Abstract
Background
The objective of this study was to analyze the effects of general anesthesia in cesarean section on the umbilical cord blood gas values and intraoperative hemodynamics of parturient women.
Material/Methods
A total of 112 parturient women who received cesarean section were eventually randomized into 2 groups, GA (general anesthesia) group (n=56), and SE (combined spinal and epidural anesthesia) group (n=56). The umbilical cord blood gas values, postpartum Apgar score, intraoperative blood loss, mean arterial pressure, heart rate, total operative time, time intervals from anesthesia to delivery and from skin incision to delivery, the incidences of adverse reactions and neonatal asphyxia, and the postoperative patient satisfaction were compared between the 2 groups.
Results
There were no significant differences between the 2 groups in total operative time, Apgar score, neonatal asphyxia rate, umbilical arterial and venous cord blood gas values, intraoperative blood loss, and time interval from skin incision to delivery (all P>0.05). The GA group was significantly shorter in the time interval from anesthesia to delivery than the SE group (P<0.05). The incidences of nausea, vomiting, and chills in the GA group were significantly lower than those in the SE group (all P<0.05). The GA group was significantly higher in postoperative patient satisfaction than the SE group (P<0.05).
Conclusions
General anesthesia has little impact on the umbilical cord blood gas values and Apgar score, and ensures better hemodynamic stability in cesarean section. Moreover, general anesthesia is characterized by rapid induction and is therefore valuable for use in clinical procedures.
MeSH Keywords: Anesthesia, Caudal; Anesthesia, General; Anesthesia, Spinal; Blood Gas Analysis; Cesarean Section
Background
Cesarean section is the most common surgery in the obstetrics department. With the increasing demand for comfort during labor and the restrictions on birth control lifted, caesarean section has become increasingly common over time. The ideal method of anesthesia for cesarean section should have good intraoperative analgesia, alleviate the discomfort during the surgery as much as possible, reduce the incidence of postoperative adverse reactions, and mitigate the adverse effects of cesarean section on the newborn [1–3]. Spinal anesthesia, as a classic method of anesthesia in cesarean section, is recommended by relevant guidelines on anesthesia. It is safe and has been widely used. Nevertheless, some patients still reject this method due to fear, anxiety, tension, and contraindications for anesthesia [4].
Traditionally, it was believed that cesarean section under general anesthesia was prone to cause birth asphyxia. Therefore, general anesthesia was rarely applied to those parturient women who required cesarean section [5]. Some parturient women who were not clinically indicated for spinal anesthesia could only receive cesarean section under local anesthesia in the past [6]. With the development and use of short-term anesthetics such as propofol, the adverse effects of general anesthesia on parturient women and newborns may be lower than before. This makes the application of general anesthesia in obstetrics draw more attention [7–9]. Therefore, the effects of cesarean section under general anesthesia on the newborn required verification.
The goal of this study was to compare general anesthesia, and combined spinal and epidural anesthesia, in cesarean section. The primary outcomes are umbilical cord blood gas values. The secondary outcomes are Apgar scores, neonatal asphyxia rate, total operative time, intraoperative vital signs, adverse reactions, and postoperative patient satisfaction ratings.
Material and Methods
General information
The parturient women who underwent cesarean section in The First People’s Hospital of Jingzhou from June 2017 to March 2018 were recruited in this study according to the inclusion and exclusion criteria. A total of 112 parturient women were randomized into 2 groups through a computer-generated random number table (providing computerized random numbers), with 56 parturient women in each group. The group given general anesthesia was defined as the GA (general anesthesia) group, and the group given combined spinal and epidural anesthesia as the SE (combined spinal and epidural anesthesia) group. This study was approved by the Ethics Committee of The First People’s Hospital of Jingzhou, The First Affiliated Hospital of Yangtze University; all participants signed informed consent before entry into the study.
Inclusion criteria
Inclusion criteria for this study was as follows: patients who opted for cesarean section or had to undergo cesarean section due to mental disorders, vaginal trauma, or intrauterine adhesions; patients who had a full-term pregnancy; patients whose results of color Doppler ultrasound combined with fetal heart rate monitoring showed no signs of fetal distress before surgery; patients whose newborns were predicted to weigh >2500 g; patients whose hemoglobin >90 g/L; and patients who were identified as singleton pregnancy using B mode ultrasound; patients who categorized as ASA (American Society of Anesthesiologists) physical status Class 1 or Class 2.
Exclusion criteria
Exclusion criteria for this study was as follows: parturient women with severe internal, surgical, or obstetric comorbidities; patients who were given analgesic and sedative drugs before surgery; patients with severe mental illness; patients could not comply with doctors’ reasonable instructions; patients who refused to participate in the study; patients who were allergic to anesthetics; and patients who had contraindications to both general anesthesia and combined spinal and epidural anesthesia.
Methods of anesthesia
After skin prepping and draping, the GA group received balanced anesthesia (intravenous anesthesia in combination with inhalation anesthesia) by using the following anesthetics: propofol (2 mg/kg, Fresenius Kabi Deutschland GmbH, Germany), remifentanil (1.5 μg/kg, Hubei Humanwell, China), and rocuronium bromide (0.6 mg/kg, Zhejiang Xianju, China). Tracheal intubation was performed after induction of anesthesia to facilitate mechanical ventilation. After delivery, sufentanil (0.3–0.5 μg/kg, Hubei Humanwell, China) was instantly intravenously injected into patients and remifentanil (0.08–0.2 μg/(kg/min), Hubei Humanwell, China) and cisatracurium besilate (1–2 μg/(kg/min), Jiangsu Hengrui, China) were given to patients using intravenous infusion pump with continuous inhalation of sevoflurane (1–5%, Jiangsu Hengrui, China).
The SE group received combined spinal and epidural anesthesia. With the patient lying in a left lateral position, the spinal needle was punctured into the subarachnoid space through L2–L3 or L3–L4 interspace and 12 mg of 0.6% ropivacaine naropine (AstraZeneca AB, Sweden) was injected. The removal of the spinal needle was followed by the placement of epidural catheter (3.5–4.5 cm). Through the epidural catheter, 5 mL of 2% lidocaine (Shanxi Shiyao Yinhu, China) was initially given to determine the anesthetic effect. The sensory block level was adjusted to approximately T6–T7. The anesthetists who performed anesthesia were similar in the level of expertise and did not know about the study protocol.
Measurements
The blood gas analysis was performed only once using the blood gas analyzer with the umbilical cord venous and arterial blood immediately drawn after the childbirth. PO2, PCO2, Hct, pH and SO2 were measured and compared between the 2 groups. The Apgar scores at 1, 5, and 10 minutes after delivery were recorded to assess the degree of neonatal asphyxia and were compared between the 2 groups. The Apgar score was assessed based on 5 criteria: activity, pulse rate, reflex irritability grimace, skin color, and respiratory effort. After delivery, the child was rated according to these aforementioned criteria. The sum of the 5 values is the Apgar score. A score of 7–10 was considered normal; 4 to 6, mild neonatal asphyxia; and 3 and below, severe neonatal asphyxia [10]. The neonatal asphyxia rates were recorded and compared between the 2 groups. Time interval from anesthesia to delivery, intraoperative blood loss, total operative time, heart rates (HR) before anesthesia (T1), and at the time of skin incision (T2) and delivery (T3), as well as mean arterial pressure (MAP) were all recorded and compared between the 2 groups. Complications including intraoperative hypotension, postoperative nausea, vomiting, bradycardia, and chills were recorded; phenylephrine was given intravenously when severe hypotension occurred during surgery to increase blood pressure; tropisetron was administered when severe nausea and vomiting occurred to stop vomiting and prevent the occurrence of reflux aspiration; atropine was given when bradycardia occurred to increase heart rate. The inflatable heating instrument was applied, and tramadol was given to patients if severe chills occurred). Postoperative patient satisfaction was also recorded.
A satisfaction questionnaire was used 3 days after surgery to investigate postoperative patient satisfaction. The questionnaire mainly consisted of intraoperative discomfort, treatment effect, adverse reactions, and physical recovery. The total score of the questionnaire was 100. A score of 81–100 indicated a very satisfactory anesthesia; 61–80, a satisfactory anesthesia; 60 and below, dissatisfactory anesthesia. Patient satisfaction=(cases of very satisfactory+cases of satisfactory)/(total number of cases) ×100%.
Statistical analysis
All data were statistically processed using SPSS 22.0 software package. The measurement data were expressed as mean ± standard deviation (χ±SD), and were compared between 2 groups based on independent-sample t-test. The enumeration data were expressed as cases/percentage (N/%), and were compared between the 2 groups based on chi-square test or Fisher’s exact test. P value of <0.05 was considered significant. The sample size was determined according the means and SD of pH values of the control group and the experimental group. We hypothesized the level of significance α=0.005 and the power=0.99 (1-β). In addition, since this was a non-inferiority trial, the margin should be positive number (odds ratio [OR] >1). Therefore, the OR was set at 2.
Results
Baseline characteristics
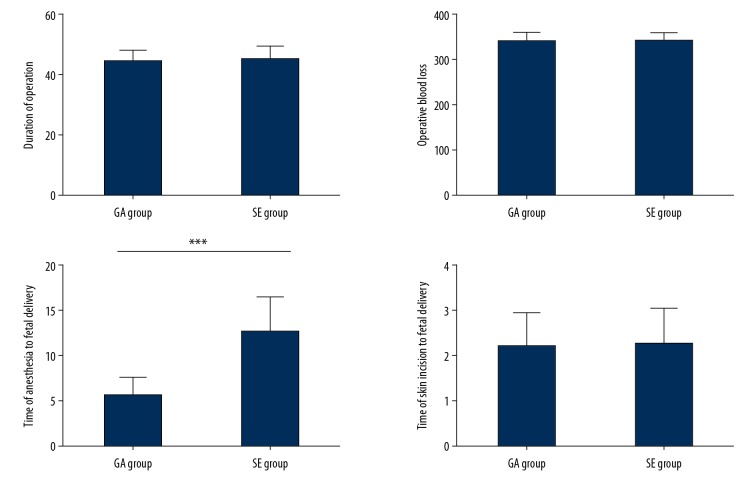
There were 157 parturient women who underwent cesarean section in The First People’s Hospital of Jingzhou from June 2017 to March 2018. They were recruited in this study according to the inclusion and exclusion criteria. A total of 112 parturient women were randomized into the GA group and the SE group through a computer-generated random number table (providing computerized random numbers), with 56 parturient women in each group (Figure 1). The sample size was determined according to the means (7.30 versus 7.32) and SD (0.80 versus 0.72) of pH values of the experimental group (n=10) and the control group (n=10) in the preliminary study. We hypothesized the level of significance α=0.005 and the power=0.99 (1-β). In addition, since a non-inferiority trial was conducted, the margin should be positive number (OR >1). Therefore, the OR was set at 2 and the sample size of in each group was equal (n=9). The sample size of this study met the requirements of the predicted sample size. None of the patients in both groups withdrew or suffered irreversible severe damages during the study. No significant differences were found in baseline characteristics between the 2 groups (all P>0.05) (Table 1).
Figure 1.
CONSORT flow chart.
Table 1.
Comparison of baseline characteristics.
| GA group (n=56) | SE group (n=56) | t/χ2 | P | |
|---|---|---|---|---|
| Age range (year) | 27.3±3.2 | 27.5±2.9 | −0.380 | 0.705 |
| Reasons for cesarean section | ||||
| Voluntary | 20 | 17 | 0.363 | 0.547 |
| Other reasons | 36 | 39 | ||
| ASA physical status | ||||
| Class 1 | 36 | 38 | 0.159 | 0.690 |
| Class 2 | 20 | 18 | ||
| Gestational week | 39.8±5.2 | 40.2±6.1 | −0.335 | 0.738 |
Voluntary refers to receiving cesarean section voluntarily; Other reasons refer to receiving cesarean section for other reasons such as vaginal delivery contraindicated; ASA – American Society of Anesthesiologists; GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group.
Blood gas analysis
The PO2, PCO2, Hct, SO2, and pH of umbilical cord arterial and venous blood were all within normal ranges. There were no significant differences in these indexes between the 2 groups (all P>0.05) (Table 2).
Table 2.
Comparisons of blood gas results of umbilical cord arterial and venous blood.
| GA group (n=56) | SE group (n=56) | t | P | |
|---|---|---|---|---|
| Umbilical cord arterial blood gas values | ||||
| pH | 7.32±0.79 | 7.31±0.86 | 0.064 | 0.949 |
| PO2 (mmHg) | 25.41±4.34 | 24.90±4.19 | 0.633 | 0.528 |
| PCO2 (mmHg) | 52.45±5.23 | 52.13±5.09 | 0.328 | 0.743 |
| Hct (%) | 54.97±5.89 | 55.01±6.02 | −0.036 | 0.972 |
| SO2 (%) | 98.34±1.12 | 98.47±1.20 | −0.593 | 0.555 |
| Umbilical cord venous blood gas values | ||||
| pH | 7.34±0.69 | 7.35±0.78 | −0.072 | 0.943 |
| PO2 (mmHg) | 34.60±7.01 | 33.24±7.21 | 1.012 | 0.314 |
| PCO2 (mmHg) | 50.90±4.78 | 49.77±5.19 | 1.198 | 0.233 |
| Hct (%) | 54.62±4.42 | 54.99±4.18 | −0.455 | 0.650 |
| SO2 (%) | 98.72±1.12 | 98.61±1.43 | 0.453 | 0.651 |
pH – pH value; PO2 – partial pressure of oxygen; PCO2 – partial pressure of carbon dioxide; Hct – hematocrit; SO2 – oxygen saturation; GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group.
Apgar score
In the GA group, the Apgar scores at 1, 5, and 10 minutes of childbirth were 9.01±0.96, 9.62±0.62, and 10.00±0.00 respectively, and the neonatal asphyxia rate was 26.79%. No significant differences were found in Apgar scores and neonatal asphyxia rates between the 2 groups (all P>0.05) (Table 3).
Table 3.
Comparisons of Apgar scores and neonatal asphyxia rates.
| GA group (n=56) | SE group (n=56) | t/χ2 | P | |
|---|---|---|---|---|
| Apgar score | ||||
| 1 min after birth | 9.01±0.96 | 8.98±0.87 | 0.173 | 0.863 |
| 5 min after birth | 9.62±0.62 | 9.65±0.71 | −0.238 | 0.812 |
| 10 min after birth | 10.00±0.00 | 10.00±0.00 | ||
| No asphyxia | 41 | 39 | ||
| Mild asphyxia | 10 | 9 | ||
| Severe asphyxia | 5 | 8 | ||
| Asphyxia rate | 26.79% | 30.36% | 0.175 | 0.676 |
GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group.
Surgical data
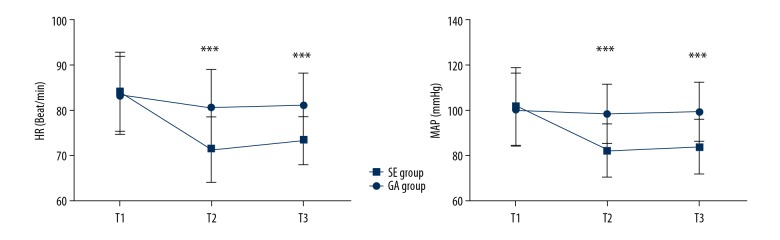
The total operative time, intraoperative blood loss, and time interval from skin incision to delivery were not significantly different between the 2 groups (all P>0.05). The difference of time interval from anesthesia to delivery between the GA group and the SE group was statistically significant (P<0.001) (Figure 2).
Figure 2.
Comparison of surgical data. (A) Comparison of total operative time (minutes). (B) Comparison of intraoperative blood loss (mL). (C) Comparison of time interval from anesthesia to delivery (minute). (D) Comparison of time interval from skin incision to delivery (minute). *** P<0.001. GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group.
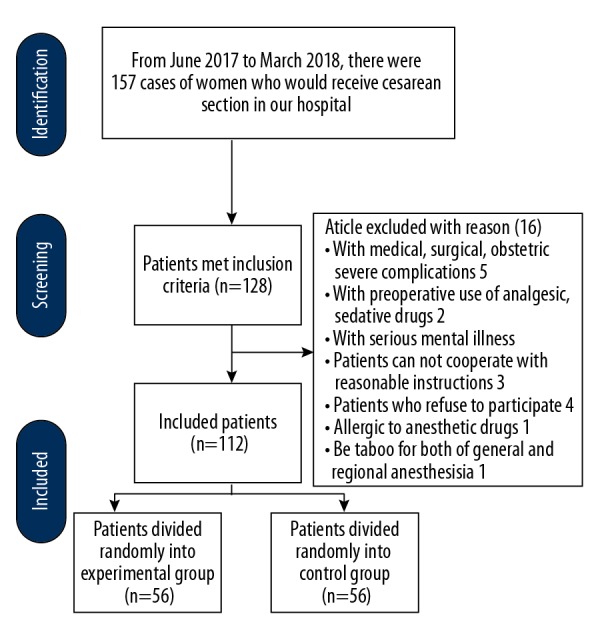
Hemodynamics
Before anesthesia (T1), there were no significant differences in patient HR and MAP values between the GA group (both P>0.05). At the time of skin incision (T2) and delivery (T3), HR in the GA group showed statistically significant differences when compared with that in the SE group (both P<0.001); MAP in the GA group showed statistically significant differences when compared with that in the SE group (both P<0.001) (Figure 3).
Figure 3.
Comparison of hemodynamics. (A) Comparison of HR between 2 groups. (B) Comparison of MAP between 2 groups. *** P<0.001. GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group; HR – heart rates; MAP – mean arterial pressure.
Postoperative adverse reactions
Adverse reactions such as nausea, vomiting, muscle pain, bradycardia and chills were found in both groups. The incidences of postoperative nausea and chills were significantly lower in GA group than in SE group (both P<0.05). But there were no significant differences in the incidences of vomiting, muscle pain and bradycardia between the 2 groups (all P>0.05) (Table 4).
Table 4.
Comparison of postoperative adverse reactions.
| GA group (n=56) | SE group (n=56) | χ2 | P | |
|---|---|---|---|---|
| Nausea | 3 | 10 | 4.264 | 0.039 |
| Vomiting | 1 | 7 | 0.067 | |
| Muscle pain | 2 | 3 | 1.000 | |
| Bradycardia | 2 | 1 | 1.000 | |
| Chills | 2 | 10 | 5.973 | 0.015 |
GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group.
Patient satisfaction
The postoperative patient satisfaction was investigated and statistically analyzed. In GA group, the postoperative patient satisfaction was 89.3%. In SE group, the postoperative patient satisfaction was 67.9%. The difference between 2 groups was statistically significant (P=0.006) (Table 5).
Table 5.
Comparison of postoperative patient satisfaction.
| GA group (n=56) | SE group (n=56) | χ2 | P | |
|---|---|---|---|---|
| Very satisfactory | 38 | 30 | ||
| Satisfactory | 12 | 8 | ||
| Dissatisfactory | 6 | 18 | ||
| Patient satisfaction | 89.3% | 67.9% | 7.636 | 0.006 |
GA group – general anesthesia group; SE group – combined spinal and epidural anesthesia group.
Discussion
Obstetric anesthesia is of great importance to cesarean section. At present, combined spinal and epidural anesthesia is a major method of anesthesia in China, but it is slow in induction and has the possibility of failing to puncture into the target site [11]. This may have a negative effect on emergency cesarean section. Moreover, the incidence of hypotension in parturient women receiving combined spinal and epidural anesthesia is high [12], which may have an impact on blood supply to fetus.
This study performed blood gas analyses based on umbilical cord arterial and venous blood. The umbilical arterial blood gas analysis is currently recognized as an important indicator of neonatal oxygenation index and acid-base status. The combination of umbilical arterial blood gas analysis and Apgar score can accurately reveal the effect of anesthesia on the fetus [13,14]. This study confirmed that the results of blood gas analysis of patients under general anesthesia were all within the normal range, and that there were no differences between general anesthesia and combined spinal and epidural anesthesia in terms of these indicators. This demonstrates that general anesthesia has no adverse effect on fetal respiratory and circulatory functions. Previous studies found that general anesthesia showed no particular effect on the rehabilitation after cesarean section [15,16]. It was also confirmed in this study that general anesthesia did not affect the Apgar score and did not increase the incidence of neonatal asphyxia. At present, general anesthesia is not widely used in cesarean section because general anesthetics may cross the placental barrier to adversely affect the fetus [17,18].
This study indicated that after the induction of anesthesia, patients in both groups had decreased HR and MAP, but the patients with combined spinal and epidural anesthesia showed a more significant decrease in HR and MAP, and substantial intraoperative fluctuations. This may be attributable to the greater impact of combined spinal and epidural anesthesia on the sympathetic nerves, resulting in the dilation of blood vessels and a slowed heart rate [12]. Moreover, we found that the time interval from anesthesia to delivery in patients under general anesthesia was significantly shortened, probably because the rapid induction of general anesthesia eliminated the need to change body position, thus saving the time of anesthesia [19].
Meanwhile, our study pointed out that the incidences of nausea and chills after general anesthesia were significantly reduced. Postoperative nausea is mainly caused by contractions or significant intraoperative fluctuations of blood pressure [20,21]. General anesthesia can prevent excessive levels of sensory block and stabilize blood pressure, thereby reducing postoperative nausea. Moreover, this study showed that general anesthesia could lead to a significant increase in postoperative patient satisfaction. There are 2 possible reasons. First, patients under general anesthesia are unconscious during surgery, thereby reducing intraoperative anxiety and discomfort. Second, patients’ adverse reactions significantly reduce after surgery.
However, the small sample size and short follow-up time of this study may cause errors in the results. Therefore, randomized controlled trials with larger sample size and longer follow-up are warranted in the future.
Conclusions
General anesthesia has little impact on umbilical cord blood gas values and Apgar score and ensures better hemodynamic stability in cesarean section. Moreover, general anesthesia is characterized by rapid induction and therefore is valuable for use in clinical procedures.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Ituk U, Thenuwara K. The effect of a single intraoperative dose of intravenous dexamethasone 8 mg on post-cesarean delivery analgesia: A randomized controlled trial. Int J Obstet Anesth. 2018;35:57–63. doi: 10.1016/j.ijoa.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Thomas S, Meadows J, Mcqueen KM. Impact of access to cesarean section and safe anesthesia on maternal mortality ratio in low-income countries: A new reality in the post 2015 era. Ann Glob Health. 2016;82:563. [Google Scholar]
- 3.Yuan QM. [Anesthesia mode and effect analysis of cesarean section in pregnancy induced hypertension]. Medical Innovation of China. 2017;14:132–34. [in Chinese] [Google Scholar]
- 4.Saygı Aİ, Özdamar Ö, Gün İ, et al. Comparison of maternal and fetal outcomes among patients undergoing cesarean section under general and spinal anesthesia: A randomized clinical trial. Sao Paulo Med J. 2015;133:227–34. doi: 10.1590/1516-3180.2014.8901012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trincado DJM, Martin SV. Fetal asphyxia caused by general anesthesia in cesarean section;new anesthetic method of preventing it. Rev Esp Obstet Ginecol. 1955;14:86–95. [PubMed] [Google Scholar]
- 6.Ranney B, Stanage WF. Advantages of local anesthesia for cesarean section. Obstet Gynecol. 1975;45:163. [PubMed] [Google Scholar]
- 7.Desai N, Wicker J, Sajayan A, Mendonca C. A survey of practice of rapid sequence induction for caesarean section in England. Int J Obstet Anesth. 2018;36:3–10. doi: 10.1016/j.ijoa.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Aregawi A, Terefe T, Admasu W, Akalu L. Comparing the effect of spinal and general anaesthesia for pre-eclamptic mothers who underwent caesarean delivery in a tertiary, Addis Ababa, Ethiopia. Ethiop J Health Sci. 2018;28:443–50. doi: 10.4314/ejhs.v28i4.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Houthoff KK, Weibel S, Kranke P, Schreiber JU. Hypnotic agents for induction of general anesthesia in cesarean section patients: A systematic review and meta-analysis of randomized controlled trials. J Clin Anesth. 2018;48:73–80. doi: 10.1016/j.jclinane.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Fauziah PN, Sitanggang E, Maskoen AM, et al. Correlation between levels of troponin T (TnT), pH cord blood, and Apgar score in fetal distress and normal pregnancy. International Journal of Chemtech Research. 2016;9:505–10. [Google Scholar]
- 11.Mccahon RA, Catling S. Time required for surgical readiness in emergency caesarean section: Spinal compared with general anaesthesia. Int J Obstet Anesth. 2003;12:178–82. doi: 10.1016/S0959-289X(02)00196-6. [DOI] [PubMed] [Google Scholar]
- 12.Soxhuku-Isufi A, Shpata V, Sula H. Maternal and neonatal effects of vasopressors used for treating hypotension after spinal anesthesia for caesarean section: A randomized controlled study. Open Access Maced J Med Sci. 2016;4:54–58. doi: 10.3889/oamjms.2016.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loh SF, Woodworth A, Yeo GS. Umbilical cord blood gas analysis at delivery. Singapore Med J. 1998;39:151–55. [PubMed] [Google Scholar]
- 14.Zhang CY, Rui LI, Zhang DC. [Value of umbilical cord blood gas analysis in diagnosis of asphyxia in preterm infants and analysis on the influencing factors]. Maternal & Child Health Care of China. 2017;5:968–71. [in Chinese] [Google Scholar]
- 15.Nafie M, Ismael S. Comparing effects of caesarean section using spinal and general anesthesia on neonatal short-term outcome. Industrial & Engineering Chemistry. 2016;42:777–86. [Google Scholar]
- 16.Van de Velde M. The use of remifentanil during general anesthesia for caesarean section. Curr Opin Anaesthesiol. 2016;29:257–60. doi: 10.1097/ACO.0000000000000334. [DOI] [PubMed] [Google Scholar]
- 17.Skerman JH, Rajab KE. Obstetric, neonatal and anesthetic considerations for preterm labor and delivery. Saudi Med J. 2003;24:582–93. [PubMed] [Google Scholar]
- 18.Vähäkangas K, Myllynen P. Drug transporters in the human blood–placental barrier. Br J Pharmacol. 2009;158:665–78. doi: 10.1111/j.1476-5381.2009.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Obi VO, Umeora OUJ. Anesthesia for emergency cesarean section: A comparison of spinal versus general anesthesia on maternal and neonatal outcomes. African Journal of Medical and Health Sciences. 2018;17:31. [Google Scholar]
- 20.Magni BJ, Dyer RA, Dyk DV, Nugteren JV. Incidence of intraoperative nausea and vomiting during spinal anaesthesia for caesarean section in two Cape Town state hospitals. Southern African Journal of Anaesthesia & Analgesia. 2016;22:131–34. [Google Scholar]
- 21.Amouee M, Montazeri S, Zadeh RA, Ghorbani M. The effect of ginger capsule on nausea and vomiting during and after caesarean section under spinal anesthesia. International Journal of Clinical Medicine. 2016;7:106–12. [Google Scholar]