Abstract
Background:
The aim of this study was to determine the frequency and nature of errors made by computer electrocardiogram (ECG) analysis of atrial fibrillation (AF), and the clinical consequences.
Hypothesis:
Computer software for interpreting ECGs has advanced.
Methods:
A total of 10279 ECGs were collected, automatically interpreted by the built‐in ECG software, and then reread by 2 cardiologists. AF‐related ECGs were classified into 3 groups: overinterpreted AF (rhythms other than AF interpreted as AF), misinterpreted AF (AF interpreted as rhythms other than AF), and true AF (AF interpreted as AF by both computer ECG interpretation and cardiologists).
Results:
There were 1057 AF‐related ECGs from 409 patients. Among these, 840 ECGs (79.5%) were true AF. Overinterpretation occurred in 98 (9.3%) cases. Sinus rhythm and sinus tachycardia with premature atrial contraction and/or baseline artifact and sinus arrhythmia were commonly overinterpreted as AF. Heart rate ≤60 bpm and baseline artifact significantly increased the likelihood of overinterpreted AF. Misdiagnosis occurred in 119 (11.3%) cases, in which AF was usually misdiagnosed as sinus or supraventricular tachycardia. The presence of tachycardia and low‐amplitude atrial activity significantly increased the likelihood of misdiagnosis of AF. Among the erroneous computer ECG interpretations, 17 cases (7.8%) were not corrected by the ordering physicians and/or repeat computer‐ECG interpretation; inappropriate follow‐up studies or treatments of the patients were undertaken with no serious sequelae.
Conclusions:
Erroneous computer ECG interpretation of AF was not rare. Attention should be concentrated on educating physicians about ECG appearance and confounding factors of AF, along with ongoing quality control of built‐in software for automatic ECG interpretation. Clin. Cardiol. 2012 DOI: 10.1002/clc.22000
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Atrial fibrillation (AF) is the most common sustained arrhythmia. It increases in prevalence with age and is associated with an increased long‐term risk of stroke, heart failure, and all‐cause mortality.1., 2., 3. Computer‐generated interpretation of 12‐lead electrocardiograms (ECG) is extremely helpful in ECG documentation of AF, and interpretation accuracy is important because erroneous computer ECG interpretation of AF can result in inappropriate management of patients with interventions such as anticoagulation and antiarrhythmic drugs as well as additional unnecessary diagnostic studies.4., 5., 6., 7., 8. Correct physician rereading is essential in avoiding such errors.5., 6. Built‐in software programs for automatic computer ECG interpretation have made advances in recent years; however, the body of evidence about improvement in the accuracy of AF interpretation by built‐in software is limited. The aim of this study was to determine the frequency and nature of erroneous ECG interpretation by built‐in software, and its clinical consequences.
Methods
A total of 10279 consecutive ECGs were collected from both inpatients and outpatients between May 2010 and August 2010 at Kyungpook National University Hospital, Daegu, South Korea. As ECGs from the same patient with the same rhythm may have different interpretations, several tracings from the same patient were included in this study. The ECGs were initially analyzed by the computer ECG interpretation program (Philips 12‐lead algorithm). The tracings were displayed to show 2.5 seconds of each of the 12 leads in 4 columns and simultaneous 10‐second strip of lead II. Artifact filter, AC (power line) filter, baseline wander filter, and frequency response filter ranging from 0.5 to 150 Hz were used to remove a variety of artifacts. On the Philips 12‐lead algorithm, fine AF was interpreted with missing P waves in most leads and marked variations in the ventricular rate, and coarse AF was interpreted from multiple shapes of P waves with a rapid apparent atrial rate and variations in the ventricular rate. Two cardiologists independently reread the ECGs to assess the accuracy of the computer ECG interpretation. Differences in interpretation were resolved by consensus. For the purpose of this study, both atrial flutter and AF were considered as AF, and if the computer incorrectly interpreted atrial flutter as AF, the computer interpretation was considered correct.
Baseline demographic characteristics of the patients and location of ECG obtained were also evaluated. Medical records of patients were reviewed to determine whether unnecessary follow‐up studies, such as repeat ECGs, 2‐dimensional echocardiography, and/or possibly inappropriate management, were initiated because of erroneous computer ECG interpretation of AF. Management was considered inappropriate when interpretation of ECGs resulted in unnecessary treatment changes, such as anticoagulation in patients without compelling indication other than AF, medications that slow the ventricular rate, or antiarrhythmic agents. The study was approved by the institutional ethics committee.
Definitions and Data Analyses
AF was defined as a supraventricular tachyarrhythmia characterized by the replacement of consistent P waves by rapid oscillations or fibrillatory waves that varied in amplitude, shape, and timing, associated with an irregular, frequently rapid ventricular response when atrioventricular (AV) conduction was intact.9 Low‐amplitude atrial activity was defined as AF in which the amplitude of the P wave was ≤0.1 mV in all leads. High and low ventricular rate were defined as a ventricular rate ≥150 bpm and ≤60 bpm, respectively. A new concept for irregularity of cardiac cycle, the irregularity index was estimated as (maximal R‐R interval − minimal R‐R interval)/minimal R‐R interval on a routine 12‐lead ECG. The presence of baseline artifact, including electrical noise as well as motion artifact, was assessed. AF‐related ECG was defined as ECG interpreted as AF by the computer and/or cardiologists, and included overinterpreted AF, misinterpreted AF, and true AF. Overinterpreted AF was assigned when rhythms other than AF were actually present but the interpretation of AF was made. Misinterpreted AF was assigned when AF actually was present, but the interpretation of rhythms other than AF was made. True AF was assigned when the diagnosis of AF was made by computer ECG interpretation and confirmed by cardiologist rereadings.
Statistical Analysis
Data are presented as mean ± SD for continuous variables and percentages for categorical variables. Comparisons were made using the Student t test for continuous variables and the χ 2 test for categorical variables. Sensitivity, specificity, and positive and negative predictive values for the diagnosis of AF were determined. The P values were 2‐sided, and P < 0.05 was considered significant. Statistical analysis was performed using SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL).
Results
Among a total of 10279 consecutive ECGs reviewed, there were 1057 AF‐related ECGs from 409 patients (age 68.4 ± 14.1 y). Among these, there were 840 cases (79.5%) of true AF, and 217 ECGs carried incorrect interpretations related to AF (98 overinterpretation and 119 misinterpretation) by computer ECG.
Underlying Rhythm in Overinterpreted Atrial Fibrillation
Overinterpretation occurred in 98 cases. The most common underlying rhythms at the time of computer ECG interpretation were sinus rhythm and sinus tachycardia with premature atrial contractions (PAC) and/or artifact and sinus arrhythmia; these 3 interpretations accounted for 59.2% of all overinterpreted AF (Table 1). Wolff‐Parkinson‐White syndrome, sinus rhythm with variable AV conduction, and AV block were also common causes of overinterpreted AF. In the cases of overinterpreted AF, patients were younger than those with true AF, and the proportion of ECGs obtained in the intensive care unit was higher. The proportions of atrial activity <0.1 mV and irregularity index ≥1 were significantly lower and the proportions of heart rate ≤60 bpm and baseline artifacts significantly higher in the group with overinterpreted AF compared with the group with true AF. However, the proportion of heart rate ≥150 bpm was not different between the 2 groups.
Table 1.
Underlying Rhythm in the 98 Patients With Overinterpretation of Atrial Fibrillation
| Underlying Rhythm | No. |
|---|---|
| Sinus rhythm | 6 |
| Sinus rhythm with first‐degree AV block | 2 |
| Sinus rhythm with second‐degree AV block | 7 |
| Sinus rhythm with atrial premature complexes | 22 |
| Sinus rhythm with ventricular premature complexes | 3 |
| Sinus rhythm with marked sinus arrhythmia | 10 |
| Sinus pause with junctional escape rhythm | 4 |
| Sinus rhythm with artifact | 19 |
| Sinus tachycardia | 3 |
| Sinus tachycardia with atrial premature complexes | 9 |
| Sinus tachycardia with artifact | 5 |
| Atrial tachycardia | 2 |
| Sinus bradycardia with atrial premature complexes | 1 |
| Junctional rhythm | 1 |
| 2:1 AV block | 3 |
| Complete AV block | 3 |
| Wolff‐Parkinson‐White syndrome | 5 |
Abbreviations: AV, atrioventricular.
Figure 1 shows examples of overinterpreted AF. Panel A shows sinus rhythm with PACs causing irregular R‐R intervals that led to the incorrect interpretation as AF. Panel B shows sinus arrhythmia with baseline artifacts. The baseline artifacts resembling F waves in lead aVF caused the incorrect interpretation as atrial flutter/AF. Panel C shows sinus arrhythmia and Wolff‐Parkinson‐White syndrome. A short P‐R interval obscuring the P wave, as well as irregular R‐R interval, resulted in inappropriate computer ECG interpretation. Panel D shows an advanced second‐degree AV block with junctional escape complexes that led to overinterpreted AF.
Figure 1.
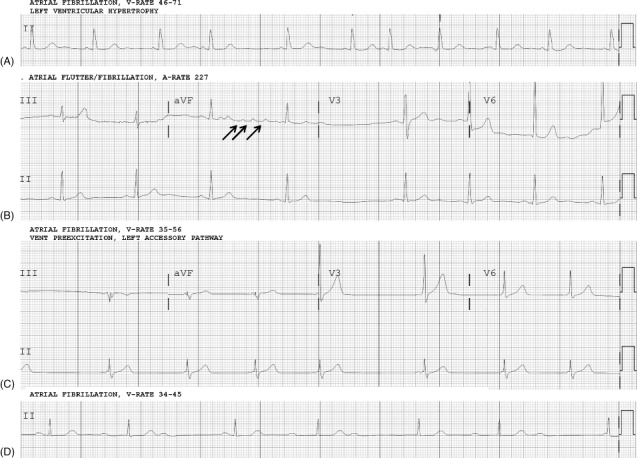
Examples of overinterpreted AF. (A) Sinus rhythm with multiple premature atrial contractions causing irregular rhythm; interpreted as AF. (B) Sinus arrhythmia with baseline artifacts resembling F waves in a VF lead; interpreted as atrial flutter/AF. (C) Sinus arrhythmia and Wolff‐Parkinson‐White syndrome. Short P‐R interval obscuring P wave, as well as irregular rhythm, contributed to overinterpretation as AF. (D) Advanced second‐degree AV block with junctional escape complexes that led to overinterpretation as AF. Abbreviations: AF, atrial fibrillation; AV, atrioventricular.
Misinterpreted Atrial Fibrillation
Misinterpretation occurred in 119 cases, including 89 cases of AF and 30 cases of atrial flutter. The most common errors of computer ECG interpretation corrected as AF by the cardiologists were tachycardia, such as supraventricular tachycardia, sinus tachycardia with irregular rate, and sinus tachycardia; these 3 interpretations accounted for 76.4% of all misinterpreted AF (Table 2). Among the 30 cases of atrial flutter, sinus or ectopic atrial rhythm, atrial arrhythmia, and sinus tachycardia were common computer ECG misinterpretations. The misinterpreted AF group had higher proportions of patients age ≥70 years and ECGs obtained in the emergency department compared with the group with true AF. The proportions of heart rate ≥150 bpm and atrial activity <0.1 mV were significantly higher and the proportion of irregularity index ≥1 was significantly lower in the group with misinterpreted AF compared with the group with true AF. The proportions of heart rate ≤60 bpm and baseline artifacts were not different between the 2 groups.
Table 2.
Misinterpretation of Atrial Fibrillation
| Computer ECG Interpretation | AF (n = 89) | Atrial Flutter (n = 30) |
|---|---|---|
| Sinus rhythm | 2 | 1 |
| Sinus rhythm with first‐degree AV block | 1 | 1 |
| Sinus rhythm with premature atrial contractions | 4 | |
| Sinus tachycardia | 11 | 5 |
| Sinus tachycardia with irregular rate | 23 | |
| Sinus tachycardia with premature ventricular contractions | 1 | |
| Supraventricular tachycardia | 34 | 3 |
| Wandering pacemaker | 4 | 2 |
| Accelerated junctional rhythm | 1 | |
| Sinus bradycardia | 4 | 2 |
| Bradycardia with irregular rate | 2 | |
| AV dissociation | 2 | |
| Atrial arrhythmia | 6 | |
| Ectopic atrial tachycardia | 2 | |
| Sinus rhythm or ectopic atrial rhythm | 7 | |
| 4:1 AV block | 1 |
Abbreviations: AF, atrial fibrillation; AV, atrioventricular; ECG, electrocardiogram.
Figure 2 shows examples of misinterpreted AF. Panel A shows relatively regular AF with a small difference in R‐R interval (30 ms). Panel B shows a typical case of AF with rapid ventricular rate ≥150 bpm and no atrial activity, which was interpreted as supraventricular tachycardia by the computer. Panel C shows atrial flutter with variable AV conduction. During 2:1 or 3:1 AV conduction, the R‐R intervals were regular and atrial waves were relatively well visualized. However, this case was incorrectly interpreted as sinus or ectopic atrial rhythm by the computer. Panel D shows atrial flutter interpreted as sinus tachycardia by the computer. A ventricular rate ≥150 bpm and F wave buried in the QRS complex caused the incorrect interpretation as sinus tachycardia.
Figure 2.

Examples of misinterpreted AF. (A) Relatively regular AF with small differences in R‐R interval (30 ms); interpreted by computer as sinus tachycardia. (B) AF with rapid ventricular rate >150 bpm and no atrial activity; interpreted as supraventricular tachycardia. (C) Atrial flutter with 2:1 or 3:1 conduction. The R‐R intervals were relatively regular and atrial waves were well visualized, but this case was incorrectly interpreted by the computer as sinus or ectopic atrial rhythm. (D) Atrial flutter with ventricular rate >150 bpm and F wave located in terminal of QRS complex; interpreted as sinus tachycardia. Abbreviations: AF, atrial fibrillation.
Interpretation Accuracy of Atrial Fibrillation‐Related Electrocardiograms
Among 1057 AF‐related ECGs, the rates of overinterpretation (n = 98), misinterpretation (n = 119), and true AF (n = 840) were 9.3%, 11.3%, and 79.5%, respectively. In analyzing the accuracy of computer ECG interpretation, the specificity of the interpretation of AF was 98.9% and the negative predictive value was 98.7%. A relatively lower sensitivity of 87.6% and positive predictive value of 89.6% were revealed.
Clinical Consequences of the Incorrectly Interpreted Atrial Fibrillation‐Related Electrocardiograms
Among the 98 overinterpreted ECGs, 83 (84.7%) cases were corrected as non‐AF by the ordering physician, whereas 15 cases (15.3%) were accepted as AF and inappropriate follow‐up interventions were undertaken, such as rate control (n = 11), rhythm control (n = 2), aspirin/anticoagulation (n = 5), and cardiology consultation (n = 1). Among the 119 ECGs misinterpreted as non‐AF, 117 cases (98.3%) were corrected by the serial computer‐ECG interpretation (92 cases, 77.3%) and the ordering physician (25 cases, 21.0%). However, 2 cases of atrial flutter were not corrected. No morbidity‐ or mortality‐related events developed after the inappropriate management of the patients.
Discussion
AF is recognized as the most important arrhythmia in terms of prevention of stroke.1., 2., 3. Computer‐generated interpretation of ECG is very useful, but often inaccurate.4., 5., 6., 7. Incorrect reading by the computer hampers the interpretation of inexperienced physicians and may result in potentially harmful treatments such as anticoagulation, antiarrhythmics, or cardioversion.4., 5., 8.
The most common underlying rhythms in overinterpreted AF were sinus rhythm and sinus tachycardia with PAC and/or baseline artifact. These results were similar those of several previous studies.4., 5., 6., 7. AF is typically defined as irregularly irregular rhythm.9 Sinus rhythm with PAC or sinus arrhythmia has commonly irregular rhythms. In addition, complete AV block and Mobitz type I AV block may have an irregular ventricular rate. The possibility of overinterpreted AF will be increased if a P wave in rhythms with irregular R‐R intervals is obscured by baseline artifact. In the present study, bradycardias ≤60 bpm were more common in the group with overinterpreted AF compared with the group with true AF. In bradycardia, the absolute value of maximal R‐R interval − minimal R‐R interval is great, although rhythm is relatively regular, as shown as low frequency of irregularity index ≥1, which may affect overinterpretation of AF by the computer. Wolff‐Parkinson‐White syndrome has a short P‐R interval, δ waves, and a wide QRS complex. Wolff‐Parkinson‐White syndrome may be overinterpreted as AF by computer ECG interpretation if a P wave is ambiguous due to very short P‐R interval or low‐amplitude atrial activity and rhythm is irregular, as in our case.
Atrial fibrillation was commonly misinterpreted as sinus and supraventricular tachycardia. In the group with misinterpretation of AF, tachycardia ≥150 bpm was more common than in the groups with true AF and overinterpreted AF. In tachycardia, the absolute difference in R‐R interval is smaller than in rhythm with normal or slower heart rate. Also in the group with misinterpretation of AF, the frequency of low atrial activity was higher compared with the 2 other groups. Moreover, the P wave is easily blurred with rapid heart rate. Therefore, the computer may misjudge irregular rhythm in AF with rapid ventricular response as regular rhythm in sinus or supraventricular tachycardia. The ambiguity of the P wave is also very important in AF interpretation. On the other hand, atrial flutter has distinct, sawtooth F waves. The computer may misjudge the F wave in atrial flutter as the P wave in sinus rhythm or as the ectopic P wave in atrial arrhythmia, and when the computer did not decide P‐wave origin, ambiguous interpretation as sinus or ectopic rhythm was observed.
Before surgery requiring general anesthesia and even when patients with noncardiac problems visit the emergency department, ECGs are almost routinely performed. Many physicians are lacking in their ability to interpret ECGs and tend to depend on computer ECG interpretation.6., 10., 11. In this study, the interpretation accuracy of AF was only about 80% and was similar to or lower than that shown in other previous studies (80.3%–92.2%).4., 5., 6., 7. Computer software for interpreting ECGs has advanced over several decades; however, its accuracy in making the interpretation of AF does not seem much improved. Although more cases of difficult ECGs with heart rate ≥150 bpm and/or baseline artifact were included in the present study compared with a previous study,6 results on the interpretation accuracy of AF, especially the sensitivity and positive predictive value, were still disappointing.
The reliability and accuracy of computer ECG interpretation have been analyzed previously. However, there were no data about the differences of erroneous ECG interpretation according to the demographic characteristics and clinical situation. The proportion of erroneous computer interpretation of AF was different according to patient age. Misinterpreted AF was more frequent in elderly patients, who have high incidence of AF, and overinterpreted AF was more common in younger patients, who have low incidence of AF. Moreover, the computer seems to make more mistakes in serious clinical situations, in which incorrect computer ECG interpretation of AF may prove more harmful. Fortunately, in the present study, most of the erroneous computer ECG interpretations were corrected by the ordering physician and serious or fatal complications did not develop. However, some patients received unnecessary additional studies and/or treatments. Attention should be concentrated on educating physicians about the nature and limitations of computer ECG interpretation of AF and the recognition of confounding factors.
Study Limitations
First, this was a retrospective, single‐center study. Electrocardiographic analysis was done by only one of several commercially available algorithms for ECG interpretation, which precludes our evaluation of the accuracy of other computer software. Second, consecutive ECGs were included in this study. As several follow‐up ECGs may have been obtained from the same patient, the incidence of AF may be different from the actual incidence of AF at our institution.
Conclusion
Erroneous computer ECG interpretation of AF was not rare. Ongoing quality control of computer ECG interpretation programs and expert consultation in complicated ECG interpretation are necessary to reduce the error rate.
References
- 1. Feinberg WM, Blackshear JL, Laupacis A, et al. Prevalence, age distribution, and gender of patients with atrial fibrillation: analysis and implications. Arch Intern Med. 1995;155:469–473. [PubMed] [Google Scholar]
- 2. Gajewski J, Singer RB. Mortality in an insured population with atrial fibrillation. JAMA. 1981;245:1540–1544. [PubMed] [Google Scholar]
- 3. Leithäuser B, Park JW. Cardioembolic stroke in atrial fibrillation: rationale for preventive closure of the left atrial appendage. Korean Circ J. 2009;39:443–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bogun F, Anh D, Kalahasty G, et al. Misdiagnosis of atrial fibrillation and its clinical consequences. Am J Med. 2004;117:636–642. [DOI] [PubMed] [Google Scholar]
- 5. Anh D, Krishnan S, Bogun F. Accuracy of electrocardiogram interpretation by cardiologists in the setting of incorrect computer analysis. J Electrocardiol. 2006;39:343–345. [DOI] [PubMed] [Google Scholar]
- 6. Davidenko JM, Snyder LS. Causes of errors in the electrocardiographic diagnosis of atrial fibrillation by physicians. J Electrocardiol. 2007;40:450–456. [DOI] [PubMed] [Google Scholar]
- 7. Guglin ME, Thatai D. Common errors in computer electrocardiogram interpretation. Int J Cardiol. 2006;106:232–237. [DOI] [PubMed] [Google Scholar]
- 8. Finsterer J, Stöllberger C, Gatterer E. Oral anticoagulation for ECG tremor artefact simulating atrial fibrillation. Acta Cardiol. 2003;58:425–429. [DOI] [PubMed] [Google Scholar]
- 9. Fuster V, Rydén LE, Cannom DS, et al. 2011. ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57:e101–e198. [DOI] [PubMed] [Google Scholar]
- 10. Tsai TL, Fridsma DB, Gatti G. Computer decision support as a source of interpretation error: the case of electrocardiograms. J Am Med Inform Assoc. 2003;10:478–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Margolis S, Reed R. EKG analysis skills of family practice residents in the United Arab Emirates: a comparison with US data. Fam Med. 2001;33:447–452. [PubMed] [Google Scholar]


