Abstract
Background:
The risk of excessive bleeding prompts physicians to stop multiple antiplatelet agents before minor surgery, which puts coronary stenting patients at risk for adverse thrombotic events.
Hypothesis:
We hypothesized that most dental extractions can be carried out safely without stopping multiple antiplatelet agents.
Methods:
All dental extraction patients who had undergone coronary stenting and who were also on oral multiple antiplatelet agents therapy were enrolled. One hundred patients underwent dental procedures without stopping antiplatelet agents. All wounds were sutured and followed up at 24 hours, 1 week, and 1 month after the procedure. There were 2233 patients who had not taken oral antiplatelet agents from a health promotion center and had teeth extracted by the same method. After performing propensity‐score matching for the entire population, a total of 100 matched pairs of patients were created. The primary outcome was a composite of excessive intraextraction blood loss, transfusion, and rehospitalization for bleeding, and the secondary outcome was a composite of death, nonfatal myocardial infarction, target lesion revascularization, and stent thrombosis within 1 month after the procedure.
Results:
There were 2 excessive intraextraction bleeding cases that continued at the extraction site for 4 and 5 hours, respectively, in the coronary stenting patients, and 1 excessive intraextraction bleeding case that continued for 3 hours in the control patients. There were no cases of transfusion, rehospitalization for bleeding, or major cardiovascular events for the 2 propensity‐matched groups.
Conclusions:
We found that most dental extractions in coronary stenting patients can be carried out safely without stopping multiple antiplatelet agents.
The authors have no conflicts of interest to disclose.
This study was supported in part by a grant from Yuhan Corporation, Ltd., Seoul, The Republic of Korea.
Introduction
Aspirin and clopidogrel (or ticlopidine) are widely used for their antiplatelet function effects, and although low‐dose aspirin (75–100 mg daily) and clopidogrel (75 mg daily) or ticlopidine (250 mg twice daily) are generally indicated in cases of angina and ischemic heart disease, especially after coronary stenting following myocardial infarction (MI) and stroke,1., 2. the fear of uncontrolled bleeding prompts physicians to recommend stopping aspirin and thienopyridine intake before surgical procedures, including dental extractions.3., 4., 5. This puts the patients at risk of developing thromboembolism, MI, or a cardiovascular accident.6., 7.
We conducted a study of 100 consecutive patients on long‐term oral multiple antiplatelet‐agent therapy scheduled for dental extractions. We did not stop antiplatelet agents and did not face any major untoward sequelae. We present our results of 100 matched pairs of patients who were compared and propose that most dental extractions can be carried out safely without stopping multiple antiplatelet‐agent therapy.
Methods
Study Group Population
One hundred patients who fulfilled all inclusion criteria were enrolled in this study. They included patients on long‐term (at least 7 days), oral, multiple antiplatelet agents, including aspirin (100 or 200 mg daily) with clopidogrel (75 mg daily), and if needed cilostazol (100 mg twice daily) therapy; patients who had undergone coronary drug‐eluting stenting; patients requiring dental extractions that could be performed on an outpatient basis; and patients who gave written informed consent to be included in the study.
Exclusion criteria were patients who were on any concurrent therapy such as birth control pills, other anticoagulation, any drug such as nonsteroidal anti‐inflammatory drugs that could interact with aspirin; patients who had atrial fibrillation or atrial flutter; patients who had cancer or a hematologic disorder; patients who had abnormal values for platelet count (<100,000/mm3); and patients who had a MI within 1 week.
Control Group Population
There were 2,233 patients enrolled from the health promotion center who had never taken oral antiplatelet agents and undergone coronary stenting, but had teeth extracted by the same method. Exclusion criteria were the same as for the study population group. After performing propensity‐score matching for the entire population, a total of 100 matched pairs of patients were created.
Dental Extraction
All dental extractions were performed on an outpatient basis under local anesthesia (xylocaine 2% with 1:200,000 epinephrine) by the same dentist (Jin Kim). Intraextraction blood loss was measured by weighing the swabs and by subtracting the volume of irrigation fluid from the total volume of fluid in the suction jar. All dental extraction sites were sutured with 3‐0 black braided silk, and a pressure pack was applied. The patients were checked 30 minutes after the completion of the procedure and were then discharged with strict instructions.
Follow‐Up and End Points
Follow‐up was completed after 24 hours, 1 week (when the sutures were removed), and 1 month. The primary outcome was a composite event during 1 month, defined as a composite of: (1) excessive intraextraction blood loss, (2) transfusion, or (3) rehospitalization for bleeding. Less than 30 mL blood loss was considered not excessive, and more than 30 mL was considered excessive. The secondary outcome was a composite of cardiac death, nonfatal MI, target lesion revascularization (TLR), and stent thrombosis (ST) within 1 month after the dental extraction. All deaths were considered cardiac unless a definite noncardiac cause could be established. ST was assessed based on the definitions of the Academic Research Consortium as definite, probable, or possible ST. An MI was defined as elevated cardiac enzymes (troponin or myocardial band fraction of creatine kinase) more than the upper limit of the normal value, with ischemic symptoms or electrocardiography findings indicative of ischemia that were not related to the index procedure. TLR was defined as repeat percutaneous coronary intervention of the lesion within 5 mm of stent deployment or bypass graft surgery of the target vessel.
Statistical Analyses
The propensity scores were estimated using multiple logistic regression analysis. Matching factors were age, gender, hypertension, diabetes, smoker, family history, number of extractive teeth, hemoglobin, HbA1c, fasting blood sugar, creatinine, hsCRP, lipid profile, uric acid, and left ventricular ejection fraction. A full nonparsimonious model was developed that included all variables listed in Tables 1, 2. The discrimination and calibration abilities of the propensity‐score model were assessed by means of the c‐statistic and the Hosmer‐Lemeshow statistic. Continuous variables were compared with a paired t test. All P values were 2‐tailed, and P < 0.05 was considered significant. All analyses were performed using the Statistical Analysis Software package version 9.1 (SAS Institute, Cary, NC).
Table 1.
Baseline Characteristics and Laboratory Data
| DES patients (n=100) | Control group (n=100) | P | ||
|---|---|---|---|---|
| Age (years) | mean ± SD | 63.26 ± 10.09 | 63.12 ± 11.01 | 0.663 |
| Male | n (%) | 72 (72) | 72 (72) | 0.782 |
| Hypertension | n (%) | 55 (55) | 54 (54) | 0.323 |
| DM | n (%) | 43 (43) | 41 (41) | 0.337 |
| Smoking | n (%) | 32 (32) | 32 (32) | 0.832 |
| FHx | n (%) | 21 (21) | 20 (20) | 0.454 |
| Dyslipidemia | n (%) | 43 (43) | 44 (44) | 0.774 |
| MI Hx | n (%) | 34 (34) | 0 (0) | — |
| CAD ‐ 1vd | n (%) | 43 (43) | 0 (0) | — |
| ‐ 2vd | n (%) | 40 (40) | 0 (0) | — |
| ‐ 3vd | n (%) | 15 (15) | 0 (0) | — |
| ‐ LM disease | n (%) | 2 (2) | 0 (0) | — |
| Aspirin + clopidogrel | n (%) | 59 (59) | 0 (0) | — |
| Asprin + clopidogrel+cliostazol | n (%) | 41 (41) | 0 (0) | — |
| Number of Stents | mean ± SD | 1.95 ± 0.94 | 0 | — |
| Number of extractive teeth | mean ± SD (Range) | 1.76 ± 1.22 (1∼ 6) | 1.75 ± 1.23 (1∼ 6) | 0.763 |
| The interval of extraction after stenting (months) | mean ± SD (Range) | 18.01 ± 11.70 (0.3∼ 51) | — | — |
| Hb (g/dl) | mean ± SD | 13.89 ± 1.54 | 14.24 ± 1.63 | 0.824 |
| Platelet (103/mm3) | mean ± SD | 126 ± 42 | 235 ± 56 | <0.001 |
| Prothrombin time (sec) | mean ± SD | 12.92 ± 0.13 | 11.64 ± 0.08 | 0.012 |
| Partial thormboplastin time (sec) | mean ± SD | 30.72 ± 0.54 | 26.74 ± 0.48 | 0.005 |
| HbA1c (%) | mean ± SD | 7.32 ± 1.07 | 7.24 ± 2.32 | 0.453 |
| FBS (mg/dL) | mean ± SD | 134.10 ± 58.04 | 128.26 ± 55.63 | 0.368 |
| Cr (mg/dL) | mean ± SD | 0.9 ± 0.23 | 0.8 ± 0.25 | 0.451 |
| hsCRP (mg/dL) | mean ± SD | 0.63 ± 1.74 | 0.52 ± 1.82 | 0.282 |
| T‐chol (mg/dL) | mean ± SD | 167.72 ± 40.57 | 172.83 ± 42.47 | 0.174 |
| TG (mg/dL) | mean ± SD | 160.18 ± 76.34 | 155.29 ± 71.28 | 0.162 |
| HDL‐c (mg/dL) | mean ± SD | 39.56 ± 9.22 | 42.39 ± 10.30 | 0.235 |
| LDL‐c (mg/dL) | mean ± SD | 107.69 ± 41.53 | 115.32 ± 43.26 | 0.262 |
| EF (%) | mean ± SD | 61.70 ± 10.02 | 64.56 ± 13.11 | 0.645 |
| Uric Acid (mg/dl) | mean ± SD | 5.37 ± 1.58 | 5.12 ± 2.02 | 0.547 |
Abbreviations: CAD, coronary artery disease; Cr, creatinine; DES, drug‐eluting stent; DM, diabetes mellitus; EF, ejection fraction; FBS, fasting blood sugar; FHx, family history; Hb, hemoglobin; HbA1c, hemoglobin A1c; HDL‐C, high‐density lipoprotein cholesterol; hsCRP, high sensitivity C‐reactive protein; LDL‐C, low‐density lipoprotein cholesterol; LM, left main; MI, myocardial infarction; SD, standard deviation; T‐chol, total cholesterol; TG, triglyceride; vd, vessel disease.
Table 2.
Characteristics of Excessive Intraextractive Bleeding Cases of Drug‐Eluting Stent Patients and Control Group Patientsa
| 1 | 2 | 3 | |
|---|---|---|---|
| Age (years) | 61 | 73 | 72 |
| gender | male | male | gender |
| Hypertension | presence | presence | presence |
| DM | presence | none | none |
| Smoking | presence | none | presence |
| FHx | none | presence | None |
| Dyslipidemia | presence | none | None |
| MI Hx | presence | none | None |
| CAD | 2 vessel disease | 1 vessel disease | None |
| Antiplatelet agents | Aspirin + clopidogrel+ cilostazol | Aspirin+ clopidogrel | None |
| Number of Stents mean ± SD | 3 | 1 | — |
| Number of extractive teeth | 2 | 3 | 3 |
| the interval of extraction after stenting (months) | 7 | 16 | — |
| the changed hemoglobin (g/dl) | −0.3 | −0.5 | −0.1 |
| Baseline Bleeding time (sec) | 125 | 155 | 115 |
| Prothormbin time (sec) | 12.6 | 11.6 | 11.8 |
| Partial thromboplastin time (sec) | 31.7 | 26.3 | 25.7 |
| Number of platelets (103/mm) | 132 | 165 | 253 |
Abbreviations: CAD, coronary artery disease; DM, diabetes mellitus; FHx, family history; MI Hx, myocardial infarction history; SD, standard deviation.
Drug‐eluting stenting patients are represented in columns labeled 1 and 2, and the control group patients in the column labeled 3.
Results
One hundred (72 males and 28 females) patients underwent coronary stenting. We used the first generation of drug‐eluting stents (DES). The stent types were the sirolimus‐eluting stent (Cordis Corp., Miami, FL) and paclitaxel‐eluting stent (Boston Scientific, Natick, MA). There were 100 patients of the matched control group who were included in this study. The mean age (± standard deviation) of patients was 63.26 ± 10.09 years (range, 46–88 years) in the coronary stenting group and 63.12 ± 11.01 years (range, 44–87 years) in the control group (P = 0.663). There were no significant differences in baseline risk factors and laboratory data except platelet count, prothrombin time (PT) and partial thromboplastin time (PTT). The coronary stenting group had lower platelet count and higher PT/PTT levels (Table 1). We thought that antiplatelet agents induced thrombocytopenia and were a strong independent factor and therefore tried unsuccessfully to control it using a propensity‐matching method. The interval of dental extraction after coronary stenting ranged from 0.3 to 51 months with a mean interval of 18.01 ± 11.70 months. The mean number of coronary stents placed was 1.95 ± 0.94, and the mean number of teeth extracted was 1.76 ± 1.22 (range, 1–6 teeth) (Table 1, Figure 1). Fifty‐nine patients had been on low‐dose aspirin and clopidogrel, whereas 41 patients had been on aspirin, clopidogrel, and cilostazol in the coronary stenting group (Table 1).
Figure 1.
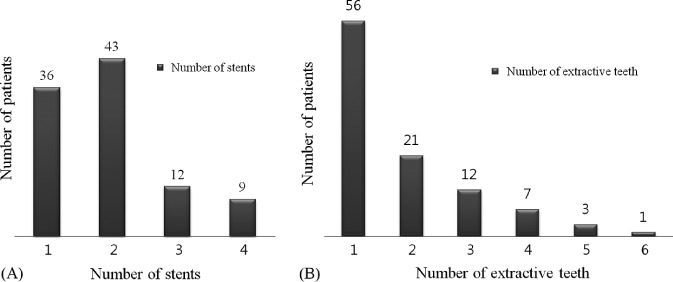
(A) Number of drug‐eluting stents for extracted patients. (B) Number of extractive teeth of drug‐eluting stenting patients.
There was no significant difference in primary and secondary outcomes (Table 3). Excessive intraextraction bleeding was encountered in 2 cases that continued at the extraction site for 4 and 5 hours, respectively, in the coronary stenting patients, and 1 excessive intraextraction bleeding case continued for 3 hours in the control patients after extraction. The patients were asked to apply a simple pressure pack. In the coronary stenting group, 1 case was on triple antiplatelet therapy, whereas the other case was on dual therapy (Table 2). There were no cases of transfusion, rehospitalization for bleeding, or major cardiovascular events within 1 month after dental extraction.
Table 3.
Primary Outcomes
| DES patients (n=100) | Control group (n=100) | P | ||
|---|---|---|---|---|
| Composite of excessive intraextractive blood loss, transfusion and re‐hospitalization | n (%) | 2 (2) | 1 (1) | 0.45 |
| Excessive intraextractive blood loss | n (%) | 2 (2) | 1 (1) | 0.36 |
| Transfusion | n (%) | 0 (0) | 0 (0) | — |
| Re‐hospitalization | n (%) | 0 (0) | 0 (0) | — |
Abbreviation: DES, drug‐eluting stent.
Discussion
Pototski and Amenabar reviewed the main anticoagulant drugs in use today and explained the dental management of patients on these drugs when subjected to minor oral surgery procedures. It can be concluded that the optimal international normalized ratio (INR) value for dental surgical procedures is 2.5 because it minimizes the risk of either hemorrhage or thromboembolism. Nevertheless, minor oral surgical procedures, such as biopsies, tooth extraction, and periodontal surgery can safely be done with an INR lower than 4.0.8 Discontinuation of dual or triple antiplatelet therapy during minor oral surgery had not been studied.
Discontinuation of antiplatelet therapy, including acetylsalicylic acid and thienopyridines, is the dominant risk factor for the occurrence of late stent thrombosis (LST) and very late stent thrombosis in patients with DES.9., 10., 11., 12., 13., 14., 15. For this reason, treatment guidelines now recommend maintaining dual antiplatelet therapy for at least 12 months.16., 17. However, because LST is such a rare event, it has been difficult to determine its exact incidence rate.18., 19., 20., 21. Importantly, for patients with DES who maintained their aspirin therapy, only 6% of cases occurred within 10 days of cessation of their thienopyridine, and only 2% of cases occurred within 5 days of cessation. In contrast, the vast majority of all cases in the other groups occurred within 2 weeks of antiplatelet discontinuation. If patients stopped both antiplatelet agents simultaneously, the median time to event was 7 days. If patients had previously stopped a thienopyridine with no ill effect and subsequently stopped acetylsalicylic acid, the median time to event was also 7 days from the time of acetylsalicylic acid cessation. If the thienopyridine was stopped but acetylsalicylic acid was maintained, the median time to event was 122 days. Among the 48 patients who stopped both agents, 36 cases (75%) occurred within 10 days. Among the 94 patients who discontinued a thienopyridine but continued acetylsalicylic acid, only 6 cases (6%) occurred within 10 days.22 These observations presented us with the dilemma of whether or not to stop antiplatelet therapy before minor oral surgery.
Our study was designed to examine the safety of continuation of antiplatelet therapy in patients with DES during dental extraction. Although several studies had concluded that long‐term low‐dose aspirin therapy should not be stopped before minor oral surgical procedures,23., 24., 25. the safety of continuation of dual or triple antiplatelet therapy during minor oral surgery had not been studied. Of the 100 patients with DES, excessive intraextraction bleeding was encountered in 2 cases that continued at the extraction site for 4 and 5 hours, respectively, after extraction. There were treated with the application of a simple pressure pack by the patients themselves. One case was on triple antiplatelet therapy, whereas the other case was on dual therapy. There were no cases of transfusion, rehospitalization for bleeding, or major cardiovascular events within 1 month after dental extraction. In addition, the minimal interval of dental extraction after coronary stenting was 9 days, and the maximal number of teeth extracted was 6. These results suggest that it is safe to continue dual (59%) or triple (41%) antiplatelet therapy during dental extraction, and that dental extraction does not need to be delayed regardless of time of coronary stenting and necessity to extract multiple teeth.
Investigation of the PT, PTT, and platelet count was performed in all patients. PT, PTT, and platelet count are first‐line basic laboratory tests for platelet function and are used to diagnose a bleeding diathesis. If these parameters are within their normal ranges, it is unlikely that a significant platelet defect is responsible for excessive clinical bleeding.26 According to our criteria, if a patient's platelet count was over 100,000/mm3, we would recommend that patients would not stop antiplatelet agents for 7 days and not delay dental extraction after coronary stenting.
Limitations
Our study has several potential limitations. First, this study was a single‐center, nonrandomized, and small‐sized study that required validation in multicenter randomized studies. Dentists are more likely to stop antiplatelet therapy before dental extraction if they think that the patient is at high risk for bleeding. It is conceivable that these patients could also be at high risk of LST if antiplatelet agents are withheld. Thus, the patients in whom antiplatelet therapy is stopped and then develop LST may be a higher‐risk subgroup of the total patient population. However, the risk for bleeding and the risk for LST do not necessarily occur in tandem. Rather, the risk for bleeding is closely related to the type of procedure the patient is undergoing, and this fact should be independent of the risk for LST. Thus, we believe that confounding by indication is not likely to be a major limitation of our study.
A second potential limitation is that only a single expert dentist extracted teeth. The results of the bleeding may vary with the degree of dentist expertise. In addition, only dental extraction cases have been reported in the literature, and other minor oral surgery cases could not be compared.
Third, the sample size is too small to make difference in the primary and secondary outcomes for our study, so we have to collect larger multicenter data for bleeding and major adverse cardiac events in a further evaluation.
Finally, our data do not include long‐term follow‐up. Furthermore, because of the large differences we observed in the timing of major adverse cardiovascular events, any such bias could affect the magnitude of the differences, but it is unlikely to affect the overall conclusions from our study.
Conclusion
Our study was designed to examine the safety of continuation during dental extraction of dual or triple antiplatelet therapy in patients with DES. We found that no severe bleeding or major cardiovascular events occurred after dental extraction except for 2 cases (2%). These data suggest that it may be feasible for patients with DES to continue their antiplatelet therapy, even triple antiplatelet therapy, for dental extraction. Although there remains a risk for bleeding with this strategy, continuation of multiple antiplatelet therapy may be relatively safe.
References
- 1. White HD, Gersh BJ, Opie LH. Antithrombotic agents: platelet inhibitors, anticoagulants, and fibrinolytics. In: Opie LH, Gersh BJ, eds. Drugs for the Heart. 5th ed. New Delhi, India: Saunders (Indian Edition); 2001:273–322. [Google Scholar]
- 2. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy: evidence‐based guidelines. Chest. 2004;126:163S–696S. [DOI] [PubMed] [Google Scholar]
- 3. Madan GA, Madan SG, Madan G, et al. Minor oral surgery without stopping daily low‐dose aspirin therapy: a study of 51 patients. J Oral Maxillofac Surg. 2005;63:1262–1265. [DOI] [PubMed] [Google Scholar]
- 4. Conti CR. Aspirin and elective surgical procedures [editorial]. Clin Cardiol. 1992;15:709. [DOI] [PubMed] [Google Scholar]
- 5. Speechley JA, Rugman FP. Some problems with anticoagulants in dental surgery. Dent Update. 1992;19:204–206. [PubMed] [Google Scholar]
- 6. Collet JP, Himbet F, Steg PG. Myocardial infarction after aspirin cessation in stable coronary artery disease patients. Int J Cardiol. 2000;76:257–258. [DOI] [PubMed] [Google Scholar]
- 7. Kaluza GL, Joseph J, Lee JR, et al. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol. 2000;35:1288–1294. [DOI] [PubMed] [Google Scholar]
- 8. Pototski M, Amenabar JM. Dental management of patients receiving anticoagulation or antiplatelet treatment. J Oral Sci. 2007;49:253–258. [DOI] [PubMed] [Google Scholar]
- 9. Eisenstein EL, Anstrom KJ, Kong DF, et al. Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation. JAMA. 2007;297:159–168. [DOI] [PubMed] [Google Scholar]
- 10. Park DW, Park SW, Park KH, et al. Frequency of and risk factors for stent thrombosis after drug‐eluting stent implantation during long‐term follow‐up. Am J Cardiol. 2006;98:352–356. [DOI] [PubMed] [Google Scholar]
- 11. Ho PM, Fihn SD, Wang L, et al. Clopidogrel and long‐term outcomes after stent implantation for acute coronary syndrome. Am Heart J. 2007;154:846–851. [DOI] [PubMed] [Google Scholar]
- 12. Spertus JA, Kettelkamp R, Vance C, et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug‐eluting stent placement: results from the PREMIER registry. Circulation. 2006;113:2803–2809. [DOI] [PubMed] [Google Scholar]
- 13. Artang R, Dieter RS. Analysis of 36 reported cases of late thrombosis in drug‐eluting stents placed in coronary arteries. Am J Cardiol. 2007;99:1039–1043. [DOI] [PubMed] [Google Scholar]
- 14. Kim SS, Jeong MH, Sim DS, et al. Very late thrombosis of a drug‐eluting stent after discontinuation of dual antiplatelet therapy in a patient treated with both drug‐eluting and bare‐metal stents. Korean Circ J. 2009;39:205–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jeon DS, Yoo KD, Park CS, et al. The effect of cilostazol on stent thrombosis after drug‐eluting stent implantation. Korean Circ J. 2010;40:10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. King SB III, Smith SC Jr, Hirshfeld JW Jr, et al. 2007. Focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:172–209. [DOI] [PubMed] [Google Scholar]
- 17. Grines CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Circulation. 2007;115:813–818. [DOI] [PubMed] [Google Scholar]
- 18. Shuchman M. Debating the risks of drug‐eluting stents. N Engl J Med. 2007;356:325–328. [DOI] [PubMed] [Google Scholar]
- 19. Stone GW, Moses JW, Ellis SG, et al. Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents. N Engl J Med. 2007;356:998–1008. [DOI] [PubMed] [Google Scholar]
- 20. Lagerqvist B, James SK, Stenestrand U, et al. Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden. N Engl J Med. 2007;356:1009–1019. [DOI] [PubMed] [Google Scholar]
- 21. Mauri L, Hsieh WH, Massaro JM, et al. Stent thrombosis in randomized clinical trials of drug‐eluting stents. N Engl J Med. 2007;356:1020–1029. [DOI] [PubMed] [Google Scholar]
- 22. Eisenberg MJ, Richard PR, Libersan D, et al. Safety of short‐term discontinuation of antiplatelet therapy in patients with drug‐eluting stents. Circulation. 2009;119:1634–1642. [DOI] [PubMed] [Google Scholar]
- 23. Ferraris VA, Swanson E. Aspirin usage and intraoperative blood loss in patients undergoing unexpected operations. Surg Gynecol Obstet. 1983;156:439–442. [PubMed] [Google Scholar]
- 24. Lawrence C, Sakuntabhai A, Tiling‐Grosse S. Effect of aspirin and nonsteroidal anti‐inflammatory drug therapy on bleeding complications in dermatologic surgical patients. J Am Acad Dermatol. 1994;31:988–992. [DOI] [PubMed] [Google Scholar]
- 25. Ardekian L, Gaspar R, Peled M, et al. Does low‐dose aspirin therapy complicate oral surgical procedures? J Am Dent Assoc. 2000;131:331–335. [DOI] [PubMed] [Google Scholar]
- 26. Chanarin I. Platelet function tests. In: Chanarin I, ed. Laboratory Hematology. London, UK: Churchill Livingstone; 1991:371–399. [Google Scholar]


