Abstract
Background:
Optimal revascularization strategy is still under debate in patients with coronary artery disease, particularly due to the results of the Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery (SYNTAX) trial. Although medical prevention has been clearly shown to be beneficial in coronary artery disease, it has been suggested that patients were significantly undertreated with evidence‐based medications for cardiovascular protection.
Hypothesis:
The purpose of the study was to evaluate concomitant medical treatment in cardiovascular interventional head‐to‐head trials comparing coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI).
Methods:
A systematic search of the literature regarding documentation and reports of medical treatment in cardiovascular interventional head‐to‐head trials with more than 500 patients comparing CABG and PCI was performed.
Results:
Systematic research of the literature identified 2106 articles of potential interest. After review and selection, only 3 trials reported on medical treatment. Baseline medication was reported in the RITA (Randomized Intervention Treatment of Angina), CABRI (Coronary Angioplasty versus Bypass Revascularisation Investigation), and SYNTAX trials, and follow‐up data were provided by the CABRI and SYNTAX 3‐year trials only.
Conclusions:
Poor reporting of medical treatment at discharge might reflect an underestimation of secondary prevention in patients undergoing cardiac surgery or interventional procedures in head‐to‐head interventional trials. Thus, discussion of optimal revascularization procedure has to remain open, even in terms of concomitant medical treatment of patients.
Additional Supporting Information may be found in the online version of this article.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
The benefits of medical treatment for secondary prevention have been clearly demonstrated in patients with coronary artery disease, but optimal revascularization strategy is still under debate, particularly due to the results of the SYNTAX (Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery) trial.1 However, in SYNTAX, coronary artery bypass grafting (CABG) patients compared to percutaneous coronary intervention (PCI) patients were significantly undertreated with evidence‐based medications for cardiovascular protection. Thus, the short outcome limits the interpretation for long‐term outcome judgment in cardiovascular high‐risk patients. Therefore, a systematic search of the literature regarding concomitant medical treatment in cardiovascular interventional head‐to‐head trials comparing CABG and PCI was conducted by 2 independent reviewers.
Methods
MEDLINE and Embase databases were searched for studies by using the following terms: “coronary” and “angioplasty” in combination with “coronary artery bypass surgery” and “randomized controlled trial.” Selection of references was performed in 2 steps. First, abstracts were excluded if they were about nonhuman data, letters, reviews, case reports, in a language other than English, trials with <500 patients in both treatment arms, or trials with an additional medical treatment arm. Second, articles without information on recommended medical treatment for cardiovascular secondary prevention such as statins, angiotensin‐converting enzyme (ACE) inhibitors or angiotensin‐receptor blockers (ARBs), β‐blockers, and platelet inhibitors were also excluded. Trials without a prospective design or randomization were not included. Conflicts between reviewers were resolved through discussion and rereview.
Results
Systematic research of the literature identified 2106 articles (Figure 1) of potential interest. After the first selection step, 118 articles remained. References for these articles are shown in the online supplement. Further selection excluded another 115 articles, of which 91 had to be excluded due to missing information on medical drug treatment. Only 3 of the 2106 trials reported medical treatment.
Figure 1.
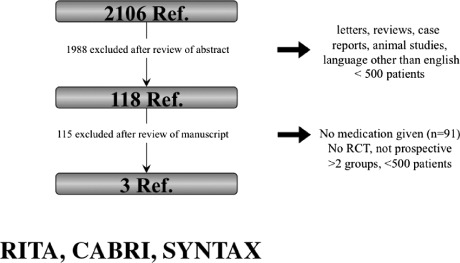
Systematic search of literature regarding concomitant medical treatment in cardiovascular interventional trials. Abbreviations: CABRI, Coronary Angioplasty versus Bypass Revascularisation Investigation trial; RCT, randomized controlled trial; Ref, references; RITA, Randomized Intervention Treatment of Angina trial; SYNTAX, Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery trial.
The Randomized Intervention Treatment of Angina (RITA) trial published in 1988 included 1011 patients, reported baseline medication (platelet inhibitors and β‐blockers) without a significant intergroup difference.2 The Coronary Angioplasty versus Bypass Revascularisation Investigation (CABRI) trial enrolled 1054 patients between 1988 and 1992. Medical treatment with platelet inhibitors and β‐blockers was evaluated at baseline and at 12 months follow‐up without significant differences between the interventional or surgical treatment arm.3 Recently, the SYNTAX (Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery) trial, with 1800 patients enrolled between 2005 and 2007, revealed a highly significant underuse of platelet inhibitors, ACE‐inhibitors, ARBs, and statins in CABG patients compared to the PCI stratum at baseline,1 indicating insufficient secondary prevention in high‐risk patients. This becomes even more prominent when compared to trials including patients with medical treatment only.4 Even at 12 months follow‐up there was still a significant difference between the groups with regard to platelet inhibitors, whereas there was no information given about ACE inhibitors, ARBs, β‐blockers, or statins. Recently, the 3‐year follow‐up data of the SYNTAX trial demonstrated no significant differences regarding medical treatment.5 However, overall use of ACE inhibitors (≈︁52%), ARBs (≈︁20%), statins (≈︁86%), and β‐blockers (≈︁77%) was low.
Discussion
Recommended medical treatment guidelines for secondary prevention of patients with coronary artery disease was demonstrated to decrease cardiovascular morbidity and mortality and should be applied for all patients at cardiovascular risk, irrespective of prior revascularization procedure. The recent SYNTAX trial revealed a highly significant underuse of evidence‐based best practices in patients undergoing surgical revascularization at baseline, likely affecting cardiovascular outcome. These data are in line with the results of the Get With the Guidelines Database, where recommended medical treatment guidelines in patients undergoing PCI was superior compared to surgical revascularization.6 Those differences in medical treatment might affect the results of head‐to‐head trials comparing PCI and CABG in cardiovascular risk patients. Moreover, the importance of medical treatment in patients with coronary artery disease was recently demonstrated by the Surgical Treatment for Ischemic Heart Failure trial.7 Additional CABG on top of best medical therapy did not significantly reduce the primary outcome of death from any cause.
Conclusion
Systematic search of the literature revealed insufficient information regarding medical drug treatment in randomized controlled trials except RITA, CABRI, and SYNTAX. Thus, discussion of optimal revascularization procedure has to remain open, even in terms of concomitant medical treatment of patients. The poor reporting of medical treatment at discharge might reflect an underestimation of secondary prevention in patients undergoing cardiac surgery or interventional procedures.
References
- 1. Serruys PW, Morice MC, Kappetein AP, et al; SYNTAX Investigators. Percutaneous coronary intervention versus coronary‐artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–972. [DOI] [PubMed] [Google Scholar]
- 2. Coronary angioplasty versus coronary artery bypass surgery: the Randomized Intervention Treatment of Angina (RITA) trial. Lancet. 1993;341:573–580. [PubMed] [Google Scholar]
- 3. First‐year results of CABRI (Coronary Angioplasty versus Bypass Revascularisation Investigation). CABRI Trial Participants. Lancet. 1995;346:1179–1184. [PubMed] [Google Scholar]
- 4. Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. [DOI] [PubMed] [Google Scholar]
- 5. Kappetein AP, Feldman TE, Mack MJ, et al. Comparison of coronary bypass surgery with drug‐eluting stenting for the treatment of left main and/or three‐vessel disease: 3‐year follow‐up of the SYNTAX trial. Eur Heart. 2011;32:2125–2134. [DOI] [PubMed] [Google Scholar]
- 6. Hiratzka LF, Eagle KA, Liang L, et al. Atherosclerosis secondary prevention performance measures after coronary bypass graft surgery compared with percutaneous catheter intervention and nonintervention patients in the Get With the Guidelines database. Circulation. 2007;116(11 suppl):I207–I212. [DOI] [PubMed] [Google Scholar]
- 7. Velazquez EJ, Lee KL, Deja MA, et al. Coronary‐artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364:1607–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]


