Abstract
Atrial fibrillation (AF) is the most common arrhythmia encountered by generalists and cardiologists alike. Much of the attendant morbidity from AF arises from systemic embolic complications which are effectively reduced with utilization of anti‐platelet and/or anticoagulant therapy. The systemic embolic complications of AF and the medical therapy to attenuate these risks are very well established. Through the course of this review, we aim to highlight the complex relationship between AF and other, “non‐embolic” outcomes. The presence of AF has been demonstrated to be associated with a 1.5 to 2‐fold increase in mortality across numerous observational cohorts. Still further, AF frequently coexists with heart failure, whether as a causative factor or a consequence of underlying structural heart disease or neurohumoral derangement, where its presence is associated with worse clinical outcomes. Whether AF is an independent risk factor for acute coronary syndromes (ACS) remains controversial, though its occurrence in patients with ACS has been shown to be associated with adverse outcomes both in observational cohorts as well as clinical trial populations. Individuals with AF have a 1.5 to 3‐fold increase in the rate of hospitalization and are at elevated risk for other arrhythmic disorders including both bradyarrhythmias as well as tachyarrhythmias. AF leads to considerable morbidity and mortality for patients and exacts a tremendous financial toll on the healthcare system—estimated to range from $6.0 to $26.0 billion. Given the current demographic transition in developed countries, the prevalence of AF will continue to increase and the need for refined approaches to risk stratification and pharmacotherapeutic interventions to attenuate the burden on patients will only become more important.
N.R. Desai and R.P. Giugliano received an honorarium through an educational grant from Sanofi Aventis for their time and expertise spent writing this article. R.P. Giugliano has also received research grant support and honoraria for CME lectures/consulting services from Daiichi‐Sankyo, Merck. He has also received honoraria for CME lectures from Bristol Myers Squibb.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia requiring medical attention. Its incidence and prevalence increase with advancing age, affecting nearly 10% of individuals age 80 years or older, and in the presence of concomitant cardiovascular (CV) disease.1 The estimated incremental costs of AF using current demographic data range from $6.0 to $26.0 billion.2 Much of the attendant morbidity from AF arises from systemic embolic complications that are effectively reduced with use of antiplatelet and/or anticoagulant therapy. In fact, well‐established risk‐stratification models exist to estimate embolic risk and enable patients and providers to make informed treatment decisions. However, in this review article we hope to synthesize information regarding the relationship between AF with other adverse outcomes, including mortality, heart failure (HF), acute coronary syndrome (ACS), other arrhythmias, and hospitalizations (Figure 1) and ask whether a global risk model can be created for patients with AF.
Figure 1.
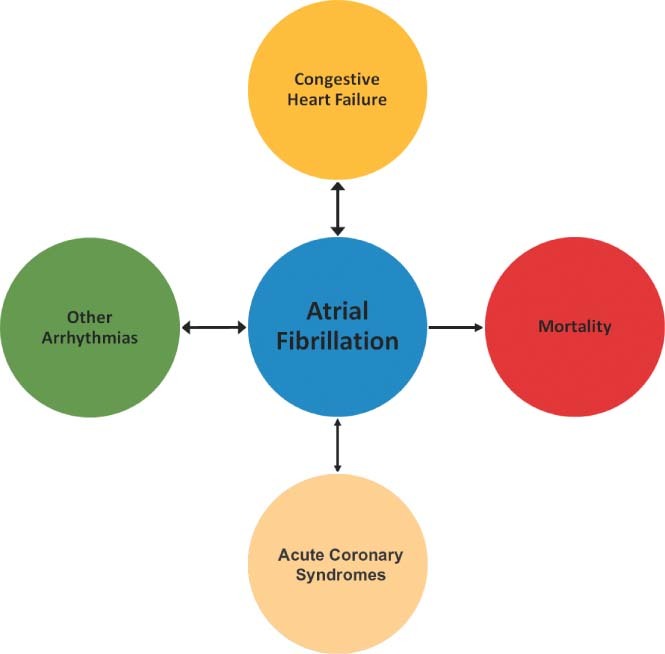
The relationship between atrial fibrillation with other adverse outcomes, including mortality, heart failure, acute coronary syndrome, other arrhythmias, and hospitalizations. The direction and size of the arrows is meant to convey the directional relationship and strength of association.
Mortality
The relationship between AF and increased mortality has been demonstrated in several large cohorts (Table 1). An analysis from the Framingham Heart Study, comparing 621 subjects who developed AF with those who did not, found that even after adjusting for the presence of associated CV diseases, AF was associated with nearly a 2‐fold increase in death for women and a 50% increase in death for men.3 This association was confirmed using data from the Renfrew/Paisley study, an observational cohort of over 15000 individuals from Scotland, where AF was found to be an independent predictor of all‐cause mortality for both women and men, with a relative risk of 2.2 and 1.5, respectively.4 Using data from 1993 through 2010 in the Women's Health Study, Conen et al found that not only was AF significantly associated with all‐cause mortality but also CV and non‐CV mortality.5 Contemporary clinical trials continue to highlight the risk of death that accompanies AF. Annualized event rates across different recent AF trial populations with varying risk factor profiles have ranged from 1.9% to 6.6% for all‐cause mortality and 1.5% to 3.1% for death from CV causes.6., 7., 8. Of note, findings from the AFFIRM (Atrial Fibrillation Follow‐Up Investigation of Rhythm Management) trial9 and the RACE (Rate Control versus Electrical Cardioversion for Persistent Atrial Fibrillation) trial10 demonstrated no difference in survival between patients managed with a rate‐control vs. rhythm‐control strategy. Finally, in the recently completed RACE‐II (Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II) study, which randomly assigned 614 patients with permanent AF to either a resting heart rate target of 110 (lenient) or 80 (strict) beats per minute, no difference was found in the rate of death from any cause at 3 years (5.6% vs 6.6%; hazard ratio [HR], 0.91; 90% confidence interval [CI]: 0.52–1.59).11
Table 1.
Relationship Between Atrial Fibrillation and Increased Mortality
| Study | Setting | Population | Endpoint | HR/OR (95% CI) |
|---|---|---|---|---|
| Framingham Heart Study | Longitudinal‐observational cohort | 5209 subjects | All‐cause mortality | 1.5 (1.2–1.8) for men; 1.9 (1.5–2.2) for women |
| Renfrew/Paisley study | Longitudinal‐observational cohort | 15 406 subjects | All‐cause mortality | 1.5 (1.2–2.2) for men; 2.2 (1.5–3.2) for women |
| Death or hospitalization | 1.8 (1.3–2.5) for men; 3.0 (2.1–4.2) for women | |||
| Heart failure | 3.4 (1.7–6.8) for men; 3.4 (1.9–6.2) for women | |||
| Women's Health study | Longitudinal‐observational cohort | 34 722 women | All‐cause mortality | 1.7 (1.3–2.2) |
| Cardiovascular mortality | 2.6 (1.6–4.1) | |||
| Noncardiovascular mortality | 1.4 (1.0–2.0) | |||
| SOLVDtrials | Randomized clinical trial | 6517 patients with NYHA class II or III heart failure | All‐cause mortality | 1.3 (1.1–1.6) |
| Death or hospitalization for heart failure | 1.3 (1.0–1.4) | |||
| CHARM program | Randomized clinical trial of candesartan vs placebo | 7599 patients with symptomatic heart failure | All‐cause mortality | 1.8 (1.5–2.2) for preserved ejection fraction; 1.4 (1.2–1.6) for reduced ejection fraction |
| Cardiovascular death or hospitalization for worsening heart failure | 1.7 (1.5–2.1) for preserved ejection fraction; 1.3 (1.1–1.5) for reduced ejection fraction | |||
| V‐HeFT trials | Randomized clinical trials of various vasodilators | 1427 patients with NYHA class II or III heart failure | All‐cause mortality | No significant difference |
| Hospitalizations of heart failure | No significant difference | |||
| GUSTO‐I trial | Randomized clinical trial of streptokinase vstPA | 40 891 patients with STEMI | In‐hospital mortality | 1.3 (1.2–1.4) |
| GUSTO‐III trial | Randomized clinical trial of reteplasevstPA | 13 858 patients with STEMI | In‐hospital mortality | 1.6 (1.3–2.0) |
| 1‐year mortality | 1.6 (1.3–2.0) | |||
| OPTIMAAL trial | Randomized clinical trial of losartan vs captopril | 5477 patients with STEMI and heart failure | In‐hospital mortality | 3.8 (2.0–7.4) |
| 30‐day mortality | 1.8 (1.4–2.4) | |||
| VALIANT trial | Randomized clinical trial of valsartan vs captopril vs both | 14 703 patients with STEMI and heart failure, LV dysfunction, or both | 3‐year mortality | 1.3 (1.2–1.5) |
Abbreviations: CHARM, Candesartan in Heart failure‐Assessment of Reduction in Mortality and morbidity program; CI, confidence interval; GUSTO, Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries; HR, hazard ratio; LV, left ventricular; NYHA, New York Heart Association; OPTIMAAL, Optimal Trial in Myocardial Infarction with the Angiotensin II Antagonist Losartan; OR, odds ratio; SOLVD, Studies of Left Ventricular Dysfunction Prevention and Treatment Trials; STEMI, ST‐elevation myocardial infarction; tPA, tissue plasminogen activator; VALIANT, Valsartan in Acute Myocardial Infarction; V‐HeFT, Vasodilator Heart Failure Trial.
Heart Failure (HF)
There is a well‐recognized association between AF and HF, and these 2 entities are inter‐related in a variety of ways. A significant burden of AF with rapid ventricular response can lead to left ventricular (LV) chamber dilation and systolic dysfunction, commonly referred to as tachycardia‐induced cardiomyopathy.12 In this instance, intensified rate control or a rhythm control strategy can lead to improvements in LV function.13 The incidence of tachycardia‐mediated cardiomyopathy and the mechanism underlying its development remain unclear but are thought, in part, to be related to disturbances in calcium handling, adrenergic receptor sensitivity, and depletion of cellular energy stores.14 In a Japanese study of 213 consecutive patients with coexistent HF and AF, tachycardia‐induced cardiomyopathy was the presumed etiology in 29% of cases.15
Beyond the direct causative relationship between AF and HF, the 2 conditions frequently coexist.The incidence of HF in patients with AF using data from 1470 subjects in the Framingham study was estimated at 3.3% per year.16 Moreover, AF was associated with a more than 3‐fold increase in the long‐term risk of HF in the Renfrew/Paisley observational study.4
In addition to these epidemiological connections between AF and HF, the presence of AF in patients with HF has been shown to be a poor prognostic factor. Among subjects with HF in the Framingham Heart Study, the development of AF was associated with a 1.6‐fold and 2.7‐fold increasein mortality for men and women, respectively.16 Mixed results have been noted in large clinical trials populations, with most supporting these observational data from Framingham. In the SOLVD (Studies of Left Ventricular Dysfunction) trials, among 6517 patients with both asymptomatic and symptomatic LV dysfunction, AF was associated with a 34% relative risk increase (95% CI: 1.12–1.62) in all‐cause mortality, a 42% increase in the risk of progressive pump‐failure death, and a 26% increase in the risk of death or hospitalizations for HF.17 Similarly, the presence of AF was associated with an increased risk of CV death, hospitalizations for worsening HF, and all‐cause mortality in the CHARM (Candesartan in Heart failure‐Assessment of Reduction in Mortality and Morbidity) trial across all ranges of ejection fraction (EF).18 Among patients with preserved EF, the presence of AF was associated with a relative risk of 1.72 (95% CI: 1.45–2.06) for CV death or hospitalization for HF and 1.80 (95% CI: 1.46–2.21) for all‐cause mortality. Similarly, among patients with depressed ventricular function, those with AF had a 29% relative risk increase in CV death and hospitalization for HF, and a 38% relative risk increase in all‐cause mortality. In contrast, experience from the Veterans Affairs Medical Center in patients with New York Hospital Association class II or III HF suggested that AF was not independently associated with adverse events.19
Acute Coronary Syndrome (ACS)
Whether AF is an independent risk factor for ACS remains a point of considerable controversy. Data from observational studies have not found a consistent association between AF and the risk of ACS. A retrospective analysis of over 800 patients found no significant difference in the rate of ACS for patients with AF and matched controls, 11.4% and 10.8% respectively.20 Results from contemporary clinical trials have shown that ACS and myocardial infarction (MI) are relatively infrequent events among patients with AF. In the 7554 patients enrolled in the ACTIVE‐A (Atrial Fibrillation Clopidogrel Trial with Irbesartan for Prevention of Vascular Events – Aspirin) trial, there were a total of 205 MIs, yielding an annualized event rate of <1%.6 Similar rates of MI were observed in the 6706 subjects in the ACTIVE‐W (Atrial Fibrillation Clopidogrel Trial with Irbesartan for Prevention of Vascular Events – Warfarin) trial, which compared oral anticoagulation with warfarin to dual antiplatelet therapy with aspirin and clopidogrel.21 Use of antiplatelet therapy may have attenuated the rates of ACS among ACTIVE trial participants. In the ATHENA (A Placebo‐Controlled, Double‐Blind, Parallel Arm Trial to Assess the Efficacy of Dronedarone 400 mg bid for the Prevention of Cardiovascular Hospitalization or Death from Any Cause in Patients with Atrial Fibrillation/Atrial Flutter) trial, which compared dronedarone with placebo, the cumulative rate of hospitalization for ACS was 2.7% in the active treatment arm and 3.8% in the placebo group.8
Although AF does not appear to be independently associated with ACS, its occurrence in patients with ACS has been shown to be associated with adverse outcomes. It is estimated that the overall incidence of AF postinfarction ranges from 5% to 20%.22 In the GUSTO‐I (Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries‐I) trial of 40 981 ST‐elevation myocardial infarction patients comparing 2 thrombolytic regimens, 7.9% developed AF during their hospitalization and had a significantly higher in‐hospital mortality and a 30% relative risk increase in the rate of 30‐day mortality after adjusting for differences in baseline covariates.23 This finding has been corroborated in other large ACS clinical trials, including GUSTO‐III24 and GISSI‐III (Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico‐III),25 where AF was associated with a relative risk increase of 1.63 and 1.98, respectively, in in‐hospital mortality but challenged by a longitudinal observational study of 4108 patients with acute MI (AMI), among whom AF was not found to be an independent risk factor for mortality.26 An analysis from the OPTIMAAL (Optimal Trial in Myocardial Infarction with the Angiotensin II Antagonist Losartan) trial of 5770 patients with AMI and LV dysfunction stratified patients by timing of AF—whether it was present on admission or developed during the hospitalization—and noted nearly a 4‐fold increase in 30‐day mortality in the latter group, with no association between AF and mortality in the former.27 Finally, an analysis from the EARLY ACS (Early Glycoprotein IIb/IIIa Inhibition in Non–ST‐Segment Elevation Acute Coronary Syndrome) trial of 9492 patients demonstrated that the 6% of subjects who developed in‐hospital AF within 7 days post ACS had a nearly 5‐fold higher risk for death between 7 and 30 days (HR, 4.83; 95% CI: 3.06–7.62).
There are also considerable data suggesting that AF is associated with worse long‐term mortality in post‐MI patients. Kinjo et al studied 2475 patients with AMI who underwent percutaneous coronary intervention and noted that 1‐year mortality was significantly increased in subjects who developed AF during their hospitalization (odds ratio [OR], 3.04; 95% CI: 1.40–7.48).28 Over the 3‐year follow‐up of the OPTIMAAL trial, patients with both AF at baseline and those with new‐onset AF had a significantly increased risk of mortality post‐AMI.27 In the VALIANT (Valsartan in Acute Myocardial Infarction) trial, a randomized study of angiotensin‐converting enzyme inhibitors andangiotensin receptor blockers in 14,703 patients with AMI and HF, there were 1812 subjects with new onset AF and 339 patients with a prior history of AF. Compared with subjects without AF, both new onset and prior AF were significantly associated with all‐cause mortality after adjusting for baseline differences.29 Finally, a retrospective examination of 3220 individuals post‐MI from Olmstead County, Minnesota found that AF any time after MI was associated with a 1.63 to 2.58 relative risk increase in the risk of death for AF within 30 days or after 30 days, respectively.30
Other Arrhythmias
Patients with AF can also develop other electrical disorders, both bradycardia, as part of the tachycardia‐bradycardia syndrome, and tachycardia, including ventricular tachycardia and ventricular fibrillation.The tachycardia‐bradycardia syndrome, a cardinal manifestation of sick sinus syndrome, refers to sinus node dysfunction leading to alternating atrial tachyarrhythmias and bradyarrhythmias. AF is the most common atrial arrhythmia, which coexists with significant symptomatic sinus pauses during AF conversion. Patients with tachycardia‐bradycardia syndrome are at increased risk for adverse CV events. A single‐center prospective study of 35 patients found that over 17 months of follow‐up, 57% had a CV event—23% syncope, 17% HF, 11% chronic AF, and 6% with a poorly tolerated tachyarrhythmia.31 Still further, such patients have a high likelihood of developing progressive sinus node dysfunction and high‐grade atrioventricular node block requiring implantation of a permanent pacemaker.32 In addition to the increased morbidity that these patients face, there is also significant mortality. After 33 months of follow‐up, 20% of the 2010 patients in MOST (Mode Selection trial) had died, with 35% of these from cardiac causes.33
AF has also been shown to be associated with ventricular tachycardia and ventricular fibrillation. The PROFIT (Prospective Analysis of Risk Factor for Appropriate ICD Therapy) trial of 250 patients found that in addition to depressed EF and QRS duration, AF was associated with a 1.8‐fold increase in the risk for ventricular tachycardia/ventricular fibrillation.34 In addition, it is estimated that up to 30% of patients with Wolff‐Parkinson‐White syndrome will develop AF, which may lead to unstable arrhythmias and CV collapse, particularly in the setting of being administered atrioventricular nodal blocking agents.35., 36.
Hospitalizations
Beside the impact of AF on mortality, the presence of AF has also been shown to be associated with increased rates of hospitalizations for a variety of reasons (eg, rapid ventricular response, embolic complications, HF). Using longitudinal administrative claims data, Kim et al noted that 37.5% of the 89 066 AF patients in the cohort were hospitalized as compared with 17.5% of matched non‐AF controls.2 In a 20‐year observational cohort from the United Kingdom, AF was associated with nearly a 2‐fold increase in the rate of CV hospitalization among men and more than a 3‐fold increase for women.4 Although the rates of hospitalization for CV causes observed in these population studies exceed those seen in clinical trials, the association between AF and hospitalizations has been clearly demonstrated in the latter. For instance, in the AVERROES (Apixaban versus Acetylsalicylic Acid to Prevent Strokes in Atrial Fibrillation Patients Who Have Failed or Are Unsuitable for Vitamin K Antagonist Treatment) trial, the annualized rate of hospitalization for CV causes was 12.6% in the apixaban arm and 15.9% in the placebo arm.7 Of the 4628 patients enrolled in the ATHENA trial, 1534 (33%) were hospitalized for CV events over 24 months, mostly consisting of hospitalizations related to AF.
Summary
AF is the most common arrhythmia encountered by generalists and cardiologists alike. It leads to considerable morbidity and mortality for patients and exacts a tremendous financial toll on the healthcare system. The systemic embolic complications of AF and the medical therapy to attenuate these risks are very well established. Estimating the risk of stroke and deciding on the appropriate antiplatelet or anticoagulant regimen have become routine in daily practice. Through the course of this review, we aimed to highlight the complex relationship between AF and other nonembolic outcomes. We examined the data linking AF with increased rates of mortality, HF, ACS, other arrhythmias, and hospitalization. The interplay between AF and each of these outcomes is quite complex, in some instances circumstantial, whereas in others it is causative or associative. The presence of AF is not only a marker of underlying structural heart disease, comorbid medical conditions, and electrical irritability, but also altered neurohormonal mediators and hemodynamic derangement. Developing a risk score for other events that is analogous to the CHADS2 or CHADS2‐VASC that exists for embolic events, would therefore be quite challenging. Still further, it remains to be seen whether an individual patient's score would have any specific therapeutic implication. For example, if a risk score were developed that could accurately predict the future risk of HF in patients with AF, how might that change the treatment of AF? Nonetheless, given the current demographic transition in developed countries, the prevalence of AF will continue to escalate and the need for refined approaches to risk stratification and pharmacotherapeutic interventions to attenuate the burden on patients will only become more important.
References
- 1. Wattigney WA, Mensah GA, Croft JB. Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 Through 1999. Circulation. 2003;108:711–716. [DOI] [PubMed] [Google Scholar]
- 2. Kim MH, Johnston SS, Chu BC, et al. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–320. [DOI] [PubMed] [Google Scholar]
- 3. Benjamin EJ, Wolf PA, D'Agostino RB, et al. Impact of atrial fibrillation on the risk of death: The Framingham Heart Study. Circulation. 1998;98:946–952. [DOI] [PubMed] [Google Scholar]
- 4. Stewart S. A population‐based study of the long‐term risks associated with atrial fibrillation: 20‐year follow‐up of the Renfrew/ Paisley study. Am J Med. 2002;113:359–364. [DOI] [PubMed] [Google Scholar]
- 5. Conen D, Chae CU, Glynn RJ, et al. Risk of death and cardiovascular events in initially healthy women with new‐onset atrial fibrillation. JAMA. 2011;305:2080–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Go AS. The ACTIVE Pursuit of Stroke Prevention in Patients with Atrial Fibrillation. N Engl J Med. 2009;360:2127–2129. [DOI] [PubMed] [Google Scholar]
- 7. Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364:806–817. [DOI] [PubMed] [Google Scholar]
- 8. Hohnloser SH, Crijns HJGM, van Eickels M, et al. Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med. 2009;360:668–378. [DOI] [PubMed] [Google Scholar]
- 9. Wyse DG, Waldo AL, DiMarco JP, et al. Atrial Fibrillation Follow‐up Investigation of Rhythm Management (AFFIRM) Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825–1833. [DOI] [PubMed] [Google Scholar]
- 10. Van Gelder IC, Hagens VE, Bosker HA, et al. Rate Control versus Electrical Cardioversion for Persistent Atrial Fibrillation Study Group. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002;347: 1834–1840. [DOI] [PubMed] [Google Scholar]
- 11. Van Gelder IC, Groenveld HF, Crijns HJGM, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363–1373. [DOI] [PubMed] [Google Scholar]
- 12. Redfield MM. Tachycardia‐related cardiomyopathy: a common cause of ventricular dysfunction in patients with atrial fibrillation referred for atrioventricular ablation. Mayo Clin Proc. 2000;75: 790–795. [DOI] [PubMed] [Google Scholar]
- 13. Kieny JR. Increase in radionuclide left ventricular ejection fraction after cardioversion of chronic atrial fibrillation in idiopathic dilated cardiomyopathy. Eur Heart J. 1992;13:1290–1295. [DOI] [PubMed] [Google Scholar]
- 14. Ohno M, Cheng CP, Little WC. Mechanism of altered patterns of left ventricular filling during the development of congestive heart failure. Circulation 1994;89:2241–2250. [DOI] [PubMed] [Google Scholar]
- 15. Fujino T, Yamashita T, Suzuki S, et al. Characteristics of congestive heart failure accompanied by atrial fibrillation with special reference to tachycardia‐induced cardiomyopathy. Circ J. 2007;71: 936–940. [DOI] [PubMed] [Google Scholar]
- 16. Wang TJ. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003;107:2920–2925. [DOI] [PubMed] [Google Scholar]
- 17. Dries DL. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: a retrospective analysis of the SOLVD trials. Studies of Left Ventricular Dysfunction. J Am CollCardiol. 1998;32:695–703. [DOI] [PubMed] [Google Scholar]
- 18. Olsson LG. Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure‐Assessment of Reduction in Mortality and morbidity (CHARM) program. J Am CollCardiol. 2006;47:1997–2004. [DOI] [PubMed] [Google Scholar]
- 19. Carson PE. The influence of atrial fibrillation on prognosis in mild to moderate heart failure. The V‐HeFT Studies. The V‐HeFT VA Cooperative Studies Group. Circulation. 1993;87:VI102–VI110. [PubMed] [Google Scholar]
- 20. Brown AM, Sease KL, Robey JL, et al. The risk for acute coronary syndrome associated with atrial fibrillation among ED patients with chest pain syndromes. Am J Emerg Med. 2007;25:523–528. [DOI] [PubMed] [Google Scholar]
- 21. ACTIVE Writing Group of the ACTIVE Investigators ; Connolly S, Pogue J, Hart R, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet. 2006;367:1903–1912. [DOI] [PubMed] [Google Scholar]
- 22. Schmitt J. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. EurHeart J. 2009;30:1038–1045. [DOI] [PubMed] [Google Scholar]
- 23. Crenshaw BS, Ward SR, Granger CB, et al. Atrial fibrillation in the setting of acute myocardial infarction: the GUSTO‐I experience. Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries. J Am CollCardiol. 1997;30:406–413. [DOI] [PubMed] [Google Scholar]
- 24. Wong CK, White HD, Wilcox RG, et al. New atrial fibrillation after acute myocardial infarction independently predicts death: the GUSTO‐III experience. Am Heart J. 2000;140:878–885. [DOI] [PubMed] [Google Scholar]
- 25. Pizzetti F, Turazza FM, Franzosi MG, et al. GISSI‐3 Investigators. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI‐3 data. Heart 2001;86:527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goldberg RJ, Seeley D, Becker RC, et al. Impact of atrial fibrillation on the in‐hospital and long‐term survival of patients with acute myocardial infarction: a community‐wide perspective. Am Heart J. 1990;119:996–1001. [DOI] [PubMed] [Google Scholar]
- 27. Lehto M, Snapinn S, Dickstein K, et al. Prognostic risk of atrial fibrillation in acute myocardial infarction complicated by left ventricular dysfunction: the OPTIMAAL experience. EurHeart J. 2005;26: 350–356. [DOI] [PubMed] [Google Scholar]
- 28. Kinjo K, Sato H, Ohnishi Y, et al. Prognostic significance of atrial fibrillation/atrial flutter in patients with acute myocardial infarction treated with percutaneous coronary intervention. Am J Cardiol. 2003;92:1150–1154. [DOI] [PubMed] [Google Scholar]
- 29. Kober L, Swedberg K, McMurray JJ, et al. Previously known and newly diagnosed atrial fibrillation: a major risk indicator after a myocardial infarction complicated by heart failure or left ventricular dysfunction. Eur J Heart Fail 2006;8:591–598. [DOI] [PubMed] [Google Scholar]
- 30. Jabre P, Jouven X, Adnet F, et al. Atrial fibrillation and death after myocardial infarction: a community study. Circulation. 2011;123: 2094–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Menozzi C, Brignole M, Alboni P, et al. The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome. Am J Cardiol. 1998;82:1205–1209. [DOI] [PubMed] [Google Scholar]
- 32. Kuga K, Yamaguchi I, Sugishita Y, et al. Assessment by autonomic blockade of age‐related changes of the sinus node function and autonomic regulation in sick sinus syndrome. Am J Cardiol. 1988; 61:361–366. [DOI] [PubMed] [Google Scholar]
- 33. Flaker G, Greenspon A, Tardiff B, et al. Death in patients with permanent pacemakers for sick sinus syndrome. Am Heart J. 2003; 146:887–893. [DOI] [PubMed] [Google Scholar]
- 34. Klein G, Lissel C, Fuchs AC, et al. Predictors of VT/VF‐occurrence in ICD patients: results from the PROFIT‐Study. Europace. 2006;8: 618–624. [DOI] [PubMed] [Google Scholar]
- 35. Sharma AD, Klein GJ, Guiraudon GM, et al. Atrial fibrillation in patients with Wolff‐Parkinson‐White syndrome: incidence after surgical ablation of the accessory pathway. Circulation. 1985;72: 161–169. [DOI] [PubMed] [Google Scholar]
- 36. Gulamhusein S, Ko P, Carruthers SG, et al. Acceleration of the ventricular response during atrial fibrillation in the Wolff‐Parkinson‐White syndrome after verapamil. Circulation. 1982;65: 348–354. [DOI] [PubMed] [Google Scholar]


