Abstract
Background
A substantial minority of patients with acute coronary syndromes (ACS) do not have a diameter stenosis of any major epicardial coronary artery on angiography (“no obstruction at angiography”) of ≥ 50%. We examined the frequency of this finding and its relationship to race and sex.
Hypothesis
Among patients with myocardial infarction, younger age, female sex and non‐white race are associated with the absence of obstructive coronary artery disease at angiography.
Methods
We reviewed the results of all angiograms performed from May 19, 2006 to September 29, 2006 at 1 private (n = 793) and 1 public (n = 578) urban academic medical center. Charts were reviewed for indication and results of angiography, and for demographics.
Results
The cohort included 518 patients with ACS. There was no obstruction at angiography in 106 patients (21%), including 48 (18%) of 258 patients with myocardial infarction. Women were more likely to have no obstruction at angiography than men, both in the overall cohort (55/170 women [32%] vs 51/348 men [15%], P < 0.001) and in the subset with MI (29/90 women [32%] vs 19/168 men [11%], P < 0.001). Black patients were more likely to have no obstruction at angiography relative to any other subgroup (24/66 [36%] vs 41/229 [18%] Whites, 31/150 [21%] Hispanics, and 5/58 [9%] Asians, P = 0.001). Among women, Black patients more frequently had no obstruction at angiography compared with other ethnic groups (16/27 [59%] vs 17/59 [29%] Whites, 17/60 [28%] Hispanics, and 3/19 [6%] Asians, P = 0.001).
Conclusions
A high proportion of a multiethnic sample of patients with ACS were found to have no stenosis ≥ 50% in diameter at coronary angiography. This was particularly common among women and Black patients. Copyright © 2010 Wiley Periodicals, Inc.
This work was supported by the Doris Duke Charitable Foundation. Dr Reynolds is a recipient of the Doris Duke Charitable Foundation Clinical Scientist Development Award. The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
A substantial minority of patients presenting with acute coronary syndrome (ACS) are found to have no stenosis ≥ 50% diameter at angiography,1,2 and these patients are now recognized to accrue events in follow‐up.3, 4, 5 Secondary prevention strategies have been underutilized in this population.5
The mechanism of ACS in patients without obstructive coronary artery disease (CAD) is not well understood. Hypotheses include occult plaque disruption and transient luminal occlusion, endothelial or arteriolar dysfunction, and coronary vasospasm. Some patients presenting with chest pain and positive troponin (Tn) may have a nonischemic mechanism for myocyte injury, such as myocarditis or heart failure.6 Determining risk factors for events and differentiating between the possible causes may identify patients at higher risk for future cardiac events and ultimately guide preventive therapy.
Studies have suggested a lower frequency of obstructive CAD at angiography among Black patients, but these studies have been limited by smaller size or inclusion of a mostly White population.7, 8, 9, 10
We sought to examine the prevalence of absence of obstructive CAD and the effects of sex, race, and age on its prevalence in a diverse group of patients undergoing angiography at our medical center.
Methods
Results of all angiograms performed between May 19, 2006 and September 29, 2006 at 1 private (n = 793) and 1 public (n = 578) urban academic medical center were reviewed. Charts were reviewed for demographic data, and the final catheterization report was the source document for determining the indication for angiography. Race and ethnicity were self‐reported. We categorized patients as follows: White non‐Hispanic, Black non‐Hispanic, Asian non‐Hispanic, Hispanic (any race), other. Data for the group reporting other race are not reported here due to small numbers (n = 27). Data regarding risk factors for CAD, stress testing, and electrocardiographic (ECG) findings were not available for all patients examined. Therefore, these parameters are not reported in the present analysis.
Patients with the following indications for angiography were excluded from analysis: arrhythmia, planned percutaneous coronary intervention (PCI), preoperative evaluation for cardiac surgery, right heart catheterization, or valvular disease. If multiple angiograms had been performed on a patient during the study period, only the first angiogram was included in the analysis. After these exclusions, there were 1088 patients for analysis.
The indication for angiography was considered to be ACS if myocardial infarction (MI) (non–ST‐segment elevation or ST‐segment elevation) or unstable angina (UA) was listed on the catheterization report. Patients with elevated cardiac markers prior to catheterization were identified as having non–ST‐segment elevation myocardial infarction (NSTEMI) and ST‐segment elevation myocardial infarction (STEMI). The remaining indications were categorized as non‐ACS based on chart review and included stable angina, abnormal coronary artery computed tomography, abnormal stress test, and new diagnosis of congestive heart failure. The degree of stenosis on angiography was determined by visual estimation as assessed by experienced angiographers. Attending cardiologists and fellows performing angiography served both the private and public institutions.
No obstructive CAD at angiography was defined as the absence of ≥ 50% stenosis in any major epicardial vessel. The 50% stenosis level has frequently been used as the definition of “significant” or “obstructive” CAD. Results were categorized as normal if all arterial segments were described as “normal” by the angiographer. Angiograms with segments described as having even minimal luminal irregularities were categorized as nonobstructive (or mild) CAD.
Statistical Analysis
Dichotomous variables were compared by χ2 test. Continuous variables including age and estimated glomerular filtration rate (GFR) were analyzed by t test. GFR was calculated using the 4‐component Modification of Diet in Renal Disease Study equation. Frequencies of different clinical presentations (UA, STEMI, and NSTEMI) and frequency of obstructive CAD were compared by sex and by race/ethnicity. Individual race/ethnicity comparisons were performed based on a priori hypotheses (Black vs others, Asian vs others). For the analysis by age, we categorized patients based an age in years < 55, 55–69, and ≥ 70. The age threshold of 55 years was selected based on its use in the ongoing, National Heart, Lung, and Blood Institute (NHLBI)‐ funded Variation in Recovery: Role of Gender on Outcomes of Young Acute Myocardial Infarction Patients (VIRGO) registry, as well as other studies examining the effects of sex and age on outcomes in patients with coronary artery disease.11, 12
Results
A total of 1088 patients including 679 men (62%) and 409 women (39%) underwent coronary angiography for a variety of indications. Among these, 362 (33%) patients had no stenosis ≥ 50% diameter (186/409 women [43%] vs 176/679 men [20%], P < 0.001).
The ACS cohort that was the subject of remaining analyses included 518 patients, 258 (50%) of whom had MI as confirmed by cardiac marker elevation. Patient characteristics are shown in Table 1. No obstruction at angiography was found in 106 (21%) ACS patients and in 48 (18%) patients with confirmed MI. The frequency of no obstruction at angiography was similar in all types of ACS (58/260 [22%] UA vs 13/76 [19%] NSTEMI vs 35/185 [17%] STEMI, P = 0.538) (Figure 1). Women were as likely as men to have Tn elevation in our cohort (90/170 [48%] vs 168/348 [53%], P = 0.319). There was no difference in the frequency of nonobstructive CAD by center.
Table 1.
Patient Characteristics
| All | Non‐obstructivea | Obstructive | pValue | |
|---|---|---|---|---|
| 518 | 106 (20.5) | 412 (79.5) | ||
| Sex | ||||
| M, n (%) | 348 (67.2) | 51 (14.7) | 297 (85.3) | <0.001 |
| F, n (%) | 170 (32.8) | 55 (32.3) | 115 (67.6) | |
| Race/ethnicityb | ||||
| Asian, n (%) | 58 (11.2) | 5 (8.6) | 53 (91.4) | 0.001 |
| Black, n (%) | 66 (12.7) | 24 (36.4) | 42 (63.6) | |
| Hispanic, n (%) | 149 (29.0) | 31 (20.8) | 118 (79.2) | |
| White, n (%) | 229 (44.2) | 41 (17.9) | 188 (82.1) | |
| Age (y) | ||||
| All | 61±14 | 65±12 | 0.002 | |
| M | 57±14 | 64±12 | <0.001 | |
| F | 65±14 | 68±11 | 0.081 | |
| Indication for angiography | ||||
| STEMI, n (%) | 76 (14.7) | 13 (17.1) | 63 (82.9) | 0.538 |
| NSTEMI, n (%) | 182 (35.1) | 35 (19.2) | 147 (80.8) | |
| UA, n (%) | 260 (50.2) | 58 (22.3) | 202 (77.7) | |
| Hospital | ||||
| BHC, n (%) | 255 (49.2) | 57 (22.4) | 198 (77.6) | 0.294 |
| NYU, n (%) | 263 (50.8) | 49 (18.6) | 214 (81.4) | |
Abbreviations: ACS, acute coronary syndrome; BHC, Bellevue Hospital Center; F, female; M, male; n, number of patients; NSTEMI, non– ST‐segment elevation myocardial infarction; NYU, New York University Langone Medical Center; STEMI, ST‐segment elevation myocardial infarction; UA, unstable angina.
“Non‐obstructive” specifies <50% stenosis in all epicardial vessels.
Excludes 15 patients in race category “other”
Figure 1.
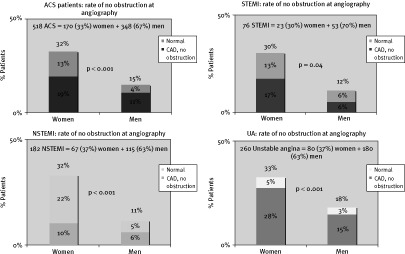
Rates of no obstruction at angiography by sex and indication for angiography. Abbreviations: ACS, acute coronary syndrome; CAD, coronary artery disease; NSTEMI, non–ST‐segment elevation myocardial infarction; STEMI, ST‐segment elevation myocardial infarction; UA, unstable angina. “No obstruction” specifies < 50% stenosis in all epicardial vessels
The absence of obstructive disease at angiography was more frequent in women than in men (55/170 [32%] vs 51/348 [15%], P < 0.001). Among those patients with NSTEMI or STEMI, women remained more likely than men to have no obstruction at angiography (29/90 [32%] vs 19/168 [11%], respectively, P < 0.001).
Black patients were more likely to have no obstruction at angiography than patients of other race/ethnic groups (24/66 [36%] vs 106/518 [20%], P < 0.001) (Figure 2). There was heterogeneity by race in the prevalence of no obstruction at angiography in women (P = 0.007) and not men (P = 0.254). In particular, Black women had a much higher likelihood of no obstruction at angiography compared with other racial/ethnic groups of women (16/27 [59%] vs 37/138 [27%], P = 0.001). Asian patients were less likely than other groups to have no obstruction at angiography (P = 0.036) (Figure 2). Patients who reported race/ethnicity other than White were more likely to have positive cardiac markers (Figure 2). This may reflect referral patterns to angiography at our institution. There was no difference in the prevalence of nonobstructive disease in any category of race/ethnicity by center, public vs private (data not shown). Among patients with positive cardiac markers, Blacks were more likely than patients of other races to have no obstruction at angiography (15/45 [33%] vs 18/134 [13%], respectively, P = 0.003).
Figure 2.
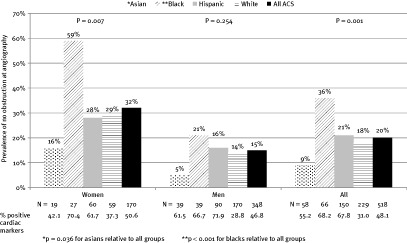
Prevalence of no obstruction at angiography by sex and race, along with percentages of positive cardiac markers. Abbreviations: ACS, acute coronary syndrome; N, number of patients. “No obstruction” specifies < 50% stenosis in all epicardial vessels
Obstructive CAD was more likely with increasing age (P < 0.0001). As seen in Figure 3, the highest prevalence of no obstruction at angiography was seen among the youngest women, such that the majority of women age > 55 years in our cohort had no obstructive CAD at angiography even though nearly half of this subgroup had positive cardiac markers.
Figure 3.
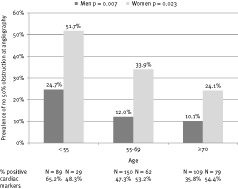
Prevalence of no obstruction at angiography by sex and age, along with percentages of positive cardiac markers. Abbreviations: N, number of patients. “No 50% obstruction” specifies < 50% stenosis in all epicardial vessels
The estimated GFR was slightly lower in patients with obstructive disease (71.3 ± 26.4 vs 79.2 ± 21.7 without, P = 0.002.)
Discussion
In this study, obstructive CAD was more often absent than present in Black women with ACS. This finding is even more striking considering that the large majority of Black female patients in our ACS cohort had objective evidence of myocardial necrosis. Given that patients, particularly women, may present with atypical ischemic symptoms, the lack of obstruction might otherwise be attributed to the subjective nature of clinician assessments.
Overall, 20% of our cohort of 518 patients with ACS had no obstructive CAD at angiography, and nearly one‐third of women had no obstructive CAD. The absence of obstructive CAD was more common in women, younger patients, patients without ST elevation, and Blacks. Our findings are consistent with prior reports in less racially and socioeconomically diverse cohorts.2, 3, 4,7, 8, 9, 10,13 The large American College of Cardiology‐National Cardiovascular Data Registry (ACC‐NCDR) database was recently analyzed for severity of CAD in patients with ACS; no stenosis > 50% was identified at angiography in 36% of Black women and 32% of Hispanic women.7 Although this was a large study (n = 450 329), the group consisted predominantly of White, Non‐Hispanic patients (91.6%), with Blacks, Hispanics, and Asians making up 5.2%, 1.9%, and 0.8% of the group, respectively. In the present study, Black, Asian, and Hispanic patients represented 13%, 11%, and 31% of the group, respectively.
We have demonstrated a relatively high frequency of no obstruction at angiography among women and men with all ACS subtypes as compared with a prior report based on a clinical‐trial population.14 These differences likely reflect our multiethnic population and higher sensitivity of Tn than creatine kinase‐myocardial band for myonecrosis.
Normal and Nonobstructive Angiography
Angiograms were categorized as normal if all arterial segments were described as “normal” by the angiographer, whereas angiograms with segments described as having even minimal luminal irregularities were categorized as nonobstructive (or mild) CAD. Patients with ACS and “normal” angiography have similar mortality and MI rates compared with those with “nonobstructive” disease.2 Furthermore, patients with normal coronary angiograms often have atherosclerosis on intravascular ultrasound.15, 16, 17 Therefore, we grouped patients with “normal” and “nonobstructive” CAD on angiography together in our analysis, as has been done previously.7,18
Possible Explanations for Less‐Frequent Obstructive CAD in Black Women
The high frequency of no obstruction at angiography among Black women in our study and others is noteworthy and has several potential explanations. Identification of etiologies of ACS in women with nonobstructive CAD is important because these patients are more likely to have adverse cardiovascular outcomes than asymptomatic women matched for age and number of CAD risk factors.19
Endothelial Dysfunction
Inability of the endothelium to induce appropriate vasodilatation in response to stressors is a frequently postulated etiology for ACS with no obstruction at angiography. Several studies have suggested that endothelial function varies with race. Blacks have been shown to have less vigorous brachial artery vasodilatation in response to endothelium‐dependent and endothelium‐independent stimulation of blood flow compared with Whites.20 In addition, young Black males have stronger microvascular and macrovascular responses to cold pressor testing.21 However, in a smaller (n = 39) study, Black and White women with chest‐pain syndromes and normal coronary arteries at angiography with no cardiovascular risk factors had similar vascular reactivity on invasive testing.22
Hypertension causes endothelial dysfunction23, 24, 25 and is more common among Blacks.26 Left ventricular hypertrophy, a consequence of hypertension that is more prevalent in Blacks,27 increases myocardial oxygen demand, which may predispose toward secondary MI.28, 29, 30 In patients with ischemic symptoms and no significant obstruction on coronary angiography, left ventricular hypertrophy is associated with perfusion defects on nuclear imaging as well as depressed coronary vasodilator reserve.31,32 In addition, hypertensive urgency is a well‐known cause of ischemic symptoms and elevation of cardiac markers.33 Data on the prevalence by race of hypertensive urgency and emergency are extremely limited, but there is some suggestion that Blacks (and women) are over‐ represented.34
Occult Plaque Rupture
It is well established that coronary angiography may fail to detect atherosclerotic plaque, including plaques that have ruptured.15, 16, 17 In the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study, Black patients were shown to have a more extensive burden of atherosclerosis than White patients at autopsy. The mean percent intimal surface area involved with total atherosclerotic lesions for all segments was greater in Blacks than in Whites, though the mean percent area involved with raised lesions (which are more likely to be apparent at angiography) did not differ between the 2 groups.35 It is plausible that angiography has poorer sensitivity for atherosclerosis in this racial subgroup. Similarly, positive (outward) remodeling of the coronary arteries, which is known to be more common in women than men, could explain a higher prevalence of nonobstructive disease on angiography in women with cardiovascular events.36 These independent findings in Blacks and women may help to explain our findings.
Blood Disorders
Sickle cell disease and mutations in the β chain of hemoglobin may play a role in vascular thrombosis. In a group of Black African subjects with ACS, hemoglobin S or C trait was identified in 57% of those with no obstructive CAD at angiography as compared with 22% of those with obstructive CAD (P < 0.03).37 We do not have information about hemoglobin mutations in our patients.
In addition, Black patients are known to have higher levels of fibrinogen, D‐dimer, and factor VII relative to other races, even after adjusting for cardiovascular risk factors.38 Black women have particularly high levels of fibrinogen.38 Fibrinogen has been consistently associated with increased risk of coronary heart disease.39 This could be a mechanism by which Black men and women may be more susceptible to acute coronary thrombosis without obstructive atherosclerosis.
Low Prevalence of Nonobstructive CAD Among Asian Patients
We found a lower prevalence of no obstruction at angiography among Asian patients than other groups, consistent with previous literature.7 However, South Asians, typically reported under the Asian category, have an unusually high rate of obstructive CAD and may have different underlying pathophysiology.40 Analyzing South Asian and East Asian patients together therefore is likely to introduce inaccuracies. Future studies should be designed to collect subgroup data within the Asian population.
Study Limitations
This is a retrospective study in which the main patient and angiographic data source was the cardiac catheterization report. Cardiovascular risk factors, medication, and illegal drug use data were not available for all patients examined. The group of patients studied may not be representative of minority patients in the general population because of potential sex‐based and race/ethnicity‐based referral bias for angiography. No quantitative coronary angiography was performed. Only half of the patients referred for angiography during the study time period were referred for evaluation of ACS. Given the study design and limited prospective data collection, no treatment or outcome results were studied.
Conclusion
The rate of no obstructive CAD at angiography was high in this multiethnic sample of patients with ACS. The absence of obstruction at angiography was particularly common among women and Blacks, the majority of whom had MI as evidenced by biochemical evidence of myocardial necrosis. Effective treatment will require a better understanding of the pathophysiology in these patients. Further study regarding mechanism(s) of ACS with no obstruction at angiography, particularly in Black patients, may provide insight into these findings.
REFERENCES
- 1. Rigatelli G, Rigatelli G, Rossi P, et al. Normal angiogram in acute coronary syndromes: the underestimated role of alternative substrates of myocardial ischemia. Int J Cardiovasc Imaging 2004; 20: 471–475. [DOI] [PubMed] [Google Scholar]
- 2. Bugiardini R, Bairey Merz CN. Angina with “normal” coronary arteries: a changing philosophy. JAMA 2005; 293: 477–484. [DOI] [PubMed] [Google Scholar]
- 3. Diver DJ, Bier JD, Ferreira PE, et al. Clinical and arteriographic characterization of patients with unstable angina without critical coronary arterial narrowing (from the TIMI‐IIIA Trial). Am J Cardiol 1994; 74: 531–537. [DOI] [PubMed] [Google Scholar]
- 4. Johnson BD, Shaw LJ, Buchthal SD, et al. Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: results from the National Institutes of Health‐National Heart, Lung, and Blood Institute–Sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation 2004; 109: 2993–2999. [DOI] [PubMed] [Google Scholar]
- 5. Dwyer JP, Redfern J, Freedman SB. Low utilisation of cardiovascular risk reducing therapy in patients with acute coronary syndromes and non‐obstructive coronary artery disease. Int J Cardiol 2008; 129: 394–398. [DOI] [PubMed] [Google Scholar]
- 6. Korff S, Katus HA, Giannitsis E. Differential diagnosis of elevated troponins. Heart 2006; 92: 987–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shaw LJ, Shaw RE, Merz CN, et al. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in‐hospital mortality in the American College of Cardiology‐National Cardiovascular Data Registry. Circulation 2008; 117: 1787–1801. [DOI] [PubMed] [Google Scholar]
- 8. Patel MR, Chen AY, Peterson ED, et al. Prevalence, predictors, and outcomes of patients with non–ST‐segment elevation myocardial infarction and insignificant coronary artery disease: results from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines (CRUSADE) initiative. Am Heart J 2006; 152: 641–647. [DOI] [PubMed] [Google Scholar]
- 9. Onwuanyi AE, Abe O, McMahon DJ, et al. Disparity in frequency of normal coronary artery in black and white patients undergoing cardiac catheterization. Ethn Dis 2006; 16: 370–374. [PubMed] [Google Scholar]
- 10. Peniston RL, Lu DY, Papademetriou V, et al. Severity of coronary artery disease in black and white male veterans and likelihood of revascularization. Am Heart J 2000; 139: 840–847. [DOI] [PubMed] [Google Scholar]
- 11. Vaccarino V, Parsons L, Every NR, et al. Sex‐based differences in early mortality after myocardial infarction: National Registry of Myocardial Infarction 2 Participants. N Engl J Med 1999; 341: 217–225. [DOI] [PubMed] [Google Scholar]
- 12. Lehto HR, Lehto S, Havulinna AS, et al. Are coronary event rates declining slower in women than in men—evidence from two population‐based myocardial infarction registers in Finland? BMC Cardiovasc Disord 2007; 7: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Whittle J, Conigliaro J, Good CB, et al. Black‐white differences in severity of coronary artery disease among individuals with acute coronary syndromes. J Gen Intern Med 2002; 17: 867–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hochman JS, Tamis JE, Thompson TD, et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes: Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. N Engl J Med 1999; 341: 226–232. [DOI] [PubMed] [Google Scholar]
- 15. Nissen S. Coronary angiography and intravascular ultrasound. Am J Cardiol 2001; 87(4 suppl A): 15A–20A. [DOI] [PubMed] [Google Scholar]
- 16. Schoenhagen P, Ziada KM, Kapadia SR, et al. Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation 2000; 101: 598–603. [DOI] [PubMed] [Google Scholar]
- 17. Claude M, Grodin I, Pasternac A, et al. Discrepancies between cineangiographic and postmortem findings in patients with coronary artery disease and recent myocardial revascularization Circulation 1974; 49: 703–708. [DOI] [PubMed] [Google Scholar]
- 18. Gehrie ER, Reynolds HR, Chen AY, et al. Characterization and outcomes of women and men with non–ST‐segment elevation myocardial infarction and nonobstructive coronary artery disease: results from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) quality improvement initiative. Am Heart J 2009; 158: 688–694. [DOI] [PubMed] [Google Scholar]
- 19. Gulati M, Cooper‐DeHoff RM, McClure C, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med 2009; 169: 843–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Campia U, Choucair WK, Bryant MB, et al. Reduced endothelium‐dependent and ‐independent dilation of conductance arteries in African Americans. J Am Coll Cardiol 2002; 40: 754–760. [DOI] [PubMed] [Google Scholar]
- 21. Adamopoulos D, Ngatchou W, Lemogoum D, et al. Intensified large artery and microvascular response to cold adrenergic stimulation in African Blacks. Am J Hypertens 2009; 9: 958–963. [DOI] [PubMed] [Google Scholar]
- 22. Houghton JL, Carr AA, Strogatz DS, et al. Coronary vasomotor reactivity among normotensive African and white American subjects with chest pain. Am J Med 1997; 102: 245–251. [DOI] [PubMed] [Google Scholar]
- 23. Treasure CB, Klein JL, Vita JA, et al. Hypertension and left ventricular hypertrophy are associated with impaired endothelium‐mediated relaxation in human coronary resistance vessels. Circulation 1993; 87: 86–93. [DOI] [PubMed] [Google Scholar]
- 24. Egashira K, Suzuki S, Hirooka Y, et al. Impaired endothelium‐dependent vasodilation of large epicardial and resistance coronary arteries in patients with essential hypertension: different responses to acetylcholine and substance P. Hypertension 1995; 25: 201–206. [DOI] [PubMed] [Google Scholar]
- 25. Brush JE, Jr. , Faxon DP, Salmon S, et al. Abnormal endothelium‐dependent coronary vasomotion in hypertensive patients. J Am Coll Cardiol 1992; 19: 809–815. [DOI] [PubMed] [Google Scholar]
- 26. Cooper RS, Liao Y, Rotimi C. Is hypertension more severe among U.S. blacks, or is severe hypertension more common? Ann Epidemiol 1996; 6: 173–180. [DOI] [PubMed] [Google Scholar]
- 27. Kamath S, Markham D, Drazner MH. Increased prevalence of concentric left ventricular hypertrophy in African‐Americans: will an epidemic of heart failure follow? Heart Fail Rev 2006; 11: 271–277. [DOI] [PubMed] [Google Scholar]
- 28. Clark LT, Ferdinand KC, Flack JM, et al. Coronary heart disease in African Americans. Heart Dis 2001; 3: 97–108. [DOI] [PubMed] [Google Scholar]
- 29. Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation 2007; 116: 2634–2653. [DOI] [PubMed] [Google Scholar]
- 30. Chambers J. Left ventricular hypertrophy. BMJ 1995; 311: 273–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Houghton JL, Frank MJ, Carr AA, et al. Relations among impaired coronary flow reserve, left ventricular hypertrophy and thallium perfusion defects in hypertensive patients without obstructive coronary artery disease. J Am Coll Cardiol 1990; 15: 43–51. [DOI] [PubMed] [Google Scholar]
- 32. Houghton JL, Smith VE, Strogatz DS, et al. Effect of African‐American race and hypertensive left ventricular hypertrophy on coronary vascular reactivity and endothelial function. Hypertension 1997; 29: 706–714. [DOI] [PubMed] [Google Scholar]
- 33. White HD, Steg PG, Dzavik V, et al. Predictors of reinfarction following PCI or medical management in patients with persistent total occlusion after myocardial infarction: results from the Occluded Artery Trial (OAT). Circulation 2007; 116(II): 625a. [Google Scholar]
- 34. Bender SR, Fong MW, Heitz S, et al. Characteristics and management of patients presenting to the emergency department with hypertensive urgency. J Clin Hypertens (Greenwich) 2006; 8: 12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Strong JP, Malcom GT, Oalmann MC, et al. The PDAY Study: natural history, risk factors, and pathobiology. Pathobiological Determinants of Atherosclerosis in Youth. Ann N Y Acad Sci 1997; 811: 226–237. [DOI] [PubMed] [Google Scholar]
- 36. Pepine CJ, Kerensky RA, Lambert CR, et al. Some thoughts on the vasculopathy of women with ischemic heart disease. J Am Coll Cardiol 2006; 47(3 suppl): S30–S35. [DOI] [PubMed] [Google Scholar]
- 37. Bertrand E, Renambot J, Chauvet J, et al. Coronary disease with normal coronarography in the black Africans: epidemiological and clinical data in 31 cases. Role of abnormal hemoglobins [in French.]. Arch Mal Coeur Vaiss 1993; 86: 415–419. [PubMed] [Google Scholar]
- 38. Lutsey PL, Cushman M, Steffen LM, et al. Plasma hemostatic factors and endothelial markers in four racial/ethnic groups: the MESA study. J Thromb Haemost 2006; 4: 2629–2635. [DOI] [PubMed] [Google Scholar]
- 39. Danesh J, Lewington S, Thompson SG, et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta‐analysis. JAMA 2005; 294: 1799–1809. [DOI] [PubMed] [Google Scholar]
- 40. Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation 2001; 104: 2855–2864. [DOI] [PubMed] [Google Scholar]


