Abstract
Background:
In a prospective cohort of consecutive acute coronary syndrome (ACS) patients, we compared the adherence rate of statin usage and mortality rate during a median follow‐up of 23 months.
Hypothesis:
Adherence to statin therapy after acute coronary syndrome affects mortality rate.
Methods:
We analyzed ACS patients (N = 1969; age, 65.9 ± 11.8 years; female 30.4%) who underwent angiography between March 2006 and March 2008. The postdischarge usage of statins was based on the purchase register of the Social Insurance Institution of Finland. The death rate was verified from Statistics Finland.
Results:
At discharge, the rate of statin prescription to patients was 95.4% (n = 1878). When comparing adherent patients (n = 1200; 61.7%), who purchased the medication systematically until the end of the median 23‐month follow‐up, with nonadherent patients (n = 94; 4.8%), who did not use the medication at all, there was a vast difference in absolute death rate between the groups: 4.9% vs 14.9%, respectively (P < 0.001). We conducted Cox proportional hazards model with ACS type, cerebrovascular attack, diabetes, age, 3‐artery disease, and cancer as adjusted confounders. Compared with regular statin users, nonusers were associated with a >2× increased hazard ratio of mortality (hazard ratio: 2.70, 95% confidence interval: 1.49‐4.90, P = 0.001).
Conclusions:
Statin medication is essential for discharged ACS patients. They should be strongly encouraged to purchase and use it.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Remarkable progress has been made in therapeutic procedures in the treatment of acute coronary syndrome (ACS), which has led to excellent primary results. However, care after discharge from the hospital gets much less attention. In the repertoire of ACS patients' medication, 3‐hydroxy‐3‐methyl‐glutaryl‐CoA‐reductase inhibitors (statins) are the single most important antiatherosclerotic drugs. They stabilize plaques and reduce cardiovascular morbidity and mortality.1, 2 Guidelines recommend initiating statins in all ACS patients without contraindications during the first treatment period.2, 3 Yet regardless of the overwhelming evidence of the benefits of statins, at least 5% to 20%4, 5 of the patients do not start the medication, and later on the rate of usage even decreases.5, 6, 7, 8 Patients' adherence to medication may be high in clinical trials, but in clinical practice it is unsatisfactory.9 Reasons for nonadherence are multiple. True side effects explain part of it,9, 10 but also, for example, negative media coverage may be very important. The impact of nonadherence to statins on mortality seems evident but is still scarcely studied,9, 10, 11 and the problem of adherence has been examined mainly in older populations.5, 7, 12, 13 Furthermore, many adherence analyses date back to the 1990s and early 2000s, and the general public's knowledge of the benefits (and possible side effects) of statins has increased since then.12, 13 Therefore, to investigate the relationship between adherence to statin therapy and mortality, we analyzed consecutive ACS patients who underwent coronary angiography in a recent, prospective setting. Moreover, we wanted to separate primary and secondary adherence.
Methods
Between March 2006 and March 2008, a total of 5809 consecutive patients were assigned for coronary angiography in the Helsinki University Central Hospital. Data collected for this prospective Genetic Predisposition of Coronary Artery Disease (Corogene) study register included comprehensive information gathered from all patient records and a 2‐page patient questionnaire incorporating medical history, current condition, cardiovascular risk factors, medications, and electrocardiogram, echocardiography, and coronary angiogram results.14 This material included 2091 patients with ACS, defined as an episode of typical chest pain for ischemia and >50% stenosis in ≥1 coronary artery. The electrocardiogram had to show typical ischemic changes for uns angina pectoris (UA), non–ST‐elevation myocardial infarction (NSTEMI), or ST‐elevation myocardial infarction (STEMI).2, 15 All ACS patients were treated with standard drug regimens and procedures.2, 15 The distribution of diagnoses among these ACS patients was as follows: UA, 11% (n = 214); NSTEMI, 54.3% (n = 1056); and STEMI, 34.7% (n = 675).
The information on medication usage is based on the Finnish Prescription Register maintained by the Social Insurance Institution of Finland,16 covering all the patients' medication purchases between January 1, 2005, and March 31, 2009. Causes of death were obtained from Statistics Finland and the follow‐up lasted until March 31, 2009, or until the patient's death.
Detailed information about adherence calculations is provided in supplemental online data. In brief, patients were divided into 3 groups according to the number and interval of purchases as well as the initiation of medication (Figure 1). To assess primary adherence (filling of the first prescription), we excluded patients who had purchased statins before the index date (n = 780), yielding us 1099 statin‐naïve patients by the time of the coronary angiography. Secondary adherence (continuation of existing medication) was based on the continuation and regularity of medication purchases during the follow‐up. The impact of statin usage was assessed by comparing death rates between different groups.
Figure 1.
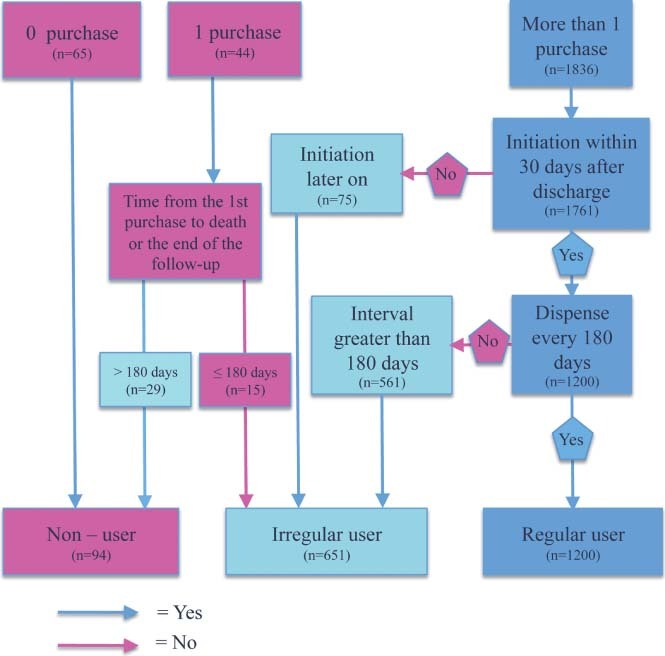
Classification of patients as regular statin users, irregular statin users, and nonusers.
All patients gave signed informed consent. The Ethics Committee of the Hospital District of Helsinki and Uusimaa, Helsinki, Finland, approved the research protocol. This study complies with the Declaration of Helsinki.
Statistical Analysis
Numbers are given as mean ± SD, median with interquartile range (IQR; 25–75 percentiles), or percentages. Categorical variables between different groups were analyzed with cross‐tabulation and χ 2 analyses or Fisher exact test where appropriate. Normally distributed continuous scale variables (body mass index, age, and cholesterol levels) were analyzed with independent t test and 1‐way ANOVA where appropriate. To adjust for differences between various groups, we conducted multivariate Cox proportional hazards models. We chose prior myocardial infarction (MI), comorbidities (cerebrovascular attack [CVA], peripheral vascular disease, cancer, kidney disease, and arrhythmia), prior procedures (percutaneous coronary intervention, coronary artery bypass grafting), severity of disease (3‐artery disease), ACS type, medications (acetylsalicylic acid, angiotensin blockers, angiotensin‐converting enzyme inhibitors, clopidogrel, and β‐blockers), cholesterol levels, body mass index, hypertension, diabetes mellitus (DM), age, sex, and smoking as candidate variables for Cox proportional hazards models. Final variables were chosen by the significance level of P ≤ 0.05 for each variable in different regression models. Hazard ratios (HR) with their 95% confidence intervals (CI) are reported. All tests were 2‐sided and used a significance level of 0.05. All statistical analyses were conducted with PASW Statistics version 18.0 (SPSS Inc., Chicago, IL).
Results
There were 2091 consecutive ACS patients in the Corogene database, and we had complete data for 2018 patients (97%). Of the latter, 1969 (98%) patients were discharged alive and 1878 (95%) with a prescription for statins according to hospital medical charts. Twenty‐four patients (1.2%) died during the first month after discharge. The overall mortality rate from discharge until the end of the follow‐up among patients who had a prescription at discharge was 7.2% (n = 136) vs 24.4% (n = 22) among patients who did not get a prescription (HR: 0.47, 95% CI: 0.30‐0.75, P = 0.001).
For comparative purposes, the 1945 patients alive 1 month after discharge form the cohort for the analyses of both secondary adherence for statins and the impact of primary adherence on mortality. Their baseline characteristics at the time of angiography are shown in the Table 1.
Table 1.
Baseline Characteristics of the Patient Cohort: Regular Statin Users, Irregular Users, and Nonusers
| Valid Cases | All | Statin Users | Irregular Users | Nonusers | P Value | |
|---|---|---|---|---|---|---|
| Patients, n (%) | 1945 | 1945 | 1200 (61.7) | 651 (33.5) | 94 (4.8) | |
| Age, y, mean ± SD | 1945 | 65.6 ± 11.8 | 65.2 ± 11.7 | 66.1 ± 11.6 | 68.4 ± 13.3 | 0.011 |
| Female sex | 1945 | 30.1 | 29.9 | 30.3 | 31.9 | 0.684 |
| BMI, mean ± SD | 1929 | 27.5 ± 4.8 | 27.4 ± 4.8 | 27.6 ± 4.8 | 27.1 ± 4.7 | 0.614 |
| Cholesterol levels at admission (mmol/L) | ||||||
| fP‐Cholesterol, mean ± SD | 1608 | 4.33 ± 1.09 | 4.35 ± 1.09 | 4.32 ± 1.10 | 4.16 ± 0.99 | 0.332 |
| fP‐LDL‐C, mean ± SD | 1543 | 2.40 ± 0.89 | 2.42 ± 0.89 | 2.40 ± 0.91 | 2.29 ± 0.82 | 0.475 |
| fP‐HDL‐C, mean ± SD | 1608 | 1.24 ± 0.36 | 1.24 ± 0.35 | 1.24 ± 0.39 | 1.22 ± 0.38 | 0.892 |
| Risk factors and prior procedures | ||||||
| Smoker | 1928 | 31.6 | 30.8 | 34.5 | 23.1 | 0.098 |
| Ex‐smoker | 1928 | 32.2 | 31.7 | 32.2 | 32.4 | 0.365 |
| Hypertension | 1945 | 65.6 | 64.4 | 68.2 | 61.7 | 0.607 |
| DM | 1945 | 22.8 | 19.8 | 27.8 | 26.6 | 0.034 |
| Dyslipidemia | 1945 | 71.1 | 70.2 | 75.1 | 54.3 | 0.002 |
| Prior MI | 1926 | 20.4 | 18.6 | 24.3 | 21.5 | 0.050 |
| Prior PCI | 1945 | 11.5 | 11.0 | 12.4 | 10.6 | 0.869 |
| Prior CABG | 1945 | 9.6 | 9.2 | 10.4 | 9.6 | 0.903 |
| Vessel status | ||||||
| 1‐artery disease | 1945 | 41.1 | 42.2 | 38.1 | 47.9 | 0.861 |
| 2‐artery disease | 1945 | 26.1 | 25.8 | 26.4 | 26.6 | 0.861 |
| 3‐artery disease | 1945 | 32.4 | 31.8 | 34.7 | 25.5 | 0.861 |
| ACS type | ||||||
| UA | 1945 | 11.0 | 11.6 | 10.0 | 10.6 | 0.474 |
| NSTEMI | 1945 | 54.3 | 52.9 | 56.2 | 58.5 | 0.474 |
| STEMI | 1945 | 34.7 | 35.5 | 33.8 | 30.9 | 0.474 |
| Procedures during this care period or later | ||||||
| PCI | 1945 | 71.0 | 72.2 | 68.5 | 73.4 | 0.872 |
| CABG | 1945 | 14.0 | 14.4 | 14.3 | 6.4 | 0.027 |
| Comorbidities | ||||||
| Arrhythmias | 1929 | 16.7 | 16.0 | 17.4 | 21.3 | 0.072 |
| Cancer | 1943 | 7.1 | 6.3 | 8.4 | 8.5 | 0.120 |
| Kidney disease | 1945 | 2.4 | 2.2 | 2.8 | 2.1 | 0.859 |
| Rheumatoid arthritis | 1944 | 4.6 | 4.8 | 4.1 | 4.3 | 0.636 |
| Psychiatric disorder | 1945 | 2.4 | 2.9 | 3.4 | 3.2 | 0.418 |
| CVA | 1920 | 11.9 | 10.1 | 15.6 | 8.7 | 0.002 |
| PVD | 1921 | 9.2 | 9.1 | 9.5 | 8.7 | 0.954 |
| Concurrent drugs | ||||||
| β‐Blockers | 1942 | 92.6 | 91.3 | 92.2 | 90.4 | 0.536 |
| ASA | 1945 | 91.4 | 93.2 | 91.7 | 91.5 | 0.761 |
| ACE inhibitors | 1939 | 57.7 | 59.0 | 56.1 | 57.0 | 0.523 |
| ATR blockers | 1939 | 15.1 | 14.5 | 16.5 | 13.5 | 0.489 |
| Clopidogrel | 1943 | 79.7 | 79.6 | 80.0 | 79.6 | 0.858 |
| Ca blockers | 1935 | 12.9 | 11.7 | 15.5 | 10.6 | 0.054 |
Abbreviations: ACE, angiotensin‐converting enzyme; ACS, acute coronary syndrome; ASA, acetylsalicylic acid; ATR, angiotensin receptor; BMI, body mass index; Ca, calcium; CABG, coronary artery bypass graft; CV, cardiovascular; CVA, cerebrovascular attack; DM, diabetes mellitus; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; MI, myocardial infarction; NSTEMI, non–ST‐elevation myocardial infarction; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease; SD, standard deviation; STEMI, ST‐elevation myocardial infarction; UA, unstable angina.
Primary Adherence
Of the patients with a statin prescription but no prior purchases (statin naïve), 79.9% (n = 878/1099) had bought the medication within 7 days, 13.1% (n = 144) within 7 to 120 days, and 7.0% (n = 77) later than 120 days after discharge, or did not buy the drugs at all, and were therefore primarily nonadherent for statins.
Those who acquired their medicines within 7 days after discharge (n = 878) were more likely to be strictly adherent statin users during the whole follow‐up period than those who bought the prescribed statin between 7 and 120 days after discharge (n = 144) (76.5% vs 49.3%, respectively; P < 0.001). They were also less likely to be irregular users (21.5% vs 49.3%, respectively; P < 0.001) in the future.
Secondary Adherence
According to the Social Insurance Institution, 90.5% (n = 1761/1945) of discharged patients had initiated statins before hospitalization or within 30 days after discharge. After 1 and 2 years from hospitalization, 62.0% (n = 1205) and 59.4% (n = 1155), respectively, were still using the medication without a single purchase interval longer than 180 days. Of the patients, 61.7% (n = 1200/1945) purchased their statin medication systematically throughout the follow‐up and were categorized as regular statin users; 33.5% (n = 651) were determined as irregular users; and 4.8% (n = 94) fell into the nonuser group. In sensitivity analyses with purchase intervals of 90, 120, and 150 days, 1.7% (n = 33), 32.2% (n = 627), and 51.6% (n = 1004) of the patients, respectively, purchased medication systematically.
Among regular statin users, the mean duration of medication use during the follow‐up (from January 1, 2005, to March 31, 2009) was 27.5 months (SD ± 12.4; IQR, 16.5 mo), the number of purchases was 11.4 (SD ± 5.9; IQR, 8.0), and the purchase interval time was 85.4 days (SD ± 19.0; IQR, 21.8 days). Among regular users, ≥1 purchase interval was longer than 90, 120, or 150 days in 97.3% (n = 1168), 45.4% (n = 545), or 14.9% (n = 179) of the patients, respectively.
To further characterize the 1200 regular statin users, we divided them into 2 subgroups based on the mean interval time between purchases. The cutoff time of 100 days was decided based on the assumption that medication users buy medications for a 3‐month period, which they are maximally allowed. The mean interval time was ≤100 days vs >100 days among 86.3% (n = 1036) and 13.7% (n = 164) of the regular users, respectively.
Impact of Medication Usage on Mortality
Primary Adherence:
Of the 1099 patients without previous statin purchases, 1021 patients were alive 30 days after their discharge. During the follow‐up, patients who purchased their first statin prescription within 7 days after discharge had a significantly lower mortality rate than those who did so between 7 and 120 days after discharge (3.2% vs 10.4%, respectively; P < 0.001). In an age‐ and CVA‐adjusted Cox proportional hazards model, the sloppier primary adherence was associated with a 2‐fold relative risk (RR) of death (HR: 2.34, 95% CI: 1.19‐4.59, P = 0.013) (Figure 2).
Figure 2.
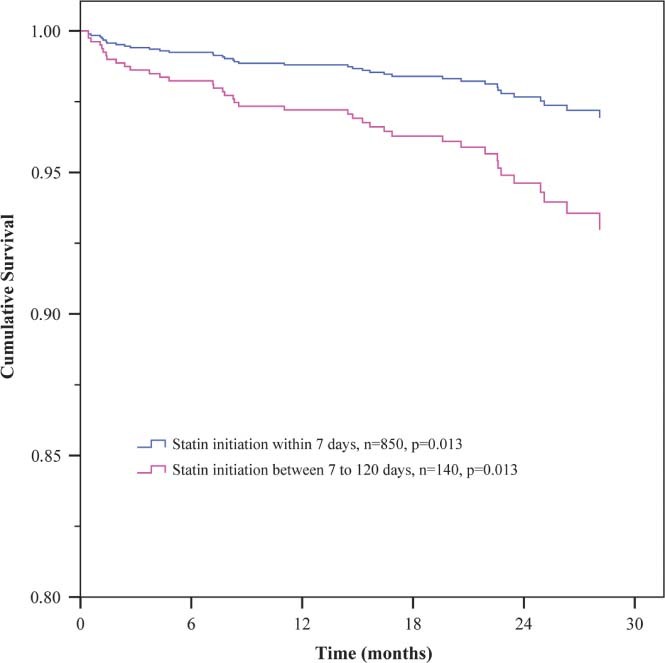
Adjusted Cox regression survival curves for primary adherent patients: first purchase within 7 days vs first purchase between 7 and 120 days.
Secondary Adherence:
During the follow‐up, there was a graded difference in mortality between patient groups with regular, irregular, and nonuse of statins (unadjusted rate 4.9%, 9.4%, and 14.9%, respectively; P < 0.001). The respective rates of cardiovascular death were 2.9%, 5.1%, and 7.4% (P = 0.013). Total cholesterol, low‐density lipoprotein cholesterol, and high‐density lipoprotein cholesterol levels taken at the admission did not alter between different statin user groups. We conducted Cox proportional hazards model with ACS type, CVA, DM, age, 3‐artery disease, and cancer as adjusted confounders. Compared with regular statin users, nonusers were associated with >2× increased HR of mortality (HR: 2.70, 95% CI: 1.49‐4.90, P = 0.001) (Figure 3). Irregular use of statins increased the RR by 50% (HR: 1.53, 95% CI: 1.06‐2.21, P = 0.023).
Figure 3.
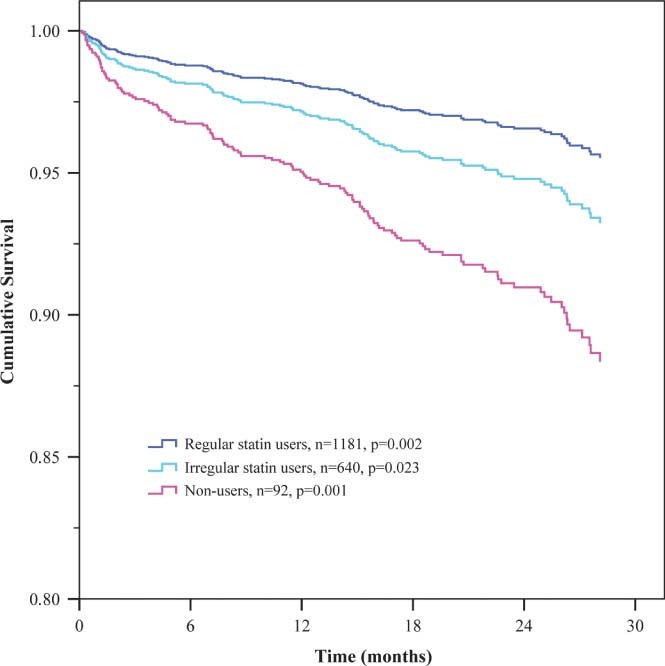
Adjusted Cox regression survival curves for secondary adherence: regular statin users, irregular users, and nonusers.
In sensitivity analyses, death rates differed in a similar trend. Medication users with systematic purchases every 120 and 150 days had lower mortality rates of 3.7% (P < 0.001) and 3.9% (P < 0.001) compared with nonusers at 14.9%, respectively. The difference in mortality between nonusers and medication users with regular purchases every 90 days was insignificant because of the low number of patients in the group with a purchase every 90 days.
Death rates differed statistically significantly also among medication users when the regularity groups based on mean purchase interval times (≤100 days vs >100 days) were compared (4.0% and 11.0%, respectively; P < 0.001). In a Cox proportional hazards model adjusted for age, DM, acetylsalicylic acid, 3‐artery disease, CVA, ACS type, and bypass operation, the mean interval time of >100 days was associated with higher RR of death among regular statin users (HR: 2.34, 95% CI: 1.33‐4.12, P = 0.003).
Discussion
Mortality rate increases steeply with nonadherence to statin therapy in patients with ACS. Therefore, adherence to statin therapy is vital to them. The absolute death rate was about 3× higher in nonadherent patients compared with adherent patients. This difference is 3×–5× higher than in placebo‐controlled clinical trials17, 18, 19 and quite consistent with a previously published statin adherence–mortality study.20 The relative reduction in mortality was also consistent with adherence studies and mostly higher than in case‐control studies.11, 17, 18, 19, 20, 21, 22 The obvious rising trend of mortality from regular statin use through irregular use to nonuse supports the notion that proper regularity in statin therapy does make a difference. Even among regular users, the most strictly adherent patients had the lowest mortality.
The initial prescription rate of statins at discharge was almost complete (95.4%), indicating hospital physicians' good adherence to guidelines.23, 24, 25 The primary adherence rates resembled remarkably previous results26 and also proved that primary nonadherence to statins is associated with an increased risk of death after ACS. Interestingly, we found that a delay in initiation of statins after ACS reflects in future medication usage as more irregular usage habits. Thus, it is vitally important to emphasize to patients the significance of immediate initiation and continuation of statin medication. If the patient is truly convinced to use statins regularly right after a serious health‐threatening episode, she or he will probably use it strictly in the future as well. The proportion of statin initiators around the ACS episode was as much as 90.5%, whereas the crude proportion of strictly adherent patients throughout our median of 2‐year follow‐up was clearly less, 61.7%. This figure is similar to those in previous studies, where adherence varied from 30% to 75%.5, 6, 7, 8, 20, 27 The high discontinuation rates are in grim contrast to the 5‐year discontinuation rates of 6% to 19%17, 19, 28 in the landmark secondary prevention trials demonstrating clinical benefits of statin treatment.
It is quite possible that the pharmacological effects of statins do not completely explain the differences in mortality between adherence groups, because adherence to statin medication may be a broader indicator of a patient's compliance, healthy behavior, and overall mental and physical condition.21 It has also been shown that even placebo nonadherence may increase mortality almost 2× compared with placebo‐adherent patients.21, 29 Our prospective study was based on consecutive ACS patients, irrespective of their socioeconomic position, in a teaching hospital with outstanding registers. The results thus give valid information on medications both before and after the index hospitalization in an unselected cohort. Contrary to prior studies, all patients in our cohort were thoroughly examined using coronary artery angiography to assure the diagnosis and grade of the coronary artery disease. Thus, for example, the age variance (26 to 93 years) is wider than in most of the previous studies.5, 7, 13, 30
Study Limitations
All our patients were of Caucasian origin and living in a society with a drug‐reimbursement system. If anything, these aspects could be anticipated to improve adherence, and may thus limit generalizability. Our register was based on medication purchases, which naturally does not guarantee the actual consumption of the medication, but regular consecutive purchases logically reflect it. During the follow‐up, we did not measure total cholesterol, low‐density lipoprotein cholesterol, or high‐density lipoprotein cholesterol levels, which would have reflected the impact of statin medication use.
Conclusion
The stage of adherence to statin therapy correlates with the risk of death after ACS. Even in a society with population‐wide and high‐level medical care, more efforts are needed to ensure that ACS patients seamlessly continue using statins after discharge from the hospital and realize the importance of their use.
Supporting information
Additional Supporting Information may be found in the online version of this article.
References
- 1. Ward S, Lloyd Jones M, Pandor A, et al. A systematic review and economic evaluation of statins for the prevention of coronary events. Health Technol Assess. 2007;11:1–160. [DOI] [PubMed] [Google Scholar]
- 2. Van de Werf F, Bax J, Betriu A, et al; ESC Committee for Practice Guidelines (CPG). Management of acute myocardial infarction in patients presenting with persistent ST‐segment elevation: the Task Force on the Management of ST‐Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–2945. [DOI] [PubMed] [Google Scholar]
- 3. Waters DD, Ku I. Early statin therapy in acute coronary syndromes: the successful cycle of evidence, guidelines, and implementation. J Am Coll Cardiol. 2009;54:1434–1437. [DOI] [PubMed] [Google Scholar]
- 4. Karter AJ, Parker MM, Moffet HH, et al. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009;44(5 part 1):1640–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Benner JS, Glynn RJ, Mogun H, et al. Long‐term persistence in use of statin therapy in elderly patients. JAMA. 2002;288: 455–461. [DOI] [PubMed] [Google Scholar]
- 6. Helin‐Salmivaara A, Lavikainen P, Korhonen MJ, et al. Long‐term persistence with statin therapy: a nationwide register study in Finland. Clin Ther. 2008;30(part 2):2228–2240. [DOI] [PubMed] [Google Scholar]
- 7. Avorn J, Monette J, Lacour A, et al. Persistence of use of lipid‐lowering medications: a cross‐national study. JAMA. 1998;279: 1458–1462. [DOI] [PubMed] [Google Scholar]
- 8. Blackburn DF, Dobson RT, Blackburn JL, et al. Adherence to statins, β‐blockers and angiotensin‐converting enzyme inhibitors following a first cardiovascular event: a retrospective cohort study. Can J Cardiol. 2005;21:485–488. [PubMed] [Google Scholar]
- 9. West of Scotland Study Group. Compliance and adverse event withdrawal: their impact on the West of Scotland Coronary Prevention Study. Eur Heart J. 1997;18:1718–1724. [DOI] [PubMed] [Google Scholar]
- 10. McGinnis B, Olson KL, Magid D, et al. Factors related to adherence to statin therapy. Ann Pharmacother. 2007;41:1805–1811. [DOI] [PubMed] [Google Scholar]
- 11. Shalev V, Chodick G, Silber H, et al. Continuation of statin treatment and all‐cause mortality: a population‐based cohort study. Arch Intern Med. 2009;169:260–268. [DOI] [PubMed] [Google Scholar]
- 12. Jackevicius CA, Anderson GM, Leiter L, et al. Use of the statins in patients after acute myocardial infarction: does evidence change practice? Arch Intern Med 2001;161:183–188. [DOI] [PubMed] [Google Scholar]
- 13. Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462–467. [DOI] [PubMed] [Google Scholar]
- 14. Vaara S, Nieminen MS, Lokki M‐L, et al. Cohort Profile: the Corogene study. Int J Epidemiol 2011; doi:10.1093/ije/dyr090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bassand JP, Hamm CW, Ardissino D, et al; Task Force for Diagnosis and Treatment of Non–ST‐Segment Elevation Acute Coronary Syndromes of European Society of Cardiology. Guidelines for the diagnosis and treatment of non–ST‐segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1598–1660. [DOI] [PubMed] [Google Scholar]
- 16. Helin‐Salmivaara A, Lavikainen PT, Korhonen MJ, et al. Pattern of statin use among 10 cohorts of new users from 1995 to 2004: a register‐based nationwide study. Am J Manag Care. 2010; 16:116–122. [PubMed] [Google Scholar]
- 17. Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 18. Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists' (CTT) Collaborators. Efficacy and safety of cholesterol‐lowering treatment: prospective meta‐analysis of data from 90,056 participants in 14 randomised trials of statins [published corrections appear in Lancet. 2005;366:1358 and Lancet. 2008;371:2084]. Lancet. 2005;366:1267–1278. [DOI] [PubMed] [Google Scholar]
- 19. The Long‐Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998; 339:1349–1357. [DOI] [PubMed] [Google Scholar]
- 20. Cooke CA, Kirkland SA, Sketris IS, et al. The impact of statins on health services utilization and mortality in older adults discharged from hospital with ischemic heart disease: a cohort study. BMC Health Serv Res. 2009;9:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Simpson SH, Eurich DT, Majumdar SR, et al. A meta‐analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hippisley‐Cox J, Coupland C. Effect of statins on the mortality of patients with ischaemic heart disease: population based cohort study with nested case‐control analysis. Heart. 2006;92:752–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ab E, Denig P, van Vliet T, et al. Reasons of general practitioners for not prescribing lipid‐lowering medication to patients with diabetes: a qualitative study. BMC Fam Pract. 2009;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ohlsson H, Merlo J. Is physician adherence to prescription guidelines a general trait of health care practices or dependent on drug type?—a multilevel logistic regression analysis in South Sweden. Pharmacoepidemiol Drug Saf. 2009;18:682–690. [DOI] [PubMed] [Google Scholar]
- 25. Cohen SM, Kataoka‐Yahiro M. Provider adherence to clinical guidelines related to lipid‐lowering medications. Mil Med. 2010;175:122–126. [DOI] [PubMed] [Google Scholar]
- 26. Jackevicius CA, Li P, Tu JV. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation. 2008;117:1028–1036. [DOI] [PubMed] [Google Scholar]
- 27. Ellis JJ, Erickson SR, Stevenson JG, et al. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19:638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sacks FM, Pfeffer MA, Moye LA, et al; Cholesterol and Recurrent Events Trial Investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–1009. [DOI] [PubMed] [Google Scholar]
- 29. McDermott MM, Schmitt B, Wallner E. Impact of medication nonadherence on coronary heart disease outcomes: a critical review. Arch Intern Med. 1997;157:1921–1929. [PubMed] [Google Scholar]
- 30. Dragomir A, Côté R, White M, et al. Relationship between adherence level to statins, clinical issues and health‐care costs in real‐life clinical setting. Value Health. 2010;13:87–94. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional Supporting Information may be found in the online version of this article.


