Abstract
Background:
Successful smoking cessation in stroke and coronary artery disease (CAD) patients is important, as smoking contributes to significant morbidity and mortality. The American Heart Association developed Get With The Guidelines (GWTG) to improve compliance with national guideline recommendations for cardiovascular care. Using data from GWTG, we examined trends associated with the smoking‐cessation counseling (SCC) performance measure.
Hypothesis:
Implementation of a systematic quality improvement program will increase compliance with the SCC performance measure.
Methods:
We evaluated compliance with SCC in current or recent smokers identified from 224 671 CAD admissions between 2002 and 2008 in the GWTG‐CAD database, and from 405 681 stroke admissions between 2002 and 2007 in the GWTG‐Stroke database. Additionally, we examined adherence to other performance and quality measures related to CAD and stroke care.
Results:
Overall, 55 904 GWTG‐CAD and 58 865 GWTG‐Stroke admissions were used for the analysis. Rates of SCC improved in each successive year during the study, from 67.6% to 97.4% (P < 0.001) in GWTG‐CAD and from 40.1% to 90.7% (P < 0.001) in GWTG‐Stroke. Compliance with SCC was up to 34.7% lower (P < 0.0001) in GWTG‐Stroke compared with GWTG‐CAD, but this difference decreased to 6.7% (P < 0.0001) by the end of the study period. Compliance with many other performance and quality measures was significantly lower among patients not receiving SCC.
Conclusions:
Get With The Guidelines has improved compliance with the SCC performance measure among patients with CAD and stroke. Although the initial disparity in rates of SCC between CAD and stroke patients gradually improved, the difference remained significant.
All authors had access to the data and participated in the preparation of this manuscript. GWTG‐CAD is a program of the American Heart Association (Dallas, TX) and is supported in part by an unrestricted educational grant from Merck/Schering‐Plough Pharmaceutical (White House Station, NJ) and Pfizer (New York, NY). The analysis of registry data was performed at Duke Clinical Research Institute (Durham, NC), which receives funding from the American Heart Association. The sponsors were not involved in the design, analysis, preparation, review, or approval of this manuscript.
Pei‐Hsiu Huang, Charles X. Kim, Amir Lerman, David Dai, Warren Laskey, W. Frank Peacock, Eric D. Peterson, Eric E. Smith, Gregg C. Fonarow, and Lee H. Schwamm have no relevant disclosures. Christopher P. Cannon reports receiving research grants and support from Accumetrics, AstraZeneca, GlaxoSmithKline, Merck, Essentialis, and Takeda; involvement in the advisory board for Bristol‐Myers Squibb/Sanofi, Novartis, and Alnylam; honoraria for development of independent educational symposia from Pfizer and AstraZeneca; and is a clinical advisor having equity in Automedics Medical Systems. Adrian F. Hernandez reports receiving research grants from Johnson & Johnson and Amylin, and honoraria from AstraZeneca, Corthera, and Sanofi‐Aventis. Deepak L. Bhatt reports the following associations and memberships: advisory board, Medscape Cardiology; board of directors, Boston VA Research Institute, Society of Chest Pain Centers; chair, American Heart Association Get With The Guidelines Science Subcommittee; honoraria, American College of Cardiology (editor, Clinical Trials, Cardiosource), Duke Clinical Research Institute (clinical trial steering committees), Slack Publications (chief medical editor, Cardiology Today Intervention), and WebMD (CME steering committees); research grants, Amarin, AstraZeneca, Bristol‐Myers Squibb, Eisai, Ethicon, Medtronic, Sanofi Aventis, and The Medicines Company; and unfunded research, PLx Pharma and Takeda.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
Cigarette smoking remains a prevalent modifiable risk factor for cardiovascular disease, with an estimated 21% of adults in the United States reporting current cigarette use in 2009.1 As smoking is associated with 2‐ to 4‐fold increased relative risk for stroke2, 3, 4, 5 and 1.5‐ to 3‐fold increased relative risk for myocardial infarction (MI),6, 7 smoking cessation can have a large impact on health outcomes. Patients who quit smoking after an acute MI (AMI) have an approximate 50% reduction in mortality.8, 9, 10
The challenge of successful smoking cessation involves multiple patient and physician barriers. Patients often fail to acknowledge the risks of smoking and therefore lack the motivation to quit.11 Because physicians often experience limited success using smoking‐cessation counseling (SCC), they frequently do not intervene.12 However, even brief physician advice may lead a small percentage of smokers to quit.12, 13 SCC initiated during hospitalization may potentially result in greater effectiveness, particularly when coupled with inpatient smoking‐cessation programs or cardiac rehabilitation and when support continues after discharge.14, 15
Recognizing the significant benefits of smoking cessation, national guidelines from the American Heart Association (AHA), American College of Cardiology, and American Stroke Association recommend smoking cessation as part of the strategy for secondary prevention of MI and stroke.16, 17 Evidence suggests that a significant gap exists between guideline knowledge and its adoption into clinical practice.18, 19 To address these gaps in care, the AHA established Get With The Guidelines (GWTG) based on core performance measures, including SCC, developed by the Centers for Medicare & Medicaid Services and the Joint Commission to improve the quality of care in the treatment of cardiovascular disease. Using this large national database, we examined adherence to SCC in patients admitted for coronary artery disease (CAD)‐related diagnoses and stroke.
Methods
The AHA designed the GWTG quality‐improvement initiative to address deficiencies in implementing evidence‐based guidelines for secondary prevention in cardiovascular disease. Get With The Guidelines provides a simple set of tools for hospitals to modify their systems of healthcare delivery to improve outcomes in cardiovascular care. Participating hospitals attend a series of multidisciplinary workshops reviewing guidelines evidence and implementation strategies. Hospitals use a web‐based Patient Management Tool to submit data, allowing the option for point‐of‐service data collection. The Patient Management Tool also provides feedback to hospitals through real‐time online reports. Further specifics about the program design have been described extensively.20, 21, 22, 23
Patient Population
We examined data from 350 221 admissions in the GWTG‐CAD database from 574 sites between January 1, 2000, and March 28, 2008, and 529 287 stroke admissions from 1056 sites between October 1, 2001, and December 30, 2007, in the GWTG‐Stroke database. We excluded 48 308 admissions from GWTG‐CAD that were not for a primary CAD‐related diagnosis (AMI, unstable angina, chronic stable angina, or ischemic heart disease). Additionally, 120 875 admissions in the Stroke module with the primary diagnosis of transient ischemic attack were excluded. All data from sites missing past medical‐history information for >25% of admissions were also excluded (n = 62 302 in GWTG‐CAD; n = 519 in GWTG‐Stroke), as were admissions without documentation of smoking history (n = 14 192 in GWTG‐CAD; n = 1508 in GWTG‐Stroke). Finally, data from admissions prior to 2002 were excluded (n = 748 in GWTG‐CAD; n = 704 in GWTG‐Stroke). After all exclusions, patients identified as current or recent (within 1 y) smokers were eligible for SCC. In the end, data from 55 904 GWTG‐CAD and 58 865 GWTG‐Stroke admissions were used in the analysis.
Performance Measures
Performance‐measure definitions were modeled after those of the Centers for Medicare & Medicaid Services and the Joint Commission ORYX quality‐measure sets.24, 25 Eligible patients did not have any contraindication or intolerance to each specific measure. Data for measures were recorded as a binary variable and expressed as a percentage of eligible patients in the analysis.
Performance measures assessed in GWTG‐CAD were (1) aspirin use within the first 24 hours of admission, (2) aspirin use on discharge, (3) β‐blocker use on discharge, (4) angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker use on discharge for patients with left ventricular systolic dysfunction (ejection fraction <40%), and (5) use of lipid‐lowering therapy on discharge for patients with low‐density lipoprotein (LDL) >100 mg/dL. We also created a composite performance measure calculated by dividing the total number of interventions performed for all 5 individual measures by the aggregate number of eligible patients for each individual measure. Additionally, we assessed the following acute and discharge quality measures: (1) β‐blocker use in the first 24 hours of admission, (2) thrombolytics administered within 30 minutes for patients with ST‐segment elevation or new left bundle branch block on electrocardiogram, (3) percutaneous coronary intervention within 90 minutes for patients with ST‐segment elevation or new left bundle branch block on electrocardiogram, (4) angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker on discharge for AMI patients, (5) clopidogrel use on discharge for patients with AMI or percutaneous coronary intervention, (5) blood pressure <140/90 mm Hg within 48 hours of discharge, (6) measurement of LDL during hospitalization, (7) weight‐management or physical‐activity recommendations for overweight patients, and (8) cardiac rehabilitation referral or recommendations for physical activity.
Performance measures reported in GWTG‐Stroke included (1) intravenous tissue plasminogen activator (t‐PA) given within 3 hours of symptom onset for patients presenting within 2 hours of symptom onset, (2) use of antithrombotics in the first 48 hours of admission, (3) antithrombotics prescribed on discharge, (4) use of anticoagulation for patients with atrial fibrillation, (5) venous thromboembolism prophylaxis, and (6) lipid‐lowering therapy on discharge for patients with LDL >100 mg/dL. A composite performance measure similar to that for the GWTG‐CAD measures was also evaluated. Additional quality measures include (1) t‐PA within 3 hours of symptom onset for patients presenting within 3 hours of symptom onset, (2) t‐PA within 60 minutes of arrival to the emergency department, (3) door‐to‐computed tomographic imaging in 25 minutes or less, (4) measurement of LDL during hospitalization, (5) dysphagia screening, (6) diabetic medication use on discharge for diabetics, and (7) weight‐management recommendations for overweight patients.
Statistical Analysis
Categorical variables are presented as the percentage of eligible patients. Continuous variables are expressed as mean ± SD or median and interquartile range (IQR). The Pearson χ 2 test was used for univariate analysis of categorical variables and the Wilcoxon rank‐sum test for continuous variables. Generalized estimating equation (GEE) multivariate models were used to examine the rates of SCC per year after adjustment for age, sex, race, body mass index, insurance, medical history, cardiac or neurologic diagnosis, and hospital type and region. The yearly rates of SCC among eligible patients in GWTG‐CAD and GWTG‐Stroke were compared using the χ 2 test. All analyses were performed using SAS software, version 9.1 (SAS Institute, Cary, NC).
Results
The population used for this analysis consisted of 55 904 GWTG‐CAD and 58 865 GWTG‐Stroke patient admissions who were documented to be current or recent smokers. Overall, 87.9% of eligible GWTG‐CAD patients and 80.7% of eligible GWTG‐Stroke patients were documented to have received SCC prior to or at the time of hospital discharge over the study period. Table 1 shows the baseline characteristics of patients eligible for SCC from GWTG‐CAD and GWTG‐Stroke. The mean age of CAD patients was 57.7 ± 11.8 years with 68.9% males, whereas the mean age of the stroke patients was 59.4 ± 12.9 years with 57.6% males. In both cohorts, white patients made up the largest portion of the population, followed by African American, Hispanic, Asian, and others. Among the CAD patients, 11.2% were diagnosed with ST‐segment elevation MI (STEMI), 14.8% with non–ST‐segment elevation MI (NSTEMI), and 50.4% with an unspecified MI. Additionally, 11.1% of patients were admitted for a primary diagnosis of heart failure with CAD. The majority of stoke patients were diagnosed with ischemic stroke (82.7%).
Table 1.
Patient and Hospital Characteristics
| GWTG‐CAD | Overall [N = 55 904] | SCC [N = 49 114] | No SCC [N = 6790] | GWTG‐Stroke | Overall [N = 58 865] | SCC [N = 47 449] | No SCC [N = 11 366] |
|---|---|---|---|---|---|---|---|
| Age, y | 57.7 ± 11.8 | 57.1 ± 11.6 | 61.5 ± 12.9 | Age, y | 59.4 ± 12.9 | 59.0 ± 12.6 | 60.9 ± 13.8 |
| Male sex (%) | 68.9 | 69.2 | 66.4 | Male sex (%) | 57.6 | 59.1 | 56.1 |
| Race (%) | Race (%) | ||||||
| White | 73.7 | 74.4 | 68.8 | White | 69.3 | 70.0 | 66.3 |
| African | 9.9 | 9.9 | 9.8 | African | 20.7 | 20.5 | 21.9 |
| American | American | ||||||
| Hispanic | 6.2 | 6.1 | 7.1 | Hispanic | 3.7 | 3.7 | 3.7 |
| Asian | 2.1 | 1.9 | 4.1 | Asian | 1.4 | 1.4 | 1.6 |
| Other/unknown | 8.0 | 7.7 | 10.2 | Other/unknown | 4.9 | 4.6 | 6.5 |
| Medical history (%) | Medical history (%) | ||||||
| Hypertensiona | 57.5 | 56.9 | 61.7 | Hypertension | 66.3 | 66.1 | 66.8 |
| Dyslipidemiaa | 40.1 | 41.6 | 29.2 | Dyslipidemiaa | 32.0 | 32.9 | 28.3 |
| DMa | 24.9 | 24.1 | 30.2 | DM | 23.5 | 23.4 | 24.2 |
| Prior MIa | 19.7 | 19.4 | 21.99 | Prior stroke or TIAb | 23.4 | 23.2 | 24.7 |
| Heart failure | 13.4 | 11.9 | 24.2 | Carotid stenosisb | 5.1 | 4.9 | 5.8 |
| PVDa | 8.7 | 8.4 | 11.1 | AFa | 6.3 | 5.9 | 7.7 |
| Prior stroke or TIAa | 5.4 | 5.1 | 8.0 | CAD or prior MIc | 20.6 | 20.4 | 21.3 |
| CAD diagnosis (%)a | Stroke diagnosis (%)a | ||||||
| STEMI | 11.2 | 12.4 | 2.9 | Ischemic stroke | 82.7 | 84.3 | 75.9 |
| NSTEMI | 14.8 | 16.3 | 4.0 | Intracerebral hemorrhage | 8.7 | 8.0 | 11.5 |
| CAD | 12.5 | 12.4 | 13.2 | Subarachnoid hemorrhage | 5.4 | 4.8 | 8.2 |
| Heart failure with CAD | 11.1 | 9.2 | 24.7 | Unspecified stroke | 3.2 | 2.9 | 4.5 |
| Unspecified MI | 50.4 | 49.8 | 55.1 | ||||
| Hospital type (%)a | Hospital type (%)a | ||||||
| Academic | 58.9 | 59.7 | 53.2 | Academic | 65.8 | 65.4 | 67.6 |
| Nonacademic | 40.7 | 39.9 | 46.4 | Nonacademic | 33.0 | 33.7 | 30.2 |
| Unknown | 0.4 | 0.4 | 0.5 | Unknown | 1.1 | 0.9 | 2.3 |
| Region (%)a | Region (%)a | ||||||
| Northeast | 17.2 | 17.5 | 15.2 | Northeast | 20.4 | 20.4 | 20.5 |
| Midwest | 25.0 | 25.5 | 21.3 | Midwest | 23.3 | 22.3 | 27.5 |
| South | 33.3 | 33.8 | 29.7 | South | 41.5 | 42.9 | 35.5 |
| West | 24.5 | 23.2 | 33.8 | West | 14.8 | 14.3 | 16.5 |
Abbreviations: AF, atrial fibrillation; CAD, coronary artery disease; DM, diabetes mellitus; GWTG, Get With The Guidelines; MI, myocardial infarction; NSTEMI, non–ST‐segment elevation myocardial infarction; PVD, peripheral vascular disease; SCC, smoking‐cessation counseling; STEMI, ST‐segment elevation myocardial infarction; TIA, transient ischemic attack.
P < 0.0001.
P < 0.001.
p < 0.05.
The characteristics among patients who did and did not receive SCC are also shown in Table 1. Patients who were offered SCC were younger and more frequently male. White patients received SCC more often than patients of other races. Although a greater portion of patients receiving SCC had dyslipidemia, no other cardiovascular risk factor was more prevalent in these patients. In both CAD and stroke cohorts, SCC was offered more frequently in patients with a definitive diagnosis of an ischemic process (STEMI, NSTEMI, ischemic stroke). Academic hospitals adhered to the SCC performance measure more frequently than nonacademic hospitals in GWTG‐CAD; the opposite was true in GWTG‐Stroke.
In multivariable GEE analyses after adjusting for the correlation of data in hospitals as well as for patient and hospital characteristics, there were significant improvements in the odds of SSC being provided in both GWTG‐CAD (odds ratio: 1.50 [1.39–1.62] per year; P < 0.001) and GWTG‐Stroke (odds ratio: 1.62 [1.53–1.71] per year; P < 0.001). However, there was a difference in the rates of SCC between the 2 cohorts for each year of the study (P < 0.0001 for each year; Figure 1). In 2002, 67.6% of eligible patients in GWTG‐CAD received SCC compared with 40.1% of eligible patients in GWTG‐Stroke, a 27.5% difference. In 2003, the difference in rates of SCC between the CAD and Stroke patients increased to 34.7% before decreasing in each subsequent year for the remainder of the study period. In 2007, 97.4% of eligible GWTG‐CAD patients and 90.7% of eligible GWTG‐Stroke patients received SCC, a difference of only 6.7%.
Figure 1.
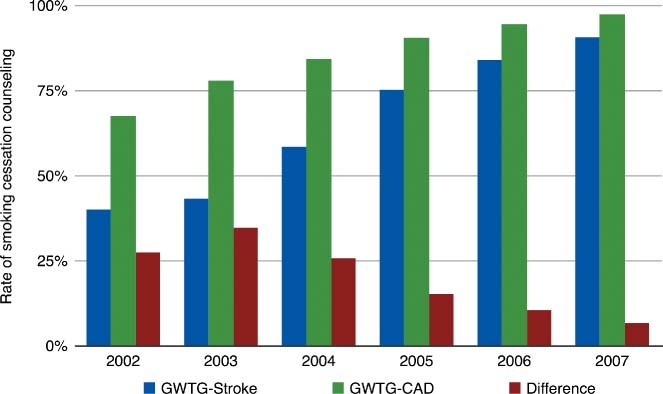
Rates of smoking cessation counseling among eligible patients in GWTG‐CAD and GWTG‐Stroke. p < 0.001 for the yearly increase in both GWTG‐CAD and GWTG‐Stroke. The red bars represent the difference between the GWTG‐CAD and GWTG‐Stroke rates of smoking cessation counseling (p < 0.0001 for each year).
Additional analyses were performed to explore the rates of compliance with other performance measures and to assess the association of discharge destination with SCC being provided or not. Tables 2 and 3 show the rates of adherence to the CAD performance and quality measures. Tables 4 and 5 display corresponding data about adherence to stroke performance and quality measures. Rates of adherence with all other performance measures as well as compliance with most of the quality measures were significantly lower among patients who did not receive SCC.
Table 2.
Rate of Adherence to GWTG‐CAD Performance Measures
| GWTG‐CAD Performance Measure | Overall [N = 55 904] | SCC [N = 49 114] | No SCC [N = 6790] |
| Aspirin given in the first 24 hours of admissiona | 94.2% | 94.9% | 88.4% |
| Aspirin on discharged on aspirina | 93.9% | 95.3% | 82.8% |
| β‐Blocker on dischargea | 92.7% | 94.2% | 81.9% |
| ACE inhibitor or ARB on discharge for patients with LVSDa | 82.7% | 84.2% | 73.3% |
| Lipid‐lowering therapy on discharge for patients with LDL >100 mg/dLa | 88.9% | 90.1% | 75.1% |
| Composite performance measurea,b | 89.5% | 95.2% | 59.8% |
Abbreviations: ACE, angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; CAD, coronary artery disease; GWTG, Get With The Guidelines; LDL, low‐density lipoprotein; LVSD, left ventricular systolic dysfunction; SCC, smoking‐cessation counseling.
P < 0.0001 (% of eligible patients).
Composite performance measure = total no. interventions ÷ no. eligible patients.
Table 3.
Rate of Adherence to GWTG‐CAD Quality Measures
| GWTG‐CAD Quality Measure | Overall [N = 55 904] | SCC [N = 49 114] | No SCC [N = 6790] |
|---|---|---|---|
| Acute Quality Measures | |||
| β‐Blocker given within the first 24 hours of admission (%)a | 89.4 | 90.6 | 79.1 |
| Thrombolytics administered within 30 minutes (%) | 39.2 | 39.0 | 40.3 |
| Time to thrombolytic administration, min, median (IQR) | 38 (23–65) | 38 (23–64) | 34.5 (20–78) |
| PCI within 90 min (%)a | 54.6 | 55.1 | 44.5 |
| Time to PCI, min, median (IQR)a | 86 (62–121) | 86 (62–120) | 96 (71–147) |
| Discharge Quality Measures (%) | |||
| ACE inhibitor or ARB on discharge for AMI patientsa | 72.3 | 73.8 | 59.6 |
| Clopidogrel on discharge for patients with AMI or PCIa | 88.1 | 88.4 | 83.9 |
| Blood pressure <140/90 mm Hg within 48 hours prior to discharge | 54.2 | 54.4 | 56.6 |
| Measurement of LDL during hospitalization | 68.3 | 70.8 | 50.3 |
| Weight management or physical activity recommendations for overweight patientsa | 83.4 | 85.8 | 64.1 |
| Referral to cardiac rehabilitation or given physical activity recommendations | 82.8 | 85.5 | 62.9 |
Abbreviations: ACE, angiotensin‐converting enzyme; AMI, acute myocardial infarction; ARB, angiotensin receptor blocker; CAD, coronary artery disease; GWTG, Get With The Guidelines; LDL, low‐density lipoprotein; PCI, percutaneous coronary intervention; SCC, smoking‐cessation counseling. Percent of eligible patients.
P ≤ 0.0001.
Table 4.
Rate of Adherence to GWTG‐Stroke Performance Measures
| GWTG‐Stroke Performance Measure | Overall [N = 58 865] % | SCC [N = 47 449] % | No SCC [N = 11 366] % |
|---|---|---|---|
| t‐PA for patients arriving within 2 hours of symptom onseta,b | 65.3 | 69.4 | 48.6 |
| Antithrombotics given within 48 hoursb | 95.6 | 96.5 | 91.5 |
| Antithrombotics on dischargeb | 98.5 | 99.0 | 96.4 |
| Anticoagulation discharge for AFb | 97.0 | 97.9 | 93.5 |
| Venous thromboembolism prophylaxisb | 87.1 | 88.6 | 81.2 |
| Lipid‐lowering therapy on dischargeb | 82.7 | 84.4 | 73.3 |
| Composite performance measureb,c | 88.8 | 94.7 | 62.0 |
Abbreviations: AF, atrial fibrillation; GWTG, Get With The Guidelines; SCC, smoking cessation counseling; t‐PA, tissue plasminogen activator. Percent of eligible patients.
t‐PA given within 3 hours of symptom onset for patients presenting within 2 hours of symptom onset.
P < 0.0001.
Composite performance measure = total no. interventions ÷ no. eligible patients.
Table 5.
Rate of Adherence to GWTG‐Stroke Quality Measures
| GWTG‐Stroke Quality Measure | Overall [N = 58 865] | SCC [N = 47 449] | No SCC [N = 11 366] |
|---|---|---|---|
| t‐PA <3 hours from onset of symptoms if arrival to ED <3 hours from onset of symptoms, %a | 52.9 | 56.7 | 38.2 |
| Time from symptom onset to t‐PA, min, median (IQR) | 144 (116–169) | 144 (116–169) | 143 (120–167) |
| t‐PA ≤ 60 min from arrival to ED, %b | 26.4 | 27.5 | 20.4 |
| Time from ED arrival to t‐PA, min, median (IQR)b | 80 (60–103) | 79 (59–101) | 85 (65–107) |
| Reasons for no intravenous t‐PA, %a | 91.1 | 93.0 | 83.0 |
| Door to CT ≤ 25 min, % | 36.8 | 37.8 | 32.5 |
| Door to CT time, min, median (IQR)a | 34 (20–63) | 33 (19–62) | 37 (21–69.5) |
| Measurement of LDL during hospitalization, %a | 80.4 | 83.3 | 67.0 |
| Dysphagia screening, %a | 60.7 | 62.7 | 53.9 |
| Diabetic medications on discharge, %a | 82.5 | 84.5 | 74.7 |
| Discharged with weight‐management recommendations, %a | 46.8 | 51.7 | 22.1 |
Abbreviations: CT, computed tomography; ED, emergency department; GWTG, Get With The Guidelines; LDL, low‐density lipoprotein; SCC, smoking cessation counseling; t‐PA, tissue plasminogen activator.
Percent of eligible patients.
P ≤ 0.0001.
P < 0.05.
Discussion
In this study we demonstrate the following key findings: (1) adherence to the SCC performance measure increased with each subsequent study year in GWTG‐CAD and GWTG‐Stroke, (2) the rate of SCC was lower in GWTG‐Stroke compared with GWTG‐CAD for every year of the study, (3) the difference in rates of SCC between GWTG‐CAD and GWTG‐Stroke decreased over time, and (4) rates of compliance with other performance measures were lower among patients who did not receive SCC in both GWTG‐CAD and GWTG‐Stroke.
Historically, SCC was provided to only 40% to 58% of eligible patients admitted for AMI19, 22, 26 and to only 5% to 21% of eligible patients admitted for stroke.27, 28 We show that implementation of GWTG significantly improved adherence to the SCC metric in both CAD (68% to 97%) and stroke (40% to 91%) patients. This finding is consistent with results seen in other quality‐improvement programs. Adherence to SCC increased from 58% to 73% in a study conducted at southeast Michigan hospitals for AMI patients.26 The Michigan Acute Stroke Care Overview and Treatment Surveillance System (MAS‐COTS) program demonstrated an improvement in smoking cessation from 37% to 68% during a 6‐month period in 2004.29 The larger Paul Coverdell National Acute Stroke Registry reported an improvement in SCC from 21% at baseline to 79%.30
However, despite improvement in the rates of SCC, we found a difference of up to 35% between the CAD and stroke patients during the study period. This difference in SCC rates decreased with each successive study year. To our knowledge, the potential reasons for this disparity have not previously been explored. Part of this difference may be attributed to the emphasis on different aspects of care between cardiac and stroke patients. Medical complications frequently occur after stroke and contribute to significant morbidity and mortality. In the placebo arm of the Randomized Trial of Tirilazad Mesylate in Acute Stroke (RANTTAS) study, ≥1 complication occurred in 95% of patients and 32% suffered ≥1 serious complication.31 Another study reported serious cardiac adverse events in 19% of patients, with 4% of deaths attributed to cardiac causes.32 Recent AHA/American Stroke Association guidelines on the management of ischemic stroke emphasize the importance of monitoring for and prevention of complications.33 Attention to these issues lead physicians to dedicate much of the evaluation and treatment during the hospitalization toward rehabilitation of physical health and mental function rather than smoking cessation. Although the majority of stroke survivors regain functional independence, approximately one‐third continue to have significant disabilities several months after discharge and 20% to 26% require institutional care at discharge.34 Allen et al recently demonstrated lower performance measure compliance, including SCC, in Medicare recipients with heart failure discharged to a skilled nursing facility compared with patients discharged home.35 This finding may again illustrate the difference in the primary treatment focus during hospitalization between those planning to continue care at a subsequent medical facility and those discharged home with risk of re‐establishing prior habits.
Barriers relating to physician knowledge, attitude, and behavior explain some of the deficiencies in applying guideline recommendations.36 In our analysis, SCC was provided at a greater frequency to CAD patients admitted for a diagnosis relating to an ischemic etiology (NSTEMI, STEMI) compared with patients with a diagnosis less clearly associated with ischemia. Likewise, SCC was provided more often for patients with ischemic stroke, which comprised >80% of the total stroke diagnoses and about 75% of stroke diagnoses among those not receiving SCC in GWTG‐Stroke, compared with strokes of other etiologies. Additionally, we showed that patients who did not receive SCC were more often deficient in other core CAD and stroke performance measures as well as other CAD and stroke quality measures. Thus, it appears that a significant portion of patients not provided SCC also receives suboptimal treatment in many key areas of cardiovascular care. Get With The Guidelines attempts to address some of these barriers on a system level by implementing interdisciplinary workshops to bridge knowledge gaps or change physician attitudes about evidence‐based guidelines. Since inception, GWTG has successfully improved adherence to all CAD37 and stroke38 performance measures including SCC in participating hospitals.
The rates of SCC improved in CAD and stroke patients over the study period and also the difference in counseling between CAD and stroke patients diminished. However, we must be careful not to interpret these findings as necessarily indicating improvements in actual smoking cessation or clinical outcomes. Although studies have correlated smoking cessation with lower short‐ and long‐term mortality,39, 40, 41 the SCC performance measure as implemented by hospitals may not actually reflect the provision of counseling sufficient to improve the actual rates of smoking cessation. In an analysis of the Prospective Registry Evaluating Myocardial Infarction: Events and Recovery (PREMIER) registry in patients hospitalized with AMI, although patients with documented SCC were more likely to recall receiving SCC at 1 month, their rate of quitting at 1 year was actually lower than that of patients without SCC. At the hospital level there was no correlation of SCC with either 6‐month or 1‐year rates of successful quitting.42 These observations question the value of the SCC performance measure in its current form. Efforts are needed to develop a measure that can more reliably capture clinically effective SCC and/or measures of actual cessation rates.
Other limitations need to be considered when interpreting our results. Hospital participation in GWTG programs is voluntary and may select institutions with different levels of motivation and resources. Although there is some overlap, different hospitals were participating in GWTG‐CAD and GWTG‐Stroke. Compliance with the SCC metric was based on documentation in the medical record alone. The quality of SCC and actual quit rates were not assessed. We did not report data on mortality and we were unable to explore the association of these results to patient outcomes. Furthermore, we cannot determine if our observations were due to external factors such as increased guidelines awareness or implementation of pay‐for‐performance programs. Additional methodological considerations include statistically significant findings of seemingly small absolute differences due to multiple comparisons and the large sample sizes.
Conclusion
We have found that GWTG effectively improved compliance with the SCC performance metric in patients admitted with stroke and CAD‐related diagnoses and that the disparity in rates of SCC between stroke and CAD patients decreased over the length of our study. Further studies are needed to clarify the reasons for the disparity in stroke patients. Get With The Guidelines represents an important step in improvement of patient care, but we must continue to explore and implement effective treatments for smoking cessation.
References
- 1. Vital signs: current cigarette smoking among adults aged ≥18 years—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1135–1140. [PubMed] [Google Scholar]
- 2. Kawachi I, Colditz GA, Stampfer MJ, et al. Smoking cessation and decreased risk of stroke in women. JAMA. 1993;269:232–236. [PubMed] [Google Scholar]
- 3. Wannamethee SG, Shaper AG, Whincup PH, et al. Smoking cessation and the risk of stroke in middle‐aged men. JAMA. 1995;274:155–160. [PubMed] [Google Scholar]
- 4. Kurth T, Kase CS, Berger K, et al. Smoking and the risk of hemorrhagic stroke in men. Stroke. 2003;34:1151–1155. [DOI] [PubMed] [Google Scholar]
- 5. Kurth T, Kase CS, Berger K, et al. Smoking and risk of hemorrhagic stroke in women. Stroke. 2003;34:2792–2795. [DOI] [PubMed] [Google Scholar]
- 6. Njolstad I, Arnesen E, Lund‐Larsen PG. Smoking, serum lipids, blood pressure, and sex differences in myocardial infarction: a 12‐year follow‐up of the Finnmark Study. Circulation. 1996;93:450–456. [DOI] [PubMed] [Google Scholar]
- 7. Prescott E, Hippe M, Schnohr P, et al. Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ. 1998;316:1043–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilson K, Gibson N, Willan A, et al. Effect of smoking cessation on mortality after myocardial infarction: meta‐analysis of cohort studies. Arch Intern Med. 2000;160:939–944. [DOI] [PubMed] [Google Scholar]
- 9. Chow CK, Jolly S, Rao‐Melacini P, et al. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121:750–758. [DOI] [PubMed] [Google Scholar]
- 10. Gerber Y, Rosen LJ, Goldbourt U, et al. Smoking status and long‐term survival after first acute myocardial infarction a population‐based cohort study. J Am Coll Cardiol. 2009;54:2382–2387. [DOI] [PubMed] [Google Scholar]
- 11. Ayanian JZ, Cleary PD. Perceived risks of heart disease and cancer among cigarette smokers. JAMA. 1999;281:1019–1021. [DOI] [PubMed] [Google Scholar]
- 12. Ockene JK. Physician‐delivered interventions for smoking cessation: strategies for increasing effectiveness. Prev Med. 1987;16:723–737. [DOI] [PubMed] [Google Scholar]
- 13. Lancaster T, Stead L. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2004;CD000165. [DOI] [PubMed] [Google Scholar]
- 14. Dawood N, Vaccarino V, Reid KJ, et al. Predictors of smoking cessation after a myocardial infarction: the role of institutional smoking cessation programs in improving success. Arch Intern Med. 2008;168:1961–1967. [DOI] [PubMed] [Google Scholar]
- 15. Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008;168:1950–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Smith SC Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006;47:2130–2139. [DOI] [PubMed] [Google Scholar]
- 17. Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:227–276. [DOI] [PubMed] [Google Scholar]
- 18. O'Connor GT, Quinton HB, Traven ND, et al. Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. JAMA. 1999;281:627–633. [DOI] [PubMed] [Google Scholar]
- 19. Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels. JAMA. 2000;284:1670–1676. [DOI] [PubMed] [Google Scholar]
- 20. LaBresh KA, Tyler PA. A collaborative model for hospital‐based cardiovascular secondary prevention. Qual Manag Health Care. 2003;12:20–27. [DOI] [PubMed] [Google Scholar]
- 21. Hong Y, LaBresh KA. Overview of the American Heart Association “Get with the Guidelines” programs: coronary heart disease, stroke, and heart failure. Crit Pathw Cardiol. 2006;5:179–186. [DOI] [PubMed] [Google Scholar]
- 22. LaBresh KA, Ellrodt AG, Gliklich R, et al. Get with the guidelines for cardiovascular secondary prevention: pilot results. Arch Intern Med. 2004;164:203–209. [DOI] [PubMed] [Google Scholar]
- 23. LaBresh KA, Reeves MJ, Frankel MR, et al. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med. 2008;168:411–417. [DOI] [PubMed] [Google Scholar]
- 24. The Joint Commission. Acute Myocardial Infarction Core Measure Set. http://www.jointcommission.org/assets/1/6/Acute%20Myocardial%20Infarction.pdf. Accessed January 14, 2012..
- 25. The Joint Commission. Stroke (STK) Core Measure Set. http://www.jointcommission.org/assets/1/6/Stroke.pdf. Acces sed; January 14, 2012.. [Google Scholar]
- 26. Mehta RH, Montoye CK, Faul J, et al. Enhancing quality of care for acute myocardial infarction: shifting the focus of improvement from key indicators to process of care and tool use: the American College of Cardiology Acute Myocardial Infarction Guidelines Applied in Practice Project in Michigan: Flint and Saginaw Expansion. J Am Coll Cardiol. 2004;43:2166–2173. [DOI] [PubMed] [Google Scholar]
- 27. The impact of standardized stroke orders on adherence to best practices. Neurology. 2005;65:360–365. [DOI] [PubMed] [Google Scholar]
- 28. Reeves MJ, Broderick JP, Frankel M, et al. The Paul Coverdell National Acute Stroke Registry: initial results from four prototypes. Am J Prev Med. 2006;31(6 suppl 2):S202–S209. [DOI] [PubMed] [Google Scholar]
- 29. Stoeckle‐Roberts S, Reeves MJ, Jacobs BS, et al. Closing gaps between evidence‐based stroke care guidelines and practices with a collaborative quality improvement project. Jt Comm J Qual Patient Saf. 2006;32:517–527. [DOI] [PubMed] [Google Scholar]
- 30. George MG, Tong X, McGruder H, et al. Paul Coverdell National Acute Stroke Registry Surveillance—four states, 2005–2007. MMWR Surveill Summ. 2009;58:1–23. [PubMed] [Google Scholar]
- 31. Johnston KC, Li JY, Lyden PD, et al; RANTTAS Investigators. Medical and neurological complications of ischemic stroke: experience from the RANTTAS trial. Stroke. 1998;29:447–453. [DOI] [PubMed] [Google Scholar]
- 32. Prosser J, MacGregor L, Lees KR, et al. Predictors of early cardiac morbidity and mortality after ischemic stroke. Stroke. 2007;38:2295–2302. [DOI] [PubMed] [Google Scholar]
- 33. Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38:1655–1711. [DOI] [PubMed] [Google Scholar]
- 34. Roger VL, Go AS, Lloyd‐Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. [DOI] [PubMed] [Google Scholar]
- 37. Xian Y, Pan W, Peterson ED, et al. Are quality improvements associated with the Get With the Guidelines‐Coronary Artery Disease (GWTG‐CAD) program sustained over time? A longitudinal comparison of GWTG‐CAD hospitals versus non‐GWTG‐CAD hospitals. Am Heart J. 2010;159:207–214. [DOI] [PubMed] [Google Scholar]
- 38. Fonarow GC, Reeves MJ, Smith EE, et al. Characteristics, performance measures, and in‐hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines‐stroke. Circ Cardiovasc Qual Outcomes. 2010;3:291–302. [DOI] [PubMed] [Google Scholar]
- 39. Houston TK, Allison JJ, Person S, et al. Post‐myocardial infarction smoking cessation counseling: associations with immediate and late mortality in older Medicare patients. Am J Med. 2005;118:269–275. [DOI] [PubMed] [Google Scholar]
- 40. Brown DW, Croft JB, Schenck AP, et al. Inpatient smoking‐cessation counseling and all‐cause mortality among the elderly. Am J Prev Med. 2004;26:112–118. [DOI] [PubMed] [Google Scholar]
- 41. Van Spall HG, Chong A, Tu JV. Inpatient smoking‐cessation counseling and all‐cause mortality in patients with acute myocardial infarction. Am Heart J. 2007;154: 213–220. [DOI] [PubMed] [Google Scholar]
- 42. Reeves GR, Wang TY, Reid KJ, et al. Dissociation between hospital performance of the smoking cessation counseling quality metric and cessation outcomes after myocardial infarction. Arch Intern Med. 2008;168:2111–2117. [DOI] [PubMed] [Google Scholar]


