Abstract
Alveolar soft part sarcoma is a rare soft‐tissue neoplasm that accounts for <1% of all soft‐tissue sarcomas. Most cases arise in the extremities and head and neck region of young adults. The common sites of metastasis are lung, brain, and bone. Cardiac metastasis is extremely rare, in particular. Here we present the diagnostic evaluation and successful surgical resection of such a cardiac tumor in a patient aged 50 years with a histology‐confirmed diagnosis of metastatic alveolar soft part sarcoma. © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Clinical Summary
A woman aged 50 years with symptoms of heart failure was referred to our hospital for further diagnostic evaluation. Twenty years before, the patient had been diagnosed with alveolar soft part sarcoma (ASPS) in her right thigh. The primary tumor was treated by complete surgical resection and radiotherapy. Five years later, a brain metastasis was excised. Thereafter, the patient remained alive and well, with no evidence of disease for the last 15 years.
At admission, transthoracic echocardiography (TTE) revealed an unexpected mass measuring 37 × 34 mm within the left ventricle, with a blockade of the right coronary leaflet of the aortic valve. The aortic valve itself appeared not pathological, without any tumor infiltration (Figure 1). Subsequently, magnetic resonance imaging (MRI) visualized a large (41 × 31 × 44 mm), slightly inhomogeneous mass in the anterior basal septum narrowing the left ventricular outflow tract. The well‐definable tumor was presenting with rapid contrast enhancement in first‐pass perfusion imaging with accentuation of the peripheral parts presumably due to central tumor necrosis. On early and late enhancement imaging, inhomogeneous contrast uptake was revealed (Figure 2).
Figure 1.
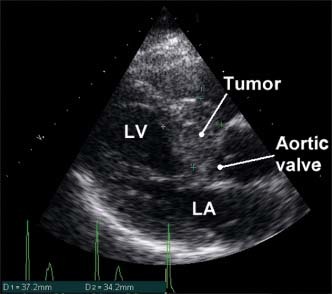
Transthoracic echocardiography: parasternal long axis showing a large round mass adherent to the anterior basal septum narrowing the left ventricular outflow tract. Abbreviations: LA, left atrium; LV, left ventricle.
Figure 2.
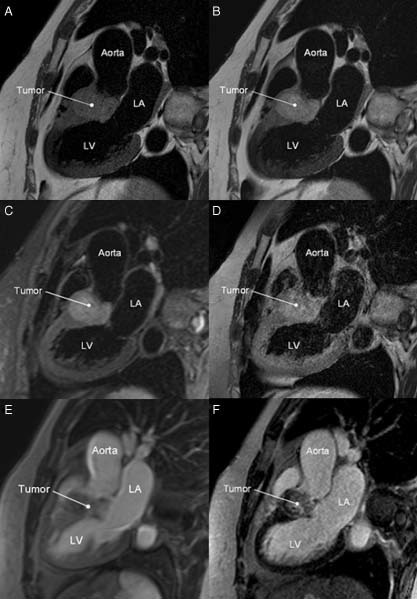
On MRI, the tumor was isointense to normal myocardium on T1‐weighted imaging (A) and hyperintense on T2‐weighted imaging without (B) and with (C) fat suppression. After application of contrast media, the mass was presenting with inhomogeneous contrast uptake on T1‐weighted imaging with fat suppression (D) as well as on early (E) and delayed (F) enhanced imaging. Abbreviations: LA, left atrium; LV, left ventricle; MRI, magnetic resonance imaging.
The patient was taken to the operating theater, where a median sternotomy was performed and cardiopulmonary bypass was installed via aorta‐right atrium cannulation with moderate hypothermia. Because of the extensive growth and infiltration, it was impossible to excise the tumor mass completely. After cleaning and testing of the leaflets, the aortic valve was functioning normally (Figure 3). The resected specimen measured 30 × 25 × 15 mm and was composed of a marginally excised soft polypoid mass measuring 25 mm in maximum diameter. The cut section was tan‐yellow and glistening. Histological examination of the tumor confirmed the diagnosis of metastatic ASPS (Figure 4).
Figure 3.
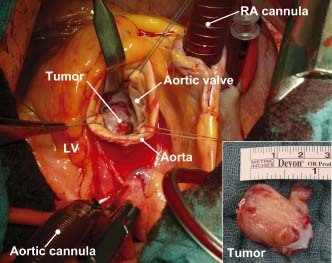
Intraoperative photograph showing the resected tumor formation attached to the right coronary leaflet of the aortic valve. Abbreviations: LA, left atrium; LV, left ventricle.
Figure 4.
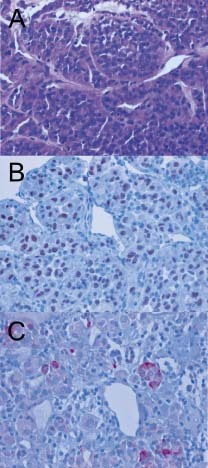
Histology of the resected tumor tissue from the left ventricle. The tumor consisted of large, polygonal tumor cells (A) arranged in an alveolar pattern and variably sized compact cell nests surrounded by well‐vascularized and partially hyalinized fibrous stroma. Mitotic figures were scarce. Several tumor cells contained brightly eosinophilic intracytoplasmic crystalloid inclusions. Immunohistochemistry (B) revealed strong nuclear reactivity for TFE3. In addition, isolated tumor cells (C) were also reactive for desmin. Abbreviations: TFE3, transcription factor binding to IGHM enhancer 3.
Comment
Alveolar soft part sarcoma is a rare soft‐tissue tumor that accounts for 0.5%–0.9% of all soft‐tissue sarcomas.1 It usually presents as an indolent slow‐growing malignancy in adolescents and younger adults.2 These tumors are most often seen in the deep soft tissue of the extremities or head and neck region, but ASPS has been reported in numerous sites, including bone, mediastinum, and uterus.3., 4. The common sites of metastasis are lung, bone, and brain.5 The coexistence of ASPS and cardiac metastasis is very rare6; however, because ASPS might metastasize to the heart and induce severe heart failure, a cardiac examination should be performed in patients with ASPS.
Clinical symptoms of these cardiac tumors could be absent or nonspecific, so their diagnosis and treatment may be delayed.2 The radiological evaluation of these neoplasms has been greatly facilitated by the development of noninvasive cardiac imaging. Although TTE is useful in the initial evaluation of suspected cardiac tumors, transesophageal echocardiography is frequently required for a more comprehensive and accurate assessment.7 The utility of cardiac‐gated MRI in the preoperative evaluation of cardiac tumors is well established. The wide field of view, high contrast and spatial resolution, and multiplanar imaging capabilities allow precise demonstration and localization of a tumor, including its anatomic relationship to the cardiac chambers and any involvement of the myocardium, pericardium, or contiguous structures.8
Conclusion
The presented case shows a patient with a very rare huge metastatic ASPS in the left ventricle. These tumors produce a wide variety of symptoms. Although the mean survival time of patients with ASPS is relatively long, it remains as a malignant disease with fatal outcome. The most useful diagnostic tools are echocardiography and MRI, which in almost all cases precisely locates the tumor and defines its extent. The treatment of choice for these cardiac tumors is a combination of surgical resection and radiotherapy, which may significantly prolong the survival time in many patients.
Acknowledgements
The authors would like to thank Johannes Rösch for his excellent technical assistance.
References
- 1. Ordóñez NG. Alveolar soft part sarcoma: a review and update. Adv Anat Pathol. 1999;6:125–139. [DOI] [PubMed] [Google Scholar]
- 2. Lieberman PH, Brennan MF, Kimmel M, et al. Alveolar soft‐part sarcoma: a clinico‐pathologic study of half a century. Cancer. 1989;63:1–13. [DOI] [PubMed] [Google Scholar]
- 3. Anderson ME, Hornicek FJ, Gebhardt MC, et al. Alveolar soft part sarcoma: a rare and enigmatic entity. Clin Orthop Relat Res. 2005; 438:144–148. [DOI] [PubMed] [Google Scholar]
- 4. Aulmann S, Longerich T, Schirmacher P, et al. Detection of the ASPSCR1‐TFE3 gene fusion in paraffin‐embedded alveolar soft part sarcomas. Histopathology. 2007;50:881–886. [DOI] [PubMed] [Google Scholar]
- 5. Akiyama Y, Baba T, Ibayashi Y, et al. Alveolar soft part sarcoma in brain with cardiac metastasis: a case report. Int J Cardiol. 2007;114:e93–95. [DOI] [PubMed] [Google Scholar]
- 6. Oniki T, Hashimoto Y, Fujinuma Y, et al. Hypervascular metastatic cardiac tumors: an unknown cause of mitral valve prolapse. Intern Med. 1992;31:78–81. [DOI] [PubMed] [Google Scholar]
- 7. Alam M, Rosman HS, Grullon C. Transesophageal echocardiography in evaluation of atrial masses. Angiology. 1995;46:123–128. [DOI] [PubMed] [Google Scholar]
- 8. Freedberg RS, Kronzon I, Rumancik WM, et al. The contribution of magnetic resonance imaging to the evaluation of intracardiac tumors diagnosed by echocardiography. Circulation. 1988;77: 96–103. [DOI] [PubMed] [Google Scholar]


