Abstract
Background
Original descriptions of the takotsubo syndrome (TS) included a characteristic left ventricular (LV) contraction pattern, “apical ballooning.” Recently, several reports have associated contraction patterns not strictly conforming to the original description with TS. The specifics of the contraction pattern seem to set TS apart from the much larger population of patients with acute coronary syndrome (ACS) but no obstructive coronary artery disease (OCAD). This study was undertaken to compare patients with midventricular and apical dysfunction with those with other LV contraction patterns.
Hypothesis
If TS can present with a variety of patterns of LV dysfunction, then both those with and those without the pattern should have the clinical components previously assigned to the syndrome.
Methods
We studied LV contraction patterns in consecutive ACS patients referred for consideration of emergent or urgent percutaneous coronary intervention.
Results
Of the 893 patients evaluated in 2008, we excluded 862 on the basis of OCAD, preexisting LV dysfunction, or an obvious alternative cause of symptoms. The remaining 31 (3.5%) also had no OCAD but manifested an LV contraction abnormality. We compared the 15 patients (1.7%) whose ventriculograms met criteria for TS with the 16 patients (1.8%) whose did not. The most common alternative pattern was global hypokinesis, followed by a variety of segmental contraction abnormalities. Patients with the TS pattern were older and had evidence of greater myocardial injury. More than 85% were women.
Conclusions
The TS pattern identifies a distinct subset of ACS patients with a remarkable predominance of postmenopausal women and is therefore fundamental to the definition of this entity. This distinctive facet of the syndrome is likely to be an important clue to its pathogenesis. We did not encounter patients with other patterns of LV dysfunction that could be thought to represent stress‐induced cardiomyopathy. Copyright © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
First described in 1991, the takotsubo syndrome (TS), also known as “stress‐induced cardiomyopathy” or “apical ballooning syndrome,” is characterized by chest discomfort, elevated myocardial markers, and ischemic electrocardiographic (ECG) changes.1 Two features justify viewing this group as distinct from the vast majority of patients with acute coronary syndromes (ACS): 1) absence of obstructive coronary artery disease (OCAD) on angiography, and 2) a distinctive contraction abnormality of the left ventricle (LV). The syndrome draws its name from the latter. “Takotsubo” is the Japanese term for an octopus trap. The pot shape of this trap resembles the systolic deformity of the LV resulting from this contraction pattern.
Normal or near‐normal coronary arteries on angiography are not rare in patients with suspected ACS. They have been reported in 2.6% to 13% of such patients.2, 3, 4, 5 On the other hand, the LV contraction pattern is distinctive and a critical part of the syndrome. It is most often described as akinesis or dyskinesis of the apical segment of the LV as well as hypercontractility of the base.6, 7, 8 This pattern seems to reflect ischemic injury that encompasses > 1 coronary distribution.8 Evidence has appeared suggesting that TS may present with midventricular dysfunction sparing the apex.9 This has been well studied and incorporated into the most recent set of diagnostic criteria.8 Recently, some have argued that even other patterns of LV dysfunction, such as global hypokinesis or focal wall motion abnormalities, should also be considered variants of this clinical syndrome.10, 11, 12, 13, 14, 15 Adding to this debate, apical ballooning has been identified in a significant proportion of patients with anteroseptal myocardial infarction (MI).16
Thus, investigators have proposed that the pathogenetic mechanisms responsible for TS may result in a variety of LV contraction abnormalities. Insofar as this is true, the classic octopus‐pot shape is neither completely sensitive nor specific for these mechanisms. As yet a large population with suspected ACS meeting criteria for stress‐induced cardiomyopathy has not been systematically reviewed for the presence of alternate patterns of LV dysfunction.
We undertook this study to compare ACS patients without OCAD who manifest midventricular and apical dysfunction with those with other LV contraction patterns. Our hypothesis was that if TS can present itself with any form of LV dysfunction, the 2 groups will be similar and fit the phenotype previously described for the syndrome.
Methods
This project was approved by the institutional review board of the Medstar Research Institute. All patients provided consent to the operator prior to the cardiac catheterization procedure.
From our ongoing registry of patients referred for consideration of percutaneous coronary intervention (PCI), we identified all those who underwent emergent or urgent cardiac catheterization between January 1, 2008 and December 31, 2008 because of suspected ACS. Patients with ST‐elevation and non–ST‐elevation ACS were included. The decision to proceed with coronary angiography was based on the clinical presentation, electrocardiographic findings, and levels of cardiac markers. We selected for analysis those with normal or near‐normal coronary angiograms. We excluded those with: 1) an obvious noncardiac cause of the syndrome, 2) known or probable preexisting LV dysfunction from any cause, 3) a history of revascularization (surgical or percutaneous), or 4) known coronary artery disease (eg, documented prior MI or abnormal coronary angiography). The remaining patients were included in our initial analysis.
Two of the investigators independently reviewed their coronary angiograms and LV angiograms. A complete review of available records was carried out on those with abnormal LV contraction patterns. Those with a presenting illness that might plausibly account for the LV dysfunction (eg, sepsis or cardiac arrest) were excluded. Thus, the study population consisted of consecutive patients presenting with: 1) symptoms consistent with ACS, 2) no OCAD, and 3) LV dysfunction with no other apparent reason. Patients were considered to have the “TS pattern” if they met Mayo Clinic criteria, which considered midventricular dysfunction with or without apical ballooning to be necessary for its diagnosis.8
Statistical Analysis
Continuous variables were reported as mean ± SD and compared using the Student t test. Categorical variables were expressed as proportions and compared by means of contingency tables. Differences were tested by means of either the χ 2 or Fisher exact test. A 2‐tailed P value < 0.05 was considered to indicate statistical significance. Statistical analysis was performed using SAS version 9.1 (SAS Institute, Cary, NC).
Results
Of the 893 patients with ACS referred for urgent or emergent PCI during the calendar year 2008, 767 (85.9%) were excluded on the basis of OCAD on angiography, a history of revascularization, an obvious noncardiac cause of the syndrome, or known prior LV dysfunction. Of the remaining 126 (14.1%) patients, 83 had normal LV systolic function on LV ventriculography and were not further analyzed. Twelve patients were found to have a presenting illness that plausibly could have been an alternative cause for LV dysfunction (eg, cardiac arrest, septic shock) and were excluded from final analysis.
Therefore, the study population consisted of 31 consecutive patients presenting with: 1) apparent ACS, 2) normal or near‐normal coronary arteriograms, and 3) no other reason for LV dysfunction. Of those, 15 (1.7%) had a LV contraction pattern meeting the Mayo Clinic criteria for TS. Among the 16 (1.8%) without the TS contraction pattern, the most common alternative pattern of LV dysfunction was global hypokinesis, followed by a variety of segmental abnormalities (Figure 1). The most common clinical diagnosis for these was myocarditis. Figure 2 depicts the specifics of patient selection.
Figure 1.
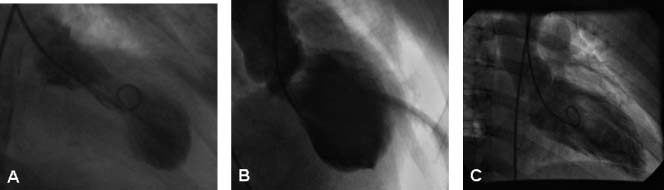
Left ventriculograms/systolic images. (A) Apical ballooning. (B) Midventricular dysfunction without ballooning of the apex. (C) Global hypokinesis.
Figure 2.
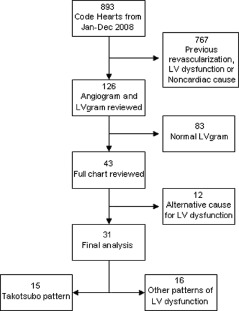
Study design. Abbreviation: LV, left ventricular.
Table 1 shows the characteristics of these 31 patients. Patients with the TS pattern were significantly older (P < 0.001). Thirteen (86.7%) were female. There was no difference in the presence of cardiac risk factors such as hypertension, diabetes, and hyperlipidemia (Table 2). Nearly all patients in both groups presented with chest pain, shortness of breath, or a combination of both (Table 1). Psychological or physiological stress preceding the onset of symptoms was documented in 5 patients in the TS group and only in 1 patient in the control group. The clinical records were often incomplete with regard to this aspect of the history.
Table 1.
Presentation, Electrocardiogram, and Troponin
| Takotsubo (n = 15) | Other (n = 16) | P Value | |
|---|---|---|---|
| CC | |||
| Chest pain | 12/15 (80%) | 14/16 (87.5%) | 0.7 |
| Dyspnea | 6/15 (40%) | 10/16 (62.5%) | 0.4 |
| Nausea | 1/15 (6.7%) | 2/16 (12.5%) | 1.0 |
| Others | 5/15 (33.3%) | 4/16 (25%) | 0.7 |
| ECG | |||
| ST‐segment abnormality | 7/13 (53.8%) | 2/12 (16.7%) | 0.1 |
| T‐wave abnormality | 9/13 (69.2%) | 0/12 (0%) | 0.005 |
| Either | 11/13 (84.6%) | 2/12 (16.7%) | 0.003 |
| Cardiac markers | |||
| TnI >ULN | 13/14 (92.9%) | 9/15 (60%) | 0.08 |
| TnI > 3 × ULN | 11/14 (78.3%) | 6/15 (40%) | 0.08 |
Abbreviations: CC, chief complaint; ECG, electrocardiogram; TnI, troponin I; ULN, upper limit of normal
Table 2.
BaselineCharacteristics
| Takotsubo (n = 15) | Other (n = 16) | P Value | |
|---|---|---|---|
| Mean age, y | 66.3 ± 11.5 | 42.1 ± 15.5 | < 0.001 |
| F | 13 (86.7%) | 8 (50%) | 0.05 |
| HT | 9 (60%) | 4 (26.7%) | 0.1 |
| DM | 1 (6.7%) | 0 (0%) | 1.0 |
| HL | 4 (26.7%) | 3 (20%) | 1.0 |
| Serum Cr > 2 mg/dL | 3 (21.4%) | 2 (15.4%) | 0.6 |
Abbreviations: Cr, creatinine; DM, diabetes mellitus; F, female; HL, hyperlipidemia; HT, hypertension
Patients with the TS pattern were more likely to have striking ECG abnormalities defined as either 2 mm of ST‐segment elevation or 5 mm of T‐wave inversion. In the 2 patients without the TS pattern who had ST‐segment elevation, the changes were diffuse and were accompanied by PR‐segment depression, findings suggestive of pericarditis. Both were discharged with the diagnosis of myopericarditis. Patients with the TS pattern tended to have higher peak troponin values, but this difference did not reach statistical significance (P = 0.08).
By definition, all patients in the takotsubo group had midventricular dysfunction. All but one had apical ballooning. In the other group, the most common pattern was global hypokinesis (n = 7). Others had segmental contraction abnormalities inconsistent with the TS pattern, such as inferior or basal hypokinesis. Patients without the TS pattern had significantly higher ejection fractions (48.2% ± 6.7% vs 33.6% ± 7.7%, P < 0.001).
The discharge diagnosis assigned by the primary team to all patients with midventricular dysfunction was TS. In the other group, the most common discharge diagnosis was suspected myocarditis. This diagnosis was supported by a compatible magnetic resonance imaging (MRI) with delayed contrast enhancement in half of the cases. Other diagnoses recorded at discharge were pericarditis, MI, and noncardiac causes (Table 3).
Table 3.
Discharge Diagnosis
| Takotsubo (n = 15) | Other (n = 16) | |
|---|---|---|
| Takotsubo | 15 (100%) | 0 (0%) |
| Possible myocarditis | 0 (0%) | 6 (37.5%) |
| Pericarditis | 0 (0%) | 1 (6.2%) |
| NSTEMI | 0 (0%) | 2 (12.5%) |
| Noncardiac | 0 (0%) | 2 (12.5%) |
| None | 0 (0%) | 5 (31.2%) |
Abbreviations: NSTEMI, non–ST‐segment‐elevation myocardial infarction
Discussion
Most of what is known about TS comes from case series in which patients were selected based on the typical contraction pattern or on the suspicion of stress‐induced cardiomyopathy by the attending physician. This may have caused patients with similar pathogenetic mechanisms but with different forms of LV dysfunction to be inappropriately excluded. The present study spreads a wider net. It describes a consecutive series of patients with suspected ACS and focuses on those with no OCAD but with LV dysfunction of any form. Unlike previous studies, we reviewed all left ventriculograms, including all patients who could be thought to have stress‐induced cardiomyopathy.
The frequency of midventricular dysfunction in our study was 1.7%. This is similar to the frequency of TS in larger series that selected patients based on this contraction pattern.17 Importantly, 1 of our patients had midventricular dysfunction without ballooning of the apex, a pattern consistent with that described by Hurst et al and incorporated into Mayo Clinic criteria.9 The proportion of patients with this variant in our series was much lower than the 40% reported by Kurowski et al, which puts its true incidence in question.17
When those with the TS pattern were compared with those with other abnormalities of LV contraction, the usual cardiac risk factors were similar. There were, however, important differences: takotsubo patients were older (P < 0.001), more often female (P = 0.05), and had evidence of larger areas of LV injury (eg, more dramatic ECG changes [P = 0.003], greater elevation in biomarkers [P = 0.08], and lower LV ejection fraction [P < 0.001]). Physical or emotional stressors were more frequently recorded in this group, even though documentation in this regard was often lacking. These features have all been associated with TS in previous case series.6, 7, 17, 18, 19, 20 Thus, the clinical features of the patients with the typical contraction pattern of TS differed from those with other patterns and fit with those previously attributed to the syndrome. This observation supports the idea that apical and midventricular ballooning, but not other contraction abnormalities, identifies a population with distinctive clinical features that may prove to be key to understanding the pathogenesis of the disorder. Moreover, this notion gains further support from the observation that in almost 900 patients with suspected ACS, no patients with other patterns of LV dysfunction could be thought to represent stress‐induced cardiomyopathy as recently described.10, 11, 12, 13, 14, 15 If those variants truly exist, they are far less commonly encountered than the typical pattern, and the diagnosis of TS in these patients should be pursued with caution.
Although it was not the aim of this study, it is probably important to comment on the cause of LV dysfunction in the control group. The heterogeneity observed in those patients may indicate that they represent a mixture of atypical presentation of myopericarditis, previously unrecognized contraction abnormalities, coronary vasospasm, or underestimated coronary artery disease. Potentially useful tests, such as cardiac MRI, were available in only a few cases. Previous studies using this imaging modality have identified findings consistent with myocarditis in about half of the patients with suspected ACS and no OCAD.21, 22 MRI has also been shown to be of value in the workup of TS. In this setting however, specific patterns have yet to be determined.23, 24, 25, 26
Over the years, the participation of a stress‐induced catecholamine surge in TS has gained significant support. Wittstein et al studied catecholamine levels in 19 patients who were admitted with cardiac symptoms and LV dysfunction following severe psychological trauma.27 Only 1 of the 19 had obstructive coronary disease. They found levels of plasma catecholamines on admission in TS patients to be markedly higher than in 7 control patients with Killip class III heart failure after MI. Others have also found higher catecholamine levels in TS patients as compared with those with MI.28 The mechanisms through which a catecholamine surge might result in the TS contraction pattern have been a target of research interest. Even though most adrenergic nerve endings are thought to be located around the base of the LV, there is some evidence that the apex has a higher density of receptors, making it more susceptible to catecholamine‐induced microvascular dysfunction and direct myocyte toxicity.29, 30, 31, 32 Other explanations for midventricular and apical abnormalities are a “base‐to‐apex perfusion gradient” and even transient occlusion of a “wraparound” left anterior descending artery.27, 33, 34
The most remarkable difference between the 2 groups in this study was the clear predilection for women, (postmenopausal women in particular). This has been consistent in most previous reports, including those in which the syndrome was attributed to unrecognized OCAD.34 It is also a feature that sets TS apart from all other ACS. We conclude that the consistency with which female preponderance occurred both in our patients and in prior reports supports a conclusion that physiological differences between genders play a major role in the mechanism of this distinctive contractive pattern, and consequently provide a strategic direction for new investigations. Importantly, 2 studies provide an investigational underpinning to a link between female hormones or lack thereof and TS. The work of Sung et al and Komesaroff et al suggests that estrogen therapy attenuates the response of the vasculature to catecholamines or to mental stress in postmenopausal women.35, 36
Study Limitations
The number of patients available for the comparison limits the ability of the data to convincingly detect differences between patients with contrasting contraction patterns. Nevertheless, the consistency of female dominance in our data and that in clinical series provides reassurance that the difference with regard to gender is real. That fact that physical or emotional stressors were more often recorded in patients with the takotsubo pattern may simply reflect the fact that doctors are more likely to search for it once this diagnosis is considered. The presence of such events is not necessary for the diagnosis of TS, according to current criteria, and was not critical to our conclusions. Our study also has the limitations inherent to all retrospective analysis, and tests such as cardiac MRI were not available for all patients.
Conclusion
Even though there have been previous studies comparing “typical vs atypical” TS, namely apical vs midventricular ballooning,11, 37 this is the first study to investigate the much larger population of patients with suspected ACS and LV dysfunction but no OCAD. We conclude that the predilection for women and for the apical and midventricular segments should guide future research into the pathogenesis of this entity; that if other variants of TS exist, they are quite rare; and that the diagnosis of stress‐induced cardiomyopathy in this setting should be considered with prudence.
References
- 1. Dote K, Sato H, Tateishi H, et al. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases [in Japanese]. J Cardiol 1991. 21 203–214. [PubMed] [Google Scholar]
- 2. Widimsky P, Stellova B, Groch L, et al. Prevalence of normal coronary angiography in the acute phase of suspected ST‐elevation myocardial infarction: experience from the PRAGUE studies. Can J Cardiol 2006. 22 1147–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prasad SB, Richards DA, Sadick N, et al. Clinical and electrocardiographic correlates of normal coronary angiography in patients referred for primary percutaneous coronary intervention. Am J Cardiol 2008. 102 155–159. [DOI] [PubMed] [Google Scholar]
- 4. Larsen AI, Galbraith PD, Ghali WA, et al. Characteristics and outcomes of patients with acute myocardial infarction and angiographically normal coronary arteries. Am J Cardiol 2005. 95 261–263. [DOI] [PubMed] [Google Scholar]
- 5. Patel MR, Chen AY, Peterson ED, et al. Prevalence, predictors and outcomes of patients with non‐ST segment elevation myocardial infarction and insignificant coronary artery disease: results from the CRUSADE initiative. Am Heart J 2006. 152 641–647. [DOI] [PubMed] [Google Scholar]
- 6. Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006. 27 1523–1529. [DOI] [PubMed] [Google Scholar]
- 7. Sharkey SW, Lesser JR, Zenovich AG, et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 2005. 111 472–479. [DOI] [PubMed] [Google Scholar]
- 8. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako‐Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008. 155 408–417. [DOI] [PubMed] [Google Scholar]
- 9. Hurst RT, Askew JW, Reuss CS, et al. Transient midventricular ballooning syndrome: a new variant. J Am Coll Cardiol 2006. 48 579–583. [DOI] [PubMed] [Google Scholar]
- 10. Derian W, Soundarraj D, Rosenberg MJ. Stress‐induced cardiomyopathy: not always apical ballooning. Rev Cardiovasc Med 2007. 8 228–233. [PubMed] [Google Scholar]
- 11. Phanthawimol W, Ito H, Fukuyama O. A case with transient anterolateral wall ballooning syndrome; new variant form of Takotsubo cardiomyopathy? Hawaii Med J 2009. 68 249–252. [PubMed] [Google Scholar]
- 12. Kim DH, Bang DW, Park HK. Atypical basal type takotsubo cardiomyopathy: MDCT findings correlated with echocardiography. Int J Cardiol 2010. 141 e28–e30. [DOI] [PubMed] [Google Scholar]
- 13. Ripa C, Olivieri F, Antonicelli R. Tako‐tsubo‐like syndrome with atypical clinical presentation: case report and literature review. Angiology 2009. 60 513–517. [DOI] [PubMed] [Google Scholar]
- 14. Ferrer MC, Moreno R, Villarreal S, et al. Transient inferior dyskinesia: the tako‐tsubo syndrome applied to the right coronary artery. Int J Cardiol 2007. 116 403–404. [DOI] [PubMed] [Google Scholar]
- 15. Abdulla I, Kay S, Mussap C, et al. Apical sparing in tako‐tsubo cardiomyopathy. Intern Med J 2006. 36 414–418. [DOI] [PubMed] [Google Scholar]
- 16. Chao T, Lindsay J, Collins S, et al. Can acute occlusion of the left anterior descending coronary artery produce a typical “takotsubo” left ventricular contraction pattern? Am J Cardiol 2009. 104 202–204. [DOI] [PubMed] [Google Scholar]
- 17. Kurowski V, Kaiser A, von Hof K, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako‐tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest 2007. 132 809–816. [DOI] [PubMed] [Google Scholar]
- 18. Elian D, Osherov A, Matetzky S, et al. Left ventricular apical ballooning: not an uncommon variant of acute myocardial infarction in women. Clin Cardiol 2006. 29 9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Parodi G, Del Pace S, Carrabba N, et al. Incidence, clinical findings, and outcome of women with left ventricular apical ballooning syndrome. Am J Cardiol 2007. 99 182–185. [DOI] [PubMed] [Google Scholar]
- 20. Azzarelli S, Galassi AR, Amico F, et al. Clinical features of transient left ventricular apical ballooning. Am J Cardiol 2006. 98 1273–1276. [DOI] [PubMed] [Google Scholar]
- 21. Codreanu A, Djaballah W, Angioi M, et al. Detection of myocarditis by contrast‐enhanced MRI in patients presenting with acute coronary syndrome but no coronary stenosis. J Magn Reson Imaging 2007. 25 957–964. [DOI] [PubMed] [Google Scholar]
- 22. Assomull RG, Lyne JC, Keenan N, et al. The role of cardiovascular magnetic resonance in patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Eur Heart J 2007. 28 1242–1249. [DOI] [PubMed] [Google Scholar]
- 23. Joshi SB, Chao T, Herzka DA, et al. Cardiovascular magnetic resonance T2 signal abnormalities in left ventricular ballooning syndrome. Int J Cardiovasc Imaging 2010. 26 227–232. [DOI] [PubMed] [Google Scholar]
- 24. Mitchell JH, Hadden TB, Wilson JM, et al. Clinical features and usefulness of cardiac magnetic resonance imaging in assessing myocardial viability and prognosis in Takotsubo cardiomyopathy (transient left ventricular apical ballooning syndrome). Am J Cardiol 2007. 100 296–301. [DOI] [PubMed] [Google Scholar]
- 25. Haghi D, Fluechter S, Suselbeck T, et al. Cardiovascular magnetic resonance findings in typical versus atypical forms of the acute apical ballooning syndrome (Takotsubo cardiomyopathy). Int J Cardiol 2007. 120 205–211. [DOI] [PubMed] [Google Scholar]
- 26. Eitel I, Behrendt F, Schindler K, et al. Differential diagnosis of suspected apical ballooning syndrome using contrast‐enhanced magnetic resonance imaging. Eur Heart J 2008. 29: 2651–2659. [DOI] [PubMed] [Google Scholar]
- 27. Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005. 352 539–548. [DOI] [PubMed] [Google Scholar]
- 28. Akashi YJ, Nakazawa K, Sakakibara M, et al. The clinical features of takotsubo cardiomyopathy. QJM 2003. 96 563–573. [DOI] [PubMed] [Google Scholar]
- 29. Murphree SS, Saffitz JE. Quantitative autoradiographic delineation of the distribution of beta‐adrenergic receptors in canine and feline left ventricular myocardium. Circ Res 1987. 60 568–579. [DOI] [PubMed] [Google Scholar]
- 30. Cevik C, Nugent K. The role of cardiac autonomic control in the pathogenesis of tako‐tsubo cardiomyopathy. Am Heart J 2008. 156 e31. [DOI] [PubMed] [Google Scholar]
- 31. Lyon AR, Rees PS, Prasad S, et al. Stress (Takotsubo) cardiomyopathy—a novel pathophysiological hypothesis to explain catecholamine‐induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med 2008. 5 22–29. [DOI] [PubMed] [Google Scholar]
- 32. Mori H, Ishikawa S, Kojima S, et al. Increased responsiveness of left ventricular apical myocardium to adrenergic stimuli. Cardiovasc Res 1993. 27 192–198. [DOI] [PubMed] [Google Scholar]
- 33. Hernandez‐Pampaloni M, Keng FY, Kudo T, et al. Abnormal longitudinal, base‐to‐apex myocardial perfusion gradient by quantitative blood flow measurements in patients with coronary risk factors. Circulation 2001. 104 527–532. [DOI] [PubMed] [Google Scholar]
- 34. Ibáñez B, Navarro F, Farré J, et al. Tako‐tsubo transient left ventricular apical ballooning is associated with a left anterior descending coronary artery with a long course along the apical diaphragmatic surface of the left ventricle [in Spanish]. Rev Esp Cardiol 2004. 57 209–216. [DOI] [PubMed] [Google Scholar]
- 35. Sung BH, Ching M, Izzo JL Jr, et al. Estrogen improves abnormal norepinephrine‐induced vasoconstriction in postmenopausal women. J Hypertens 1999. 17 523–528. [DOI] [PubMed] [Google Scholar]
- 36. Komesaroff PA, Esler MD, Sudhir K. Estrogen supplementation attenuates glucocorticoid and catecholamine responses to mental stress in perimenopausal women. J Clin Endocrinol Metab 1999. 84 606–610. [DOI] [PubMed] [Google Scholar]
- 37. Jabara R, Gadesam R, Pendyala L, et al. Comparison of the clinical characteristics of apical and non‐apical variants of “broken heart” (takotsubo) syndrome in the United States. J Invasive Cardiol 2009. 21 216–222. [PubMed] [Google Scholar]


