Abstract
Background:
Earthquake exposure is associated with adverse consequences for cardiovascular disease. However, in the context of depressive symptoms, the prognostic significance of heart failure (HF) related to earthquake‐related loss has not been characterized before.
Hypothesis:
To determine the prognostic impact of earthquake‐related loss on event‐free survival in patients with HF, with depression as a modifying factor.
Methods:
Depressive symptoms were assessed by using the Zung Self‐Rating Depression Scale in 404 HF patients who were followed up for 2 years after the earthquake to collect data on mortality and readmission. The Kaplan‐Meier method was used to compare event‐free survival between patients with and without earthquake‐related loss. Cox proportional hazard regression modeling was used to examine the predicted outcomes for baseline variables.
Results:
The proportion of patients with moderate/severe depressive symptoms among the HF patients with earthquake‐related loss is much higher than their counterparts (27.038% vs 17.84%, P = 0.039). Heart failure patients without loss experienced longer event‐free survival than patients with loss (P = 0.002), especially among patients without depressive symptoms (P = 0.003). Meanwhile, in a Cox proportional hazard regression model, the event‐free survival was associated with earthquake‐related loss, left ventricular ejection fraction, depressive symptoms, and chronic obstructive pulmonary disease or asthma.
Conclusions:
Heart failure patients without earthquake‐related loss experienced longer event‐free survival than did HF patients with severe loss. Earthquake‐related loss was a predictor of poor outcomes in HF patients, particularly in patients without depression. © 2011 Wiley Periodicals, Inc.
The work was supported by grants from the National High‐Tech Research and Development Program of China (2008AA022601). The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
On May 12, 2008, an earthquake of magnitude 8.0 on the Richter scale struck the southwestern region of China, mainly in Sichuan province. Earthquakes are good examples of unique, unpredictable disasters that have an adverse effect on somatic and psychiatric morbidity. In recent years, the frequency of serious earthquakes has prompted investigators to focus attention on the effects of earthquake on cardiovascular diseases (CVD). Prior research has suggested that earthquake exposure is associated with adverse consequences for CVD. However, the prognostic significance of earthquake‐related loss in heart failure (HF) has not been characterized before.
Therefore, the purpose of this 2‐year follow‐up study after the Sichuan earthquake was to determine the effect of earthquake‐related loss and other potential factors on event‐free survival in patients with HF.
Methods
Patient Population
The study was designed to be a prospective matched cohort observational study involving 2 centers: West China Hospital, Sichuan University, Chengdu; and People's Hospital of Deyang City, Deyang. There are the 2 high‐grade hospitals to which most patients from the earthquake‐affected area were admitted. Patients were included in the study if they met all of the following criteria: (1) first admission following the 2008 earthquake with a principal diagnosis of HF, including chronic heart failure and acute heart failure, with any kind of etiology, such as hypertension, coronary heart disease, valvular heart disease, cardiomyopathy, pulmonary heart disease, congenital heart disease, and other rare diseases that can cause heart failure (ICD‐10 codes I11.0, I13, I50, I42, I97, and J81); (2) signed informed consent; and (3) age >18 years. The research protocol was approved by the research ethics committees of the West China Hospital and People's Hospital of Deyang City.
Patients were excluded if they met any of the following criteria: (1) investigators judged that the patient was unable/unwilling to comply with the study protocol (eg, lack of telephone access), (2) the patient was undergoing any form of psychotherapy before admission, (3) a female patient was pregnant or lactating, and (4) HF was combined with severe, life‐threatening renal, liver, or lung functional impairment, or cancer.
From May 12, 2008 to November 12, 2008, all patients who met the inclusion and exclusion criteria were divided to 2 groups according to whether they suffered earthquake‐related loss, which was defined as any of the following conditions: (1) death of any family member; (2) loss of a house, or more than one‐third of their property; (3) any injury caused by the earthquake that required hospitalization. Members of the group with earthquake‐related loss and the age‐matched (±1) control group without earthquake‐related loss were interviewed by an independent researcher for depression status.
Depression Measure
Depressive symptoms were to be measured with a standardized psychometric scales, the Zung Self‐Rating Depression Scale (SDS), which has 20 items describing depressive symptoms and has been shown to have satisfactory reliability and validity.1, 2 Patients were divided into 3 levels according to their SDS scores. Those with scores <50 were classified as nondepressive, those with scores between 50 and 59 were considered to have mild depression, and those with scores ≥60 were classified as having moderate/severe depression.
Follow‐Up
Patients were contacted monthly by telephone or face‐to‐face interview for 2 years following their first hospital admission by researchers who were blind to all initial medical and psychiatric assessments. The trained researchers identified and validated all causes of readmission and death by using hospital records, interviews with healthcare providers and patients' family members, and death certificates. The outcome variable was event‐free survival. A combined endpoint of mortality or all‐cause admission was used.
Statistical Analysis
Analyses were performed using SPSS software, version 16.0 (SPSS Inc., Chicago, IL), and a P value <0.05 was required for statistical significance. The baseline characteristics among groups were compared using the Student t test for continuous variables and the χ 2 test for categorical variables. Kaplan‐Meier survival analysis with a log‐rank test was used to compare overall survival time with the combined endpoint of mortality or readmission. The association between baseline variables and end events was evaluated by Cox proportional hazards models.
Results
Between May 12, 2008, and November 12, 2008, 202 pairs of patients were identified. November 12, 2010, was the end of follow‐up for the study. As of that date, the follow‐up for 185 of these 202 pairs of patients (91.58%) was complete, with 17 pairs (8.42%) lost from the study due to loss of contact or unwillingness to continue with follow‐up.
The demographic characteristics of the 2 groups are shown in Table 1. As rated by SDS, patients with earthquake‐related loss were significantly more likely to be depressed (P = 0.003) and more likely to be moderately/severely depressed (P = 0.039). A significantly higher use of diuretics, spironolactone, statins, and psychotropic agents was found in patients with earthquake‐related loss.
Table 1.
Baseline Characteristics and Outcome of Events (Mortality and Readmission) Among Patients by Earthquake‐Related Loss Following the Sichuan Earthquake
| Characteristics | Patients With Earthquake‐Related Loss, n (%), n = 185 | Patients Without Earthquake‐Related Loss, n (%), n = 185 | P Value |
|---|---|---|---|
| Demographic | |||
| Female sex | 66 (35.68) | 78 (42.16) | 0.201 |
| Age (y), mean ± SD | 67.54 ± 11.18 | 67.51 ± 11.14 | NS |
| Unmarried | 48 (25.95) | 35 (18.92) | 0.105 |
| Current or ex‐smoker | 82 (44.32) | 71 (38.37) | 0.246 |
| Cardiac | |||
| LVEF <50% | 57 (30.81) | 64 (34.59) | 0.438 |
| MI | 22 (11.89) | 17 (9.19) | 0.397 |
| Interventional or surgical therapya | 25 (13.51) | 31 (16.76) | 0.384 |
| Comorbidities | |||
| Depression (SDS scores ≥50) | |||
| None | 92 (49.73) | 120 (64.86) | 0.003 |
| Mild | 43 (23.24) | 32 (17.30) | 0.155 |
| Moderate/severeb | 50 (27.03) | 33 (17.84) | 0.039 |
| Hypertension | 73 (39.46) | 85 (45.95) | 0.207 |
| DM | 17 (9.19) | 20 (10.81) | 0.603 |
| COPD or asthma | 38 (20.54) | 45 (24.32) | 0.383 |
| Stroke or TIA | 48 (25.95) | 36 (19.46) | 0.258 |
| Renal diseases | 31 (16.76) | 24 (12.97) | 0.306 |
| Medication (at discharge) | |||
| ACEI/ARB | 168 (90.81) | 176 (95.14) | 0.238 |
| Diuretics | 158 (85.41) | 142 (76.76) | 0.034 |
| β‐Blockers | 149 (80.54) | 162 (85.57) | 0.065 |
| Spironolactone | 60 (32.43) | 42 (22.70) | 0.036 |
| Aspirin | 118 (63.78) | 126 (68.11) | 0.380 |
| Statins | 105 (56.76) | 126 (68.11) | 0.024 |
| Psychotropic agents | 39 (21.08) | 15 (8.11) | 0.000 |
| Outcome variable | |||
| Death | 15 (8.11) | 9 (4.86) | 0.205 |
| Cardiac readmissionc | 64 (34.59) | 50 (27.03) | 0.008 |
| All‐cause readmission | 98 (52.97) | 77 (41.62) | 0.029 |
| All events | 114 (61.62) | 86 (46.47) | 0.003 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CABG, coronary artery bypass grafting; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; ICD, implantable cardioverter‐defibrillator; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NS, not significant; PCI, percutaneous coronary intervention; SDS, Zung Self‐Rating Depression Scale; TIA, transient ischemic attack.
Interventional or surgical therapy included radiofrequency ablation, PCI, pacemaker or ICD implantation, valve replacement, CABG, and any interventional or surgical treatment of congenital heart disease.
The moderate and severe depression were combined for purposes of calculation.
Cardiac readmission included readmission because of unstable angina, acute MI, pulmonary edema, thromboembolism, arrhythmia, or CHF.
A total of 24 deaths (6.49%), 114 (30.81%) hospital readmissions due to cardiac reasons, and 175 (47.30%) all‐cause readmissions occurred, and the most subsequent admissions of both groups occurred within the first 12 months after the initial admission. The percentage of patients with cardiac readmission and all‐cause readmission was higher in patients with earthquake‐related loss than in those without earthquake‐related loss (34.59% vs 27.03%, P = 0.008; and 52.97% vs 41.62%, P = 0.029, respectively), but the death rate did not differ between the 2 groups. The total events differed between 2 groups (61.62% vs 46.47%, P = 0.003) (Table 1).
At 2 years' follow‐up, approximately 60% of patients without earthquake‐related loss were event‐free, whereas only 40% of patients with earthquake‐related loss were event‐free (Figure 1). When all patients were divided according to depressive symptoms, HF patients without depressive symptoms experienced longer event‐free survival than did patients with depression (log‐rank test, P = 0.000) (Figure 2). When we compared survival curves between groups with and without earthquake‐related loss stratified by presence or absence of depressive symptoms, patients without loss experienced longer event‐free survival than patients with loss in the condition of absence of depressive symptoms (Figure 3A). But the survival curves did not differ between patients with and without earthquake‐related loss in the condition of presence of depressive symptoms (Figure 3B).
Figure 1.

Kaplan‐Meier survival curves showing cumulative event‐free survival probability of HF patients in a 2‐year follow‐up period after their first admission after earthquake by earthquake‐related loss. The log‐rank statistic differences between the 2 curves was P = 0.002. Abbreviations: HF, heart failure.
Figure 2.
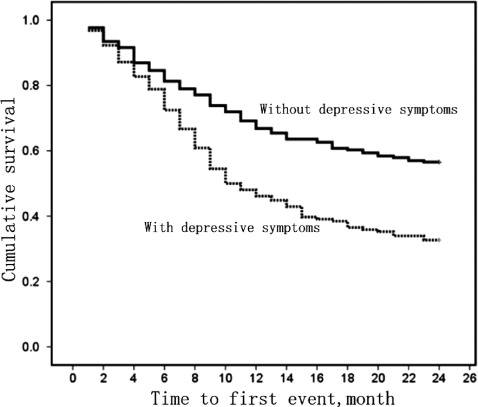
Kaplan‐Meier survival curves showing cumulative event‐free survival probability of HF patients in a 2‐year follow‐up period after their first admission after earthquake by depression. The log‐rank statistic differences between the 2 curves was P = 0.000. Abbreviations: HF, heart failure.
Figure 3.
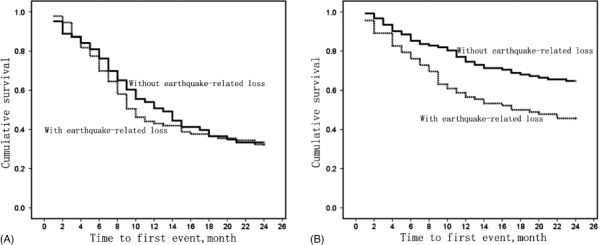
Event‐free survival according to earthquake‐related loss with (A) and without (B) depressive symptoms. The log‐rank statistic differences between the 2 curves were P = 0.003 and P = 0.692, respectively.
In a Cox proportional hazard regression model, earthquake‐related loss, low left ventricular ejection fraction (LVEF), depressive symptoms, and chronic obstructive pulmonary disease (COPD) or asthma remained independent predictors of event‐free survival, showing a significant interaction effect (Table 2).With earthquake‐related loss vs non–earthquake‐related loss, the relative risk (RR) was 1.557 (95% confidence interval [CI]: 1.154–2.102, P = 0.004).With low LVEF (<50%) vs LVEF ≥50%, the RR was 1.909 (95% CI: 1.379–2.643, P = 0.000). With moderate/severe depression vs no depression, the RR was 1.626 (95% CI: 1.150–2.301, P = 0.006); and with COPD or asthma vs no COPD or asthma, the RR was 1.571 (95% CI: 1.121–2.201, P = 0.009). Other baseline variables were not associated with risk of events.
Table 2.
Cox Regression Multivariate Analysis for 2‐Year Outcome Events of Mortality and Readmission Following Earthquake
| 95% CI | ||||
|---|---|---|---|---|
| Characteristics | OR | Lower | Upper | P Value |
| Earthquake‐related loss | 1.557 | 1.154 | 2.102 | 0.004 |
| Female sex | 1.168 | 0.870 | 1.568 | 0.302 |
| Age | 1.007 | .994 | 1.019 | 0.294 |
| Unmarried | 1.343 | .969 | 1.862 | 0.077 |
| Current or ex‐smoker | 0.963 | 0.709 | 1.310 | 0.812 |
| Cardiac | ||||
| LVEF <50% | 1.909 | 1.379 | 2.643 | 0.000 |
| MI | 1.344 | 0.853 | 2.117 | 0.202 |
| Interventional or surgical therapy | 0.809 | 0.512 | 1.277 | 0.363 |
| Comorbidities | ||||
| Depression (SDS scores ≥60) | 1.626 | 1.150 | 2.301 | 0.006 |
| Hypertension | 1.394 | 0.984 | 1.973 | 0.061 |
| DM | 1.142 | 0.679 | 1.920 | 0.617 |
| COPD or asthma | 1.571 | 1.121 | 2.201 | 0.009 |
| Stroke or TIA | 0.701 | 0.476 | 1.033 | 0.073 |
| Renal diseases | 1.031 | 0.636 | 1.671 | 0.901 |
Abbreviations: CI, confidence interval; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; LVEF, left ventricular ejection fraction; MI, myocardial infarction; OR, odds ratio; SDS, Zung Self‐Rating Depression Scale; TIA, transient ischemic attack.
Discussion
The most important finding in our study was that earthquake‐related loss was an independent predictor of outcome events in HF patients. The interaction between earthquake‐related loss and depressive symptoms was not only a combined significant predictor of event‐free survival, but earthquake‐related loss was as independently predictive of event‐free survival as depressive symptoms.
As improvements in rescue techniques and living conditions in the past few decades has reduced the risk of communicable‐disease epidemics following major disasters such as earthquake, more attention has turned to the effect of disasters on patients with chronic diseases, such as CVD and psychological illness. Prior research has suggested that earthquake exposure is associated with adverse consequences for cardiovascular disease. Katsouyanni et al3 reported a 3‐fold increase in cardiac deaths and a 1.6‐fold increase in risk for deaths from all causes after the 1978 earthquake in Thessalonika, Greece. Similar results were reported following the Athens earthquake of 1981, the Armenia earthquake of 1988, the Hanshin‐Awaji earthquake of 1994 in Japan, and the Northridge earthquake of 1994 in Los Angeles.4, 5, 6, 7 Nakagawa et al8 reported the increased long‐term mortality from acute myocardial infarction after the Niigata‐Chuetsu earthquake of October 2004 in Japan. Trevisan et al9 reported higher heart rate and serum cholesterol and triglyceride levels within the first few weeks after the earthquake following the 1980 earthquake in Naples, Italy. However, most of these studies referred to total cardiovascular disease risk based on comparison between before and after the earthquake. Only a few studies, such as that Armenian et al,4 revealed that people with increasing levels of loss of material possessions and family members had significant increases in heart disease risk after the 1988 earthquake in Armenia. But the natural history and prognostic significance of HF related to earthquake‐related loss have not been adequately characterized before. To our knowledge, this is the first longitudinal follow‐up study carried out to link personal risk of earthquake‐related loss to cardiac events, and it will help to improve the investigation of the complex relations among factors related to survival following earthquakes.
In baseline characteristics of this study, there is a slightly higher level of total depression morbidity (42.7%) among HF patients, especially among patients suffering from earthquake‐related loss (50.27%), compared with previous studies (20%–45%) concerning depression among HF patients.10, 11, 12, 13, 14 The possible interpretation is post‐traumatic stress disorder (PTSD) following the earthquake, which led to a high morbidity of depression. In fact, it has been found that 44.5% of people experiencing a traumatic event would have a diagnosis of depression. At the same time, the relatively higher morbidity of moderate/severe depression among HF patients with earthquake‐related loss than among their counterparts (27.03% vs 17.84%, P = 0.039) may also be caused by more serious somatic and psychiatric trauma in earthquake and the following PTSD. The higher proportion of diuretic, spironolactone, statin, and psychotropic agent use found in patients with earthquake‐related loss may reflect the difficulty of disease control.
In our study, patients without earthquake‐related loss experienced longer event‐free survival than their counterparts, which has not been reported before. This gap could not be narrowed by higher use of diuretics, spironolactone, statins, and psychotropic agents. One of the possible assumptions is that the higher morbidity of depression among patients with earthquake‐related loss causes the higher rate of death or readmission events. But the Kaplan‐Meier analysis also showed that time to first event was longer among nondepressive patients without earthquake‐related loss than among nondepressive patients with loss, which indicated that the effect of earthquake‐related loss is independent of depression (Figure 2 and Figure 3A). However, the time to first event did not differ among depressive patients with and without loss (Figure 3B). The possible interpretation may be that the relatively weak effect of earthquake‐related loss on the course of HF was diluted by depression.
In the multivariate Cox regression analysis, earthquake‐related loss, low LVEF, depressive symptoms, and COPD or asthma showed an independent predictive value for events in HF patients. As defined previously, the severe loss during earthquake may imply the weakening of social support, deterioration of financial situation, change of living environment, a huge psychological or physical trauma, and so on. All of these factors may worsen the prognosis of HF alone or allied directly or indirectly by means of more frequent attacks of hypertension, acute coronary syndrome, arrhythmia, and others. A higher depression score, low LVEF, and COPD or asthma comorbidity were associated with a higher rate of events during the 2 years of follow‐up. This could be attributable to several factors. First, patients with low LVEF may represent those with poor cardiac function, a tendency for fluid retention, and those for whom it is difficult to adapt to change or comply with medical advice. The second factor may be some direct effect of depressive symptoms on the cardiovascular system, mediated by endogenous neurohormonal activation, endothelium dysfunction, decreased heart rate variability, poor compliance, or other unknown mechanisms.15, 16, 17 Third, the COPD or asthma patients with impaired lung function and immunity were more susceptible to respiratory‐tract infection, and more prone to generate high pulmonary artery pressure.
Some limitations of our study should be noted. Our study design is nonrandomized, and determining which component behind the earthquake‐related loss affects the prognosis of HF patients requires further study. Also, the population we studied is limited to hospitalized patients.
Several implications of our findings may be useful: (1) following a great natural or social disaster, healthcare providers should assess HF patients' disaster‐related loss and mental status to identify patients at higher risk of poor outcomes; (2) social, financial, and medical interventions need to be developed that address the specific needs of HF patients with disaster‐related loss; and (3) interventions to improve depressive symptoms, including pharmacotherapy and nonpharmacological interventions (eg, cognitive behavioral therapy), can especially lead to an improvement the prognosis of patients with depressive symptoms.
Conclusion
This study demonstrated the effect of earthquake‐related loss in the context of depressive symptoms on readmission and mortality among HF patients. We found that severe loss in an earthquake is a predictor of poor outcomes in HF patients, which is independent of depression. This finding contributes to understanding the role of earthquake‐related loss in affecting outcomes in HF. Heart failure patients sustaining a disaster‐related loss should be closely monitored to improve their prognosis.
Acknowledgements
Professor Debarati Guha‐Sapir, Department of Public Health, Louvain School of Medicine, University of Louvain, Brussels, also contributed to this paper.
References
- 1. Dimos AK, Stougiannos PN, Kakkavas AT, et al. Depression and heart failure. Hellenic J Cardiol. 2009;50:410–417. [PubMed] [Google Scholar]
- 2. Zung WW. Zung Self‐Rating Depression Scale and Depression Status Inventory In: Satorius N, Ban TA, eds. Assessment of Depression. New York, NY: Springer‐Verlag; 1986:221–231. [Google Scholar]
- 3. Katsouyanni K, Kogevinas M, Trichopoulos D. Earthquake‐related stress and cardiac mortality. Int J Epidemiol. 1986;15:326–330. [DOI] [PubMed] [Google Scholar]
- 4. Armenian HK, Melkonian AK, Hovanesian AP. Long term mortality and morbidity related to degree of damage following the 1998 earthquake in Armenia. Am J Epidemiol. 1998;148: 1077–1084. [DOI] [PubMed] [Google Scholar]
- 5. Kloner RA, Leor J, Poole WK. Population‐based analysis of the effect of the Northridge Earthquake on cardiac death in Los Angeles County, California. J Am Coll Cardiol. 1997;30: 1174–1180. [DOI] [PubMed] [Google Scholar]
- 6. Kario K, Ohashi T. Increased coronary heart disease mortality after the Hanshin‐Awaji earthquake among the older community on Awaji Island. Tsuna Medical Association. J Am Geriatr Soc. 1997;45:610–613. [DOI] [PubMed] [Google Scholar]
- 7. Trichopoulos D, Katsouyanni K, Zavitsanos X. Psychological stress and fatal heart attack: the Athens (1981) earthquake natural experiment. Lancet. 1983;1:441–444. [DOI] [PubMed] [Google Scholar]
- 8. Nakagawa I, Nakamura K, Oyama M. Long‐term effects of the Niigata‐Chuetsu earthquake in Japan on acute myocardial infarction mortality: an analysis of death certificate data. Heart. 2009;95:2009–2013. [DOI] [PubMed] [Google Scholar]
- 9. Trevisan M, Celentano E, Meucci C. Short‐term effect of natural disasters on coronary heart disease risk factors. Arteriosclerosis. 1986;6:491–494. [DOI] [PubMed] [Google Scholar]
- 10. Jiang W, Alexander J, Christopher E. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. [DOI] [PubMed] [Google Scholar]
- 11. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure: a meta‐analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. [DOI] [PubMed] [Google Scholar]
- 12. Freedland KE, Rich MW, Skala JA, et al. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med. 2003;65:119–128. [DOI] [PubMed] [Google Scholar]
- 13. Friedmann E, Thomas SA, Liu F, et al. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152:940.e1–940.e8. [DOI] [PubMed] [Google Scholar]
- 14. De Leon CF, Grady KL, Eaton C, et al. Quality of life in a diverse population of patients with heart failure: baseline findings from the Heart Failure Adherence and Retention trial (HART). J Cardiopulm Rehabil Prev. 2009;29:171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hata S. Cardiovascular disease caused by earthquake‐induced stress: psychological stress and cardiovascular disease. Circ J. 2009;73:1195–1196. [DOI] [PubMed] [Google Scholar]
- 16. Muller JE, Abela GS, Nesto RW, et al. Triggers, acute risk factors and vulnerable plaques: the lexicon of a new frontier. J Am Coll Cardiol. 1994;23:809–813. [DOI] [PubMed] [Google Scholar]
- 17. Silver MA. Depression and heart failure: an overview of what we know and don't know. Cleve Clin J Med. 2010;77(suppl 3):S7–S11. [DOI] [PubMed] [Google Scholar]


