scholar]
- 11. Peterson ED, Jollis JG, Bebchuk JD, et al. Changes in mortality after myocardial revascularization in the elderly. The national Medicare experience. Ann Intern Med. 1994;121: 919–927. [DOI] [PubMed] [Google Scholar]
- 12. Jeroudi MO, Kleiman NS, Minor ST, et al. Percutaneous transluminal coronary angioplasty in octogenarians. Ann Intern Med. 1990;113:423–428. [DOI] [PubMed] [Google Scholar]
- 13. Kern MJ, Deligonul U, Galan K, et al. Percutaneous transluminal coronary angioplasty in octogenarians. Am J Cardiol. 1988;61:457–458. [DOI] [PubMed] [Google Scholar]
- 14. Santana JO, Haft JI, LaMarche NS, et al. Coronary angioplasty in patients eighty years of age or older. Am Heart J. 1992;124: 13–18. [DOI] [PubMed] [Google Scholar]
- 15. Klein LW, Block P, Brindis RG, et al. Percutaneous coronary interventions in octogenarians in the American College of Cardiology‐National Cardiovascular Data Registry: development of a nomogram predictive of in‐hospital mortality. J Am Coll Cardiol. 2002;40:394–402. [DOI] [PubMed] [Google Scholar]
- 16. Parikh R, Chennareddy S, Debari V, et al. Percutaneous coronary interventions in nonagenarians: in‐hospital mortality and outcome at one year follow‐up. Clin Cardiol. 2009;32:E16–E21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fuchs S, Stabile E, Kinnaird TD, et al. Stroke complicating percutaneous coronary interventions: incidence, predictors, and prognostic implications. Circulation. 2002;106:86–91. [DOI] [PubMed] [Google Scholar]
- 18. Marenzi G, Lauri G, Assanelli E, et al. Contrast‐induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004;44:1780–1785. [DOI] [PubMed] [Google Scholar]
- 19. Chauhan MS, Kuntz RE, Ho KL, et al. Coronary artery stenting in the aged. J Am Coll Cardiol. 2001;37:856–862. [DOI] [PubMed] [Google Scholar]
- 20. Yan BP, Gurvitch R, Duffy SJ, et al. An evaluation of octogenarians undergoing percutaneous coronary intervention from the Melbourne Interventional Group Registry. Catheter Cardiovasc Interv. 2007;70:928–936. [DOI] [PubMed] [Google Scholar]
- 21. Teplitsky I, Assali A, Lev E, et al. Results of percutaneous coronary interventions in patients ≥90 years of age. Catheter Cardiovasc Interv. 2007;70:937–943. [DOI] [PubMed] [Google Scholar]
- 22. Ma HY, Zhou YJ, Dick RJ, et al. Long‐term outcome of patients of over 85 years old with acute coronary syndrome undergoing percutaneous coronary stenting: a comparison of bare metal stent and drug eluting stent. Chin Med J (Engl). 2008;121:887–891. [PubMed] [Google Scholar]
- 23. Lefevre T, Morice MC, Eltchaninoff H, et al. One‐month results of coronary stenting in patients ≥75 years of age. Am J Cardiol. 1998;82:17–21. [DOI] [PubMed] [Google Scholar]
- 24. Dynina O, Vakili BA, Slater JN, et al. In‐hospital outcomes of contemporary percutaneous coronary interventions in the very elderly. Catheter Cardiovasc Interv. 2003;58:351–357. [DOI] [PubMed] [Google Scholar]
- 25. Pfisterer M, Buser P, Osswald S, et al. Outcome of elderly patients with chronic symptomatic coronary artery disease with an invasive vs optimized medical treatment strategy: one‐year results of the randomized TIME trial. JAMA. 2003;289:1117–1123. [DOI] [PubMed] [Google Scholar]
- 26. Pepine CJ, Sharaf B, Andrews TC, et al. Relation between clinical, angiographic and ischemic findings at baseline and ischemia‐related adverse outcomes at 1 year in the Asymptomatic Cardiac Ischemia Pilot study. ACIP Study Group. J Am Coll Cardiol. 1997;29:1483–1489. [DOI] [PubMed] [Google Scholar]
- 27. Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. [DOI] [PubMed] [Google Scholar]
- 28. Koutouzis M, Grip L, Matejka G, et al. Primary percutaneous coronary interventions in nonagenarians. Clin Cardiol. 2010;33:157–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jeger RV, Tseng CH, Hochman JS, et al. Interhospital transfer for early revascularization in patients with ST‐elevation myocardial infarction complicated by cardiogenic shock—a report from the SHould we revascularize Occluded Coronaries for cardiogenic shocK? (SHOCK) trial and registry. Am Heart J. 2006;152:686–692. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information may be found in the online version of this article


