Abstract
Background:
Short sleep duration was reported to be associated with an increased risk of hypertension among adults. The present study aimed to investigate this association in children and adolescents.
Hypothesis:
Short sleep duration is related to higher risk of hypertension among children and adolescents.
Methods:
We conducted a cross‐sectional study of 4902 children and adolescents age 5 to 18 years. Blood pressure (BP) was measured at the research center and classified using the population‐based percentiles. Sleep duration and related information were determined through questionnaires.
Results:
The prevalence of hypertension and prehypertension were 20.3% and 15%, respectively. The median sleep duration was 8.77 ± 1.07 hours (mean ± standard deviation). A short sleep duration (<9 hours) was associated with a higher risk of hypertension when compared with the group sleeping longer (9–10 h), among boys age 11 to 14 years old (OR, 1.5; 95% CI, 1.04–2.15), adjusting for age, body mass index, waist circumference, and physical activity. The linear regression stratified by age indicated that for boys age 11 to 14 years the inverse association existed after adjustment with the coefficients −1.04 mm Hg and −0.55 mm Hg per hour of sleep for systolic BP and diastolic BP, respectively.
Conclusions:
Short sleep duration (<9 h) is independently associated with hypertension among Chinese boys age 11 to 14 years old. © 2011 Wiley Periodicals, Inc.
L. Zheng and X. Guo contributed equally to this work.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Hypertension and prehypertension have been found to be highly prevalent in children and adolescents in recent years.1, 2, 3, 4 High blood pressure (BP) in childhood is associated with target organ damage, notably left ventricular hypertrophy, which is an independent risk factor for cardiovascular disease among adults.5, 6 Children and adolescents with high BP may be at risk for hypertensive disease in adulthood,7, 8 contributing to adverse cardiovascular outcomes. Appropriate changes in lifestyle patterns would be able to decrease the later incidence and severity of cardiovascular diseases.9, 10
The association between sleep duration and BP has been the subject of multiple experimental and epidemiological studies. Both short and long sleep durations are associated with an increased risk of higher BP. Although the etiology is unclear, several studies indicate that the mechanisms are related to overactivity of the sympathetic nervous and rennin angiotensin aldosterone systems,11, 12, 13 alteration of the circadian rhythm,14, 15 and hormone concentrations.16, 17 Studies have generally reported that short sleep duration is strongly associated with hypertension in adults18, 19, 20, 21, 22, 23 except for 2 studies in the elderly.24, 25 The impact of sleep duration on BP may differ depending on age.26, 27
A few studies have investigated the relationship between sleep duration and high BP in children and adolescents, and have reported conflicting results.28, 29, 30, 31 Presently, there are scant reports on this relationship in Asian populations with large sample sizes. Therefore, we conducted this study to investigate the association between the prevalence of hypertension and different BP indexes [systolic BP (SBP) and diastolic BP (DBP)] with self‐reported sleep duration in a population of children and adolescents in Liaoning, northern China.
Methods
Study Population
The study was approved by the Ethics Committee of China Medical University. We conducted a cross‐sectional study from July 2010 to January 2011. A total of 5512 children and adolescents age 5 to 18 years from 12 schools in rural areas of Shenyang, Liaoning Province were recruited into the study by multistage sampling irrespective of their socioeconomic class. Informed parental consent was obtained in all cases. The final sample included 4902 students who were free of severe illnesses such as heart, kidney, or neurological diseases.
Blood Pressure
According to the standardized technique described by the American Heart Association,32 resting arterial BP was measured while the participant was in a seated position after 5 minutes of rest with the back supported and arms bared at the heart level. A mercury sphygmomanometer with an appropriate arm cuff length was used. Two measurements were taken with 2‐minute intervals and the average value was used in the analysis. Pulse pressure (PP) and mean arterial pressure (MAP) were calculated from the average SBP and DBP (PP = SBP − DBP,MAP = DBP + 1/3PP). BP was classified using the population‐based percentiles.32, 33 Normal BP was defined as SBP and/or DBP <90th percentile for age, sex, and height; prehypertension was defined as SBP and/or DBP ≥90th and <95th percentile for age, sex, and height, or if the SBP was more than 120 mmHg or DBP was more than 80 mmHg. Hypertension (HTN) was defined as SBP and/or DBP ≥95th percentile.
Sleep Duration
Sleep duration was determined for each participant by asking the participant's parent the following question, “How many hours of sleep does your child usually have in a day on average (including nocturnal sleep duration and nap duration)?” Parents were asked to answer the question with 1 digit after the decimal place allowed. Given that age‐specific effects on sleep duration exist, we categorized the participants into three age groups (5–10, 11–14, and >15 years) in accordance with their educational levels (primary, junior, and senior high school). Since the recommendations for sleep duration were established (for 5–10 years old: 10–11 h; for 11–14 years old: 9–10 h; for 15–18 years old: 8–9 h according to US reference33 and the recommendations of the Chinese government), we categorized children based on how different their sleep duration was from the recommended level; ie, <1 h less and >1 h more than recommended in each age group (for 5–10 years old: <10, 10–11, and ≥11 h; for 11–14 years old: <9, 9–10, and ≥10 h; and for 15–18 years old: <8, 8–9, and ≥9 h).
Covariates
Anthropometric measures including height, body weight, and waist circumference (WC) were evaluated by trained personnel using standard protocols. Height was measured using a portable stadiometer to the nearest 0.5 cm and body weight was measured using a professional scale to the nearest 100 g while the subjects were wearing light clothes without shoes. Body mass index (BMI) was calculated as the subject's weight (in kg) divided by the height (in m) squared. Detailed data on personal characteristics, such as age and gender were collected using a questionnaire.
Statistical Analysis
Data are expressed as the mean and standard deviation (SD) (continuous variables) or numbers and percentages (categorical variables). We performed analysis of variance (ANOVA) test (Dunnett method was used for pairwise comparisons) and χ 2 test for continuous and categorical variables, respectively. Univariate and multivariate regression analyses were preformed to test the association between sleep duration and BP. Polynomial in regression analysis was also performed. First a linear model was built as: BP = a + (b × Sleep duration), where a and b are calculated regression parameters and BP includes SBP and DBP. In order to identify the rate of changes in BP over time, second‐degree regression analysis was performed for each subject to match available BP values to the formula: BP = a + (b × sleep duration) + c × (sleep duration)2, where c is a third calculated quantity, the “acceleration parameter,” that measures the rate of changes in BP. The null hypothesis is that the rate is constant; ie, mean c is zero. One‐sample t test was performed to testify whether c values are significantly different from zero. We further performed curve fitting of quadratic model and calculated coefficients of determination (R2) categorized by sex and age groups. All of the statistical analyses were calculated with SPSS version 17.0 software (SPSS, Inc., Chicago, IL), and P values <0.05 were considered to be statistically significant.
Results
The overall response rate in the present study was 88.9%. Of the 4902 participants (48% girls and 52% boys; mean age 10.93 years; SD 2.67 years), 20.3% had hypertension and 15% had prehypertension. Mean ± SD as well as interquartile ranges (Q) of sleep duration were calculated. On average, the participants slept 8.77 ± 1.07 hours (including nocturnal sleep and nap duration). The mean levels of sleep duration were 9.0 ± 0.9 hours (Q 2 h), 8.7 ± 1.1 hours (Q 1 h), and 8.1 ± 1.2 hours (Q 2 h) for male participants age 5 to 10 years, 11 to 14 years, and 15 years or older, respectively. The mean levels of sleep duration were 9.0 ± 0.9 hours (Q 2 h), 8.7 ± 1.1 hours (Q 1 h), and 7.8 ± 1.3 hours (Q 1.5 h) for female participants age 5 to 10 years, 11 to 14 years, and 15 years or older, respectively. Sleep duration ranged from 6 to 12 hours in each age group by sex.
Table 1 presents the characteristics of the male participants by age and sleep duration. Among boys age 5 to 10 years, participants sleeping <10 hours had lower mean DBP and MAP levels than the participants sleeping 10 to 11 hours. For boys age 11 to 14 years, sleep duration <9 hours was associated with older age, larger BMI, and higher mean levels of all 4 BP indexes (SBP, DBP, PP, and MAP). In the group 15 to 18 years old, participants sleeping 8 hours or less were associated with higher DBP levels using 8 to 9 hours as reference.
Table 1.
Baseline Characteristics of Male Subjects Categorized by Sleep Duration and Age (N = 2547)
| Sleep Duration (h) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 5–10 years old (n = 1182) | 11–14 years old (n = 1116) | 15–18 years old (n = 249) | |||||||
| <10 (n = 879) | 10–11 (n = 265) | ≥11 (n = 38) | <9 (n = 543) | 9–10 (n = 336) | ≥10 (n = 237) | <8 (n = 81) | 8–9 (n = 103) | ≥9 (n = 65) | |
| Age (y) | 8.5 ± 1.2 | 8.5 ± 1.2 | 8.8 ± 1.4 | 12.8 ± 1.1a | 12.3 ± 1.1 | 12.4 ± 1.1 | 15.3 ± 0.6 | 15.4 ± 0.6 | 15.3 ± 0.6 |
| BMI (kg/m2) | 18.1 ± 3.8 | 17.8 ± 3.4 | 17.7 ± 3.2 | 20.8 ± 4.7a | 19.8 ± 4.1 | 20.1 ± 4.2 | 21.4 ± 3.9 | 21.4 ± 4.0 | 21.2 ± 4.0 |
| WC (cm) | 58.7 ± 9.1 | 58.0 ± 10.0 | 57.3 ± 8.5 | 69.4 ± 12.8a | 68.6 ± 38.4 | 67.4 ± 11.6 | 72.2 ± 11.0 | 73.1 ± 10.3 | 74.0 ± 10.7 |
| SBP (mmHg) | 103.5 ± 11.5 | 104.8 ± 12.0 | 101.7 ± 10.5 | 115.3 ± 13.1a | 112.1 ± 13.1 | 111.0 ± 13.5 | 119.3 ± 10.7 | 119.6 ± 11.8 | 120.3 ± 10.4 |
| DBP (mmHg) | 62.7 ± 9.8a | 64.9 ± 9.7 | 62.9 ± 8.6 | 69.6 ± 9.5a | 68.0 ± 9.1 | 67.7 ± 10.4 | 74.1 ± 8.3a | 70.3 ± 9.1 | 73.2 ± 6.6 |
| MAP (mmHg) | 76.3 ± 9.6a | 78.2 ± 9.7 | 75.8 ± 8.6 | 84.8 ± 9.6a | 82.7 ± 9.2 | 82.2 ± 10.6 | 89.2 ± 8.0 | 86.8 ± 8.8 | 88.9 ± 7.0 |
| PP (mmHg) | 40.8 ± 8.7 | 39.9 ± 8.7 | 38.8 ± 7.5 | 45.7 ± 10.6a | 44.0 ± 11.1 | 43.3 ± 9.8 | 45.2 ± 9.2a | 49.3 ± 10.4 | 47.1 ± 8.6 |
| Physical activity, times/week | |||||||||
| None | 21 (2.4) | 10 (3.8) | 2 (5.3) | 8 (1.5) | 10 (3.0) | 4 (1.7) | 3 (3.7) | 5 (4.9) | 3 (4.6) |
| 1–4 | 514 (58.5) | 173 (65.3) | 24 (63.2) | 294 (54.1) | 160 (47.6) | 144 (60.8) | 47 (58.0) | 66 (64.1) | 30 (46.2) |
| 5 or more | 344 (39.1)b | 82 (30.9) | 12 (31.6) | 241 (44.4) | 166 (49.4) | 89 (37.6)b | 31 (38.3) | 32 (31.1) | 32 (49.2) |
| Sleep duration (h/d) | 8.6 ± 0.6a | 10.0 ± 0.1 | 11.3 ± 0.5a | 7.8 ± 0.6a | 9.0 ± 0.1 | 10.3 ± 0.6a | 6.8 ± 0.6a | 8.1 ± 0.2 | 9.7 ± 0.7a |
Abbreviations: ANOVA, analysis of variance; BMI, body mass index; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; SBP, systolic blood pressure; SD, standard deviation; WC, waist circumference. Data are expressed as the mean ± SD or as n (%). Significantly different from the referent group of 10 to 11 hours for 5 to 10 year‐olds; 9 to 10 hours for 11 to 14 year‐olds; and 8 to 9 hours for 15 to 18 year‐olds:
P < 0.05 from ANOVA test using Dunnett method,
P < 0.05 from x2 analysis.
Table 2 presents the characteristics of the female participants by age and sleep duration. For girls age 11 to 14 years, sleeping <9 hours was associated with older age compared to those sleeping 9 to 10 hours. No significance was observed between the longer sleep duration and the reference duration across the 3 age groups.
Table 2.
Baseline Characteristics of Female Subjects Categorized by Sleep Duration and Age (N = 2355)
| Sleep duration (h) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 5–10 years old (n = 1094) | 11–14 years old (n = 1037) | 15–18 years old (n = 224) | |||||||
| <10 (n = 801) | 10–11 (n = 260) | ≥11 (n = 33) | <9 (n = 518) | 9–10 (n = 283) | ≥10 (n = 236) | <8 (n = 103) | 8–9 (n = 68) | ≥9 (n = 53) | |
| Age (y) | 8.4 ± 1.3 | 8.5 ± 1.3 | 8.6 ± 1.2 | 12.8 ± 1.1a | 12.4 ± 1.1 | 12.3 ± 1.1 | 15.4 ± 0.7 | 15.2 ± 0.5 | 15.3 ± 0.6 |
| BMI (kg/m2) | 17.0 ± 3.3 | 17.3 ± 3.1 | 17.4 ± 2.4 | 19.5 ± 3.3 | 19.2 ± 3.2 | 18.9 ± 3.2 | 21.2 ± 3.1 | 21.5 ± 4.9 | 20.8 ± 3.7 |
| WC (cm) | 55.3 ± 7.6 | 55.8 ± 7.7 | 57.2 ± 6.4 | 64.5 ± 8.0 | 63.3 ± 7.8 | 63.8 ± 8.3 | 67.4 ± 6.9 | 68.2 ± 7.0 | 67.5 ± 7.5 |
| SBP (mmHg) | 101.5 ± 11.6 | 102.2 ± 11.6 | 100.9 ± 14.0 | 113.4 ± 12.5 | 111.4 ± 13.5 | 110.8 ± 13.6 | 115.2 ± 11.4 | 118.5 ± 11.6 | 116.9 ± 11.9 |
| DBP (mmHg) | 63.0 ± 9.0 | 62.4 ± 8.6 | 61.4 ± 9.9 | 70.9 ± 9.3 | 69.6 ± 9.8 | 68.6 ± 11.3 | 72.6 ± 6.7 | 74.3 ± 9.4 | 73.8 ± 6.6 |
| MAP (mmHg) | 75.9 ± 9.2 | 75.6 ± 8.7 | 74.6 ± 10.4 | 85.0 ± 9.6 | 83.5 ± 10.1 | 82.6 ± 11.4 | 86.8 ± 7.6 | 89.0 ± 9.5 | 88.2 ± 7.5 |
| PP (mmHg) | 38.5 ± 7.8 | 39.8 ± 9.1 | 39.5 ± 9.9 | 42.6 ± 9.1 | 41.8 ± 10.3 | 42.3 ± 8.7 | 42.7 ± 8.5 | 44.3 ± 7.7 | 43.1 ± 9.6 |
| Physical activity, times/week | |||||||||
| None | 24 (3) | 7 (2.7) | 016 (3.1) | 4 (1.4) | 6 (2.5) | 1 (1) | 4 (5.9) | 4 (7.5) | |
| 1–4 | 486 (60.7) | 149 (57.3) | 22 (66.7) | 312 (60.2) | 171 (60.4) | 149 (63.1) | 71 (68.9) | 36 (52.9) | 30 (56.6) |
| 5 or more | 291 (36.3) | 104 (40) | 11 (33.3) | 190 (36.7) | 108 (38.2) | 81 (34.3) | 31 (30.1)b | 28 (41.2) | 19 (35.8) |
| Sleep duration (h/d) | 8.5 ± 0.6a | 10.0 ± 0.1 | 11.3 ± 0.5a | 7.8 ± 0.5a | 9.0 ± 0.1 | 10.3 ± 0.6a | 6.7 ± 0.5a | 8.1 ± 0.2 | 9.6 ± 0.9a |
Abbreviations: ANOVA, analysis of variance; BMI, body mass index; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; SBP, systolic blood pressure; SD, standard deviation; WC, waist circumference. Data are expressed as the mean ± SD or as n (%). Significantly different from the referent group of 10 to 11 hours for 5 to 10 year‐olds; 9 to 10 hours for 11 to 14 year‐olds; and 8 to 9 hours for 15 to 18 year‐olds:
P < 0.05 from ANOVA test using Dunnett method,
P < 0.05 from x2 analysis.
Figure 1 presents the prevalence of hypertension by sex and age. Girls sleeping 8 to 9 hours had a higher prevalence of hypertension than their male counterparts in the group 15 to 18 years old (P = 0.024).
Figure 1.
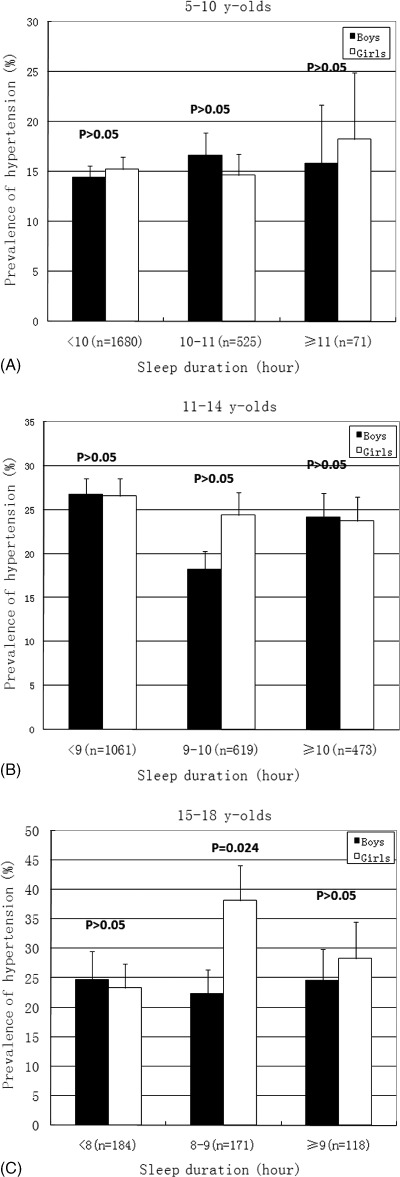
Prevalence of hypertension by sex and sleep duration among 3 age groups. (A) 5 to 10 years old; (B) 11 to 14 years old; and (C) 15 to 18 years old. Error bars represent standard errors. P value for comparison between boys and girls using chi‐square analysis.
Table 3 presents the results of the logistic regression analyses. For boys age 11 to 14 years, a short sleep duration (<9 h) was significantly associated with increased odds of hypertension in comparison to those sleeping 9 to 10 hours (OR, 1.5; 95% CI, 1.04–2.15) after adjusting for age, BMI, WC, and physical activity. For girls age 15 to 18 years old, participants sleeping <8 hours had significantly lower odds of hypertension compared with the participants sleeping 8 to 9 hours (OR, 0.46; 95% CI, 0.23–0.94), after adjustment.
Table 3.
Logistic Regressions of Hypertension Prevalence According to Categories of Sleep Duration
| Odds Ratio (95% confidence interval) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 5–10 years old (n = 2276) | 11–14 years old (n = 2153) | 15–18 years old (n = 473) | |||||||
| <10 (n = 1680) | 10–11 (n = 525) | ≥11 (n = 71) | <9 (n = 1061) | 9–10 (n = 619) | ≥10 (n = 473) | <8 (n = 184) | 8–9 (n = 171) | ≥9 (n = 118) | |
| Boys | |||||||||
| Unadjusted | 0.85 (0.58–1.23) | 1 (ref) | 0.94 (0.37–2.39) | 1.64 (1.17–2.30)b | 1 (ref) | 1.43 (0.95–2.15) | 1.14 (0.58–2.26) | 1 (ref) | 1.14 (0.55–2.36) |
| Adjusteda | 0.81 (0.55–1.19) | 1 (ref) | 0.97 (0.36–2.56) | 1.50 (1.04–2.15)b | 1 (ref) | 1.43 (0.93–2.20) | 1.01 (0.48–2.10) | 1 (ref) | 1.27 (0.57–2.81) |
| Girls | |||||||||
| Unadjusted | 1.05 (0.71–1.56) | 1 (ref) | 1.30 (0.50–3.35) | 1.13 (0.81–1.57) | 1 (ref) | 0.97 (0.64–1.45) | 0.49 (0.25–0.96)b | 1 (ref) | 0.64 (0.30–1.38) |
| Adjusteda | 1.07 (0.72–1.59) | 1 (ref) | 1.30 (0.50–3.34) | 1.15 (0.81–1.64) | 1 (ref) | 0.96 (0.63–1.47) | 0.46 (0.23–0.94)b | 1 (ref) | 0.65 (0.29–1.45) |
Abbreviations: BMI, body mass index; WC, waist circumference.
Adjusted for age, BMI, WC, and physical activity.
P < 0.05.
Table 4 presents the results from the linear regression models. We found that for male participants age 11 to 14 years, there were significant inverse associations (P < 0.05) between sleep duration and either SBP (β = −1.04 mm Hg per 1 h of sleep) or DBP (β = −0.55 mm Hg per 1 h of sleep). For boys age 5 to 10 years, a positive association was observed.
Table 4.
Association Between Sleep Duration (per 1 hour increase) and Different Blood Pressure Indexes (SBP and DBP)
| SBP | DBP | |||
|---|---|---|---|---|
| Beta (95% CI) | P Value | Beta (95% CI) | P Value | |
| Boys | ||||
| 5–10 years old | 0.60 (−0.09 to 1.30) | 0.090 | 0.82 (0.21 to 1.43) | 0.008 |
| 11–14 years old | −1.04 (−1.65 to −0.42) | 0.001 | −0.55 (−1.05 to −0.05) | 0.030 |
| 15–18 years old | 0.62 (−0.40 to 1.64) | 0.230 | −0.30 (−1.14 to 0.55) | 0.493 |
| Girls | ||||
| 5–10 years old | −0.13 (−0.88 to 0.62) | 0.737 | −0.36 (−0.94 to 0.21) | 0.212 |
| 11–14 years old | −0.43 (−1.13 to 0.27) | 0.225 | −0.55 (−1.10 to 0.00) | 0.050 |
| 15–18 years old | 0.44 (−0.70 to 1.58) | 0.451 | 0.13 (−0.64 to 0.90) | 0.736 |
Abbreviations: BMI, body mass index; CI, confidence interval; DBP, diastolic blood pressure; SBP, systolic blood pressure; WC, waist circumference. Adjusted for age, BMI, WC, and physical activity.
In the second‐degree regression analysis, mean values of acceleration parameter c were all >0. There was overall a significant acceleration in changes of BP (all P < 0.001). R2 values in curve fitting of the quadratic model in each age group by sex were <0.5 (all P < 0.001).
Discussion
In a cross‐sectional study of 4902 children and adolescents, we mainly found that among boys age 11 to 14 years, a short sleep duration (<9 h) was associated with a higher risk of prevalent hypertension than a sleep duration of 9 to 10 hours. No relationship was observed between longer sleep duration (more than the reference duration) and hypertension in both genders.
Consistent with other studies,1, 2, 3, 4 we observed a high prevalence of hypertension and prehypertension among children and adolescents. The average sleep durations in the present study, as categorized by age, were lower than the US references33 and the recommendations of the Chinese government (at least 10 h for children <10 years old, 9 h for 11–14 years old, and 8 h for >15 years old).
There is substantial evidence regarding the link between sleep duration and hypertension in adults.18, 19, 20, 21, 22, 23, 34, 35 Children and adolescents have their own lifestyle characteristics that differ from adults. Several studies investigated the predictive effect of sleep duration on the risk of hypertension in children and adolescents and reported conflicting results.28, 29, 30, 31, 36, 37 In a recent study on 238 adolescents age 13 to 16 years,30 the odds of prehypertension was increased 2.5‐fold for short sleep (<6.5 h) adjusted for gender, BMI percentile, and socioeconomic status. However, 3 other studies observed no independent association between sleep duration and BP in different age groups (3–10 years, 10–12 years, and 16–19 years).29, 31, 37 The mechanism underlying the association between sleep duration and hypertension is not fully understood. A link between insufficient sleep and metabolic changes, such as reduced glucose tolerance, have been considered to play important roles in the complicated mechanisms leading to hypertension.14, 15, 16, 17
A novel finding in the present study is that short sleep duration was only associated with a higher risk of hypertension among boys. Previously, short sleep duration was found to be associated with a higher risk of hypertension among female adults, and the proposed mechanisms included menopausal theory and differences in body composition.21, 23, 38 However, an opposite gender‐specific association could still exist among children, since the endocrine status and psychosocial states are dramatically different between children and adults. Previous studies on children and adolescents rarely performed gender‐specific analyses to test this hypothesis. Only Bayer et al mentioned that the effect of sleep duration on BP tended to be stronger in boys, but this effect did not result in a significant outcome in any of the ancillary analyses.29 More investigations are needed to understand the underlying mechanisms. Interestingly, we observed that there was an inverse association only in participants age 11 to 14 years, which might result from a higher sensitivity of the body to the sleep duration during this developmental period.
In addition, we found short sleep duration (<8 h) was a protective factor for hypertension among girls age 15 to 18 years, and there was a positive association between sleep duration and DBP among boys age 5 to 10 years. These disparate phenomena could exist because endocrine status and life habits differ markedly in different sexes and age groups. However, it should be noticed that there were very few individuals in these 2 subgroups.
In the second‐degree regression analysis, there was overall a significant acceleration in changes of BP, indicating that the rate of BP change was not constant. However, the results from curve fitting of the quadratic model were suboptimal. This might be explained by our limited range of sleep duration (6–12 h) and small sample size in some subgroups of sleep duration.
There are limitations in the present study. First, information about sleep duration was self‐reported by the parents of the participants. Although good correlations between objectively measured and the self‐reported durations in children have been observed,39, 40 this may still compromise the accuracy of the study. Second, there were very few 5 to 10‐year‐olds in our study who slept at least 11 hours and there were few 15 to 18‐year‐olds overall, thus yielding a limited statistical power to test the association between sleep duration and hypertension in these subgroups. Third, our results are based on a cross‐sectional design. Thus, we could not define a causal association between sleep duration and hypertension. In addition, residual confounding could also occur inside the age categories used, and there might be important confounders that were not taken into account in our analysis, because research on this issue among children and adolescents is relatively limited.
Conclusion
In summary, the effect of short sleep duration on BP, which was previously documented among adults, was observed among Chinese boys age 11 to 14 years. The odds of hypertension were raised 1.5‐fold for male participants sleeping 9 hours or less compared to those sleeping 9 to 10 hours. Further research is needed to clarify the mechanisms of this gender‐specific relationship with better control for confounders in a prospective longitudinal study before causality can be determined.
References
- 1. Rafraf M, Gargari BP, Safaiyan A. Prevalence of prehypertension and hypertension among adolescent high school girls in Tabriz, Iran. Food Nutr Bull. 2010;31:461–465. [DOI] [PubMed] [Google Scholar]
- 2. Rosa ML, Fonseca VM, Oigman G, et al. Arterial prehypertension and elevated pulse pressure in adolescents: prevalence and associated factors. Arq Bras Cardiol. 2006;87:46–53. [DOI] [PubMed] [Google Scholar]
- 3. Moore WE, Eichner JE, Cohn EM, et al. Blood pressure screening of school children in a multiracial school district: the Healthy Kids Project. Am J Hypertens. 2009;22:351–356. [DOI] [PubMed] [Google Scholar]
- 4. Ejike CE, Ugwu CE, Ezeanyika LU. Variations in the prevalence of point (pre)hypertension in a Nigerian school‐going adolescent population living in a semi‐urban and an urban area. BMC Pediatr. 2010;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McNiece KL, Gupta‐Malhotra M, Samuels J, et al. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National High Blood Pressure Education Program Working Group staging criteria. Hypertension. 2007;50:392–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vakili BA, Okin PM, Devereux RB. Prognostic implications of left ventricular hypertrophy. Am Heart J. 2001;141:334–341. [DOI] [PubMed] [Google Scholar]
- 7. Tirosh A, Afek A, Rudich A, et al. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension. 2010;56:203–209. [DOI] [PubMed] [Google Scholar]
- 8. Falkner B, Gidding SS, Portman R, et al. Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics. 2008;122:238–242. [DOI] [PubMed] [Google Scholar]
- 9. Massin M, Vandoorne C, Coremans C, et al. Preventive cardiology: strategies in children. Rev Med Liege. 2002;57:207–212. [PubMed] [Google Scholar]
- 10. Armstrong N, Balding J, Gentle P, et al. Estimation of coronary risk factors in British schoolchildren: a preliminary report. Br J Sports Med. 1990;24:61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tochikubo O, Ikeda A, Miyajima E, et al. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension. 1996;27:1318–1324. [DOI] [PubMed] [Google Scholar]
- 12. Lusardi P, Mugellini A, Preti P, et al. Effects of a restricted sleep regimen on ambulatory blood pressure monitoring in normotensive subjects. Am J Hypertens. 1996;9:503–505. [DOI] [PubMed] [Google Scholar]
- 13. Lusardi P, Zoppi A, Preti P, et al. Effects of insufficient sleep on blood pressure in hypertensive patients: a 24‐h study. Am J Hypertens. 1999;12:63–68. [DOI] [PubMed] [Google Scholar]
- 14. Scheer FA, Van Montfrans GA, van Someren EJ, et al. Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension. Hypertension. 2004;43:192–197. [DOI] [PubMed] [Google Scholar]
- 15. Goncharuk VD, Van Heerikhuize J, Dai JP, et al. Neuropeptide changes in the suprachiasmatic nucleus in primary hypertension indicate functional impairment of the biological clock. J Comp Neurol. 2001;431:320–330. [DOI] [PubMed] [Google Scholar]
- 16. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. [DOI] [PubMed] [Google Scholar]
- 17. Spiegel K, Tasali E, Penev P, et al. Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–850. [DOI] [PubMed] [Google Scholar]
- 18. Gangwisch JE, Heymsfield SB, Boden‐Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–839. [DOI] [PubMed] [Google Scholar]
- 19. Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–1014. [DOI] [PubMed] [Google Scholar]
- 20. Kotani K, Saiga K, Sakane N, et al. Sleep status and blood pressure in a healthy normotensive female population. Int J Cardiol. 2007;125:425–427. [DOI] [PubMed] [Google Scholar]
- 21. Cappuccio FP, Stranges S, Kandala NB, et al. Gender‐specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kawabe H, Saito I. Does short sleep duration in daily life affect morning home blood pressure? Evaluation in Japanese people. Clin Exp Hypertens. 2008;30:183–190. [DOI] [PubMed] [Google Scholar]
- 23. Stang A, Moebus S, Mohlenkamp S, et al. Gender‐specific associations of short sleep duration with prevalent hypertension. Hypertension. 2008;51:e15–e16. [DOI] [PubMed] [Google Scholar]
- 24. van den Berg JF, Tulen JH, Neven AK, et al. Sleep duration and hypertension are not associated in the elderly. Hypertension. 2007;50:585–589. [DOI] [PubMed] [Google Scholar]
- 25. Lima‐Costa MF, Peixoto SV, Rocha FL. Usual sleep duration is not associated with hypertension in Brazilian elderly: the Bambui Health Aging Study (BHAS). Sleep Med. 2008;9:806–807. [DOI] [PubMed] [Google Scholar]
- 26. Haas DC, Foster GL, Nieto FJ, et al. Age‐dependent associations between sleep‐disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation. 2005;111:614–621. [DOI] [PubMed] [Google Scholar]
- 27. Kim J, Jo I. Age‐dependent association between sleep duration and hypertension in the adult Korean population. Am J Hypertens. 2010;23:1286–1291. [DOI] [PubMed] [Google Scholar]
- 28. Sampei M, Dakeishi M, Wood DC, et al. Impact of total sleep duration on blood pressure in preschool children. Biomed Res. 2006;27:111–115. [DOI] [PubMed] [Google Scholar]
- 29. Bayer O, Neuhauser H, von Kries R. Sleep duration and blood pressure in children: a cross‐sectional study. J Hypertens. 2009;27:1789–1793. [DOI] [PubMed] [Google Scholar]
- 30. Javaheri S, Storfer‐Isser A, Rosen CL, et al. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118:1034–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shaikh WA, Patel M, Singh S. Association of sleep duration with arterial blood pressure profile of Gujarati Indian adolescents. Indian J Community Med. 2010;35:125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents . The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 33. Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–307. [DOI] [PubMed] [Google Scholar]
- 34. Salgado CM, Carvalhaes JT. Arterial hypertension in childhood. J Pediatr. 2003;79(suppl 1):S115–S124. [DOI] [PubMed] [Google Scholar]
- 35. Heslop P, Smith GD, Metcalfe C, et al. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all‐cause mortality in working men and women. Sleep Med. 2002;3:305–314. [DOI] [PubMed] [Google Scholar]
- 36. Sung RYT, Choi KC, So H‐K, et al. Oscillometrically measured blood pressure in Hong Kong Chinese children and associations with anthropometric parameters. J Hypertens. 2008;4: 678–684. [DOI] [PubMed] [Google Scholar]
- 37. Wells JC, Hallal PC, Reichert FF, et al. Sleep patterns and television viewing in relation to obesity and blood pressure: evidence from an adolescent Brazilian birth cohort. Int J Obes (Lond). 2008;32:1042–1049. [DOI] [PubMed] [Google Scholar]
- 38. St‐Onge MP, Perumean‐Chaney S, Desmond R, et al. Gender Differences in the Association between Sleep Duration and Body Composition: The Cardia Study. Int J Endocrinol. 2010;2010: 726071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sekine M, Chen X, Hamanishi S, et al. The validity of sleeping hours of healthy young children as reported by their parents. J Epidemiol. 2002;3:237–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lauderdale DS, Knutson KL, Yan LL, et al. Self‐reported and measured sleep duration: how similar are they? Epidemiology. 2008;6:838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]


