Abstract
Background:
Nonischemic dilated cardiomyopathy (DCM) is associated with high mortality and morbidity. Cardiovascular magnetic resonance allows for the noninvasive assessment of function, morphology, and myocardial edema. Activation of inflammatory pathways may play an important role in the etiology of chronic DCM and may also be involved in the disease progression.
Hypothesis:
The purpose of our study was to assess the incidence of myocardial edema as a marker for myocardial inflammation in patients with nonischemic DCM.
Methods:
We examined 31 consecutive patients ( mean age, 57 ± 12 years) with idiopathic DCM. Results were compared with 39 controls matched for gender and age (mean age, 53 ± 13 years). Parameters of left ventricular function and volumes, and electrocardiogram‐triggered, T2‐weighted, fast spin echo triple inversion recovery sequences were applied in all patients and controls. Variables between patients and controls were compared using t tests for quantitative and χ 2 tests for categorical variables.
Results:
Ejection fraction (EF) was 40.3 ± 7.8% in patients and 62.6 ± 5.0% in controls (P < 0.0001). In T2‐weighted images, patients with DCM had a significantly higher normalized global signal intensity ratio compared to controls (2.2 ± 0.6 and 1.8 ± 0.3, respectively, P = 0.0006), consistent with global myocardial edema. There was a significant but moderate negative correlation between signal intensity ratio in T2‐weighted images and EF (−0.39, P < 0.001).
Conclusions:
Evidence shows that myocardial edema is associated with idiopathic nonischemic DCM. Further studies are needed to assess the clinical and prognostic impact of these findings. Clin. Cardiol. 2012 DOI: 10.1002/clc.21979
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Dilated cardiomyopathy (DCM) is a significant cause of morbidity and mortality worldwide.1., 2. Noninvasive imaging plays a central role in the diagnosis, assessment of prognosis, and monitoring of therapy. Several reports have indicated an increased activation of inflammatory pathways in patients with idiopathic DCM, notably in the absence of systemic infection.3., 4., 5., 6. Furthermore, inflammation may affect disease progression4 and thus serves as a therapeutic target in heart failure.4., 5. Tissue edema is an integral component of inflammatory reaction in the myocardium and may exacerbate the extent of necrosis7 and interstitial fibrosis.8
Cardiovascular magnetic resonance (CMR) is a rapidly evolving technology increasingly used for noninvasive imaging of the expanding heart failure population. Tissue with a high content of protons bound to free water appears brighter on T2‐weighted images due to stronger signal intensity feedback from the protons.9., 10. Myocardial edema was introduced in the clinical setting as a specific marker for the acuity of myocardial injury in acute myocardial infarction.11., 12. It was shown to improve the diagnostic accuracy of a comprehensive CMR protocol in patients with acute coronary syndrome.13 Edema imaging is also useful in other cardiac diseases such as sarcoidosis, acute rejection following cardiac transplantation,14., 15. and stress‐induced cardiomyopathy.16., 17. Triple inversion breath hold sequence with short acquisition time (fast spin echo triple inversion recovery sequence [STIR]) is used in the clinical routine. These sequences have also demonstrated diagnostic value in patients with acute or chronic myocarditis.18., 19., 20., 21. Furthermore, CMR studies allow evaluation of cardiac morphology, function, flow, perfusion, and myocardial edema with a single examination.9., 22., 23. The purpose of our study was to assess the frequency, and if present, regional distribution of myocardial edema in patients with chronic nonischemic DCM.
Methods
Patients
We prospectively studied 33 consecutive patients with nonischemic DCM. These patients were compared to 39 age‐ and gender‐matched controls with normal left ventricular (LV) function and without any clinical evidence for cardiac disease. Patients and controls were examined by experienced cardiologists. Coronary artery disease was ruled out via coronary angiography in 29 patients, and via bicycle exercise tests, stress echocardiography, or adenosine stress perfusion CMR in 2 patients and in all controls. Both patients and controls underwent 12‐lead electrocardiogram (ECG) and transthoracic echocardiography, and the controls took a noninvasive stress test (bicycle exercise and/or dynamic stress echocardiography or adenosine CMR examination).
Inclusion criteria for the patients were an LV ejection fraction <50% for at least 6 months and no underlying coronary heart disease. Patients were excluded if they had coronary artery disease (stenosis of ≥50% of 1 or more coronary arteries), congenital heart disease, LV hypertrophy (diameter of the septum or inferior wall ≥11 mm), clinical evidence of acute myocardial disease (clinical suspicion of acute myo/pericarditis, symptoms of recent respiratory or gastrointestinal viral illness, ECG changes consistent with myopericarditis, or elevated biomarkers and inflammation markers indicative of recent myocardial injury or infection), or acute cardiac failure, significant valvular regurgitation (≥degree 2 on echocardiography and CMR), valvular stenosis, renal failure (creatinine ≥1.8 mg/dL), or a known history of claustrophobia. All patients and controls gave written informed consent and the study was approved by the local ethics board. One patient experienced claustrophobia during the CMR examination, and the STIR image quality in another was insufficient. Our final cohort thus comprised 31 patients whom we compared to 39 age‐ and sex‐matched controls without structural heart disease.
Cardiovascular Magnetic Resonance Imaging
All images were acquired on a 1.5 T magnetic resonance system (Intera CV 1.5T; Phillips Medical Systems, Best, The Netherlands) using built‐in software (release 11). We used a 5‐element cardiac phased‐array coil combined with a homogeneity correction algorithm (Constant Level AppeaRance). This algorithm generates sensitivity maps for each synergy coil element (relative to the body coil sensitivity) to calculate uniformity correction.24 Data acquisition was ECG‐triggered.
Functional and morphological data were evaluated using the 6.5 view forum (Philips Medical Systems). Regions of interest were drawn manually. To evaluate LV function and dimensions, we took 2‐, 3‐, and 4‐chamber long‐axis views and 3‐dimensional (3D) short‐axis volume data assessed by steady‐state free precession imaging (field of view, 350 mm; matrix, 256 × 256; echo time, 1.6 ms; repetition time, 4.0 ms; flip angle, 60°; slice thickness, 10 mm; no gap). Phase‐contrast velocity images in the ascending aorta were obtained to measure stroke volume and rule out significant aortic insufficiency. ECG‐triggered, T2‐weighted, STIR sequences in a short‐axis view covering the whole left ventricle (7–9 acquisitions; field of view, 350 mm; matrix size, 512 × 512; flip angle, 90°; slice thickness, 10 mm; no gap; echo time, 100 ms; TR (repetition time), 2) were performed in all patients and controls. We measured the signal intensity in the myocardial wall and in skeletal muscle. Five to 10 regions of interest were drawn into the septum, anterior, lateral, and inferior wall of the myocardium and the regional and global intensity obtained. In addition, 5 to 10 regions of interests were drawn into the skeletal muscles (erector spinae muscle or lattissimus dorsi) with homogenous signal. The size of each region of interest (ROI) was standardized 60 to 70 mm 2 . We then calculated the averages of the septal, anterior, lateral, and inferior ROIs and of the muscle ROIs. The relative myocardial signal intensity was calculated by the ratio of myocardial signal intensity and muscle signal intensity.
As a result of our previous studies the cutoff value of an elevated ratio of signal intensity in STIR images between myocardial and skeletal muscle was fixed to 2.1.18., 24. Late gadolinium enhancement (LGE) imaging was obtained in all patients and controls 10 minutes after intravenous administration of 0.2 mmol/kg gadolinium using 3D inversion recovery turbo gradient echo sequences as previously reported.24
Statistical Analysis
Data are presented as mean and standard deviation for quantitative variables and as absolute and relative frequencies for categorical variables. Variables between patients and controls were compared using t tests for quantitative and χ 2 tests for categorical variables. Correlations between quantitative patient characteristics were estimated by means of Pearson correlation coefficient (r). All tests were 2‐sided and used 0.05 to indicate statistical significance. Statistical analysis took place using SAS software version 9 (SAS Institute Inc., Cary, NC).
Results
Patient Characteristics
Patient and control baseline characteristics are shown in Table 1. The control group did not differ regarding age and gender. Seven patients had moderately elevated blood pressure values; however, none of them revealed an increased LV mass. Nine patients were in New York Heart Association (NYHA) class I, 15 in class II, and 7 in class III. Mean NYHA class was 1.8 ± 0.9. Mean B‐type natriuretic peptide (BNP) levels were 119 pg/ml (range, 8–457 pg/mL). All patients had an end‐diastolic LV diameter of 53 mm and larger, and 90% of the patients had ≥55 mm.
Table 1.
Clinical Characteristics of the Patients and Controls
| Variables | Patients, n = 31 | Controls, n = 39 | P |
|---|---|---|---|
| Mean age, y | 56.9 ± 12.2 | 52.9 ± 13.3 | 0.24 |
| Female, no. (%) | 5 (16) | 13 (33) | 0.16 |
| Height, cm | 172.4 ± 5.3 | 176 ± 11.2 | 0.22 |
| Weight, kg | 80.1 ± 16.6 | 80.8 ± 17.4 | 0.92 |
| Systolic blood pressure, mm Hg | 134.9 ± 20.9 | 129.1 ± 16.0 | 0.33 |
| Diastolic blood pressure, mm Hg | 79.3 ± 13.8 | 74.1 ± 8.7 | 0.17 |
| NYHA I, no. | 10 | 0 | |
| NYHA II, no. | 14 | 0 | |
| NYHA III, no. | 7 | 0 |
Abbreviations: NYHA, New York Heart Association.
Values are expressed as mean ± standard deviation unless indicated otherwise.
Functional Parameters
Results for functional data are listed in Table 2. Patients had significantly lower LV ejection fractions than controls. LV end‐diastolic volumes and LV end‐diastolic diameters were greater in patients than in controls. Stroke volume and cardiac output did not significantly differ between patients and controls.
Table 2.
Magnetic Resonance Functional Measurements in Patients and Controls
| Variables | Patients, n = 31 | Controls, n = 39 | P |
|---|---|---|---|
| Heart rate, beats/min | 73.5 ± 14.9 | 73.6 ± 11.4 | 0.98 |
| LV ejection fraction, % | 40.3 ± 7.8 | 62.6 ± 5.0 | <0.0001 |
| LV stroke volume, mL | 90.5 ± 18.0 | 97.5 ± 20.3 | 0.14 |
| LV end‐diastolic volume, mL | 228.9 ± 71.5 | 157.3 ± 43.0 | <0.0001 |
| LV end‐diastolic diameter, mm | 62.4 ± 6.4 | 51.9 ± 4.0 | <0.0001 |
| Cardiac output, L/min | 6.5 ± 1.3 | 6.9 ± 1.5 | 0.26 |
Abbreviations: LV, left ventricular.
Values are expressed as mean ± standard deviation.
Assessment of Myocardial Edema
We observed a highly significant difference in global myocardial signal intensity between patients and controls (645 ± 128 vs 534 ± 89, P = 0.001). The ratio of signal intensity between myocardial and skeletal muscle differed between groups as well. In addition, signal intensities ratios in T2‐weighted images of the septum, anterior, lateral, and inferior walls differed from controls (Table 3).
Table 3.
Magnetic Resonance Measurements of Edema in Patients and Controls
| Variables | Patients, n = 31 | Controls, n = 39 | P |
|---|---|---|---|
| STIR myocardium/skeletal muscle | 2.2 ± 0.6 | 1.8 ± 0.3 | 0.0006 |
| STIR septum/skeletal muscle | 2.2 ± 0.5 | 1.9 ± 0.3 | 0.001 |
| STIR anterior wall/skeletal muscle | 2.1 ± 0.6 | 1.8 ± 0.3 | 0.003 |
| STIR lateral wall/skeletal muscle | 2.3 ± 0.7 | 1.9 ± 0.3 | <0.0001 |
| STIR inferior wall/skeletal muscle | 2.4 ± 0.6 | 1.9 ± 0.4 | 0.002 |
Abbreviations: STIR, fast spin echo triple inversion recovery sequence.
Values are expressed as mean ± standard deviation.
Sixteen of 31 patients (52%) had an increased signal intensity ratio in T2‐weighted images (>2.1), consistent with global myocardial edema. No patient had acute myocardial infarction, acute rejection following cardiac transplantation, or sarcoidosis, which are associated with elevated T2 signal. Mean age was 55.0 ± 15.2 years (with edema) and 59.7 ± 9.3 years (without edema) (P = 0.32). Two patients were female with edema and 3 without. NYHA class was 7 vs 2 (NYHA I), 5 vs 10 (NYHA II), and 4 vs 3 (NYHA III), edema vs no edema. BNP values were 103 ± 127 pg/mL and 142 ± 163, P = 0.61. Three patients in each group had decompensated heart failure 6 to 12 months prior to the study. During examination the patients were in stable conditions. Blood pressure was not different between patients with and without edema (Table 4). There was a significant difference in global relative enhancement (2.5 ± 0.6 vs 1.9 ± 0.2, P < 0.001) between patients with and without edema and in the relative enhancement of the septum (2.5 ± 0.6 vs 1.9 ± 0.3, P = 0.002), anterior (2.4 ± 0.7 vs 1.8 ± 0.2, P = 0.001), lateral (2.7 ± 0.7 vs 1.9 ± 0.2, P = 0.001), and inferior wall (2.7 ± 0.7 vs 2.0 ± 0.2, P = 0.001) (Figs 1, 2).
Table 4.
Clinical Characteristics of the Patients With and Without Edema
| Variables | Edema, n = 16 | Without Edema, n = 15 | P |
|---|---|---|---|
| Mean age, y | 55.0 ± 15.2 | 59.7 ± 9.3 | 0.32 |
| Female, no. (%) | 2 (13) | 3 (20) | 0.64 |
| Height, cm | 172.5 ± 3.5 | 173.0 ± 5.0 | 0.90 |
| Weight, kg | 82.5 ± 24.7 | 88.8 ± 18.0 | 0.70 |
| Systolic blood pressure, mm Hg | 136.0 ± 18.2 | 140.3 ± 22.5 | 0.31 |
| Diastolic blood pressure, mm Hg | 77.8 ± 16.3 | 82.9 ± 13.4 | 0.13 |
| NYHA I, no. | 7 | 2 | |
| NYHA II, no. | 5 | 10 | |
| NYHA III, no. | 4 | 3 |
Abbreviations: NYHA, New York Heart Association.
Values are expressed as mean ± standard deviation unless indicated otherwise.
Figure 1.
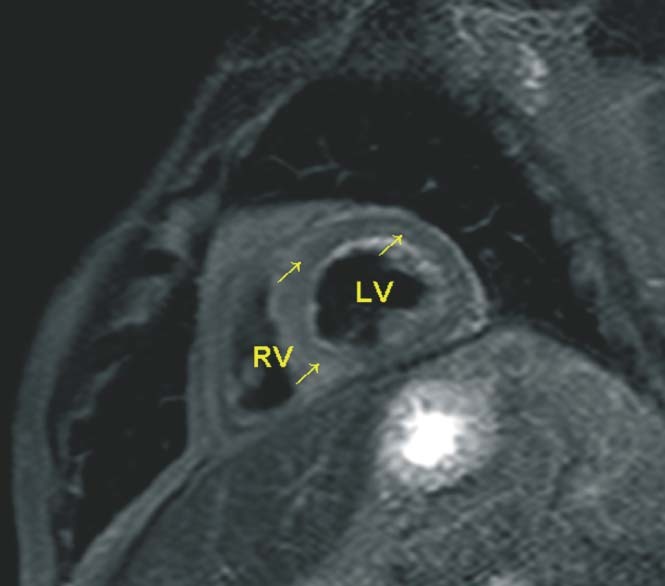
An example of T2‐weighted (fast spin echo triple inversion recovery sequence) image of a 51‐year‐old male with reduced function (left ventricular ejection fraction 34%) and enhanced signal intensity of the myocardium of the left ventricle. This provides evidence of myocardial edema. The arrows signify elevated signal intensity of the myocardium. Abbreviations: LV, left ventricle; RV, right ventricle.
Figure 2.
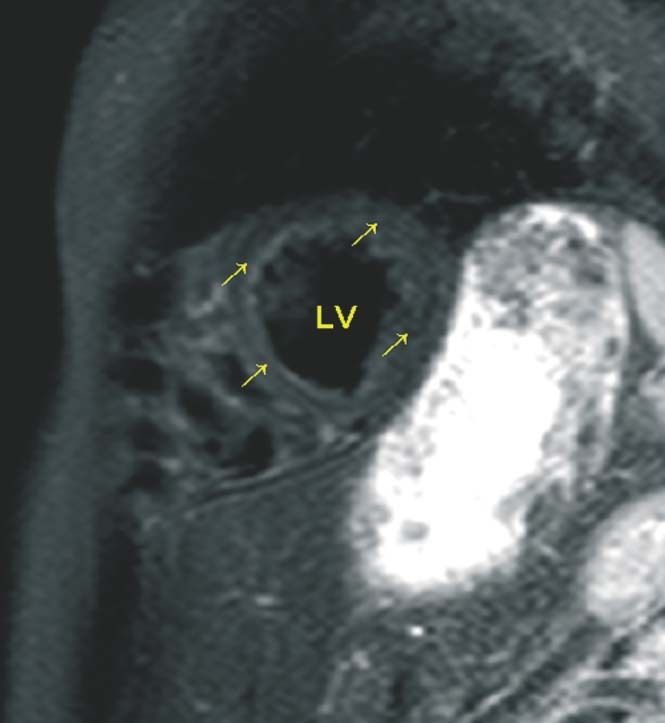
A 47‐year‐old female control with normal signal of the myocardium (arrows). Abbreviations: LV, left ventricle.
There was a significant but moderate negative correlation between signal intensity ratio in T2‐weighted images and ejection fraction (EF) (−0.39, P < 0.001). We evaluated a relationship between the increased relative signal intensity measurement and NYHA functional class. There was no difference between patients with elevated and normal T2 values and NYHA class (1.9 ± 0.8 vs 2.1 ± 0.6, P = not significant).There were no significant correlations to stroke volume (−0.23, P = 0.057), end‐diastolic volume (+0.16, P = 0.18), cardiac output (−0.14, P = 0.25), and LV end‐diastolic diameter (+0.11, P = 0.34).
Myocardial Contrast Enhancement (LGE)
In 21 of 31 patients (68%), we found small midmyocardial or subepicardial enhancing lesions. No patient had subendocardial or transmural scars as would be typical for coronary artery disease. There was no correlation between contrast enhancement and T2 (STIR) measurements. The global STIR/muscle ratio of patients without LGE was 2.17 ± 0.15 and with LGE 2.26 ± 0.73, P = 0.70. In patients with elevated STIR, we predominantly found a global elevated pattern. Thus, there was no correlation with regional STIR values and the location of LGE.
Discussion
In patients with nonischemic DCM we found evidence for global myocardial edema, which was correlated with global systolic dysfunction. Noninvasive imaging plays a central role in the diagnosis of DCM, in the determination of etiology and prognosis, as well as in monitoring therapeutic effects. An increased myocardial signal intensity in T2‐weighted CMR images has been repeatedly associated with acute myocardial injury or acute inflammation as it reflects elevated intramyocardial free water content.11., 12., 13. We observed that patients with idiopathic DCM presented an increased myocardial T2 signal that might represent ongoing myocardial inflammation that must be further addressed by biopsy studies. This may have significant therapeutic and prognostic implications, because knowledge of the etiology of cardiac dysfunction in patients with heart failure impacts management and prognosis,25 yet is not identified in 50% of patients with DCM.25., 26. Recent data suggest that many patients may be suffering from chronic myocardial inflammation due to persistent viral replication or autoimmune activation after a viral infection.3., 25. Specific noninvasive tests for myocardial inflammation, however, have not been used in clinical settings. In the present study we found a significantly increased native and normalized signal intensity in T2‐weighted CMR images in patients compared to controls. Moreover, we observed that this finding was moderately associated with lower EF. This new finding might be related to the known impact of edema itself on LV function.7., 8.
A substantial proportion (10%–34%) of patients with DCM may in fact suffer from viral myocarditis,27 and a substantial portion of patients with myocarditis and DCM represent different stages of an organ‐specific autoimmune disease in genetically predisposed individuals.28., 29. CMR is considered an important diagnostic tool for myocarditis,21., 23. and an increased signal in T2‐weighted images is a typical finding in patients with acute myocarditis.18., 19., 20., 24. Importantly, in uncomplicated acute myocarditis, the signal normalizes over time,30 but signal abnormalities may persist in chronic myocarditis. Gutberlet et al21 also observed an elevated T2 ratio in 25 of 83 patients with suspected chronic myocarditis. T2 signals have not been examined routinely so far in patients with DCM. Thus, our new findings may reinforce the notion of chronic myocarditis as a possible cause of DCM in some patients.
There are reports of an increased inflammatory activation in patients with idiopathic DCM and no systemic infection.3., 4., 5., 6. The observation that about 50% of our patients had evidence for global myocardial edema may indicate a different pathophysiologic situation such as chronic inflammation. This is in line with reports of chronic inflammation in 30% to 60% of patients with DCM.4., 5., 6. Larger and longitudinal studies with endomyocardial biopsies from patients with DCM are warranted to extrapolate on our preliminary findings and evaluate their diagnostic impact.
About two‐thirds of our patients had small midmyocardial or subepicardial lesions of contrast enhancement. No patient had subendocardial or transmural scars as would be typical for coronary artery disease. There was no correlation between contrast enhancement and measurements of myocardial edema, indicating that edema may not necessarily be related to irreversible injury. In addition, there was no correlation with regional STIR values and the location of LGE. Myocardial LGE in DCM could indicate focal replacement fibrosis, and although the mechanisms underlying this have not yet been elucidated, a potential factor may be myocardial inflammation. The absence of a correlation between LGE and T2 measurements found in our study could be due to the fact that we found a more global elevated T2 pattern indicating global edema in these patients.
An increased myocardial signal intensity in T2‐weighted CMR images (STIR) has been used to detect edema in acute myocardial infarction, acute rejection following cardiac transplantation, and sarcoidosis.11., 12., 14., 15. These diseases were excluded by patient selection criteria. Undetectable small vessel ischemia would be another possibility for increased myocardial intensity, but it is unlikely in our patients because coronary artery disease was ruled out.
In a recent study by Voigt et al,31 23 adults with chronic DCM were examined by CMR and endomyocardial biopsy. Myocardial inflammation was confirmed by immunohistology using the Lake Louise Criteria in 12 patients (52.2%). They found a high sensitivity, specificity, and diagnostic accuracy of CMR to detect immunohistologically confirmed myocardial inflammation. Thus, there is a good agreement between that study and our results regarding the frequency of patients with DCM and myocardial edema: 52% in both studies. Both studies confirm that CMR is a promising tool for assessment of myocardial inflammation in patients with DCM.
Clinical Implications
Despite impressive medical advances, heart failure is still a significant cause of morbidity and mortality worldwide.1., 2. Chronic idiopathic DCM is 1 of the main underlying diseases; yet, its pathophysiology and especially determinants of progression and remodeling are not thoroughly understood.32 Ongoing inflammatory processes may play an important role in the course of the disease; therefore, the noninvasive assessment of global myocardial edema as a diagnostic marker for inflammation may provide very useful information for a better understanding and management of these patients.9 Although precise mechanisms of how edema affects function, long‐term tissue composition, and prognoses of the patients with DCM are to be elucidated further, it is known that increased stiffness and the reduced compliance of edematous myocardium affect diastolic and systolic function.9 Changes in intramyocardial pressure, and a high protein content of edema may promote myocardial fibrosis,8 which is extensive in patients with DCM.33., 34.
Limitations
Our sample size is limited, and therefore our study may not have been powered to detect relationships of edema to clinical markers such as the severity of heart failure (NYHA class functional status). We did not perform biopsies to corroborate our results by ultrastructural and/or histological data. Biopsy data, however, reflect regional but not global changes and therefore are limited in their generalization. Patients with heart failure and controls had similar cardiac output and were clinically stable, suggesting that the patients had relatively mild disease. The mean NYHA class was 1.8, thus our findings cannot be extrapolated to patients with more severe disease or unstable conditions.
Conclusion
Our study indicates that patients with nonischemic DCM have evidence for global myocardial edema, which was related to systolic dysfunction. This may reflect inflammatory activity. Further studies are needed to assess the clinical and prognostic impact of these findings.
Acknowledgements
We would like to thank Petra Nuss for collecting the data and typing parts of the manuscript, and Carole Cürten for proofreading.
References
- 1. Nieminen MS, Harjola VP. Definition and epidemiology of acute heart failure syndromes. Am J Cardiol. 2005;19:5G–10G. [DOI] [PubMed] [Google Scholar]
- 2. Dayer M, Cowie MR. Heart failure: diagnosis and health care burden. Clin Med. 2004;4:13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sampietro T, Neglia D, Bionda A, et al. Inflammatory markers and serum lipids in idiopathic dilated cardiomyopathy. Am J Cardiol. 2005;96:1718–1720. [DOI] [PubMed] [Google Scholar]
- 4. Heymans S, Hirsch E, Anker SD, et al. Inflammation as a therapeutic target in heart failure? A scientific statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Failure. 2009;11:119–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Noutsias M, Pauschinger M, Poller WC, et al. Current insights into the pathogenesis, diagnosis and therapy of inflammatory cardiomyopathy. Heart Fail Monit. 2003;3:127–135. [PubMed] [Google Scholar]
- 6. Kuhl U, Noutsias M, Seeberg B, et al. Immunohistological evidence for a chronic intramyocardial inflammatory process in dilated cardiomyopathy. Heart. 1996;75:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. DiBona , DR , Powell WJ Jr. Quantitative correlation between cell swelling and necrosis in myocardial ischemia in dogs. Circ Res. 1980;47:653–665. [DOI] [PubMed] [Google Scholar]
- 8. Laine GA, Allen SJ. Left ventricular myocardial edema. Lymph flow, interstitial fibrosis, and cardiac function. Circ Res. 1991;68:1713–1721. [DOI] [PubMed] [Google Scholar]
- 9. Friedrich MG. Myocardial edema–a new clinical entity? Nat Rev Cardiol. 2010;7:292–296. [DOI] [PubMed] [Google Scholar]
- 10. Abdel‐Aty H, Simonetti O, Friedrich MG. T2‐weighted cardiovascular magnetic resonance imaging. Magn Reson Imaging. 2007;26:452–459. [DOI] [PubMed] [Google Scholar]
- 11. Abdel‐Aty H, Zagrosek A, Schulz‐Menger J, et al. Delayed enhancement and T2‐weighted cardiovascular magnetic resonance imaging differentiate acute from chronic myocardial infarction. Circulation. 2004;109:2411–2416. [DOI] [PubMed] [Google Scholar]
- 12. Berry C, Kellman P, Mancini C, et al. Magnetic resonance imaging delineates the ischemic area at risk and myocardial salvage in patients with acute myocardial infarction. Circ Cardiovasc Imaging. 2010;3:527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cury , RC , Shash K, Nagurney JT, et al. Cardiac magnetic resonance with T2‐weighted imaging improves detection of patients with acute coronary syndrome in the emergency department. Circulation. 2008;118:837–844. [DOI] [PubMed] [Google Scholar]
- 14. Vignaux O, Dhote R, Duboc D, et al. Clinical significance of myocardial magnetic resonance abnormalities in patients with sarcoidosis: a 1‐year follow‐up study. Chest. 202;122: 1895–1901. [DOI] [PubMed] [Google Scholar]
- 15. Marie PY, Angioi M, Carteaux JP, et al. Detection and prediction of acute heart transplant rejection with the myocardial T2 determination provided by a black‐blood magnetic resonance imaging sequence. J Am Coll Cardiol. 2001;37:825–831. [DOI] [PubMed] [Google Scholar]
- 16. Muellerleile K, Lund G, Groth M, et al. Delayed‐enhancement magnetic resonance imaging in patients with clinically suspected stress cardiomyopathy (Tako‐tsubo). Rofo. 2010;182: 29–35. [DOI] [PubMed] [Google Scholar]
- 17. Abdel‐Aty H, Cocker M, Friedrich MG. Myocardial edema is a feature of Tako‐Tsubo cardiomyopathy and is related to the severity of systolic dysfunction: insights from T2‐weighted cardiovascular magnetic resonance. Int J Cardiol. 2009;132:291–293. [DOI] [PubMed] [Google Scholar]
- 18. Jeserich M, Olschewski M, Bley TH, et al. Cardiac involvement after respiratory tract viral infection—detection by cardiac magnetic resonance. J Comput Assist Tomogr. 2009;33:15–19. [DOI] [PubMed] [Google Scholar]
- 19. Abdel‐Aty H, Boye P, Zagrosek A, et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005;45:1815–1822. [DOI] [PubMed] [Google Scholar]
- 20. Assomull RG, Lyne JC, Keenan N, et al. The role of cardiovascular magnetic resonance in patients presenting with chest pain, raised troponin and unobstructed coronary arteries. Eur Heart J. 2007;28:1242–1249. [DOI] [PubMed] [Google Scholar]
- 21. Gutberlet M, Spors B, Thoma T, et al. Suspected chronic myocarditis at cardiac MR: diagnostic accuracy and association with immunohistologically detected inflammation and viral persistence. Radiology. 2008;246:401–409. [DOI] [PubMed] [Google Scholar]
- 22. White JA, Patel MR. The role of cardiovascular MRI in heart failure and the cardiomyopathies. Cardiol Clin. 2007;25:71–95, vi. [DOI] [PubMed] [Google Scholar]
- 23. Friedrich MG, Sechtem U, Holmvang G, et al; International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol. 2009;53:1475–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jeserich M, Konstantinides S, Olschewski M, et al. Diagnosis of early myocarditis after respiratory or gastrointestinal tract viral infection: insights from cardiovascular magnetic resonance. Clin Res Cardiol. 2010;99:707–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long‐term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342:1077–1084. [DOI] [PubMed] [Google Scholar]
- 26. Dec GW Jr, Palacios IF, Fallon JT, et al. Active myocarditis in the spectrum of acute dilated cardiomyopathies: clinical features, histologic correlates, and clinical outcome. N Engl J Med. 1985;312:885–890. [DOI] [PubMed] [Google Scholar]
- 27. Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000;343:1388–1398. [DOI] [PubMed] [Google Scholar]
- 28. Spotnitz MD, Lesch M. Idiopathic dilated cardiomyopathy as a late complication of healed viral (Coxsackie B virus) myocarditis: historical analysis, review of the literature, and a postulated unifying hypothesis. Prog Cardiovasc Dis. 2006;49:42–57. [DOI] [PubMed] [Google Scholar]
- 29. Caforio AL, Iliceto S. Genetically determined myocarditis: clinical presentation and immunological characteristics. Curr Opin Cardiol. 2008;23:219–226. [DOI] [PubMed] [Google Scholar]
- 30. Zagrosk A, Wassmuth R, Abdel‐Aty H, et al. Relation between myocardial edema and myocardial mass during the acute and convalescent phase of myocarditis—a CMR study. J Cardiovasc Magn Reson. 2008;10:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Voigt A, Elgeti T, Durmus T, et al. Cardiac magnetic resonance imaging in dilated cardiomyopathy in adults—towards identification of myocardial inflammation. Eur Radiol. 2011;21:925–935. [DOI] [PubMed] [Google Scholar]
- 32. Tang WH. The year in heart failure. J Am Coll Cardiol. 2010;55:688–696. [DOI] [PubMed] [Google Scholar]
- 33. Unverferth DV, Baker PB, Swift SE, et al. Extent of myocardial fibrosis and cellular hypertrophy in dilated cardiomyopathy. Am J Cardiol. 1986;57:816–820. [DOI] [PubMed] [Google Scholar]
- 34. Roberts WC, Siegel RJ, McManus BM. Idiopathic dilated cardiomyopathy: analysis of 152 necropsy patients. Am J Cardiol. 1987;60:1340–1355. [DOI] [PubMed] [Google Scholar]


