Abstract
Background:
Congestive heart failure (CHF) has become a major clinical and public health challenge with the aging of the population in China. However, the effect of the coexistence of multiple cardiovascular diseases on the prognosis of hospitalized patients with CHF remains unclear. A comparative analysis was performed to explore the etiology and comorbidities of CHF and in‐hospital mortality in patients with CHF.
Hypothesis:
The coexistence of multiple cardiovascular diseases is an independent predictor of the 30‐day mortality of hospitalized patients with CHF.
Methods:
All 6949 patients (4344 males, 2605 females) in the database with a principal ICD‐9‐CM discharge diagnosis of CHF were identified and divided into 5 groups according to the number of comorbidities. Cox proportional hazards regression was used to examine the association between the number of comorbidities and in‐hospital mortality in patients with CHF.
Results:
A single comorbidity was predominant in younger patients (18–39 years, P<0.001), whereas multiple comorbidities were predominant in the elderly (≥80 years, P<0.001). The most common single etiology was valvular heart disease, and the most common triple etiology was hypertension and diabetes mellitus complicated by coronary artery disease. Cox regression analysis showed a higher hospital mortality rate associated with an increased number of comorbidities (hazard ratio [HR] from 1.22 [95% CI: 0.89–1.68] to HR 3.49 [95% CI: 2.55–4.78], P<0.001).
Conclusions:
This study demonstrates the coexistence of multiple cardiovascular diseases is an independent predictor of the 30‐day mortality of hospitalized patients with CHF. © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Congestive heart failure (CHF) has become a major clinical and public health challenge with the aging of the population in China and the rest of the world.1 Although modern treatment has improved dramatically, the prognosis is still poor and primary prevention is important. The incidence, prognosis, risk factors and clinical backgrounds of patients with CHF have been well described by a number of population‐based2, 3 and hospital‐based studies4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 in the United States and worldwide. However, these prior studies have generally focused on individual cardiovascular disease risk factors, and the effect of the coexistence of multiple cardiovascular diseases on the prognosis of hospitalized patients with CHF has not been clearly demonstrated.
Recently, the Atherosclerosis Risk in Communities (ARIC) study summed the number of risk factors to create the 4‐factor scores (blood pressure, plasma cholesterol, diabetes, and smoking) and 5‐factor scores (including body mass), which suggested that the incidence of heart failure is largely explained (77% or more) by traditional coronary heart disease (CHD) risk factors.19 Furthermore, recent evidence suggests substantial differences in the epidemiology of the incidence of CHF and its progression among sex‐ and race‐based subgroups.17, 18 Understanding these differences is imperative for planning appropriate preventive and therapeutic interventions based on the population and healthcare system in China. The aim of the present study, therefore, was to investigate the effect of the number of simultaneous cardiovascular diseases and comorbidities on the 30‐day mortality of hospitalized patients with CHF.
Methods
We reviewed data from all patients age 18 years or older admitted to the Chinese People's Liberation Army (PLA) General Hospital in Beijing, from January 1, 1993 to December 31, 2007 using the hospital administrative database. Patients for the study were identified by screening the database for International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM)20 principal discharge diagnoses of CHF (ICD‐9‐CM codes 428). All 6949 patients (4344 males, 2605 females) in the database with a principal ICD‐9‐CM discharge diagnosis of CHF were identified. Fifteen comorbidity variables (coronary artery disease, hypertension, diabetes mellitus, cor pulmonale, cardiomyopathy, valvular disease, congenital heart disease, anemia, atrial fibrillation, myocardial infarction, pneumonia, gastrointestinal bleeding, cerebrovascular disease, renal failure, and liver cirrhosis) were identified using an ICD‐9‐CM discharge diagnosis coding scheme. Renal failure was defined as an estimated glomerular filtration rate (eGFR) ≤60 mL/min−1/1.73 m−2, recalibrated for Chinese individuals,21 to estimate the glomerular filtration rate (eGFR) in mL/ min−11.73 m−2: eGFR = 186× [SCR × 0.011] −1.154 × [age] −0.203 × [0.742 if female] × 1.233. All comorbidities showing a significant univariate relationship with 30‐day mortality of the patient with CHF at follow‐up were included in a logistic regression model. Model reduction was performed by stepwise regression excluding variables from the model with a P value <0.10. All variables that were independently associated with 30‐day mortality of the patient with CHF were tested for interactions. The patients were divided into 5 groups based on the number of etiologies and comorbidities: group 1, one comorbidity; group 2, two comorbidities; group 3, three comorbidities; group 4, four comorbidities; and group 5, five or more comorbidities. A comparative analysis was performed to explore the etiology of CHF, comorbidities, and 30‐day mortalities of hospitalized patients in each group.
Statistical Analysis
Categorical variables are presented as percentages. The duration of in‐hospital stay and other continuous variables are expressed as mean ± standard deviation. Categorical variables were compared using the χ 2 test, and the continuous variables were compared among the 5 groups using 1‐way analysis of variance followed by the post hoc Bonferroni multiple comparisons test. The cumulative survival probabilities were estimated using the method of Kaplan‐Meier and Cox proportional hazards models. The raw and adjusted hazard ratios (HRs) and corresponding confidence intervals (CIs) were obtained using Cox proportional hazards regression models. All statistical tests were performed using SPSS 16.0 for Windows (SPSS Inc., Chicago, IL).
Results
Etiology of CHF
The baseline demographics of patients in the different groups are given in the Table 1. The etiology of hospitalization for patients with CHF were coronary artery disease (45.0%), hypertension (38.7%), valvular heart disease (27.5%), and diabetes mellitus (18.3%) (Figure 1). Table 1 also illustrates the etiology of hospitalization for patients in different groups. The most common etiology was valvular disease (34.3%) in group 1 (1 comorbidity). However, in group 5 (5 or more comorbidities), the most common etiologies were coronary artery disease (87.9%), hypertension (78.4%), and diabetes mellitus(66.3%).
Table 1.
Baseline Demographics, Etiology, and Comorbidities of Patients With CHF at Different Groups
| Group 1, n = 2215 | Group 2, n = 2512 | Group 3, n = 1436 | Group 4, n = 587 | Group 5, n = 199 | P Value | |
|---|---|---|---|---|---|---|
| Sex (%, M/F) | 63/37 | 62/38 | 64/36 | 61/39 | 63/37 | 0.501 |
| Age (y, mean [SD]) | 55 [17] | 59 [16] | 66 [14] | 67 [13] | 69 [12] | <0.001 |
| Length of stay (d, mean [SD]) | 23 [15] | 23 [15] | 24 [17] | 26 [18] | 26 [20] | <0.001 |
| Etiology (%) | ||||||
| Coronary artery disease | 20.0 | 42.3 | 67.2 | 81.8 | 87.9 | <0.001 |
| Hypertension | 10.8 | 37.4 | 65.5 | 70.4 | 78.4 | <0.001 |
| Diabetes mellitus | 2.3 | 12.3 | 34.5 | 48.9 | 66.3 | <0.001 |
| Cor pulmonale | 9.7 | 8.6 | 11.1 | 8.3 | 14.6 | <0.001 |
| Cardiomyopathya | 9.5 | 7.7 | 5.5 | 3.9 | 5.0 | <0.001 |
| Valvular disease | 34.3 | 30.1 | 17.5 | 18.6 | 18.6 | <0.001 |
| Congenital heart diseaseb | 1.7 | 5.9 | 2.1 | 0.9 | 0.5 | <0.001 |
| Comorbidities (%) | ||||||
| Atrial fibrillation | 4.3 | 29.9 | 30.0 | 41.1 | 45.7 | <0.001 |
| Myocardial infarction | 0.0 | 7.0 | 24.6 | 43.4 | 54.8 | <0.001 |
| Pneumonia | 3.0 | 7.6 | 18.0 | 30.8 | 55.3 | <0.001 |
| Anemia | 0.6 | 2.1 | 5.0 | 10.1 | 23.1 | <0.001 |
| Cerebrovascular disease | 0.3 | 1.9 | 4.5 | 12.1 | 18.1 | <0.001 |
| Gastrointestinal bleeding | 0.5 | 0.6 | 1.1 | 3.4 | 7.5 | <0.001 |
| Renal failure | 1.3 | 4.7 | 10.6 | 21.3 | 35.7 | <0.001 |
| Cirrhosis of liver | 0.5 | 2.0 | 2.8 | 5.1 | 5.5 | <0.001 |
Abbreviations: F, female; M, male; SD, standard deviation.
Excludes cardiomyopathy complicating: pregnancy, puerperium, and ischemic cardiomyopathy.
Congenital malformation of cardiac septa: including atrial septal defect, ventricular septal defect, and tetralogy of Fallot.
Figure 1.
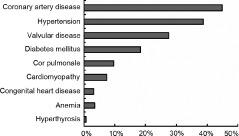
Etiology of congestive heart failure in patients hospitalized.
Precipitating Factors and Comorbidities
The patients' precipitating factors and comorbidities are reported in the Table 1. Atrial fibrillation was the most prevalent precipitating factor for CHF hospitalization, which was present in 23.3% of total cases, with 4.3% in group 1, and 45.7% in group 5 (P<0.001). In the majority of these cases, atrial fibrillation was either long‐standing (present on electrocardiograms recorded months to years before the onset of heart failure) or associated with other cardiac pathologies (eg, myocardial infarction, valvular heart disease, or dilated cardiomyopathy). Myocardial infarction was equally prevalent as a precipitating factor in CHF patients. However, in group 5 only patients over the age of 32 years were present, and pneumonia (55.3%) was the predominant precipitating factor. Renal failure was extremely prevalent in patients in groups 4 and 5 (21.3% group 4, 35.7% group 5). We found that the number of comorbidities rose very steeply with age. A single comorbidity was predominant in younger patients (18–39 years, 53.5%; ≥80 years, 18.8%). However, in group 5, five or more comorbidities were predominant (18–39 years, 0.3%; ≥80 years, 5.6%) (Figure 2).
Figure 2.
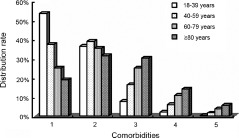
Distribution of comorbidity number among hospitalized patients with congestive heart failure by age.
In‐Hospital Mortality
The survival of hospitalized patients with CHF was poor. Figure 3 shows the change in 30‐day mortality among those hospitalized either by age or by the number of comorbidities. In‐hospital mortality was 5.4%. The in‐hospital mortality was almost twice as high (3.2% vs 1.8% or 16.1% vs 11.4%, P = 0.148 or P = 0.086, respectively) for women than for men at an age range of 18 to 39 years or ≥80 years. Overall, as the age and the number of comorbidities increased, in‐hospital mortality also increased for both men and women. Cox regression analysis showed higher hospital mortality associated with an increased number of etiologies and comorbidities. HRs were as follows: group 2 vs group 1, HR: 1.22 (95% CI: 0.89–1.68, P = 0.218); group 3, HR: 1.62 (95% CI: 1.25–2.09, P<0.001); group 4, HR: 2.2 (95% CI: 1.65–2.83, P<0.001); and group 5, HR: 3.49 (95% CI: 2.55–4.78, P<0.001). The hazard of death increased with the number of comorbidities (Figures 3 and 4).
Figure 3.
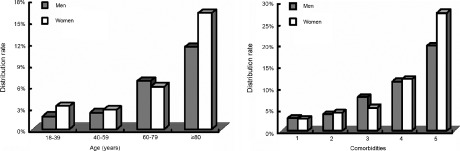
Age and comorbidity distribution of 30‐day mortality.
Figure 4.
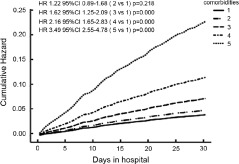
In‐hospital mortality curves according to comorbidities by Cox regression analysis. Abbreviations: CI, confidence interval; HR, hazard ratio.
Discussion
This study has a number of important strengths. Not only does it describe the etiology of heart failure over the last 15 years, but it also describes the precipitating factors and comorbidities in patients primarily hospitalized for CHF based on their admission history. Furthermore, to the best of our knowledge our study is the first detailed analysis of the effect of the coexistence of multiple cardiovascular diseases on the prognosis of hospitalized patients with CHF, and this is the largest study of the etiology and prognosis of CHF in China. Finally, we also describe the change in 30‐day mortality among hospitalized patients with CHF based on age or the number of comorbidities.
Etiology of CHF
A number of prior population‐based2, 3 and hospital‐based studies6, 7, 8, 9 have shown that coronary artery disease has become the single most important cause of CHF in Western populations and other Asian populations.10, 11 More than 45% of the CHF cases in our study population were attributed to coronary artery disease, which is very close to that found in the Epidémiologie de l'Insuffisance Cardiaque Avancée en Lorraine (EPICAL) study (46.3% attributed to coronary artery disease).4 In the Acute Decompensated Heart Failure National Registry (ADHERE) study, CHD was the underlying cause of CHF in 57% of patients.5 Our study also found that hypertension and diabetes are common causes of heart failure (about 38.7% and 18.3%, respectively), but are much lower than the corresponding findings in Western populations (about 60%–70% and 22%–44%, respectively).5, 12 However, the single most common etiology was valvular disease (group 1). Valvular disease was 27.5% in the etiology of hospitalization for patients with CHF, including rheumatic (21.8%) and nonrheumatic valvular disease (5.7%). Rheumatic valvular disease in China was much higher than the prevalence in Western populations (7%–11%).12, 13 Among the 1500 cases of rheumatic valvular disease, 1364 (90.9%) patients had mitral valve diseases and 659 (43.9%) had aortic valve diseases. Multivariate analysis of results from a population‐based study has shown that rheumatic valvular heart disease is 1 of risk factors for development of atrial fibrillation in developing countries.14 Other Chinese investigations found that the causes of CHF had shifted from rheumatic valvular disease to coronary heart disease during the past 2 decades. Rheumatic valvular disease had fallen from 46.8% to 8.9% (an average of 28%, which is similar to the present study), whereas coronary heart disease had increased from 31.1% to 55.7%.15, 16 Anemia and cor pulmonale also occurred at a much higher prevalence than in Western populations. Differences between developed and developing countries and racial variation may explain these results.
Precipitating Factors and Comorbidities
The most common precipitating factor was atrial fibrillation (AF). AF has previously been reported to occur at a high frequency in CHF patients (about 33%–40%),6, 7, 8 but we found AF in 23.3% of total cases, which is relatively lower than that in Western populations. However, the prevalence of AF increasing with age is consistent with Western populations and similar to the results of another study in China.17 In addition, we found that the prevalence of AF increased with the number of comorbidities. AF may promote heart failure especially when the ventricular rate is uncontrolled, but CHF may also promote atrial fibrillation. Eventually, between AF and CHF could constitute a vicious cycle. Pneumonia (55.3%, group 5) was the predominantly precipitating factor. It is commonly recognized that elderly patients with pneumonia often develop CHF, particularly when confined to a bed. Identification of the precipitating factors of CHF is very important, because an episode of CHF can often be terminated by treating a specific precipitating factor. Persons with CHF often have multiple cardiovascular risk factors.17 Renal failure was the most frequent coexisting comorbidity in this study. In a meta‐analysis of 16 studies, Smith et al found that 63% of 80 098 patients with CHF had some degree of concomitant impaired renal function, and 29% presented with severe renal failure.22 Worsening renal function during the treatment of CHF is sometimes referred to as cardiorenal syndrome. Furthermore, worsening renal function is strongly independent of general mortality in patients with CHF.23, 24
In‐Hospital Mortality
Despite major advances in the treatment of CHF, morbidity and mortality remain high.4, 6, 9 In‐hospital mortality was about 8% to 10%.10, 13 In the present study, in‐hospital 30‐day mortality was 5.4%. It is difficult to precisely compare our findings with the Western studies, as those studies did not address the same span of years and did not include the age range of the entire population. However, in contrast to Western countries, the proportion of the patients with rheumatic valvular disease in China is higher than in Western countries, and the incidence of rheumatic valvular disease among women is significantly higher than among men (33.4% vs 14.5%, P<0.001). The in‐hospital mortality was lower in patients with rheumatic valvular disease than without (2.5% vs 6.1%, P<0.001) in this study.
Limitations
The study was conducted at a single teaching hospital, and the proportions in the study patients do not reflect hospitalized patients in general. First, the Chinese PLA General Hospital is 1 of the largest general hospitals in China, with 4000 beds. For these reasons, the results of this study may not be generalizable to all CHF populations in China. Second, the diagnosis of CHF in our study was based on CHF hospitalization. Therefore, we likely underestimated the true incidence of CHF. These may affect the development and outcomes of CHF. Third, in all retrospective studies, bias is inevitable.
Conclusion
The present study indicated that in‐hospital mortality increased with the age and the number of comorbidities for both men and women. Our findings further highlight that the coexistence of multiple cardiovascular diseases is an independent predictor of 30‐day mortality in hospitalized patients with CHF.
References
- 1. Zhang ZB, Cheng TO, Zhang YC. Introduction. In Textbook of CongestiveHeart Failure, p.15. Beijing, China: Science & Technology Publishers, 2003. [Google Scholar]
- 2. Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community‐based population. JAMA. 2004;292:344–350. [DOI] [PubMed] [Google Scholar]
- 3. Goldberg RJ, Spencer FA, Former C, et al. Incidence and hospital death rate associated with heart failure: a community‐wide perspective. Am J Med. 2005;118:728–734. [DOI] [PubMed] [Google Scholar]
- 4. Zannad F, Briancon S, Juilliere Y, et al. Incidence, clinical and etiologic features, and outcomes of advanced chronic heart failure: the EPICAL Study. Epidémiologie de l'Insuffisance Cardiaque Avancée en Lorraine. J Am Coll Cardiol. 1999;33:734–742. [DOI] [PubMed] [Google Scholar]
- 5. Adams KF Jr, Fonarow GC, Emerman CL, et al. ADHERE Scientific Advisory Committee and Investigators . Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the acute decompensated heart failure national registry (ADHERE). Am Heart J. 2005;149:209–216. [DOI] [PubMed] [Google Scholar]
- 6. Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27: 2725–2736. [DOI] [PubMed] [Google Scholar]
- 7. Rudiger A, Harjola VP, Muller A, et al. Acute heart failure: clinical presentation, one‐year mortality and prognostic factors. Eur J Heart Fail. 2005;7:662–670. [DOI] [PubMed] [Google Scholar]
- 8. Cleland JG, Swedberg K, Follath F, et al. The EuroHeart failure survey programme—a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J. 2003;24:442–463. [DOI] [PubMed] [Google Scholar]
- 9. Lee D, Austin PC, Rouleau JL, et al. Predicting mortality among patients hospitalised for heart failure. JAMA. 2003;290:2581–2587. [DOI] [PubMed] [Google Scholar]
- 10. Goda A, Yamashita T, Suzuki S, et al. Prevalence and prognosis of patients with heart failure in Tokyo: a prospective cohort of Shinken Database 2004‐5. Int Heart J. 2009;50:609–625. [DOI] [PubMed] [Google Scholar]
- 11. Tsuchihashi M, Tsutsui H, Kodama K, et al. Clinical characteristics and prognosis of hospitalized patients with congestive heart failure—a study in Fukuoka, Japan. Jpn Circ J. 2000; 64:953–959. [DOI] [PubMed] [Google Scholar]
- 12. Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5:167–173. [DOI] [PubMed] [Google Scholar]
- 13. Sarmento PM, Fonseca C, Marques F, et al. Acutely decompensated heart failure: characteristics of hospitalized patients and opportunities to improve their care. Rev Port Cardiol. 2006;25:13–27. [PubMed] [Google Scholar]
- 14. Vora A. Management of atrial fibrillation in rheumatic valvular heart disease. Curr Opin Cardiol. 2006;21:47–50. [DOI] [PubMed] [Google Scholar]
- 15. Cao YM, Hu DY, Wu Y, et al. A pilot survey of the main causes of chronic heart failure in patients treated in primary hospitals in China. Chin J Intern Med. 2005;44:487–489. [PubMed] [Google Scholar]
- 16. Shanghai Investigation Group of Heart Failure . The evolving trends in the epidemiologic factors and treatment of hospitalized patients with congestive heart failure in Shanghai during the years of 1980, 1990 and 2000. Chin J Cardiol. 2002;30:24–26. [Google Scholar]
- 17. Yang JF, Liu B, Liu DG, et al. Prevalence and risk factors of atrial fibrillation in preterminal inpatients aged 60 years and over. Chin Med J. 2008;121:2046–2049. [PubMed] [Google Scholar]
- 18. East MA, Peterson ED, Shaw LK, et al. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148:151–156. [DOI] [PubMed] [Google Scholar]
- 19. Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, et al. Epidemiology of incident heart failure in a contemporary elderly cohort. The Health, Aging, and Body Composition Study. Arch Intern Med. 2009;169:708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. International Classification of Diseases, Ninth Revision, Clinical Modification. Washington, D.C.: Public Health Service, U.S. Dept of Health and Human Services; 1988. [Google Scholar]
- 21. Folsom AR, Yamagishi K, Hozawa A, et al. Absolute and attributable risks of heart failure incidence in relation to optimal risk factors. Circ Heart Fail. 2009;2:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure. J Am Coll Cardiol. 2006;47:1987–1996. [DOI] [PubMed] [Google Scholar]
- 23. Tang WH, Mullens W. Cardiorenal syndrome in decompensated heart failure. Heart. 2010;96:255–260. [DOI] [PubMed] [Google Scholar]
- 24. Zeeuw AC, Hampton JR, Dirk J, et al. Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation. 2000;102:203–210. [DOI] [PubMed] [Google Scholar]


