Abstract
Background:
Non–ST‐segment myocardial infarction (NSTEMI) is one of the major causes of hospital admissions. Mortality trend in patients with NSTEMI over the years has not been studied well. The goal of this study is to explore age‐adjusted long‐term mortality trends from NSTEMI in the United States using a very large database.
Methods:
We used the National Inpatient Sample (NIS) database, a component of the Health Care Cost and Utilization (HCUP) project, for this study. International Classification of Disease, Ninth Revision, Clinical Modification (ICD‐9‐CM) codes were used to identify NSTEMI cases in patients >40 years old. Age‐adjusted mortality rates for NSTEMI cases were calculated by multiplying the age‐specific mortality rates of NSTEMI by age‐specific weights.
Results:
A total of 1,400,234 patients above the age of 40 years were identified. The mean age of this cohort was 77.1±10.7 years, with a total of 179,361 deaths being reported over this 16‐year period. Among patients who died, 51.2% were men and 48.8% were women. The age‐adjusted mortality from NSTEMI declined from 1988 (727 per 100,000) to 2004 (305 per 100,000) until the middle of the decade when mortality from NSTEMI started leveling off. Total mortality decreased from 29.6% in 1988 to 11.3% in 2004.
Conclusions:
Our analysis showed a significant reduction in the age‐adjusted and total mortality for NSTEMI over the years studied. The cause of this trend is not known but most likely reflects advancement in the treatment of patients with acute coronary syndrome. © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
In 2003, cardiovascular disease accounted for 37.3% of all deaths in the United States, making it the single largest cause of mortality among the US population.1 Acute coronary syndrome (ACS) is an expression of cardiovascular disease and its occurrence frequently foretells short‐term and long‐term mortality. ACS is an umbrella term that encompasses unstable angina, non–ST‐segment elevation myocardial infarction (NSTEMI), and ST‐segment elevation myocardial infarction (STEMI). Of the 1.4 million patients admitted to hospitals in the United States with an ACS, almost 70% tend to have unstable angina or NSTEMI.2 The 2000 consensus document defining myocardial infarction (MI), establishes NSTEMI as a substantiated clinical entity and diagnosis.3 NSTEMI patients do not have the typical ST segment elevation characteristic of patients with STEMI, but still have release of cardiac biomarkers signifying myocardial necrosis secondary to coronary ischemia. Despite repeated guidelines,4 the management of NSTEMI has not been as rigorously defined as that of its more easily identifiable counterpart, STEMI. The aggressive revascularization strategies that have been championed for STEMI and have led to a decrease in STEMI mortality have not consistently been extended to patients with NSTEMI. Patients with NSTEMI also tend to be demographically different, when compared to patients who have STEMI.5 Secular trends for STEMI have shown a gradual decline in mortality in the United States,6 but the trends for mortality of NSTEMI remain imprecise. The goal of this study is to explore age‐adjusted long‐term mortality trends from NSTEMI in the United States using a very large database of inpatients, the National Inpatient Sample (NIS) database.
Methods
Our data has been obtained from the NIS database, a component of the Health Care Cost and Utilization (HCUP) project,7 which is sponsored by the Agency for Healthcare Research and Quality (AHRQ). The HCUP databases have been developed as a collective effort between government (both Federal and State) and industry, and serves as the largest collection of longitudinal hospital care data in the United States. The NIS contains data from roughly 8 million hospital stays per year, and is built from submitted payer information from hospital inpatient admissions in the United States, from 1988 through 2004. The database tries to provide a 20% stratified sample that reflects trends from community hospitals in the United States. The database discloses patient demographics, procedures, admission, and discharge status as well as primary and secondary discharge diagnoses. The International Classification of Disease, Ninth Revision, Clinical Modification (ICD‐9‐CM) coding system was used to identify NSTEMI cases. The specific codes that were utilized for the purposes of this study were: subendocardial infarction (410.71) and acute MI of unspecified site (410.91). We limited our analysis to patients >40 years old in order to exclude the majority of nonatherosclerotic causes of NSTEMI.
Age‐adjusted mortality rates for NSTEMI patients were calculated by multiplying NSTEMI age‐specific mortalities by age‐specific weights. The age‐specific mortality rates for NSTEMI patients were obtained from the NIS database. The age‐specific weights were calculated from the National Center for Health Statistics recommended standardized US 2000 population. Statistical Package for the Social Sciences (SPSS) (SPSS, Inc., Chicago, IL) software was utilized for statistical analysis. Quantitative variables were expressed as means ± standard deviation (SD) and independent samples Student t test was used for comparative analysis. A P value of <0.05 was regarded as statistically significant.
Results
A total of 1,400,234 patients above the age of 40 years were selected from the NIS database based on the aforementioned ICD‐9‐CM codes. The mean age of this cohort was 77.1±10.7 years, with a total of 179,361 deaths being reported over this 16‐year period. Among patients who died, 51.2% were men and 48.8% were women. The age‐adjusted mortality from NSTEMI declined from 1988 (727 per 100,000) to 2004 (305 per 100,000) (Table 1). A closer review of the table shows that there was a gradual decline in the mortality until the end of the 1990s when mortality from NSTEMI started leveling off (Figure 1). Total mortality also decreased from 29.6% in 1988 to 11.3% in 2004 (Figure 2).
Table 1.
NSTEMI Age‐Adjusted Mortality from 1988 through 2004
| Year | Population | Age‐Adjusted Mortality (per 100,000) | Lower CI | Upper CI |
|---|---|---|---|---|
| 1988 | 20977 | 727.2793 | −256.926 | 1711.484 |
| 1989 | 31432 | 556.8362 | −58.7623 | 1172.435 |
| 1990 | 50168 | 383.0445 | 47.85385 | 718.2352 |
| 1991 | 54488 | 370.5535 | 59.413 | 681.6941 |
| 1992 | 59814 | 359.9600 | 71.48454 | 648.4355 |
| 1993 | 63951 | 351.7327 | 79.1206 | 624.3449 |
| 1994 | 64767 | 322.3853 | 74.09806 | 570.6726 |
| 1995 | 71521 | 309.0036 | 82.5377 | 535.4695 |
| 1996 | 75480 | 295.9795 | 84.8243 | 507.1346 |
| 1997 | 86560 | 291.4456 | 97.28776 | 485.6035 |
| 1998 | 93354 | 291.7703 | 104.6027 | 478.9379 |
| 1999 | 103466 | 304.8158 | 119.0804 | 490.5512 |
| 2000 | 117238 | 298.6814 | 127.7074 | 469.6553 |
| 2001 | 120944 | 291.0755 | 127.028 | 455.123 |
| 2002 | 127539 | 293.6504 | 132.4874 | 454.8133 |
| 2003 | 131480 | 296.4909 | 136.2263 | 456.7556 |
| 2004 | 127055 | 305.2437 | 137.3993 | 473.0881 |
Abbreviations: CI, confidence interval; NSTEMI, non–ST‐elevation myocardial infarction.
Figure 1.
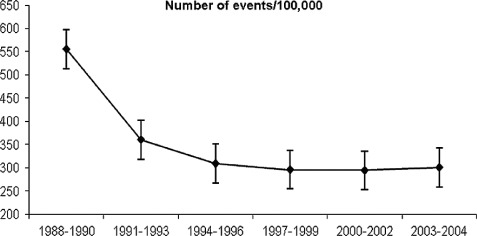
Trends in NSTEMI mortality from 1988 through 2004. Y‐axis is the number of events per 100,000. Abbreviation: NSTEMI, non–ST‐segment elevation myocardial infarction.
Figure 2.
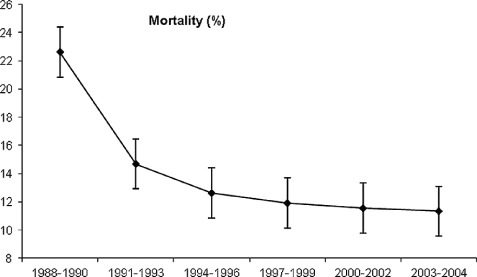
Total mortality (%) of patients with NSTEMI who died during the follow‐up period. Abbreviation: NSTEMI, non–ST‐segment elevation myocardial infarction.
Discussion
Data from the National Registry of Myocardial Infarction (NRMI) illustrates that from 1990 to 2006, the proportion of patients with NSTEMI increased while the proportion of STEMI declined.8 NSTEMI has at present replaced non‐Q wave myocardial infarction (NQWMI) as the clinical counterpart to STEMI/Q wave myocardial infarction (QWMI). An STEMI is often associated with an occlusive coronary thrombus,9 while the pathological correlate of NSTEMI is less well‐defined, likely associated with nonocclusive thrombi, inflammation, and dynamic coronary obstruction.10 Patients with NSTEMI generally tend to be older and have more extensive coronary disease than patients with STEMI.5 In comparison to STEMI, patients who experience an NSTEMI have a lower 30‐day mortality.11 However, 6‐month mortality rates are similar for STEMI and NSTEMI patients.12
Our analysis of the secular trends of over a million patients uncovers a significant reduction in age‐adjusted mortality for NSTEMI patients over the period extending from 1988 to 2004. This finding is encouraging in the setting of initially increasing and later plateaued incident of NSTEMI.13 International registry analyses have also indicated a decrease in NSTEMI mortality, signaling that this is not a phenomenon that is exclusive to the United States.14 In the NRMI database, in‐hospital mortality for NSTEMI decreased significantly by 22.6%.8 As can be expected, mortality rates from real‐world registries are higher than the rates seen in controlled clinical trials. The Global Registry of Acute Coronary Events (GRACE) registry in‐hospital mortality rate for NSTEMI was 5.9% and the 6‐month mortality rate was 6.2%, with a 6‐month rehospitalization rate of about 20%.15 Mortality from NSTEMI is affected by several factors including demographics such as age, gender, race and comorbidities, and clinical variables such as heart rate, blood pressure, electrocardiographic signs of ischemia, and presence of heart failure.16 Global risk stratification strategies, such as the GRACE and Thrombolysis in Myocardial Infarction (TIMI) scores, remain an integral component of the management of NSTEMI and assist in identifying patients at risk for recurrent ischemia and death.4, 17 Higher TIMI scores have been associated with more extensive coronary artery disease18 as well as impaired epicardial blood flow and presence of visible thrombus.19
Management of NSTEMI remains hampered by lack of definitive evidence that assures the best outcome in such patients. Guidelines have been published, but the evidence base is nowhere near as robust as the ones for STEMI.4, 20 Current treatment inclination includes an upfront medical approach followed by a downstream invasive or non‐invasive management strategy. A 2010 Cochrane Review verified a 33% reduction in angina and rehospitalization at 6 months with an invasive strategy, along with a 27% reduction in MI at 12 months, albeit with a 2‐fold increase in periprocedural MI.21 A 2006 meta‐analysis of over 8000 patients found an early invasive strategy to have a lower all cause mortality at 24 months.22 In the “Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines” (CRUSADE) registry, an early invasive strategy was associated with a 4.7% risk of death or MI as opposed to 8.9% risk with a conservative strategy.23 An early invasive strategy was shown to be beneficial by the “Fragmin and fast Revascularization during InStability in Coronary artery disease” (FRISC) II, “Treat Angina with aggrastat and determine Cost of Therapy with Invasive or Conservative Strategy” (TACTICS)‐ TIMI 18, and “Randomized Intervention Trial of unstable Angina” (RITA) 3 studies, especially in the subgroup of patients who were at a high risk, such as those patients presenting with an elevated cardiac troponin level. However, the most recent randomized “Invasive versus Conservative Treatment in Unstable Coronary Syndromes” (ICTUS) trial showed that an early invasive strategy was not superior to an early conservative strategy, even for the high risk patients, on the short‐term and long‐term clinical follow‐up.24
The role of an early invasive strategy in NSTEMI has been debated and a consensus continues to elude us, except in patients with high risk markers.24, 25 Invasive strategies do decrease recurrent angina and MI, but a decrease in mortality has not been definitively or reproducibly documented.21 Currently, it is recommended that NSTEMI patients with high‐risk features (recurrent ischemia, heart failure, left ventricular dysfunction, hemodynamic or electrical instability, and prior coronary artery bypass grafting [CABG]) undergo an invasive strategy.26
Recently, emphasis has been made to optimize guideline‐based medical therapy in patients presenting with ACS. Statins have been repeatedly shown to be effective in reducing recurrent event rates in patients with coronary artery disease. The use of high dose of statin in patients presenting with ACS has lead to lower adverse events. It has lead to improvement in the myocardial flow and lower adverse event27, 28, 29 and lower long‐term event rates.30, 31, 32 In addition to statin therapy, increases in the utilization of guideline‐based therapy in recent years among treating physicians has been documented33 as an important contributor to lower NSTEMI‐related mortality.
Limitations of this analysis include its retrospective nature, which makes it susceptible to significant selection bias. Moreover, patient inclusion was entirely predicated by ICD‐9‐CM codes, a fact that may have hampered our ability to capture the intended target population. Nevertheless, the extremely large sample size that we have analyzed here intrinsically lends itself to a more robust conclusion. In the GRACE registry, rates of percutaneous coronary intervention (PCI) increased by 18% from 1999 to 2006 and 6‐month death rates decreased by 1.6% in NSTEMI patients.34 It would not be a stretch to hypothesize that the advent of a more aggressive and invasive approach to the management of NSTEMI may have contributed to the demonstrated decline in mortality. On the other hand, this remains to be unambiguously established.
References
- 1. Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics—2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151. [DOI] [PubMed] [Google Scholar]
- 2. Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. [DOI] [PubMed] [Google Scholar]
- 3. Alpert JS, Thygesen K, Antman E, et al. Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36: 959–969. [DOI] [PubMed] [Google Scholar]
- 4. Bassand JP, Hamm CW, Ardissino D, et al. Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1598–1660. [DOI] [PubMed] [Google Scholar]
- 5. Abbott JD, Ahmed HN, Vlachos HA, et al. Comparison of outcome in patients with ST‐elevation versus non‐ST‐elevation acute myocardial infarction treated with percutaneous coronary intervention (from the National Heart, Lung, and Blood Institute Dynamic Registry). Am J Cardiol. 2007;100:190–195. [DOI] [PubMed] [Google Scholar]
- 6. Movahed MR, John J, Hashemzadeh M, et al. Trends in the age adjusted mortality from acute ST segment elevation myocardial infarction in the United States (1988‐2004) based on race, gender, infarct location and comorbidities. Am J Cardiol. 2009;104: 1030–1034. [DOI] [PubMed] [Google Scholar]
- 7. HCUP Nationwide Inpatient Sample (NIS). HCaUiP (2002). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2002. [Google Scholar]
- 8. Rogers WJ, Frederick PD, Stoehr E, et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non‐ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1026–1034. [DOI] [PubMed] [Google Scholar]
- 9. Davies MJ, Woolf N, Robertson WB. Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi. Br Heart J. 1976;38:659–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. DeWood MA, Stifter WF, Simpson CS, et al. Coronary arteriographic findings soon after non‐Q‐wave myocardial infarction. N Engl J Med. 1986;315:417–423. [DOI] [PubMed] [Google Scholar]
- 11. Armstrong PW, Fu Y, Chang WC, et al. Acute coronary syndromes in the GUSTO‐IIb trial: prognostic insights and impact of recurrent ischemia. The GUSTO‐IIb Investigators. Circulation. 1998;98:1860–1868. [DOI] [PubMed] [Google Scholar]
- 12. Volmink JA, Newton JN, Hicks NR, et al. Coronary event and case fatality rates in an English population: results of the Oxford myocardial infarction incidence study. The Oxford Myocardial Infarction Incidence Study Group. Heart. 1998;80:40–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Movahed MR, Ramaraj R, Hashemzadeh M, et al. Nationwide trends in the age adjusted prevalence of non‐ST elevation myocardial infarction (NSTEMI) across various races and gender in the USA. Acute Card Care. 2010;12:58–62. [DOI] [PubMed] [Google Scholar]
- 14. Tang EW, Wong CK, Restieaux NJ, et al. Clinical outcome of older patients with acute coronary syndrome over the last three decades. Age Ageing. 2006;35:280–285. [DOI] [PubMed] [Google Scholar]
- 15. Goldberg RJ, Currie K, White K, et al. Six‐month outcomes in a multinational registry of patients hospitalized with an acute coronary syndrome (the Global Registry of Acute Coronary Events [GRACE]). Am J Cardiol. 2004;93:288–293. [DOI] [PubMed] [Google Scholar]
- 16. Boersma E, Pieper KS, Steyerberg EW, et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST‐segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation. 2000;101: 2557–2567. [DOI] [PubMed] [Google Scholar]
- 17. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non‐ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. [DOI] [PubMed] [Google Scholar]
- 18. Garcia S, Canoniero M, Peter A, et al. Correlation of TIMI risk score with angiographic severity and extent of coronary artery disease in patients with non‐ST‐elevation acute coronary syndromes. Am J Cardiol. 2004;93:813–816. [DOI] [PubMed] [Google Scholar]
- 19. Mega JL, Morrow DA, Sabatine MS, et al. Correlation between the TIMI risk score and high‐risk angiographic findings in non‐ST‐elevation acute coronary syndromes: observations from the Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM‐PLUS) trial. Am Heart J. 2005;149:846–850. [DOI] [PubMed] [Google Scholar]
- 20. Gibler WB, Cannon CP, Blomkalns AL, et al. Practical implementation of the guidelines for unstable angina/non‐ST‐segment elevation myocardial infarction in the emergency department: a scientific statement from the American Heart Association Council on Clinical Cardiology (Subcommittee on Acute Cardiac Care), Council on Cardiovascular Nursing, and Quality of Care and Outcomes Research Interdisciplinary Working Group, in Collaboration With the Society of Chest Pain Centers. Circulation. 2005;111: 2699–2710. [DOI] [PubMed] [Google Scholar]
- 21. Hoenig MR, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina and non‐ST elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2010;(3):CD004815. [DOI] [PubMed] [Google Scholar]
- 22. Bavry AA, Kumbhani DJ, Rassi AN, Bhatt DL, Askari AT. Benefit of early invasive therapy in acute coronary syndromes: a meta‐analysis of contemporary randomized clinical trials. J Am Coll Cardiol. 2006;48:1319–1325. [DOI] [PubMed] [Google Scholar]
- 23. Bhatt DL, Roe MT, Peterson ED, et al. Utilization of early invasive management strategies for high‐risk patients with non‐ST‐segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA. 2004;292:2096–2104. [DOI] [PubMed] [Google Scholar]
- 24. de Winter RJ, Windhausen F, Cornel JH, et al. Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med. 2005;353:1095–1104. [DOI] [PubMed] [Google Scholar]
- 25. Hoenig MR, Doust JA, Aroney CN, et al. Early invasive versus conservative strategies for unstable angina & non‐ST‐elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2006;3:CD004815. [DOI] [PubMed] [Google Scholar]
- 26. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non‐ST‐segment elevation myocardial infarction– summary article: a report of the American College of Cardiology/ American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol. 2002;40:1366–1374. [DOI] [PubMed] [Google Scholar]
- 27. Kim JS, Kim J, Choi D, et al. Efficacy of high‐dose atorvastatin loading before primary percutaneous coronary intervention in ST‐segment elevation myocardial infarction: the STATIN STEMI trial. JACC Cardiovasc Interv. 2010;3:332–339. [DOI] [PubMed] [Google Scholar]
- 28. Murphy SA, Cannon CP, Wiviott SD, et al. Reduction in recurrent cardiovascular events with intensive lipid‐lowering statin therapy compared with moderate lipid‐lowering statin therapy after acute coronary syndromes from the PROVE IT‐TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy‐Thrombolysis In Myocardial Infarction 22) trial. J Am Coll Cardiol. 2009;54: 2358–2362. [DOI] [PubMed] [Google Scholar]
- 29. Gibson CM, Pride YB, Hochberg CP, et al. Effect of intensive statin therapy on clinical outcomes among patients undergoing percutaneous coronary intervention for acute coronary syndrome. PCI‐PROVE IT: A PROVE IT‐TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy‐Thrombolysis In Myocardial Infarction 22) Substudy. J Am Coll Cardiol 2009;54: 2290–2295. [DOI] [PubMed] [Google Scholar]
- 30. Pedersen TR, Cater NB, Faergeman O, et al. Comparison of atorvastatin 80 mg/day versus simvastatin 20 to 40 mg/day on frequency of cardiovascular events late (five years) after acute myocardial infarction (from the Incremental Decrease in End Points through Aggressive Lipid Lowering [IDEAL] trial). Am J Cardiol. 2010;106:354–359. [DOI] [PubMed] [Google Scholar]
- 31. Murphy SA, Cannon CP, Wiviott SD, et al. Effect of intensive lipid‐lowering therapy on mortality after acute coronary syndrome (a patient‐level analysis of the Aggrastat to Zocor and Pravastatin or Atorvastatin Evaluation and Infection Therapy‐Thrombolysis in Myocardial Infarction 22 trials). Am J Cardiol. 2007;100:1047–1051. [DOI] [PubMed] [Google Scholar]
- 32. De Denus S, Spinler SA. Early statin therapy for acute coronary syndromes. Ann Pharmacother. 2002;36:1749–1758. [DOI] [PubMed] [Google Scholar]
- 33. Peterson ED, Shah BR, Parsons L, et al. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–1055. [DOI] [PubMed] [Google Scholar]
- 34. Fox KA, Steg PG, Eagle KA, et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999‐2006. JAMA. 2007;297:1892–1900. [DOI] [PubMed] [Google Scholar]


