Abstract
Background:
Outpatients frequently present with elevated natriuretic peptides in the absence of an obvious cardiac abnormality or with normal natriuretic peptides despite echocardiographic findings.
Hypothesis:
We aimed to determine the prognostic value of N‐terminal pro B‐type natriuretic peptide (NTpBNP) in outpatients with normal and abnormal echocardiography.
Methods:
A total of 433 cardiovascular outpatients were included. The prognostic value of NTpBNP in patients with normal and abnormal echocardiography during a 2‐year follow‐up was evaluated.
Results:
Patients with abnormal echocardiography and elevated NTpBNP had a mortality rate of 8.7% and an overall event rate of 20.2% (composite end point of overall mortality, myocardial infarction, and hospitalization for heart failure), which was significantly higher than in patients with abnormal echocardiography and normal NTpBNP, in which no mortality (P = 0.011) and no events were observed (P<0.001). In patients with a normal echocardiography, mortality was 1.5% and 1.8% for patients with normal and elevated NTpBNP, respectively (P = 1.000). Composite event rate was 1.5% and 8.9% (P = 0.093), respectively.
Conclusions:
Patients with low NTpBNP have an excellent prognosis irrespective of echocardiographic findings. Therefore, determination of NTpBNP appears useful in assessing the clinical relevance of echocardiographic findings. © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Stefan Toggweiler, MD and Oliver Borst, MD contributed equally to this work.
Introduction
In patients presenting with cardiac problems in the outpatient setting, risk assessment is of increasing importance as it determines the need for preventive measures with drugs, interventions, and operations. Also, the frequency of follow‐up examinations is largely dependent on the likelihood of disease progression and future cardiovascular events. To that end, clinical findings are complemented by the determination of risk factors such as hypertension, dyslipidemia and diabetes, and cardiac function, most commonly by echocardiography. However, in clinical practice, the prognostic value of echocardiographic findings is often unknown.
Natriuretic peptides like B‐type natriuretic peptide (BNP) and N terminal proBNP (NTpBNP) are reliable biomarkers to detect systolic1 and diastolic dysfunction.2 In the last few years, natriuretic peptides have been proven useful in the diagnosis and monitoring of congestive heart failure3, 4, 5, 6, 7 and to estimate disease severity and prognosis in patients with valvular heart disease,8, 9, 10, 11 congenital heart disease,12 and other cardiac conditions.13
On the other hand, patients not infrequently present with elevated NTpBNP levels in the absence of an obvious cardiac cause.14, 15, 16 However, even in apparently asymptomatic patients and in the general population, incremental levels of BNP has been shown to be associated with increased risk of death and cardiovascular events.17, 18 Therefore, NTpBNP may be a valuable prognostic marker in patients with and without echocardiographic findings.
In outpatients presenting with different cardiac conditions, data concerning the prognostic impact of NTpBNP are quite sparse. Therefore, we examined the prognostic relevance of NTpBNP in cardiac outpatients with normal and abnormal echocardiographic findings.
Methods
Study Protocol
Patients attending the outpatient clinic of the Division of Cardiology were included in this retrospective study. As a tertiary referring clinic the patient population was mixed, consisting of patients with coronary, valvular, or hypertensive heart disease; all forms of idiopathic cardiomyopathy; and patients with congenital heart disease. Patients listed for or after cardiac transplantation and patients with severely reduced ejection fraction (<30%) are seen in a specialized heart failure clinic; they were not included in this study. Between November 2004 and July 2007, all patients whose NTpBNP was determined and who were examined with echocardiography on the same day were included for analysis (n = 470). During this time period, a total of 1700 patients were seen in our outpatient clinic. Thus, the inclusion rate was 26%. Two‐year outcome was available in the majority of the patients because patients are seen periodically, with stable patients usually seen every 1 or 2 years. In the remaining patients, the treating general practitioner was called to obtain data about clinical outcome. Eventually, the 2‐year outcome was available in 433 patients (92%). The remaining patients were excluded. Ethics review board approval was obtained and consent was waived due to the retrospective nature of the study.
NT‐pBNP
NTpBNP was determined using a microparticle enzyme immunoassay (Roche Elecsys, Basel, Switzerland). NTpBNP, clinical examination, and echocardiography were always carried out on the same day. Normal values of NTpBNP were defined according to age and gender as published by Galasko et al. A value of ≤100 ng/L for males <60 years, ≤164 ng/L for females <60 years, ≤172 ng/L for males ≥60 years and ≤225 ng/L for females ≥60 years19 was considered normal.
Echocardiography
In all subjects, Doppler echocardiography was performed by experienced echocardiographers according to the Guidelines of the American Society of Echocardiography.20 Left ventricular diameters were measured according to the Penn convention. Left ventricular mass was calculated by the Devereux‐formula and normalized by body surface area. Normal values were defined as left‐ventricular mass index <110 g/m2 for women and <134 g/m2 for men. Left ventricular ejection fraction was calculated using Simpson's apical biplane method. Diastolic function was categorized as normal, impaired relaxation, pseudonormalization, or restrictive filling. Valve disease was classified as no/trivial, mild, moderate, and severe. The function of reconstructed or replaced valves was judged similar to native valves. A normal echocardiography was defined to have (1) a left ventricular ejection fraction ≥50%, (2) no relevant diastolic dysfunction (impaired relaxation was considered normal in subjects >50 years), (3) no or only mild valvular regurgitation, (4) no valvular stenosis, and (5) a normal left ventricular mass index.
Statistical Analysis
Statistical analysis was performed using SPSS 15 (SPSS Inc., Chicago, IL). If not indicated otherwise, data are presented as mean ± the standard deviation for continuous and as number and frequencies for categorical variables. Continuous variables were compared using Student t test, and categorical variables using χ 2 test. Univariate and multivariate Cox regression analyses were carried out to identify predictors of death and cardiovascular outcome. Predictors of outcome included age, New York Heart Association (NYHA) class >I, clinical signs of heart failure, elevation of NTpBNP, an abnormal echocardiography, and medical treatment for heart failure such as angiotensin converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), β‐blockers, spironolactone/eplerenone, and loop diuretics. Parameters that were statistically significant in univariate analysis were used for multivariate analysis. Kaplan‐Meier curves were drawn to visualize the outcomes of the different groups. They were compared with the log‐rank test. A 2‐sided P < 0.05 was considered statistically significant.
Results
Study Population
A total of 433 patients were analyzed. Mean age was 60 ± 16 years, and 65% of the patients were male. Most of the patients had valvular heart disease (59%) and coronary artery disease (34%). Patients also presented with dilated (2%), hypertensive (5%), hypertrophic (2%), or restrictive (1%) cardiomyopathy, and 7% of the patients had congenital heart disease. Cardiovascular risk factors were frequently present, the most common being hypertension (59%) and current or former smoking (41%). Most of the patients were taking cardiovascular medication, including 56% taking an ACEI or ARB and 50% taking a β‐blocker. Twenty‐eight percent were taking loop diuretics. Two hundred twelve (49%) were in NYHA class I, 147 (34%) were in class II, 70 (16%) were in class III and 4 (1%) presented with NYHA class IV. NT‐pBNP was elevated in 308 (71%) of the patients. Median NTpBNP was 334 ng/L (lower quartile 124 ng/L, upper quartile 976 ng/L). Forty‐seven patients (11%) were in atrial fibrillation. Mean ejection fraction (EF) was 57 ± 13%, 339 (78%) patients had a preserved EF (≥50%). Table 1 compares baseline characteristics of patients with a normal echocardiography and normal NTpBNP to patients with a normal echocardiography and elevated NTpBNP. Table 2 compares baseline characteristics of patients with an abnormal echocardiography and normal NTpBNP to patients with an abnormal echocardiography and elevated NTpBNP.
Table 1.
Patients With Normal Echocardiography and Normal or Elevated NTpBNP
| NTpBNP Normal, n = 66 | % | NTpBNP Elevated, n = 56 | % | P Value | |
|---|---|---|---|---|---|
| Age (y) | 52 ± 15 | 63 ± 12 | <.001 | ||
| Male gender | 44 | 67 | 39 | 70 | 0.725 |
| NYHA class > I | 23 | 35 | 22 | 39 | 0.707 |
| Coronary artery disease | 16 | 24 | 30 | 54 | 0.001 |
| Prior myocardial infarction | 5 | 8 | 14 | 25 | 0.008 |
| Prior PCI/CABG | 11 | 17 | 25 | 45 | 0.001 |
| Prior valve operation | 10 | 15 | 18 | 32 | 0.026 |
| Pulmonary disease | 8 | 12 | 8 | 14 | 0.724 |
| Hypertension | 34 | 54 | 39 | 70 | 0.080 |
| Diabetes | 10 | 16 | 9 | 16 | 0.976 |
| Atrial fibrillation | 1 | 2 | 6 | 11 | 0.047 |
| NTpBNP (ng/L) | 65 ± 42 | 494 ± 514 | <0.001 | ||
| GFR (mL/min) | 85 ± 25 | 66 ± 21 | <0.001 | ||
| GFR < 60 mL/min | 11 | 17 | 21 | 38 | 0.011 |
| Echocardiography | |||||
| Ejection fraction (%) | 63 ± 5 | 62 ± 6 | 0.356 | ||
| LV‐EDD (mm) | 49 ± 5 | 48 ± 4 | 0.636 | ||
| Septum (mm) | 10.5 ± 2.0 | 10.9 ± 1.7 | 0.282 | ||
| Posterior wall (mm) | 9.2 ± 1.2 | 9.2 ± 1.3 | 0.919 | ||
| LV‐MMI | 94 ± 23 | 101 ± 23 | 0.112 | ||
Abbreviations: CABG, coronary artery bypass grafting; GFR, glomerular filtration rate; LV‐EDD, left‐ventricular end‐diastolic diameter; LV‐MMI, left‐ventricular myocardial mass index; NTpBNP, N‐terminal pro B‐type natriuretic peptide; PCI, percutaneous coronary intervention.
Table 2.
Patients With Abnormal Echocardiography and Normal or Elevated NTpBNP
| NTpBNP normal, n = 59 | % | NTpBNP elevated, n = 252 | % | P Value | |
|---|---|---|---|---|---|
| Age (y) | 54 ± 16 | 63 ± 16 | <0.001 | ||
| Male gender | 41 | 70 | 158 | 63 | 0.369 |
| NYHA class >I | 18 | 31 | 158 | 63 | <0.001 |
| Coronary artery disease | 9 | 15 | 93 | 37 | 0.001 |
| Prior myocardial infarction | 4 | 7 | 45 | 18 | 0.045 |
| Prior PCI/CABG | 7 | 12 | 70 | 28 | 0.010 |
| Prior valve operation | 8 | 14 | 70 | 28 | 0.022 |
| Pulmonary disease | 1 | 2 | 33 | 13 | 0.011 |
| Hypertension | 23 | 39 | 159 | 64 | <0.001 |
| Diabetes | 5 | 9 | 35 | 14 | 0.251 |
| Atrial fibrillation | 1 | 2 | 36 | 14 | 0.007 |
| NTpBNP (ng/L) | 85 ± 51 | 1696 ± 3503 | <0.001 | ||
| GFR (mL/min) | 85 ± 25 | 64 ± 24 | <0.001 | ||
| GFR < 60 mL/min | 6 | 10 | 121 | 49 | <0.001 |
| Echocardiography | |||||
| Ejection fraction (%) | 60 ± 9 | 54 ± 15 | 0.004 | ||
| Ejection fraction ≥ 50% | 51 | 90 | 165 | 67 | 0.001 |
| LV‐EDD (mm) | 52 ± 8 | 53 ± 10 | 0.346 | ||
| Septum (mm) | 11.6 ± 2.3 | 11.9 ± 2.9 | 0.472 | ||
| Posterior wall (mm) | 9.6 ± 1.9 | 9.9 ± 1.9 | 0.171 | ||
| LV‐MMI (g/m2) | 124 ± 40 | 140 ± 44 | 0.015 | ||
| Diastolic dysfunction | 12 | 25 | 40 | 20 | 0.397 |
| Aortic regurgitation | 8 | 14 | 25 | 10 | 0.420 |
| Mitral regurgitation | 10 | 17 | 34 | 14 | 0.508 |
| Tricuspid regurgitation | 0 | 0 | 17 | 7 | 0.051 |
| Aortic stenosis | 11 | 19 | 63 | 25 | 0.289 |
| Mitral stenosis | 6 | 10 | 31 | 12 | 0.628 |
Abbreviations: AR, aortic regurgitation; AS, aortic stenosis; CABG, coronary artery bypass grafting; GFR, glomerular filtration rate; LV‐EDD, left‐ventricular end‐diastolic diameter; LV‐MMI, left‐ventricular myocardial mass index; MR, mitral regurgitation; MS, mitral stenosis; NTpBNP, N‐terminal pro B‐type natriuretic peptide; PCI, percutaneous coronary intervention; TR, tricuspid regurgitation.
Prognostic Value of NTpBNP in Patients With Normal and Abnormal Echocardiography
To assess the prognostic relevance of elevated NTpBNP levels in the presence or absence of echocardiographic abnormalities, data were analyzed in 4 groups as presented in Table 3. In patients with normal echocardiography, 2‐year mortality was 1.5% in patients with normal NTpBNP and 1.8% in patients with an elevated NTpBNP (P = 1.000). However, the rate of hospitalization for heart failure was significantly higher in patients with elevated NTpBNP (7.3% and 0% for patients with elevated and normal NTpBNP, respectively; P = 0.042). The combined end point of death, myocardial infarction, and hospitalization for heart failure occurred in 1.5% of the patients with normal NTpBNP and in 8.9% of those with elevated NTpBNP (P = 0.093).
Table 3.
Two‐Year Outcome of Patients With Normal and Elevated NTpBNP and Normal or Abnormal Echocardiography
| Normal Echo, Normal NTpBNP, n = 66 | Normal Echo, Elevated NTpBNP, n = 56 | Abnormal Echo, Normal NTpBNP, n = 59 | Abnormal Echo, Elevated NTpBNP, n = 252 | |||||
|---|---|---|---|---|---|---|---|---|
| Mortality | 1 | (1.5%) | 1 | (1.8%) | 0 | (0.0%)a | 22 | (8.7%)a |
| Hospitalization for heart failure | 0 | (0%)a | 4 | (7.3%)a | 0 | (0.0%)b | 32 | (13.6%)b |
| Myocardial infarction | 0 | (0%) | 0 | (0%) | 0 | (0.0%) | 5 | (2.1%) |
| Any event | 1 | (1.5%) | 5 | (8.9%) | 0 | (0.0%)b | 51 | (20.2%)b |
Abbreviations: NTpBNP, N‐terminal pro B‐type natriuretic peptide.
Significant at the P < 0.05 level.
Significant at the P < 0.001 level.
Patients with abnormal echocardiography and elevated NTpBNP had a 2‐year mortality rate of 8.7%, which was significantly more than patients with a normal NTpBNP and abnormal echocardiography, which had a mortality rate of 0.0% (P = 0.011). The rate of hospitalization for heart failure was significantly higher in patients with elevated NTpBNP (13.6% and 0.0% for patients with elevated and normal NTpBNP, respectively; P = 0.001). The rate of the combined end point was 0% and 20.2% for patients with normal and elevated NTpBNP, respectively (P < 0.001).
Figure 1, A shows the Kaplan‐Meier estimate of survival free from death of any cause, hospitalization for heart failure, and myocardial infarction.
Figure 1.
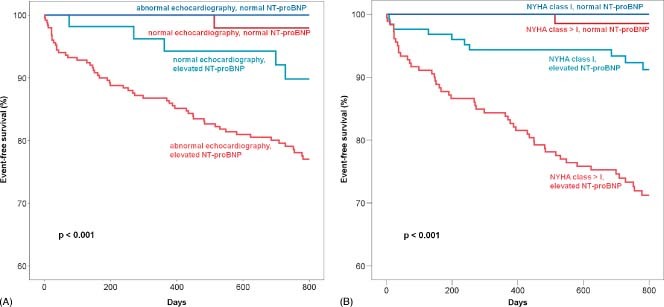
Event‐free survival in relation to N‐terminal pro B‐type natriuretic peptide (NTpBNP) and echocardiographic results (A), and in relation to NTpBNP and New York Heart Association (NYHA) class (B). Kaplan‐Meier curves are shown for patients with normal and abnormal echocardiography and normal and elevated NTpBNP (A), and for patients in NYHA class I and NYHA class >I and normal and elevated NTpBNP (B). P values indicate overall log‐rank comparison. Events are all‐cause mortality, myocardial infarction, and hospitalization for heart failure.
Patients With Preserved Ejection Fraction
In the subgroup of patients with preserved ejection fraction (≥50%, n = 339), an elevation of NTpBNP was still associated with an increased 2‐year incidence for hospitalization for heart failure (11.2% and 0% for patients with elevated and normal NTpBNP, respectively; P<0.001). Mortality was 4.5% and 0.9% for patients with elevated and normal NTpBNP, respectively (P = 0.105). The rate of the combined end point was 1% and 15% for patients with normal and elevated NTpBNP, respectively (P<0.001).
Predictors of Cardiovascular Events
In univariate analysis, age > 60 years (hazard ratio [HR]: 4.13, 95% confidence interval [CI]: 2.17–7.85), NYHA class > I (HR: 3.99, 95% CI: 2.22–7.15), clinical signs of heart failure (HR: 2.76, 95% CI: 1.72–4.44), elevated NTpBNP (HR: 14.15, 95% CI: 3.47–57.69), an abnormal echocardiography (HR: 3.10, 95% CI: 1.48–6.45), and therapy with loop diuretics (HR: 4.25, 95% CI: 2.65–6.83) were significant predictors of the combined end point of mortality, myocardial infarction, and hospitalization for heart failure. These parameters were used for multivariate analysis (Table 4). Elevated NTpBNP, NYHA class > I, age ≥ 60 years, and therapy with loop diuretics remained significant predictors of cardiovascular outcome. Therapy with relevant cardiovascular drugs (ACEI/ARB, β‐blocker, spironolactone, diuretics) did not alter the prognostic value of NT‐proBNP (multivariate analysis: HR: 9.40, 95% CI: 2.27–38.97; P = 0.002).
Table 4.
Multivariate Predictors for the Combined Endpoint of Mortality, Myocardial Infarction, and Hospitalization for Heart Failure
| Variable | HR | 95% CI | P Value |
|---|---|---|---|
| Age ≥ 60 y | 2.36 | 1.22–4.59 | 0.011 |
| NYHA class >1 | 2.03 | 1.08–3.81 | 0.028 |
| Clinical signs of heart failure | 1.48 | 0.90–2.43 | 0.119 |
| NTpBNP elevated | 6.43 | 1.53–27.00 | 0.011 |
| Abnormal echocardiography | 1.63 | 0.77–3.45 | 0.203 |
| Therapy with loop diuretics | 1.86 | 1.10–3.15 | 0.020 |
Abbreviations: CI, confidence interval; HR, hazard ratio; NTpBNP, N‐terminal pro B‐type natriuretic peptide; NYHA, New York Heart Association.
Figure 1B shows Kaplan‐Meier estimate of survival free from death of any cause, hospitalization for heart failure, and myocardial infarction in relation to NTpBNP and NYHA class.
Discussion
The present study for the first time demonstrates that NTpBNP is an important prognostic marker in cardiac outpatients assessed clinically and with the help of echocardiography. Indeed, patients with normal NTpBNP levels had an excellent prognosis irrespective of echocardiographic findings, whereas in patients with abnormal echocardiographic findings NTpBNP separated those with from those without future major cardiovascular events. Thus, NTpBNP is a useful prognostic marker not only in cardiac outpatients as a whole, but specifically in those with an abnormal echocardiography. NTpBNP levels provide important information beyond clinical findings and echocardiography as to the future clinical relevance of cardiac abnormalities, which are often difficult to classify with this imaging technique alone. In the present study, multivariate analysis including age, symptoms (NYHA class), signs of heart failure, NTpBNP, echocardiography, and therapy with diuretics revealed NTpBNP as the strongest predictor of future adverse cardiovascular events including death, myocardial infarction, and hospitalization for heart failure, with an impressive hazard ratio of 6.4. Furthermore, NTpBNP was a significant predictor for adverse outcome in patients with ejection fraction ≥50%. This finding is in line with previously published studies, where it has been demonstrated that both BNP and NTpBNP were strong predictors of adverse cardiovascular events in patients with preserved ejection fraction.20, 21, 22, 23
Use of diuretics such as furosemide or torsemide was associated with an increased incidence of adverse events in multivariate analysis (hazard ratio, 1.9). Although there is probably a selection bias (patients with severe heart failure are more likely treated with a diuretic), previous studies have shown that therapy with diuretics is associated with worse outcome, especially when used in higher doses.24, 25 However, use of cardiovascular drugs did not alter the prognostic value of NT‐pBNP.
NTpBNP in Patients With Abnormal Echocardiography
Of note, the combination of elevated levels of NTpBNP and echocardiographic abnormalities was particularly predictive of a worse outcome. Such patients exhibited a 2‐year mortality of 9%, compared to 0% for patients with abnormal echocardiography and normal NTpBNP, respectively. The prognostic impact of NTpBNP in patients with abnormal echocardiographies was not only significant for mortality, but also for hospitalization for heart failure and cumulative event rate. These findings may be of particular clinical importance as it appears from these retrospective data that a low NTpBNP predicts a very low rate of major cardiovascular events during the next 2 years. This may help in decision making in regard to the frequency of follow‐up examinations, the necessity for further evaluation, and/or possible interventions or operations.
NTpBNP in Patients With Normal Echocardiography
In patients with normal echocardiography, the rate of mortality was the same in patients with normal and elevated NTpBNP, but the rate of hospitalization for heart failure was higher in the latter. Elevated levels of NTpBNP in the absence of obvious cardiac abnormalities are not uncommon. Usually, they are related to noncardiac pathologies like renal failure, pulmonary hypertension, or chronic obstructive pulmonary disease.14, 15, 16 However, although such patients are commonly seen in cardiac clinics, the prognostic impact of elevated NTpBNP in this situation has not been appropriately studied. To address the problem of extracardiac elevation of natriuretic peptides, reference values for both BNP and NTpBNP, stratifying for different variables like renal function have been proposed.26, 27 Alternatively, grey zones have been suggested.28 In the present study, such patients presented more often with coronary artery disease and with prior percutaneous coronary intervention or coronary artery bypass grafting, and many had undergone a prior valve replacement or reconstruction. As expected, renal failure was more common in this group than in patients with normal NTpBNP. Finally, 6 patients (11%) were in atrial fibrillation, which is also a known cause for myocardial stretch and in turn elevated natriuretic peptides.29 Nevertheless, regardless of NTpBNP, patients with a normal echocardiography had a low rate of major cardiovascular events during the 2‐year follow‐up.
Limitations
This retrospective study included only patients in whom NTpBNP was determined and in whom the physician in charge ordered an echocardiography. The study population therefore represents a selection of cardiac outpatients. Although in this outpatient clinic of a university department NTpBNP and echocardiography are commonly used, inclusion of every single patient seen at this institution may have led to slightly different results. The number of patients with either normal NT‐pBNP and/or normal echocardiography is low. Furthermore, it is often difficult to classify echocardiographic findings as normal or abnormal. In this study, we considered an echocardiographic examination as normal if left ventricular systolic and/or diastolic function was normal and if no hemodynamically relevant valvular lesions and no left ventricular hypertrophy could be detected. In the absence of all these factors, it is very likely that elevated NTpBNP levels have an extracardiac cause. Among other factors, levels of NTpBNP were used for therapy adjustments in our patients, and these therapy changes may have influenced prognosis. In spite of these limitations, the results of this study reflect everyday practice and may therefore be relevant for patient management.
Conclusion
This study underscores the ability of NTpBNP as a surrogate of hemodynamics and of cardiac stress to predict future cardiovascular events in patients with normal and abnormal echocardiographic findings. NTpBNP was the strongest independent predictor of prognosis in cardiac outpatients. In addition, NTpBNP separated well patients with abnormal echocardiographic findings with an excellent or poor prognosis, respectively. Therefore, determination of NTpBNP appears useful in assessing the clinical relevance of echocardiographic findings.
References
- 1. McDonagh TA, Robb SD, Murdoch DR, et al. Biochemical detection of left‐ventricular systolic dysfunction. Lancet. 1998;351:9–13. [DOI] [PubMed] [Google Scholar]
- 2. Mottram PM, Leano R, Marwick TH. Usefulness of B‐type natriuretic peptide in hypertensive patients with exertional dyspnea and normal left ventricular ejection fraction and correlation with new echocardiographic indexes of systolic and diastolic function. Am J Cardiol. 2003;92:1434–1438. [DOI] [PubMed] [Google Scholar]
- 3. Mueller C, Breithardt T, Laule‐Kilian K, et al. The integration of BNP and NT‐proBNP into clinical medicine. Swiss Med Wkly. 2007;137:4–12. [DOI] [PubMed] [Google Scholar]
- 4. Yasue H, Yoshimura M, Sumida H, et al. Localization and mechanism of secretion of B‐type natriuretic peptide in comparison with those of A‐type natriuretic peptide in normal subjects and patients with heart failure. Circulation. 1994;90:195–203. [DOI] [PubMed] [Google Scholar]
- 5. Mueller C, Scholer A, Laule‐Kilian K, et al. Use of B‐type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med. 2004;350:647–654. [DOI] [PubMed] [Google Scholar]
- 6. Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50:2357–2368. [DOI] [PubMed] [Google Scholar]
- 7. Maeda K, Tsutamoto T, Wada A, et al. High levels of plasma brain natriuretic peptide and interleukin‐6 after optimized treatment for heart failure are independent risk factors for morbidity and mortality in patients with congestive heart failure. J Am Coll Cardiol. 2000;36:1587–1593. [DOI] [PubMed] [Google Scholar]
- 8. Lancellotti P, Moonen M, Magne J, et al. Prognostic effect of long‐axis left ventricular dysfunction and B‐type natriuretic peptide levels in asymptomatic aortic stenosis. Am J Cardiol. 2010;105:383–388. [DOI] [PubMed] [Google Scholar]
- 9. Potocki M, Mair J, Weber M, et al. Relation of N‐terminal pro‐B‐type natriuretic peptide to symptoms, severity, and left ventricular remodeling in patients with organic mitral regurgitation. Am J Cardiol. 2009;104:559–564. [DOI] [PubMed] [Google Scholar]
- 10. Pizarro R, Bazzino OO, Oberti PF, et al. Prospective validation of the prognostic usefulness of brain natriuretic peptide in asymptomatic patients with chronic severe mitral regurgitation. J Am Coll Cardiol. 2009;54:1099–1106. [DOI] [PubMed] [Google Scholar]
- 11. Nessmith MG, Fukuta H, Brucks S, et al. Usefulness of an elevated B‐type natriuretic peptide in predicting survival in patients with aortic stenosis treated without surgery. Am J Cardiol. 2005;96:1445–1448. [DOI] [PubMed] [Google Scholar]
- 12. Koch A, Zink S, Singer H. B‐type natriuretic peptide in paediatric patients with congenital heart disease. Eur Heart J. 2006;27:861–866. [DOI] [PubMed] [Google Scholar]
- 13. Allanore Y, Meune C. N‐terminal pro brain natriuretic peptide: the new cornerstone of cardiovascular assessment in systemic sclerosis. Clin Exp Rheumatol. 2009;27:59–63. [PubMed] [Google Scholar]
- 14. McCullough PA, Sandberg KR. B‐type natriuretic peptide and renal disease. Heart Fail Rev. 2003;8:355–358. [DOI] [PubMed] [Google Scholar]
- 15. Hogenhuis J, Voors AA, Jaarsma T, et al. Anaemia and renal dysfunction are independently associated with BNP and NT‐proBNP levels in patients with heart failure. Eur J Heart Fail. 2007;9:787–794. [DOI] [PubMed] [Google Scholar]
- 16. Nagaya N, Nishikimi T, Uematsu M, et al. Plasma brain natriuretic peptide as a prognostic indicator in patients with primary pulmonary hypertension. Circulation. 2000;102: 865–870. [DOI] [PubMed] [Google Scholar]
- 17. Wang TJ, Larson MG, Levy D, et al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350:655–663. [DOI] [PubMed] [Google Scholar]
- 18. Linssen GCM, Bakker SJL, Voors AA, et al. N‐terminal pro‐B‐type natriuretic peptide is an independent predictor of cardiovascular morbidity and mortality in the general population. Eur Heart J. 2010;31:120–127. [DOI] [PubMed] [Google Scholar]
- 19. Galasko GIW, Lahiri A, Barnes SC, et al. What is the normal range for N‐terminal pro‐brain natriuretic peptide? How well does this normal range screen for cardiovascular disease? Eur Heart J. 2005;26:2269–2276. [DOI] [PubMed] [Google Scholar]
- 20. Gardin JM, Adams DB, Douglas PS, et al. Recommendations for a standardized report for adult transthoracic echocardiography: a report from the American Society of Echocardiography's nomenclature and standards committee and task force for a standardized echocardiography report. J Am Soc Echocardiogr. 2002;15:275–290. [DOI] [PubMed] [Google Scholar]
- 21. Grewal J, McKelvie RS, Persson H, et al. Usefulness of N‐terminal pro‐brain natriuretic peptide and brain natriuretic peptide to predict cardiovascular outcomes in patients with heart failure and preserved left ventricular ejection fraction. Am J Cardiol. 2008;102:733–737. [DOI] [PubMed] [Google Scholar]
- 22. Valle R, Aspromonte N, Feola M, et al. B‐type natriuretic peptide can predict the medium‐term risk in patients with acute heart failure and preserved systolic function. J Card Fail. 2005;11:498–503. [DOI] [PubMed] [Google Scholar]
- 23. Paul B, Soon KH, Dunne J, et al. Diagnostic and prognostic significance of plasma N‐terminal‐pro‐brain natriuretic peptide in decompensated heart failure with preserved ejection fraction. Heart Lung Circ. 2008;17:497–501. [DOI] [PubMed] [Google Scholar]
- 24. O'Connor CM, Hasselblad V, Mehta RH, et al. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol. 2010;55:872–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Andersson SE, Edvinsson ML, Bjork J, et al. High NT‐proBNP is a strong predictor of outcome in elderly heart failure patients. Am J Geriatr Cardiol. 2008;17:13–20. [DOI] [PubMed] [Google Scholar]
- 26. O'Hanlon R, O'Shea P, Ledwidge M, et al. The biologic variability of B‐type natriuretic peptide and N‐terminal pro‐B‐type natriuretic peptide in stable heart failure patients. J Card Fail. 2007;13: 50–55. [DOI] [PubMed] [Google Scholar]
- 27. Bruins S, Fokkema MR, Romer JW, et al. High intraindividual variation of B‐type natriuretic peptide (BNP) and amino‐terminal proBNP in patients with stable chronic heart failure. Clin Chem 2004;50:2052–2058. [DOI] [PubMed] [Google Scholar]
- 28. Maisel A, Mueller C, Adams K Jr, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10:824–839. [DOI] [PubMed] [Google Scholar]
- 29. Wozakowska‐Kaplon B, Opolski G, Herman Z, et al. Natriuretic peptides in patients with atrial fibrillation. Cardiol J. 2008;15: 525–529. [PubMed] [Google Scholar]


