Abstract
Background
Lack of timely reperfusion therapy in patients with ST‐elevation myocardial infarction (STEMI) has been associated with worse outcomes. The aim of this study is to identify the frequency and predictors of delayed presentation and missed reperfusion in patients with STEMI in the Gulf Register of Acute Coronary Events (Gulf RACE) registry.
Delayed Presentation and missed reperfusion is associated with increased in hospital mortality in STEMI patients.
Methods
Gulf RACE is a prospective, multinational study of all consecutive patients hospitalized with the final diagnosis of acute coronary syndrome in 65 centers in 6 Arab countries. In this analysis, we included 3197 patients with STEMI. The independent predictors of delayed presentation and missed reperfusion therapy were identified using multivariate logistic regression.
Results
In total, 929 patients presented > 12 hours after symptom onset. The independent predictors of late presentation are older age, atypical symptoms, no family history of coronary artery disease, and being in Yemen. Of the 2268 STEMI patients presenting early, a total of 205 patients (9.3%) did not receive reperfusion therapy despite no contraindications (shortfall). The independent predictors of not receiving appropriate reperfusion therapy are older age, prior stroke, being in Yemen, and atypical symptoms. Lack of reperfusion therapy due to shortfall or delayed presentation was associated with increased in‐hospital mortality.
Conclusions
Nearly one‐third of patients with STEMI in the Arab Middle East present to the hospital > 12 hours after symptom onset, and nearly 1 in 10 eligible patients do not receive any reperfusion therapy. Community and physician awareness programs are needed to increase the utilization of appropriate lifesaving therapies. Copyright © 2010 Wiley Periodicals, Inc.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Introduction
Prompt reperfusion in patients with ST‐segment elevation myocardial infarction (STEMI) is essential to myocardial salvage and improved outcomes.1,2 Delays from symptom onset to hospital presentation have been associated with reduced likelihood of receiving appropriate timely reperfusion therapy.3, 4, 5, 6, 7 Late presenters have significantly longer delays prior to receiving evidence‐based therapies.6,8
On the other hand, more than one‐third of patients with STEMI do not receive appropriate reperfusion therapy despite early presentation.9, 10, 11, 12, 13 Failure to receive reperfusion therapy has been associated with worse outcomes.5,7,9,10,14,15 Most prior studies examining delays in presentation and the utilization of reperfusion therapy have been conducted in Western populations and developed countries. Practice patterns and patient characteristics in developing regions of the world may differ significantly from what has been observed in Western registries. In the Arab Middle East, appropriate use of reperfusion therapy in patients with STEMI has never been systematically examined. We thus evaluated the frequency and predictors of delayed presentation and missed reperfusion in a contemporary cohort with STEMI, based on data from the largest prospective multinational registry of acute coronary syndrome (ACS) in the Middle East.16
Methods
Study Population
The Gulf Registry of Acute Coronary Events (Gulf RACE) is a prospective, multinational study of all consecutive patients hospitalized with the final diagnosis of ACS in 65 centers in 6 Arab countries (Kuwait, Oman, United Arab Emirates, Yemen, Qatar, and Bahrain). Patients were enrolled from January 2007 to June 2007. Details of study organization have been previously described.17 All hospitals in Kuwait, Bahrain, and Qatar participated, and 90% of hospitals in United Arab Emirates and Oman and 85% of hospitals in Yemen participated. Nonparticipating hospitals were often small, with limited cardiac services. Of the 65 sites participating, only 18 had catheterization labs.
The definition of STEMI was based on the American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with ACS.18 For the purposes of this analysis, patients with STEMI and new left bundle‐branch block myocardial infarction (LBBB MI) were considered together, and are herein referred to as STEMI.
Data on baseline characteristics, duration of symptoms, admission profile, and in‐hospital treatments and outcomes were prospectively collected by the treating physicians. Patients were divided into 2 groups based on whether or not they presented within 12 hours of symptom onset. Contraindications to thrombolytic therapy were also recorded, including any prior intracranial hemorrhage, severely elevated blood pressure, malignant intracranial neoplasm, known structural cerebral vascular lesion, aortic dissection, trauma and cardiopulmonary resuscitation of > 20 minutes' duration, recent surgery, and pregnancy. Subsequently, patients presenting within 12 hours of symptom onset were divided into 2 groups based on whether or not they received reperfusion therapy (either thrombolytic therapy or primary coronary angioplasty).
Statistical Analysis
Continuous variables are summarized as median and interquartile ranges, and compared using the Wilcoxon rank sum test. Categorical variables are summarized as percentages, and compared using χ2 tests. Separate stepwise multivariate logistic regression analyses were used to identify independent predictors of delay in presentation, failure to receive reperfusion therapy, and in‐hospital mortality after adjusting for baseline covariates. Similarly, the association between delayed presentation and failure to receive timely reperfusion was examined using stepwise logistic regression models adjusting for age, gender, baseline covariates, and in‐hospital treatment patterns. For all multivariate modeling, the threshold for variable entry into models was P < 0.05, and the threshold for variable removal was P > 0.10. Selection of variables for entry consideration was based on clinical judgment, results of previous publications, and the expertise of the investigators. Care was given to avoidance of model overfitting by maintaining an events to covariate ratio of at least 10 to 1. Analyses were performed with the SAS 9.1 statistical package (SAS Institute, Cary, NC).
Results
Delayed Presentation
A total of 3197 patients (mean age 54 ± 12 y, 14% female) presented to the emergency room (ER) with acute STEMI/new‐onset LBBB MI, of which 929 (30%) presented > 12 hours after symptom onset (Figure 1). The baseline characteristics of the delayed patients are shown in Table 1. These patients were older (58 ± 13 vs 52 ± 11 y), more often female (20% vs 11%), and had a higher prevalence of smoking (45% vs 53%), dyslipidemia (14% vs 18%), prior stroke (5% vs 2%), and atypical symptoms (13% vs 5%). The median door‐to‐needle time for patients presenting within 12 hours of symptom onset was 36 minutes (interquartile range was 20–65 min). There were regional variations in the frequency of late presentation, with patients from Yemen most often presenting > 12 hours from symptom onset (59%). Late presenters had higher heart rate, lower systolic blood pressure, and a higher Global Registry of Acute Coronary Events (GRACE) score and Killip class (Table 1). In addition, delayed patients were less likely to receive evidence‐based therapies in the first 24 hours of hospitalization, including β‐blockers, angiotensin‐converting enzyme inhibitors (ACEIs), and statins, and were less likely to undergo coronary angiography during the index admission.
Figure 1.
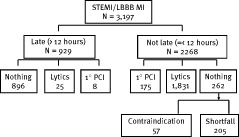
Characteristics of patients presenting with STEMI or LBBB MI. Abbreviations: LBBB MI, left bundle‐branch block myocardial infarction; N, number of patients; PCI, percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction
Table 1.
Baseline Characteristics and In‐hospital Outcomes of STEMI Patients Presenting >12 Hours and ≤12 Hours After Symptom Onset
| >12 h N=929 | ≤12 h N=2268 | ||
|---|---|---|---|
| Age, y | 57 (50–67) | 51 (45–60) | <0.0001 |
| Female gender | 19 | 11 | <0.0001 |
| Country | <0.0001 | ||
| Bahrain (n=88) | 9 | 91 | |
| Kuwait (n=754) | 15 | 85 | |
| Oman (n=479) | 22 | 78 | |
| Qatar (n=155) | 15 | 85 | |
| UAE (n=750) | 14 | 86 | |
| Yemen (n=971) | 59 | 41 | |
| HT | 32 | 33 | 0.56 |
| DM | 30 | 32 | 0.26 |
| Prior MI | 14 | 13 | 0.34 |
| Prior PCI | 3 | 6 | 0.0018 |
| Prior CABG | 2 | 1 | 0.08 |
| Smoking | 45 | 53 | 0.0002 |
| HL | 14 | 18 | 0.001 |
| Family history of CAD | 11 | 14 | 0.0066 |
| MI location | <0.0001 | ||
| Anterior | 58 | 53 | |
| Inferior | 32 | 41 | |
| Prior stroke | 5 | 2 | <0.0001 |
| Chest pain | 87 | 95 | <0.0001 |
| Resting HR (bpm) | 88 (77–100) | 80 (70–95) | <0.001 |
| SBP (mm Hg) | 130 (110–150) | 135 (120–154) | <0.001 |
| Peak CPK (mg/dL) | 455 (210–1208) | 1319 (446–2753) | <0.001 |
| Peak CKMB (mg/dL) | 71 (40–130) | 111 (50–234) | <0.001 |
| Ambulance use | 12 | 19 | <0.0001 |
| Door‐to‐ECG time (min) | 15 (8–21) | 10 (5–18) | <0.0001 |
| Killip class | <0.0001 | ||
| I (n=2555) | 71 | 83 | |
| II (n=388) | 18 | 10 | |
| III (n=153) | 7 | 4 | |
| IV (n=94) | 4 | 3 | |
| GRACE score | <0.0001 | ||
| Low (n=1131) | 28 | 47 | |
| Intermediate (n=812) | 30 | 30 | |
| High (n=734) | 42 | 23 | |
| Medication use | |||
| Aspirin | 98 | 98 | 0.30 |
| Clopidogrel | 59 | 59 | 0.96 |
| Unfractionated heparin | 74 | 63 | <0.0001 |
| LMW heparin | 22 | 31 | <0.0001 |
| IIb/IIIa inhibitors | 6 | 9 | 0.0013 |
| β‐Blockers | 55 | 65 | <0.0001 |
| ACEIs | 71 | 65 | 0.0006 |
| Statins | 88 | 91 | 0.0233 |
| Nitrates | 79 | 72 | <0.0001 |
| Diuretics | 22 | 16 | <0.0001 |
| Coronary angiography | 12 | 20 | <0.0001 |
| EF (n=2207) | 48 (40–55) | 46 (39–55) | 0.08 |
| Outcomes | |||
| Death | 10.4 | 3.9 | <0.0001 |
| Cardiogenic shock | 13 | 6 | <0.0001 |
| New‐onset heart failure | 11 | 6 | <0.0001 |
| Major bleeding | 1 | 1 | 0.72 |
| Stroke | 1 | 2 | 0.035 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; CABG, coronary artery bypass graft; CAD, coronary artery disease; CK, creatine kinase; CK‐MB, creatine kinase isoenzyme MB; DM, diabetes mellitus; ECG, electrocardiography; EF, ejection fraction; GRACE, Global Registry of Acute Coronary Events; HL, hyperlipidemia; HR, heart rate; HT, hypertension; LMW, low molecular weight; MI, myocardial infarction; n, number of patients; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; UAE, United Arab Emirates.
Continuous variables are summarized as median and interquartile ranges, and categorical variables are summarized as percentages
Outcomes of Late Presenters
A total of 186 patients (5.8%) died during hospitalization, of whom 97 patients (52.2%) presented early and 89 (47.2%) were late presenters. Delayed presentation was associated with significantly increased in‐hospital mortality (10.4% vs 3.9%, P < 0.0001). In addition, delayed presentation was associated with increased incidence of cardiogenic shock and new‐onset heart failure (Table 1).
The independent predictors of late presentation are shown in Table 2. After adjusting for potential confounders (age, gender, diabetes mellitus, hypertension, prior angioplasty, prior coronary artery bypass graft, smoking, family history of coronary artery disease [CAD], prior stroke, hyperlipidemia, presenting symptoms, country, use of ambulance, and interaction between age and gender), the independent predictors of late presentation were older age, atypical symptoms, family history of CAD, and being in Yemen (model c‐index 0.782).
Table 2.
Independent Predictors of Delayed Presentation in Patients With STEMI in the Arab Middle East
| OR | 95%CI | P Value | |
|---|---|---|---|
| Age (per 10 year) | 1.3 | 1.10–1.58 | <0.0001 |
| Prior PCI | 0.45 | 0.27–0.73 | 0.0012 |
| Atypical symptoms | 1.2 | 1.10–1.30 | <0.0001 |
| Country: Yemena | 11.8 | 5.5–25.2 | <0.0001 |
| Family history of CAD | 0.73 | 0.56–0.97 | 0.029 |
Abbreviations: CABG, coronary artery bypass graft; CAD, coronary artery disease; CI, confidence interval; DM, diabetes mellitus; HL, hyperlipidemia; HT, hypertension; OR, odds ratio; PCI, percutaneous coronary intervention.
Model adjusted for age, gender, DM, HT, prior angioplasty, prior CABG, smoking, family history of CAD, prior stroke, HL, presenting symptoms, country, use of ambulance, and interaction between age and gender. Model c‐index 0.782.
Compared with the country with lowest delayed presentation, Bahrain
Reperfusion Shortfall
A total of 2268 STEMI patients presented within 12 hours of symptom onset, of whom 2006 patients received either thrombolytic therapy (80.2%) or primary percutaneous coronary intervention (PCI) (19.8%). A total of 57 patients (2.5%) did not receive reperfusion therapy because they had contraindication to lytics, and 205 patients (9.3%) did not receive reperfusion therapy despite no contraindications (shortfall). Patients who did not receive any reperfusion therapy despite no contraindications were older, more often female, and more likely to have atherosclerotic risk factors or prior cardiovascular disease (Table 3). Shortfall patients presented less often via ambulance and had a longer door‐to‐electrocardiography (ECG) time. They complained of chest pain less often and were sicker at presentation, with higher Global Registry of Acute Coronary Events (GRACE) score, higher heart rate, lower systolic blood pressure, and higher Killip class (Table 3). In addition to not receiving reperfusion therapy, these patients received evidence‐based therapies less often, including a lower rate of statins, β‐blockers, and ACEIs. These patients had worse in‐hospital outcomes, including higher rates of death (9.3% vs 2.8%), cardiogenic shock, and new‐onset heart failure.
Table 3.
Comparison Between STEMI Patients Presenting Within 12 hours of Symptom Onset Based on Administration of Reperfusion Therapy
| Shortfall N=205 | Reperfusion N=2006 | P Value | |
|---|---|---|---|
| Age, y | 56 (48–65) | 50 (44–58) | <0.0001 |
| Female gender | 20 | 80 | <0.0001 |
| Country | <0.0001 | ||
| Bahrain (n=77) | 16 | 84 | |
| Kuwait (n=633) | 7 | 93 | |
| Oman (n=369) | 10 | 90 | |
| Qatar (n=128) | 12 | 88 | |
| UAE (n=637) | 4 | 96 | |
| Yemen (n=367) | 21 | 79 | |
| HT | 46 | 31 | <0.0001 |
| DM | 38 | 32 | 0.015 |
| Prior MI | 23 | 12 | <0.0001 |
| Prior PCI | 10 | 5 | 0.0067 |
| Prior CABG | 2 | 1 | 0.27 |
| Smoking | 42 | 54 | 0.0015 |
| HL | 22 | 18 | 0.12 |
| Family history of CAD | 18 | 14 | 0.084 |
| MI location | <0.0001 | ||
| Anterior | 54 | 53 | |
| Inferior | 32 | 41 | |
| Prior stroke | 4 | 1 | 0.0028 |
| Chest pain | 82 | 97 | <0.0001 |
| Resting HR (bpm) | 84 (72–100) | 80 (69–94) | 0.030 |
| SBP (mm Hg) | 130 (110–150) | 135 (120–152) | 0.25 |
| Peak CPK (mg/dL) | 403 (175–161) | 1471 (520–2903) | <0.0001 |
| Peak CK‐MB(mg/dL) | 57 (26–120) | 120 (56–244) | <0.0001 |
| Ambulance use | 14 | 20 | 0.032 |
| Door‐to‐ECG time (min) | 15 (10–30) | 10 (5–16) | <0.0001 |
| Killip class | <0.0001 | ||
| I (n=1862) | 71 | 85 | |
| II (n=215) | 16 | 9 | |
| III (n=79) | 7 | 3 | |
| IV (n=49) | 6 | 2 | |
| GRACE score | <0.0001 | ||
| Low (n=934) | 33 | 49 | |
| Intermediate (n=598) | 29 | 31 | |
| High (n=429) | 38 | 20 | |
| Medication use | |||
| Aspirin | 93 | 99 | <0.0001 |
| Clopidogrel | 52 | 60 | 0.021 |
| Unfractionated heparin | 60 | 63 | 0.41 |
| LMW heparin | 33 | 31 | 0.60 |
| IIb/IIIa inhibitors | 10 | 9 | 0.73 |
| β‐Blockers | 55 | 67 | 0.0008 |
| ACEIs | 54 | 66 | 0.0004 |
| Statins | 76 | 93 | <0.0001 |
| Nitrates | 74 | 71 | 0.56 |
| Diuretics | 24 | 15 | 0.0002 |
| EF (n=1524) | 50 (40–56) | 48 (40–55) | 0.34 |
| Coronary angiography | 17 | 21 | 0.204 |
| Outcomes | |||
| Death | 9.3 | 2.8 | <0.0001 |
| Cardiogenic shock | 13.7 | 6 | 0.0001 |
| New‐onset heart failure | 22 | 14 | 0.0019 |
| Major bleeding | 1 | 1 | 0.92 |
| Stroke | 0 | 0.6 | 0.26 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; CABG, coronary artery bypass graft; CAD, coronary artery disease; CK, creatine kinase; CK‐MB, creatine kinase isoenzyme MB; DM, diabetes mellitus; ECG, electrocardiography; EF, ejection fraction; GRACE, Global Registry of Acute Coronary Events; HL, hyperlipidemia; HR, heart rate; HT, hypertension; LMW, low molecular weight; MI, myocardial infarction; n, number of patients; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; UAE, United Arab Emirates.
Continuous variables are summarized as median and interquartile ranges, and categorical variables are summarized as percentages
The independent predictors of not receiving appropriate reperfusion therapy in the absence of contraindications are shown in Table 4 and include older age, prior stroke, being in Yemen, and lack of chest pain on presentation.
Table 4.
Independent Predictors of Failure to Administer Appropriate Reperfusion Therapy Among STEMI Patients Presenting Within 12 Hours of Symptom Onset
| OR | 95%CI | P Value | |
|---|---|---|---|
| Age (per 10‐y increase) | 1.2 | 1.04–1.37 | 0.012 |
| Prior stroke | 5.3 | 2.6–10.5 | <0.0001 |
| No chest pain | 1.6 | 1.4–1.8 | <0.0001 |
| HT | 1.6 | 1.2‐2.3 | 0.0046 |
| Country: Yemen vs UAE | 5.3 | 3.3–8.8 | <0.0001 |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; DM, diabetes mellitus; HT, hypertension; OR, odds ratio; SBP, systolic blood pressure; UAE, United Arab Emirates.
Model adjusted for age, gender, presentation heart rate, SBP, prior stroke, prior CAD, DM, use of ambulance, country, and chest pain on presentation (c‐index 0.773)
In‐Hospital Mortality
In univariate analysis, lack of reperfusion therapy due to shortfall or delayed presentation was associated with increased in‐hospital mortality (odds ratio [OR]: 3.9, 95% confidence interval [CI]: 2.9–5.4). Lack of appropriate reperfusion due to either delayed presentation or reperfusion shortfall was associated with a nearly 2‐fold increase in in‐hospital mortality (OR: 1.9, 95% CI: 1.2–3.0, P = 0.0074; c‐index 0.889). Other independent predictors of increased mortality were female gender, prior angioplasty, atypical symptoms, and nonambulance presentation.
Discussion
Our analysis shows that in 2007, nearly one‐third of patients with STEMI in the Arab Middle East presented to the hospital > 12 hours after symptom onset, and nearly 1 in 10 eligible patients did not receive any reperfusion therapy. Lack of reperfusion was more common in sicker patients and those with prior stroke or no chest pain on presentation, and was independently associated with a > 2‐fold increase in short‐term mortality.
This is the first report from the Arab Middle East that evaluated patient and physician factors associated with lack of appropriate reperfusion therapy. Our analysis is in agreement with previous reports from other registries. In a substudy of the National Registry of Myocardial Infarction (NRMI) in the United States, Ting and colleagues reported that the rate of delayed presentation (>12 hours) was 8.7%.6,8 Older age, female gender, minority race, and diabetes mellitus were the independent predictors of delayed presentation. Eagle et alreported that out of 2501 patients with STEMI enrolled in the GRACE study from 14 countries, only 1763 (70.5%) presented within 12 hours of symptom onset.19 Cohen et alreported that 40% of acute STEMI patients presented > 12 hours after symptom onset.13 Recently, Tatu‐Chitoiu et alreported that female gender and older age were independent predictors of late presentation in Romania.12 In our study, nearly one‐third of patients presented late. We also noted significant regional variation in the frequency of late presentation, suggesting that socioeconomic status and literacy rate may play an important role in late presentation. Future studies should evaluate potential factors contributing to delayed presentation and test whether specific programs directed toward this patient population impact the early presentation rate.
The lack of appropriate reperfusion therapy is not entirely the result of late presentation. Nearly 10% of early presenters did not receive appropriately indicated reperfusion therapy. This is lower than the previously reported shortfall rate that ranged from 22% in the Emergency Department Quality in Myocardial Infarction (EDQMI) registry to 30% in the GRACE registry.7,13,19 However, we noted significant regional variability in the rate of shortfall (4%–21%), which raises the question of whether shortfall rate is a marker of quality of care. Our analysis supports this notion, because most patients who did not receive appropriate reperfusion therapy also did not receive other important evidence‐based therapies. Increasing physician awareness of the evidence‐based practice guidelines, including but not limited to indications of reperfusion therapy, may potentially increase the utilization of the urgently needed therapies and would potentially improve patient outcomes. In addition, wider availability of healthcare facilities with rigorous processes to improve STEMI patients' early identification and treatment may improve healthcare delivery and outcomes.
Our analysis also confirms the previous observations that lack of reperfusion therapy secondary to both late presentation or shortfall is an independent predictor of in‐hospital mortality in patients with STEMI.5,7 Given the high rate of late presentation in the Arab Middle East, community‐awareness campaigns are needed, with special emphasis on women, older patients, and patients with prior stroke. Given the regional variation, these awareness campaigns may need to be prioritized to regions where late presenters are more frequent.
Our study has several limitations. Although our cohort included nearly consecutive patients with suspected ACS who live in 6 countries, we were able to include only 85% of patients in 3 of the countries. Nearly 60% of the study cohort had ejection fraction assessment, and only a minority of patients underwent coronary angiography. We did not have information about the socioeconomic status of patients and their literacy rate (the literacy rate is 28%, 53%, 89%, 89%, 91%, and 93% in Oman, Yemen, United Arab Emirates, Bahrain, Qatar, and Kuwait, respectively). Yemen is the largest country among the included countries and has the lowest income per capita.20 In addition, we did not have information about the credentials of treating physicians, thus we could not evaluate the impact of specialized training on shortfall rate.
Conclusion
Nearly one‐third of patients with STEMI in the Arab Middle East present to the hospital > 12 hours after symptom onset, and nearly 1 in 10 eligible patients do not receive any reperfusion therapy. Community and physician awareness programs are needed to increase the utilization of appropriate lifesaving therapies.
REFERENCES
- 1. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group [published correction appears in Lancet. 1994;343:742]. Lancet 1994; 343: 311–322. [PubMed] [Google Scholar]
- 2. Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2008; 51: 210–247. [DOI] [PubMed] [Google Scholar]
- 3. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000; 283: 2941–2947. [DOI] [PubMed] [Google Scholar]
- 4. Escabí‐Mendoza J. Reperfusion therapy in ST‐segment elevation myocardial infarction in the Veteran Administration Caribbean Healthcare System: search for improvement. Bol Asoc Med P R 2008; 100: 5–17. [PubMed] [Google Scholar]
- 5. McNamara RL, Herrin J, Wang Y, et al. Impact of delay in door‐to‐needle time on mortality in patients with ST‐segment elevation myocardial infarction. Am J Cardiol 2007; 100: 1227–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ting HH, Bradley EH, Wang Y, et al. Delay in presentation and reperfusion therapy in ST‐elevation myocardial infarction. Am J Med 2008; 121: 316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tricomi AJ, Magid DJ, Rumsfeld JS, et al. Missed opportunities for reperfusion therapy for ST‐segment elevation myocardial infarction: results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study. Am Heart J 2008; 155: 471–477. [DOI] [PubMed] [Google Scholar]
- 8. Ting HH, Bradley EH, Wang Y, et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST‐elevation myocardial infarction. Arch Intern Med 2008; 168: 959–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barron HV, Bowlby LJ, Breen T, et al. Use of reperfusion therapy for acute myocardial infarction in the United States: data from the National Registry of Myocardial Infarction 2. Circulation 1998; 97: 1150–1156. [DOI] [PubMed] [Google Scholar]
- 10. Fox KA, Goodman SG, Klein W, et al. Management of acute coronary syndromes. Variations in practice and outcome: findings from the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2002; 23: 1177–1189. [DOI] [PubMed] [Google Scholar]
- 11. Brady WJ, Perron A, Ullman E. Errors in emergency physician interpretation of ST‐segment elevation in emergency department chest pain patients. Acad Emerg Med 2000; 7: 1256–1260. [DOI] [PubMed] [Google Scholar]
- 12. Tatu‐Chitoiu G, Cinteza M, Dorobantu M, et al. In‐hospital case fatality rates for acute myocardial infarction in Romania. CMAJ 2009; 180: 1207–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cohen M, Gensini GF, Maritz F, et al. The role of gender and other factors as predictors of not receiving reperfusion therapy and of outcome in ST‐segment elevation myocardial infarction. J Thromb Thrombolysis 2005; 19: 155–161. [DOI] [PubMed] [Google Scholar]
- 14. Gibson CM, Pride YB, Frederick PD, et al. Trends in reperfusion strategies, door‐to‐needle and door‐to‐balloon times, and in‐hospital mortality among patients with ST‐segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J 2008; 156: 1035–1044. [DOI] [PubMed] [Google Scholar]
- 15. Masoudi FA, Magid DJ, Vinson DR, et al. Implications of the failure to identify high‐risk electrocardiogram findings for the quality of care of patients with acute myocardial infarction: results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study. Circulation 2006; 114: 1565–1571. [DOI] [PubMed] [Google Scholar]
- 16. Zubaid M, Rashed WA, Almahmeed W, et al. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE). Acta Cardiol 2009; 64: 439–446. [DOI] [PubMed] [Google Scholar]
- 17. Zubaid M, Rashed WA, Al‐Khaja N, et al. Clinical presentation and outcomes of acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE). Saudi Med J 2008; 29: 251–255. [PubMed] [Google Scholar]
- 18. Cannon CP, Battler A, Brindis RG, et al. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes: a report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee). J Am Coll Cardiol 2001; 38: 2114–2130. [DOI] [PubMed] [Google Scholar]
- 19. Eagle KA, Goodman SG, Avezum A, et al. Practice variation and missed opportunities for reperfusion in ST‐segment‐elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE). Lancet 2002; 359: 373–377. [DOI] [PubMed] [Google Scholar]
- 20.Wikipedia http://en.wikipedia.org/wiki/Yemen#Economy. Accessed April 18, 2010.


