Abstract
Background:
According to the American College of Cardiology/American Heart Association/European Society of Cardiology guidelines, the choice of aspirin or warfarin to prevent thromboembolic events (TEs) in patients with nonrheumatic atrial fibrillation (AF) should be based on the CHADS2 score. The purpose of this study was to determine the predictors of warfarin use in patients with AF at low (CHADS2 =0) or intermediate (CHADS2 =1) risk for TEs.
Hypothesis:
Warfarin use is low in intermediate‐ and low‐risk patients.
Methods:
Clinical characteristics of 3086 consecutive patients (mean age, 70 ± 13 years) with nonrheumatic AF from an academic multispecialty practice were determined between 2006 and 2008 through individual chart review. Patients were identified based on an inpatient or outpatient encounter, in which a billing diagnosis code of AF or atrial flutter (AFl) was recorded. The decision for anticoagulation was at the discretion of the primary care physician or cardiologist. No intervention to guide anticoagulant therapy was made.
Results:
Warfarin was prescribed in 180/497 low‐risk patients (36%), and in 646/938 intermediate‐risk patients (69%). Among high‐risk patients (CHADS2 ≥2), warfarin was used in 792/968 patients (82%) with a CHADS2 = 2, in 343/410 patients (84%) with a CHADS2 =3, and in 225/273 patients (82%) with a CHADS2 ≥4. On multivariate analysis, independent predictors of warfarin use in low‐risk patients were nonparoxysmal AF (odds ratio [OR]: 5.02, P<0.0001) and age between 65 and 74 years (OR: 2.21, P<0.0001). Among intermediate‐risk patients, congestive heart failure (OR: 7.34, P<0.0001), nonparoxysmal AF (OR: 4.04, P<0.0001), coronary artery disease (OR: 2.53, P<0.0001), age between 65 and 74 years (OR: 1.68, P = 0.002), and female gender (OR: 1.69, P = 0.002) were independent predictors of warfarin use. Lack of warfarin use (OR: 4.9, P<0.001) and female gender (OR: 2.0, P = 0.03) were associated with a higher risk of TEs in intermediate‐risk patients. None of the CHADS2 parameters was predictive of TEs. Warfarin was not associated with reduction in TEs in low‐risk patients. Warfarin use did not have a significant effect on bleeding.
Conclusions:
Although either aspirin or warfarin is recommended to prevent TEs in patients with AF at intermediate risk for TEs, warfarin is preferred in the majority of patients in general practice. Lack of warfarin use is associated with a higher risk of TEs in intermediate‐risk patients with AF. The adoption of new oral anticoagulants that have lower risk of major hemorrhage than warfarin for low‐ or intermediate‐risk AF patients remains to be determined. © 2011 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Atrial fibrillation (AF) is associated with a risk of thromboembolic events (TEs) and is a major cause of stroke.1 Randomized controlled trials have demonstrated that warfarin significantly reduces the risk of TEs in high‐risk patients2, 3, 4 but increases the risk of major bleeding.5 The American College of Cardiology/American Heart Association/European Society of Cardiology (ACC/AHA/ESC) guidelines on the management of AF recommend treatment with aspirin or warfarin based on the CHADS2 risk scoring system.1 Aspirin is recommended for patients with a CHADS2 score of 0, and warfarin is recommended for high‐risk patients with CHADS2 ≥2. Patients with a CHADS2 score of 1 may be treated with either aspirin or warfarin. The purpose of this study was to determine patterns and predictors of warfarin use in low‐ and intermediate‐risk patients with AF and their association with major thromboembolic and bleeding events. We hypothesize that warfarin use is low in intermediate‐ and low‐risk patients.
Methods
Study Subjects
The subjects of this study were 3086 consecutive patients identified from clinical encounters from July 1, 2006 through December 31, 2008 from the University of Michigan Health System's electronic medical records. Patients were selected based on an inpatient or outpatient encounter in which a billing diagnosis code of AF or atrial flutter (AFl) was recorded (ICD‐9‐CM 427.31 or 427.32). Patients were also included in the study if they were followed in a dedicated anticoagulation clinic for a diagnosis of AF or AFl. Patients were excluded for rheumatic heart disease or complex congenital heart disease, another indication for anticoagulant therapy such as mechanical valves or venous thromboembolic disease, or cardiac transplantation or left ventricular assist device implantation. Warfarin use among patients who had undergone a catheter ablation procedure for AF was censored for the 3 months following the procedure. Clinical characteristics of the patients are shown in Table 1.
Table 1.
Clinical Characteristics
| On Warfarin (%) | No Warfarin (%) | |
|---|---|---|
| Age, mean, years | 71.61 ± 11.97 | 65.86 ± 14.37 |
| Male | 1352/1947 (69.4) | 595/1947 (30.6) |
| Female | 837/1139 (73.5) | 302/1139 (26.5) |
| History of TEs | 387/451 (85.8) | 64/451 (14.2) |
| Hypertension | 1560/2032 (76.8) | 472/2032 (23.2) |
| Diabetes mellitus | 524/647 (81.0) | 123/647 (19.0) |
| Congestive heart failure | 272/311 (87.5) | 39/311 (12.5) |
| Age ≥75 years | 998/1253 (79.6) | 255/1253 (20.4) |
| Age 65–74, years | 613/832 (73.7) | 219/832 (26.3) |
| Coronary artery disease | 603/728 (82.8) | 125/728 (17.2) |
| CHADS2 = 0 | 180/497 (36.2) | 317/497 (63.8) |
| CHADS2 = 1 | 648/938 (69.1) | 290/938 (30.9) |
| CHADS2 = 2 | 792/968 (81.8) | 176/968 (18.2) |
| CHADS2 = 3 | 344/410 (83.9) | 66/410 (16.1) |
| CHADS2 ≥4 | 225/273 (82.4) | 48/273 (17.6) |
Abbreviations: TEs, thromboembolic events.
Data Collection and Analysis
This study protocol was approved by the University of Michigan Institutional Review Board. Data on clinical characteristics and comorbidities were collected through individual chart reviews using electronic medical records. CHADS2 score was determined as described previously: 1 point each for congestive heart failure (CHF), hypertension, diabetes mellitus, or age ≥75 years, and 2 points for a history of transient ischemic attacks (TIA) or stroke (CVA).6 In addition, as described in the ACC/AHA/ESC guidelines, minor risk factors including coronary artery disease (CAD), female gender, and age 65 to 74 years were noted for each patient.1 Adverse events were reported by physicians and collected from individual chart review. All TEs, primarily CVA or TIA, and any bleeding event such as gastrointestinal, intracranial bleeding, or other minor bleeding were noted. Self‐terminating episodes of AF within 7 days were considered paroxysmal, whereas all other types were categorized as nonparoxysmal AF.1
Statistical Analysis
Data are shown as mean ± standard deviation. Continuous variables were compared using the Student t test, and categorical variables were compared with the χ 2 test. Statistical analyses were performed using SPSS for Windows statistical software version 17.0 (SPSS Inc., Chicago, IL). Multivariate logistic regression analysis was performed to identify predictors of warfarin use. Both forward and backward likelihood ratio methods were used to evaluate agreement between the models. P<0.05 was considered statistically significant.
Results
CHADS2 Score and Warfarin Use
Warfarin was prescribed in 180/497 patients (36%) with a CHADS2 score of 0, and 646/938 patients (69%) with a CHADS2 score of 1. Among high‐risk patients, 792/968 (82%) with a CHADS2 score of 2, 343/410 (84%) with a CHADS2 score of 3, and 225/273 patients (82%) with a CHADS2 score ≥4 were receiving warfarin (Figure 1).
Figure 1.
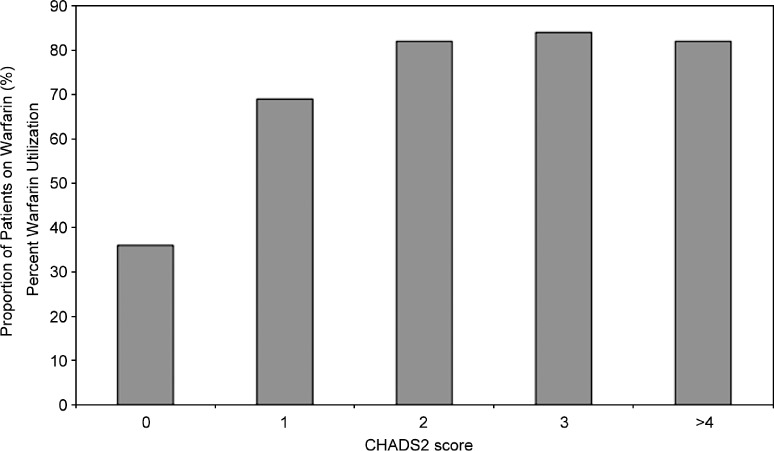
Proportion of patients on warfarin based on the CHADS2 score.
Predictors of Warfarin Use in Low‐Risk Patients (CHADS2 =0)
Among low‐risk patients with a CHADS2 score of 0, nonparoxysmal AF (61% vs 24%, P<0.001) and age between 65 to 74 years (50% vs 30%, P<0.001) were univariate predictors of warfarin use. On multivariate analysis, nonparoxysmal AF (odds ratio [OR]: 4.95, ± 95% confidence interval [CI]: 3.23–7.60, P<0.001) and age 65 to 74 years (OR: 2.22, ± 95% CI: 1.43–3.43, P<0.001) remained significant predictors of warfarin use.
Predictors of Warfarin Use in Intermediate‐Risk Patients (CHADS2 =1)
On univariate analysis, patients with nonparoxysmal AF were more likely to receive warfarin than patients with paroxysmal AF (84% vs 58%, P<0.001). Patients with CHF were more likely to be prescribed warfarin than patients with any of the other CHADS2 risk factors. In addition, patients with a CHADS2 score of 1 with CAD were more likely to receive warfarin (82% vs 66%, P<0.001). There was a trend for higher warfarin use in women than men (73% vs 67% for men, P = 0.07).
On multivariate analysis, left ventricular (LV) dysfunction with an ejection fraction ≤0.35 (OR: 6.68, ± 95% CI: 2.79–15.97, P<0.0001) and nonparoxysmal AF (OR: 4.09, ± 95% CI: 2.94–5.68, P<0.0001) were independent predictors of warfarin use in intermediate‐risk patients. The other CHADS2 risk factors did not predict warfarin use, although there was a trend toward use of warfarin in patients ≥75 years (OR: 1.489, ± 95% CI: 0.97–2.28, P = 0.067). Patients with a CHADS2 score of 1 who also had 1 of the minor risk factors, including CAD (OR: 2.53, ± 95% CI: 1.63–3.98, P<0.0001), age 65 to 74 years (OR: 1.68, ± 95% CI: 1.21–2.34, P = 0.002), or female gender (OR: 1.69, ±95% CI: 1.21–2.34, P = 0.002) were more likely to be on warfarin (Table 2).
Table 2.
Independent Predictors of Warfarin Use in Intermediate Risk Patients
| OR | ±95% CI | P | |
|---|---|---|---|
| Congestive heart failure | 6.68 | 2.79–15.97 | <0.0001 |
| Nonparoxysmal AF | 4.08 | 2.94–5.68 | <0.0001 |
| Age ≥75 years | 1.49 | 0.97–2.28 | 0.067 |
| Minor risk factors | |||
| Coronary artery disease | 2.53 | 1.55–3.61 | <0.0001 |
| Age 65–74 years | 1.81 | 1.31–2.51 | <0.0001 |
| Female | 1.50 | 1.09–2.08 | 0.013 |
Abbreviations: AF, atrial fibrillation, CI, confidence interval; OR, odds ratio. Variables included in the model were congestive heart failure, hypertension, diabetes mellitus, age 65 to 74 years, age >75 years, race, gender, paroxysmal or nonparoxysmal AF, and coronary artery disease or peripheral vascular disease.
Thromboembolic Events
TEs occurred during the study period in 110 patients. There were 331 patients who had a TE prior to the study period which is reflected in their CHADS2 score. Among the 110 patients who had a TE during the study period, 75 (68%) were not receiving warfarin and 35 patients (32%) were receiving warfarin at the time of the TE. Among the 75 patients who were not on warfarin at the time of TE, the CHADS2 score was 0 in 8 patients; 1 in 30 patients, and ≥2 in the remaining 37 patients. Among the 37 patients who were on warfarin, the CHADS2 score was 0 in 1 patient; 1 in 13 patients; and ≥2 in the remaining 23 patients (P = 0.28)(Figure 2). The TE event rate per year was 0.9% in patients with a CHADS2 score of 0 and 2.3% in patients with a CHADS2 score of 1 during the 2‐year study period.
Figure 2.
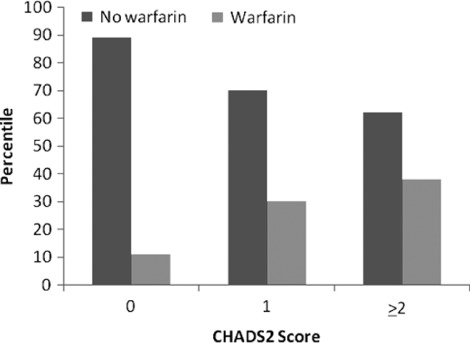
Warfarin use and thromboembolic events. The percentage of patients within each CHADS2 category who suffered from thromboembolic events and their anticoagulation status is shown.
Predictors of Thromboembolic Events
On univariate analysis, there was no association between warfarin use and the risk of TEs in patients with a CHADS2 score of 0. However, in patients with a CHADS2 score of 1, warfarin use was associated with a lower probability of TEs than aspirin or no specific therapy (2% vs 9%, P<0.001). There also was a trend toward higher prevalence of TEs in women than men (6.1% vs 3.5%, P = 0.06).
On multivariate analysis, warfarin use was not associated with a lower risk of TEs in patients with a CHADS2 score of 0. Among CHADS2 1 patients, lack of warfarin use (OR: 4.9, ± 95% CI: 2.56–9.45, P<0.001) and female gender (OR: 2.0, ± 95% CI: 1.07–3.71, P = 0.03) were both independent predictors of TEs; hypertension, diabetes, or age ≥75 years were not themselves predictors of TEs.
Bleeding Complications
A bleeding complication occurred in 15 patients (3%) with a CHADS2 score of 0, and warfarin was subsequently discontinued in 5. In patients with a CHADS2 score of 1, a bleeding complication was observed in 47 patients (3%), and warfarin was discontinued in 6. Among high‐risk patients with a CHADS2 score ≥2, warfarin had been discontinued in 50 patients (3%) due to a prior bleeding event. Nineteen patients discontinued warfarin due to prior fall or documented risk of falling (1%). Twenty‐three patients (1%) refused to take warfarin.
Discussion
Main Findings
The main findings of this study were: (1) despite ACC/AHA/ESC guidelines, ∼40% of low‐risk CHADS2 0 patients with AF and ∼70% of intermediate‐risk CHADS2 1 patients received warfarin; (2) low‐risk patients with nonparoxysmal AF or age 65 to 74 years were more likely to receive warfarin; (3) among intermediate‐risk patients, history of CHF or nonparoxysmal AF were associated with a higher probability of warfarin use; (4) the presence of an additional minor risk factor (female gender, CAD, or age 65–74 years) independently predicted warfarin use in intermediate‐risk patients, but individual CHADS2 factors alone did not; and (5) warfarin was associated with a reduction in TEs in intermediate‐risk patients with AF.
These findings suggest that warfarin is overused in patients at low risk for TEs despite ACC/AHA/ESC guidelines. However, in intermediate‐risk patients, warfarin appears to be more appropriate than aspirin in preventing TEs, particularly in the presence of additional minor risk factors.
Predictors of Warfarin Use
Although the 2006 ACC/AHA/ESC guidelines recommend risk stratification based on the CHADS2 score, our data suggest that other variables drive the decision to anticoagulate with warfarin. Specifically, the presence of nonparoxysmal AF strongly influences warfarin use among low‐ and intermediate‐risk patients with AF. Prior studies also demonstrated the tendency among physicians to prescribe warfarin based on the presence of nonparoxysmal AF.7, 8 However, current guidelines suggest that the decision to anticoagulate with warfarin should not be based on whether AF is paroxysmal or persistent, because both types of AF are associated with a similar risk of TEs.
In patients with AF at intermediate risk for TEs, either aspirin or warfarin can be used based on current guidelines. Warfarin was prescribed in 70% of CHADS2 1 patients in this study. Although there was an interaction between age and gender(ie, females with AF were older than the male patients) both female gender and age 65 to 74 years were independent predictors of warfarin use. Furthermore, age ≥75 years, a CHADS2 variable, was not an independent predictor, suggesting that there is a tendency among practitioners to prescribe warfarin earlier than the suggested age threshold of 75 years.
Our data possibly reflect an implicit adoption of a CHA2DS2‐VASc scoring system because gender, younger age, and CAD were incorporated into the decision to prescribe warfarin for many CHADS2 1 and CHADS2 0 patients. CHADS2 0 patients with a CHA2DS2‐VASc score of 1 or 2 might benefit more from warfarin than the CHADS2 scheme would suggest. Although the CHA2DS2‐VASc scoring system has only been adopted by the ESC guidelines yet was not addressed in recent updates to the ACC/AHA guidelines for the management of AF, it may be that physicians in our center had already trended toward that model of risk stratification during this study period.9, 10 However, the CHA2DS2‐VASc system still does not account for the tendency to prescribe warfarin for nonparoxysmal AF.
The 2006 ACC/AHA/ESC guidelines recommend warfarin in AF patients with LV dysfunction, although LV dysfunction by itself is not a recognized criterion for anticoagulation.1 In this study, LV dysfunction was identified as an independent predictor of warfarin use in patients with AF.
Thromboembolic Events
Warfarin was associated with a lower risk of TEs in intermediate‐risk CHADS2 1 patients with AF. Our data confirm findings in other reports that warfarin reduces the risk of TE in this patient cohort, although the risk of major bleeding may result in a marginal benefit with warfarin use for CHADS2 1 patients.11 Among CHADS2 1 patients, the tendency of physicians in our practice to prescribe warfarin when minor risk factors were present might also account for the effectiveness of warfarin in reducing TEs in this population, a difference that might have been accounted for if the CHA2DS2‐VASc scoring system had been used. However, new anticoagulants, such as dabigatran, that are associated with a lower risk of major hemorrhage than warfarin may be preferable to antiplatelet agents in patients with a CHADS2 score of 1.12, 13
Prior Studies
Several studies have already demonstrated underuse of warfarin in patients at high risk for stroke.1, 14, 15 However, there are few studies on warfarin use in low‐ and intermediate ‐risk patients. Similar to the findings of this study, warfarin was demonstrated to be beneficial in intermediate‐risk patients in a prior retrospective analysis.16 In that study, warfarin use was lower than the present study, whereas the annual TE event rate was 11%, which is higher than rates listed in other studies for CHADS2 1 patients. In this study, the annual TE event rate was consistent with other studies, yet a significant reduction in TEs was still demonstrated with warfarin.
A recent meta‐analysis of warfarin use in patients with AF that focused on the net clinical benefit by subtracting the risk of intracranial hemorrhage from the reduced risk of TEs with warfarin suggested the net effect of warfarin is pronounced in patients >85 years and who have CHADS2 score ≥4. In patients with a CHADS2 score of 1 there was marginal potential benefit.11
Limitations
A limitation of this study is that it is subject to all the inherent limitations of retrospective studies. Adverse events and comorbidities were identified through physician reporting, but there was no confirmation of events because there was no communication with patients or physicians to confirm events or diagnoses. A second limitation is that time in therapeutic range with warfarin could not be determined. A third limitation is the relatively short duration of follow‐up, limiting the ability to accurately assess long‐term cumulative risk of TEs and hemorrhagic events. A fourth limitation is that antiplatelet agent use could not be accurately captured within the dataset. A fifth limitation is that this study was performed at an academic university‐based medical center and may not represent well clinical practices in the general community.
Conclusion
This study suggests that warfarin is often used in patients at low risk for TEs without any clear indication and likely benefit. Despite the abundance of data and guideline recommendations, nonparoxysmal AF appears to influence the decision to anticoagulate patients at low and intermediate risk for TEs. Patients at intermediate risk for TEs appear to benefit from anticoagulation despite the risk of major hemorrhage. Given the results of recent trials demonstrating the superiority of new oral anticoagulants, the use of these anticoagulants among low‐ and intermediate‐risk AF patients remains to be seen.
References
- 1. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: full text: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Europace. 2006;8:651–745. [DOI] [PubMed] [Google Scholar]
- 2. Stroke Prevention in Atrial Fibrillation Study. Final results. Circulation. 1991;84:527–539. [DOI] [PubMed] [Google Scholar]
- 3. Connolly SJ, Laupacis A, Gent M, et al. Canadian Atrial Fibrillation Anticoagulation (CAFA) Study. J Am CollCardiol. 1991;18:349–355. [DOI] [PubMed] [Google Scholar]
- 4. Hart RG, Pearce LA, Aguilar MI. Meta‐analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–867. [DOI] [PubMed] [Google Scholar]
- 5. Hylek EM, Evans‐Molina C, Shea C, et al. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. 2007;115:2689–2696. [DOI] [PubMed] [Google Scholar]
- 6. Gage BF, Van Walraven C, Pearce L, et al. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation. 2004;110:2287–2292. [DOI] [PubMed] [Google Scholar]
- 7. Lewis WR, Fonarow GC, LaBresh KA, et al. Differential use of warfarin for secondary stroke prevention in patients with various types of atrial fibrillation. Am J Cardiol. 2009;103:227–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Waldo AL, Becker RC, Tapson VF, et al. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005;46:1729–1736. [DOI] [PubMed] [Google Scholar]
- 9. Camm AJ, Kirchof P, Lip GYH, et al. Guidelines for the management of atrial fibrillation. Eur Heart J. 2010;31:2369–2429. [DOI] [PubMed] [Google Scholar]
- 10. Wann LS, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/ HRS focused update on the management of patients with atrial fibrillation (update on dabigatran). Circulation. 2011;123:1144–1150. [DOI] [PubMed] [Google Scholar]
- 11. Singer DE, Chang Y, Fang MC, et al. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009;151:297–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. [DOI] [PubMed] [Google Scholar]
- 13. Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in atrial fibrillation. N Engl J Med. 2011;364:806–817. [DOI] [PubMed] [Google Scholar]
- 14. Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–2870. [DOI] [PubMed] [Google Scholar]
- 15. Brass LM, Krumholz HM, Scinto JM, et al. Warfarin use among patients with atrial fibrillation. Stroke. 1997;28:2382–2389. [DOI] [PubMed] [Google Scholar]
- 16. Lee BH, Park JS, Park JH, et al. The effect and safety of the antithrombotic therapies in patients with atrial fibrillation and CHADS score 1. J CardiovascElectrophysiol. 2010;21:501–507. [DOI] [PubMed] [Google Scholar]


