Abstract
These clinical practice guidelines are an update of the guidelines published by the Infectious Diseases Society of America (IDSA) in 2009, prior to the 2009 H1N1 influenza pandemic. This document addresses new information regarding diagnostic testing, treatment and chemoprophylaxis with antiviral medications, and issues related to institutional outbreak management for seasonal influenza. It is intended for use by primary care clinicians, obstetricians, emergency medicine providers, hospitalists, laboratorians, and infectious disease specialists, as well as other clinicians managing patients with suspected or laboratory-confirmed influenza. The guidelines consider the care of children and adults, including special populations such as pregnant and postpartum women and immunocompromised patients.
Keywords: seasonal influenza, diagnostic testing, treatment, chemoprophylaxis, institutional outbreaks
EXECUTIVE SUMMARY
Seasonal influenza A and B virus epidemics are associated with significant morbidity and mortality each year in the United States and worldwide. One study estimated that during 2010–2016, the seasonal incidence of symptomatic influenza among all ages in the United States was approximately 8% and varied from 3% to 11% [1]. Most people recover from uncomplicated influenza, but influenza can cause complications that result in severe illness and death, particularly among very young children, older adults, pregnant and postpartum women within 2 weeks of delivery, people with neurologic disorders, and people with certain chronic medical conditions including chronic pulmonary, cardiac, and metabolic disease, and those who are immunocompromised [2–8]. During 2010–2018, seasonal influenza epidemics were associated with an estimated 4.3–23 million medical visits, 140 000–960 000 hospitalizations, and 12 000–79 000 respiratory and circulatory deaths each year in the United States [9]. A recent modeling study estimated that 291 243–645 832 seasonal influenza-associated respiratory deaths occur annually worldwide [10].
Use of available diagnostic modalities and proper interpretation of results can accurately identify patients presenting with influenza. Timely diagnosis may decrease unnecessary laboratory testing for other etiologies and use of antibiotics, improve the effectiveness of infection prevention and control measures, and increase appropriate use of antiviral medications [11, 12]. Early treatment with antivirals reduces the duration of symptoms and risk of some complications (bronchitis, otitis media, and pneumonia) and hospitalization, and may decrease mortality among high-risk populations [13–16]. Annual vaccination is the best method for preventing or mitigating the impact of influenza, but in certain situations, chemoprophylaxis with antiviral medications can be used for preexposure or postexposure prevention and can help control outbreaks in certain populations.
These clinical practice guidelines are an update of the guidelines published by the Infectious Diseases Society of America (IDSA) in 2009 [17]. The guidelines consider the care of children, pregnant and postpartum women, and nonpregnant adults and include special considerations for patients who are severely immunocompromised such as hematopoietic stem cell and solid organ transplant recipients. The target audience includes primary care clinicians, obstetricians, emergency medicine providers, hospitalists, and infectious disease specialists. The guidelines may be also useful for occupational health physicians and clinicians working in long-term care facilities. It adds new information on diagnostic testing, use of antivirals, and considerations of when to use antibiotics and when to test for antiviral resistance, and presents evidence on harm associated with routine use of corticosteroids.
The panel followed a process used in the development of previous IDSA guidelines that included a systematic weighting of the strength of recommendations and quality of evidence based upon the US Public Health Service Grading System for ranking recommendations in clinical guidelines as utilized in the previous 2009 guidelines (Table 1) [17]. Summarized below are the recommendations. A detailed description of background, methods, evidence summary, and rationale that support each recommendation, and research needs are included in the full document.
Table 1.
Infectious Diseases Society of America-US Public Health Service Grading System for Ranking Recommendations in Clinical Guidelines
| Category and Grade | Definition |
|---|---|
| Strength of recommendation | |
| A | Good evidence to support a recommendation for or against use |
| B | Moderate evidence to support a recommendation for or against use |
| C | Poor evidence to support a recommendation |
| Quality of evidence | |
| I | Evidence from 1 or more properly randomized controlled trials |
| II | Evidence from 1 or more well-designed clinical trials, without randomization; from cohort or case-controlled analytic studies (preferably from >1 center); from multiple time-series; or from dramatic results from uncontrolled experiments |
| III | Evidence from opinions of respected authorities, based on clinical experience, descriptive studies, or reports of expert committees |
Adapted from the Canadian Task Force on the Periodic Health Examination [6].
Because prevention and control of influenza is a dynamic field, clinicians should consult the website of the Centers for Disease Control and Prevention (CDC) for the latest information about influenza vaccines, influenza tests, and approved antiviral medications.
DIAGNOSIS
Which Patients Should Be Tested for Influenza?
Recommendations
Outpatients (including emergency department patients).
-
1During influenza activity (defined as the circulation of seasonal influenza A and B viruses among persons in the local community) (see Figure 1):
- Clinicians should test for influenza in high-risk patients, including immunocompromised persons who present with influenza-like illness, pneumonia, or nonspecific respiratory illness (eg, cough without fever) if the testing result will influence clinical management (A-III).
- Clinicians should test for influenza in patients who present with acute onset of respiratory symptoms with or without fever, and either exacerbation of chronic medical conditions (eg, asthma, chronic obstructive pulmonary disease [COPD], heart failure) or known complications of influenza (eg, pneumonia) if the testing result will influence clinical management (A-III) (see Table 3).
- Clinicians can consider influenza testing for patients not at high risk for influenza complications who present with influenza-like illness, pneumonia, or nonspecific respiratory illness (eg, cough without fever) and who are likely to be discharged home if the results might influence antiviral treatment decisions or reduce use of unnecessary antibiotics, further diagnostic testing, and time in the emergency department, or if the results might influence antiviral treatment or chemoprophylaxis decisions for high-risk household contacts (see recommendations 40–42) (C-III).
-
2During low influenza activity without any link to an influenza outbreak:
- Clinicians can consider influenza testing in patients with acute onset of respiratory symptoms with or without fever, especially for immunocompromised and high-risk patients (B-III).
Figure 1.
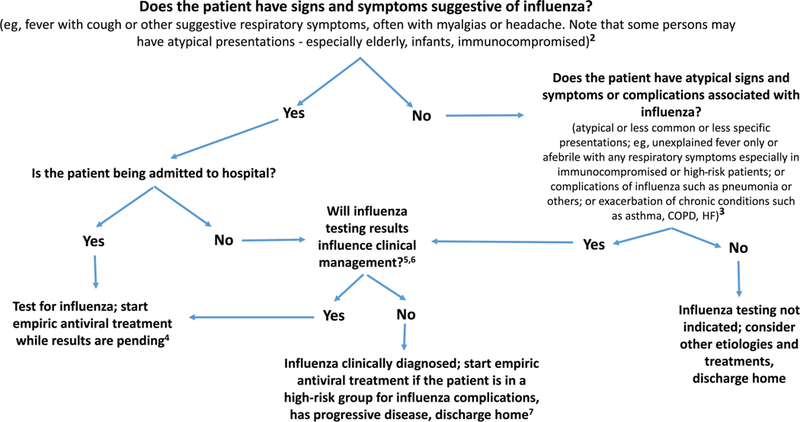
Guide for considering influenza testing when influenza viruses are circulating in the community (regardless of influenza vaccination history). 1Confirmation of influenza virus infection by diagnostic testing is not required for decisions to prescribe antiviral medication. Decision making should be based upon signs and symptoms consistent with influenza illness and epidemiologic factors. Initiation of empiric antiviral treatment should not be delayed while influenza testing results are pending. Antiviral treatment is clinically most beneficial when started as close to illness onset as possible. 2Signs and symptoms of uncomplicated influenza (see Table 2). 3Clinical manifestations and complications associated with influenza (see Table 3) and persons who are at high risk of complications from influenza (Table 4). 4All hospitalized patients with suspected influenza should be tested, as detection of influenza virus infection and prompt initiation of antiviral therapy are most clinically beneficial, and implementation of infection prevention and control measures is essential for prevention of nosocomial influenza outbreaks. 5Influenza testing may be used to inform decisions on use of antibiotics or continuation of antiviral medication, on need for further diagnostic tests, on consideration for home care, or on recommendations for ill persons living with others who are at high risk for influenza complications (see Table 4). 6Influenza testing may be required to inform decisions on infection control practices. 7Antiviral treatment is recommended for outpatients with suspected influenza who are at high risk for complications from influenza, or those with progressive disease not requiring hospital admission. Antiviral treatment of outpatients who are not at high risk for influenza complications (see Table 4) can be considered based upon clinical judgment if presenting within 2 days of illness onset. Abbreviations: HF, heart failure; COPD, chronic obstructive pulmonary disease.
Table 3.
Clinical Manifestations and Complications Associated With Influenza
| Population | Clinical Manifestation/Complication |
|---|---|
| Infants and preschool children | Fever without respiratory complications, “sepsis-like syndrome” Otitis media Parotitis Bronchiolitis Croup Reactive airway disease Pneumonia Myocarditis, pericarditis Rhabdomyolysis Febrile seizures Encephalopathy and encephalitis Invasive bacterial coinfection Reye syndrome (with aspirin exposure) Sudden death Exacerbation of chronic disease |
| School-aged children | Otitis media Parotitis Bronchitis Sinusitis Reactive airway disease Pneumonia Myocarditis, pericarditis Myositis (bilateral gastrocnemius, soleus) Rhabdomyolysis Encephalopathy and encephalitis Invasive bacterial coinfection Reye syndrome (with aspirin use) Toxic shock syndrome Sudden death Exacerbation of chronic disease |
| Adults | Parotitis Bronchitis Sinusitis Reactive airway disease Pneumonia Myocarditis, pericarditis Myositis Rhabdomyolysis Invasive bacterial coinfection Invasive fungal coinfection (rare) Toxic shock syndrome due to Staphylococcus aureus or Streptococcus pyogenes Precipitation of acute cardiovascular events (eg, cardiac failure, myocardial infarction, heart failure, cerebrovascular accident) Acute kidney injury and acute renal failure (with rhabdomyolysis or multiorgan failure) Encephalopathy and encephalitis Exacerbation of chronic disease |
| Elderly patients | Pneumonia Invasive bacterial coinfection Myositis Exacerbation of chronic disease |
| Special groups: pregnant and postpartum women | Dehydration Pneumonia Cardiopulmonary disease Premature labor Fetal loss |
| Special groups: immunocompromised, immunosuppressed | Complications similar to immunocompetent patients, but severe pneumonia and acute respiratory distress syndrome may be more common. |
| All ages | Respiratory failure Acute respiratory distress syndrome Multiorgan failure Sepsis Liver inflammation |
Adapted from Jani AA, Uyeki TM. Chapter 46. Influenza. In: Emergency management of infectious diseases. 2nd ed. Chin RL, ed. Cambridge, UK: Cambridge University Press, 2018.
Hospitalized Patients.
-
3During influenza activity:
- Clinicians should test for influenza on admission in all patients requiring hospitalization with acute respiratory illness, including pneumonia, with or without fever (A-II).
- Clinicians should test for influenza on admission in all patients with acute worsening of chronic cardiopulmonary disease (eg, COPD, asthma, coronary artery disease, or heart failure), as influenza can be associated with exacerbation of underlying conditions (A-III).
- Clinicians should test for influenza on admission in all patients who are immunocompromised or at high risk of complications and present with acute onset of respiratory symptoms with or without fever, as the manifestations of influenza in such patients are frequently less characteristic than in immunocompetent individuals (A-III).
- Clinicians should test for influenza in all patients who, while hospitalized, develop acute onset of respiratory symptoms, with or without fever, or respiratory distress, without a clear alternative diagnosis (A-III).
-
4During periods of low influenza activity:
- Clinicians should test for influenza on admission in all patients requiring hospitalization with acute respiratory illness, with or without fever, who have an epidemiological link to a person diagnosed with influenza, an influenza outbreak or outbreak of acute febrile respiratory illness of uncertain cause, or who recently traveled from an area with known influenza activity (A-II).
- Clinicians can consider testing for influenza in patients with acute, febrile respiratory tract illness, especially children and adults who are immunocompromised or at high risk of complications, or if the results might influence antiviral treatment or chemoprophylaxis decisions for high-risk household contacts (see recommendations 41–43) (B-III).
What Specimen(s) Should Be Collected When Testing Patients for Influenza?
Recommendations
-
5Clinicians should collect upper respiratory tract specimens from outpatients for influenza testing as soon after illness onset as possible, preferably within 4 days of symptom onset (A-II).
- Nasopharyngeal specimens should be collected over other upper respiratory tract specimens to increase detection of influenza viruses (A-II).
- If nasopharyngeal specimens are not available, nasal and throat swab specimens should be collected and combined together for influenza testing over single specimens from either site (particularly over throat swabs) to increase detection of influenza viruses (A-II).
- Mid-turbinate nasal swab specimens should be collected over throat swab specimens to increase detection of influenza viruses (A-II).
- Flocked swab specimens should be collected over non-flocked swab specimens to improve detection of influenza viruses (A-II).
-
6
Clinicians should collect nasopharyngeal (optimally, as for outpatients), mid-turbinate nasal, or combined nasal–throat specimens from hospitalized patients without severe lower respiratory tract disease for influenza testing as soon as possible (A-II).
-
7
Clinicians should collect endotracheal aspirate or bronchial-veolar lavage fluid specimens from hospitalized patients with respiratory failure receiving mechanical ventilation, including patients with negative influenza testing results on upper respiratory tract specimens, for influenza testing as soon as possible (A-II).
-
8
Clinicians should not collect or routinely test specimens for influenza from nonrespiratory sites such as blood, plasma, serum, cerebrospinal fluid, urine, and stool (A-III).
-
9
Clinicians should not collect serum specimens, including single or paired sera, for serological diagnosis of seasonal influenza virus infection for clinical management purposes (A-III).
What Test(s) Should Be Used to Diagnose Influenza?
Recommendations
-
10
Clinicians should use rapid molecular assays (ie, nucleic acid amplification tests) over rapid influenza diagnostic tests (RIDTs) in outpatients to improve detection of influenza virus infection (A-II) (see Table 6).
-
11
Clinicians should use reverse-transcription polymerase chain reaction (RT-PCR) or other molecular assays over other influenza tests in hospitalized patients to improve detection of influenza virus infection (A-II) (see Table 6).
-
12
Clinicians should use multiplex RT-PCR assays targeting a panel of respiratory pathogens, including influenza viruses, in hospitalized immunocompromised patients (A-III).
-
13
Clinicians can consider using multiplex RT-PCR assays targeting a panel of respiratory pathogens, including influenza viruses, in hospitalized patients who are not immunocompromised if it might influence care (eg, aid in cohorting decisions, reduce testing, or decrease antibiotic use) (B-III).
-
14
Clinicians should not use immunofluorescence assays for influenza virus antigen detection in hospitalized patients except when more sensitive molecular assays are not available (A-II), and follow-up testing with RT-PCR or other molecular assays should be performed to confirm negative immunofluorescence test results (A-III).
-
15
Clinicians should not use RIDTs in hospitalized patients except when more sensitive molecular assays are not available (A-II), and follow-up testing with RT-PCR or other molecular assays should be performed to confirm negative RIDT results (A-II).
-
16
Clinicians should not use viral culture for initial or primary diagnosis of influenza because results will not be available in a timely manner to inform clinical management (A-III), but viral culture can be considered to confirm negative test results from RIDTs and immunofluorescence assays, such as during an institutional outbreak, and to provide isolates for further characterization (C-II).
-
17
Clinicians should not use serologic testing for diagnosis of influenza because results from a single serum specimen cannot be reliably interpreted, and collection of paired (acute/convalescent) sera 2–3 weeks apart are needed for serological testing (A-III).
Table 6.
Influenza Diagnostic Tests for Respiratory Specimens
| Testing Category | Method | Influenza Viruses Detected | Distinguishes Influenza A Virus Subtypes | Time to Results | Performance |
|---|---|---|---|---|---|
| Rapid molecular assay | Nucleic acid amplification | Influenza A or B viral RNA | No | 15–30 minutes | High sensitivity; high specificity |
| Rapid influenza diagnostic test | Antigen detection | Influenza A or B virus antigens | No | 10–15 minutes | Low to moderate sensitivity (higher with analyzer device); high specificity; |
| Direct and indirect immunofluorescence assays | Antigen detection | Influenza A or B virus antigens | No | 1–4 hours | Moderate sensitivity; high specificity |
| Molecular assays (including RT-PCR) | Nucleic acid amplification | Influenza A or B viral RNA | Yes, if subtype primers are used | 1–8 hours | High sensitivity; high specificity |
| Multiplex molecular assays | Nucleic acid amplification | Influenza A or B viral RNA, other viral or bacterial targets (RNA or DNA) | Yes, if subtype primers are used | 1–2 hours | High sensitivity; high specificity |
| Rapid cell culture (shell vial and cell mixtures) | Virus isolation | Influenza A or B virus | Yes | 1–3 days | High sensitivity; high specificity |
| Viral culture (tissue cell culture) | Virus isolation | Influenza A or B virus | Yes | 3–10 days | High sensitivity; high specificity |
Negative results may not rule out influenza. Respiratory tract specimens should be collected as close to illness onset as possible for testing. Clinicians should consult the manufacturer’s package insert for the specific test for the approved respiratory specimen(s). Most US Food and Drug Administration (FDA)-cleared influenza diagnostic tests are approved for upper respiratory tract specimens but not for sputum or lower respiratory tract specimens. Specificities are generally high (>90%) for all tests compared to RT-PCR. FDA-cleared rapid influenza diagnostic tests are Clinical Laboratory Improvement Amendments (CLIA)-waived; most FDA-cleared rapid influenza molecular assays are CLIA-waived, depending on the specimen.
Abbreviation: RT-PCR, reverse-transcription polymerase chain reaction.
TREATMENT
Which Patients With Suspected or Confirmed Influenza Should Be Treated With Antivirals?
Recommendations
-
18Clinicians should start antiviral treatment as soon as possible for adults and children with documented or suspected influenza, irrespective of influenza vaccination history, who meet the following criteria:
- Persons of any age who are hospitalized with influenza, regardless of illness duration prior to hospitalization (A-II).
- Outpatients of any age with severe or progressive illness, regardless of illness duration (A-III).
- Outpatients who are at high risk of complications from influenza, including those with chronic medical conditions and immunocompromised patients (A-II).
- Children younger than 2 years and adults ≥65 years (A-III).
- Pregnant women and those within 2 weeks postpartum (A-III).
-
19Clinicians can consider antiviral treatment for adults and children who are not at high risk of influenza complications, with documented or suspected influenza, irrespective of influenza vaccination history, who are either:
- Outpatients with illness onset ≤2 days before presentation (C-I).
- Symptomatic outpatients who are household contacts of persons who are at high risk of developing complications from influenza, particularly those who are severely immunocompromised (C-III).
- Symptomatic healthcare providers who care for patients who are at high risk of developing complications from influenza, particularly those who are severely immunocompromised (C-III).
For Patients Who Are Recommended to Receive Antiviral Treatment for Suspected or Confirmed Influenza, Which Antiviral Should Be Prescribed, at What Dosing, and for What Duration?
Recommendations
-
20
Clinicians should start antiviral treatment as soon as possible with a single neuraminidase inhibitor (NAI) (either oral oseltamivir, inhaled zanamivir, or intravenous peramivir) and not use a combination of NAIs (A-1).
-
21
Clinicians should not routinely use higher doses of US Food and Drug Administration-approved NAI drugs for the treatment of seasonal influenza (A-II).
-
22
Clinicians should treat uncomplicated influenza in otherwise healthy ambulatory patients for 5 days with oral oseltamivir or inhaled zanamivir, or a single dose of intravenous peramivir (A-1).
-
23
Clinicians can consider longer duration of antiviral treatment for patients with a documented or suspected immunocompromising condition or patients requiring hospitalization for severe lower respiratory tract disease (especially pneumonia or acute respiratory distress syndrome [ARDS]), as influenza viral replication is often protracted (C-III).
In a Patient With Suspected or Confirmed Influenza, When Should Bacterial Coinfection of the Upper or Lower Respiratory Tract Be Considered, Investigated, and Treated?
Recommendations
-
24
Clinicians should investigate and empirically treat bacterial coinfection in patients with suspected or laboratory-confirmed influenza who present initially with severe disease (extensive pneumonia, respiratory failure, hypotension, and fever), in addition to antiviral treatment for influenza (A-II).
-
25
Clinicians should investigate and empirically treat bacterial coinfection in patients who deteriorate after initial improvement, particularly in those treated with antivirals (A-III).
-
26
Clinicians can consider investigating bacterial coinfection in patients who fail to improve after 3–5 days of antiviral treatment (C-III).
If a Patient With Influenza Does Not Demonstrate Clinical Improvement With Antiviral Treatment or Demonstrates Clinical Deterioration During or After Treatment, What Additional Testing and Therapy Should Be Considered?
Recommendation
-
27
Clinicians should investigate other causes besides influenza virus infection in influenza patients who fail to improve or deteriorate despite antiviral treatment (A-III).
When Should Testing Be Done for Infection With an Antiviral-resistant Influenza Virus?
Recommendations
-
28Influenza NAI resistance testing can be considered for:
- Patients who develop laboratory-confirmed influenza while on or immediately after NAI chemoprophylaxis (C-III).
- Patients with an immunocompromising condition and evidence of persistent influenza viral replication (eg, after 7–10 days, demonstrated by persistently positive RT-PCR or viral culture results) and remain ill during or after NAI treatment (B-III).
- Patients with laboratory-confirmed influenza who inadvertently received subtherapeutic NAI dosing (C-III).
- Patients with severe influenza who do not improve with NAI treatment and have evidence of persistent influenza viral replication (eg, after 7–10 days) (C-II).
-
29
Clinicians should remain informed on current CDC and World Health Organization surveillance data on the frequency and geographic distribution of NAI-resistant influenza viruses during influenza season, and with the latest CDC antiviral treatment recommendations (A-III).
Should Adjunctive Therapy Be Administered to Patients With Suspected or Confirmed Influenza?
Recommendations
-
30
Clinicians should not administer corticosteroid adjunctive therapy for the treatment of adults or children with suspected or confirmed seasonal influenza, influenza-associated pneumonia, respiratory failure, or ARDS, unless clinically indicated for other reasons (A-III).
-
31
Clinicians should not routinely administer immunomodulation using immunoglobulin preparations such as intravenous immunoglobulin for treatment of adults or children with suspected or confirmed seasonal influenza (A-III).
ANTIVIRAL CHEMOPROPHYLAXIS IN COMMUNITY SETTINGS
Who Should Be Considered for Antiviral Chemoprophylaxis to Prevent Influenza in the Absence of Exposure or an Institutional Outbreak (Preexposure Chemoprophylaxis)?
Recommendations
Antiviral drugs should not be used for routine or widespread chemoprophylaxis outside of institutional outbreaks; antiviral chemoprophylaxis can be considered in certain situations:
-
32
Clinicians can consider antiviral chemoprophylaxis for the duration of the influenza season for adults and children aged ≥3 months who are at very high risk of developing complications from influenza and for whom influenza vaccination is contraindicated, unavailable, or expected to have low effectiveness (eg, persons who are severely immunocompromised) (C-II).
-
33
Clinicians can consider antiviral chemoprophylaxis for the duration of the influenza season for adults and children aged ≥3 months who have the highest risk of influenza-associated complications, such as recipients of hematopoietic stem cell transplant in the first 6–12 months posttransplant and lung transplant recipients (B-II).
-
34
Clinicians can consider short-term antiviral chemoprophylaxis in conjunction with prompt administration of inactivated influenza vaccine for unvaccinated adults and children aged ≥3 months who are at high risk of developing complications from influenza in whom influenza vaccination is expected to be effective (but not yet administered) when influenza activity has been detected in the community (C-II).
-
35
Clinicians can consider short-term antiviral chemoprophylaxis for unvaccinated adults, including healthcare personnel, and for children aged ≥3 months who are in close contact with persons at high risk of developing influenza complications during periods of influenza activity when influenza vaccination is contraindicated or unavailable and these high-risk persons are unable to take antiviral chemoprophylaxis (C-III).
-
36
Clinicians can consider educating patients and parents of patients to arrange for early empiric initiation of antiviral treatment as an alternative to antiviral chemoprophylaxis (C-III).
Which Antiviral Drugs Should Be Used for Preexposure Chemoprophylaxis for Influenza?
Recommendation
-
37
Clinicians should use an NAI (oral oseltamivir or inhaled zanamivir) if preexposure chemoprophylaxis for influenza is administered rather than an adamantane antiviral (A-II).
What Is the Duration of Preexposure Antiviral Chemoprophylaxis to Prevent Influenza?
Recommendations
-
38
Clinicians should administer preexposure antiviral chemoprophylaxis for adults and children aged ≥3 months who are at very high risk of developing complications from influenza (eg, severely immunocompromised persons such as hematopoietic stem cell transplant recipients) for whom influenza vaccination is contraindicated, unavailable, or expected to have low effectiveness, as soon as influenza activity is detected in the community and continued for the duration of community influenza activity (A-II).
-
39
Clinicians should test for influenza and switch to antiviral treatment dosing in persons receiving preexposure antiviral chemoprophylaxis who become symptomatic, preferably with an antiviral drug with a different resistance profile if not contraindicated (A-II).
Which Asymptomatic Persons Exposed to Influenza Should Be Considered for Postexposure Antiviral Chemoprophylaxis in a Noninstitutional Setting?
Recommendations
-
40
Clinicians can consider postexposure antiviral chemoprophylaxis for asymptomatic adults and children aged ≥3 months who are at very high risk of developing complications from influenza (eg, severely immunocompromised persons) and for whom influenza vaccination is contraindicated, unavailable, or expected to have low effectiveness, after household exposure to influenza (C-II).
-
41
Clinicians can consider postexposure antiviral chemoprophylaxis (in conjunction with influenza vaccination) for adults and children aged ≥3 months who are unvaccinated and are household contacts of a person at very high risk of complications from influenza (eg, severely immunocompromised persons), after exposure to influenza (C-II).
-
42
Clinicians can consider educating patients and arranging for early empiric initiation of antiviral treatment as an alternative to postexposure antiviral chemoprophylaxis (C-III).
When Should Postexposure Antiviral Chemoprophylaxis Be Started?
Recommendations
-
43
If chemoprophylaxis is given, clinicians should administer postexposure antiviral chemoprophylaxis as soon as possible after exposure, ideally no later than 48 hours after exposure (A-III).
-
44
Clinicians should not administer once-daily postexposure anti-viral chemoprophylaxis if >48 hours has elapsed since exposure. Full-dose empiric antiviral treatment should be initiated as soon as symptoms occur, if treatment is indicated (A-III).
How Long Should Postexposure Antiviral Chemoprophylaxis Be Given?
Recommendations
-
45
Clinicians should administer postexposure antiviral chemoprophylaxis in a nonoutbreak setting for 7 days after the most recent exposure to a close contact with influenza (A-III).
-
46
Clinicians should test for influenza and switch to antiviral treatment dosing in persons receiving postexposure antiviral chemoprophylaxis who become symptomatic, preferably with an antiviral drug with a different resistance profile if not contraindicated (A-III).
Which Antiviral Drugs Should Be Used for Postexposure Chemoprophylaxis?
Recommendation
-
47
Clinicians should administer an NAI (inhaled zanamivir or oral oseltamivir) if postexposure chemoprophylaxis for influenza is given, rather than an adamantane antiviral (A-II).
INSTITUTIONAL OUTBREAK CONTROL
When Is There Sufficient Evidence of an Influenza Outbreak in a Long-term Care Facility or Hospital to Trigger Implementation of Control Measures Among Exposed Residents or Patients and Healthcare Personnel to Prevent Additional Cases of Influenza?
Recommendations
-
48
Active surveillance for additional cases should be implemented as soon as possible when one healthcare-associated laboratory-confirmed influenza case is identified in a hospital or one case of laboratory-confirmed influenza is identified in a long-term care facility (A-III).
-
49
Outbreak control measures should be implemented as soon as possible, including antiviral chemoprophylaxis of residents/patients, and active surveillance for new cases, when 2 cases of healthcare-associated laboratory-confirmed influenza are identified within 72 hours of each other in residents or patients of the same ward or unit (A-III).
-
50
Implementation of outbreak control measures can be considered as soon as possible if one or more residents or patients has suspected healthcare-associated influenza and results of influenza molecular testing are not available on the day of specimen collection (B-III).
Which Residents/Patients Should Be Considered to Have Influenza and Be Treated With Antivirals During an Influenza Outbreak in a Long-term Care Facility or Hospital?
Recommendations
-
51
When an influenza outbreak has been identified in a long-term care facility or hospital, influenza testing should be done for any resident/patient with one or more acute respiratory symptoms, with or without fever, or any of the following without respiratory symptoms: temperature elevation or reduction, or behavioral change (A-III).
-
52
Empiric antiviral treatment should be administered as soon as possible to any resident or patient with suspected influenza during an influenza outbreak without waiting for the results of influenza diagnostic testing (A-III).
To Control an Influenza Outbreak in a Long-term Care Facility or Hospital, Should Antiviral Chemoprophylaxis Be Administered to Exposed Residents/Patients?
Recommendation
-
53
Antiviral chemoprophylaxis should be administered as soon as possible to all exposed residents or patients who do not have suspected or laboratory-confirmed influenza regardless of influenza vaccination history, in addition to implementa]tion of all other recommended influenza outbreak control measures, when an influenza outbreak has been identified in a long-term care facility or hospital (A-III).
During an Influenza Outbreak at a Long-term Care Facility, Should Antiviral Chemoprophylaxis Be Administered to Residents Only on Affected Units or to All Residents in the Facility?
Recommendation
-
54
Antiviral chemoprophylaxis should be administered to residents on outbreak-affected units, in addition to implementing active daily surveillance for new influenza cases throughout the facility (A-II).
Which Healthcare Personnel Should Receive Antiviral Chemoprophylaxis During an Institutional Outbreak?
Recommendations
-
55
Clinicians can consider antiviral chemoprophylaxis for unvaccinated staff, including those for whom chemoprophylaxis may be indicated based upon underlying conditions of the staff or their household members (see recommendations 40–44) for the duration of the outbreak (C-III).
-
56
Clinicians can consider antiviral chemoprophylaxis for staff who receive inactivated influenza vaccine during an institutional influenza outbreak for 14 days postvaccination (C-III).
-
57
Clinicians can consider antiviral chemoprophylaxis for staff regardless of influenza vaccination status to reduce the risk of short staffing in facilities and wards where clinical staff are limited and to reduce staff reluctance to care for patients with suspected influenza (C-III).
How Long Should Antiviral Chemoprophylaxis Be Given to Residents During an Influenza Outbreak in a Long-term Care Facility?
Recommendation
-
58
Clinicians should administer antiviral chemoprophylaxis for 14 days and continue for at least 7 days after the onset of symptoms in the last case identified during an institutional influenza outbreak (A-III).
INTRODUCTION
These clinical practice guidelines are an update of the guidelines published by the Infectious Diseases Society of America (IDSA) in 2009 [17], just prior to the recognition of the emergence of influenza A(H1N1) pdm09 virus as the cause of the 2009 H1N1 pandemic. Since then, new rapid molecular diagnostic assays became available, new risk factors for severe disease were recognized, and a parenteral neuraminidase inhibitor (NAI), peramivir, was approved for use in the United States. In addition, many observational studies in hospitalized patients with seasonal influenza A or B virus infection have been conducted, including studies of influenza A(H1N1) pdm09 virus infections, that have addressed the effectiveness of antiviral treatment and adjunctive therapies. Additional information is also available about the emergence of antiviral resistance. However, only a small proportion of the new data arises from randomized controlled clinical trials.
The purpose of this guideline’s recommendations is to provide clinicians with evidence-based recommendations for the diagnosis and treatment of seasonal influenza, including use of commercially available influenza diagnostic tests, use of approved antiviral agents for treatment and chemoprophylaxis of influenza, and use of antibiotics or other adjunctive measures for treatment of complications associated with influenza. The recommendations also address the use of diagnostic tests and antiviral agents for the control of institutional influenza outbreaks. The care of specific patient populations is addressed, including children, pregnant and postpartum women, and persons who are severely immunocompromised such as hematopoietic stem cell and solid organ transplant recipients. The target audience includes primary care clinicians, obstetricians, emergency medicine providers, hospitalists, and infectious disease specialists.
The guidelines do not provide recommendations on infection prevention and control (IPC) measures for seasonal influenza in all healthcare settings; these are available on the Centers for Disease Control and Prevention (CDC) website [18]. Influenza outbreaks outside of healthcare settings (eg, daycare, schools, and workplaces) are not addressed; public health authorities should be consulted for outbreaks in these settings. The guidelines do not provide recommendations on diagnosis or treatment of human infections with novel influenza A viruses of animal origin following exposure to poultry or pigs (eg, avian influenza A viruses, or swine-origin [variant] viruses); current recommendations for IPC, specimen collection, diagnosis, and treatment of novel influenza A virus infections are available on the CDC website [19, 20]. The guideline also does not provide specific recommendations for the supportive clinical management of critical illness resulting from complications of influenza virus infection. Influenza vaccination is not addressed because annual influenza vaccination recommendations are published by the Advisory Committee on Immunization Practices (available on the CDC website and published in the Morbidity and Mortality Weekly Report) and the Committee on Infectious Diseases of the American Academy of Pediatrics.
METHODOLOGY
Guidelines Panel Composition
For this update, the IDSA chose 2 co-chairs to lead the process and convened a multidisciplinary panel of 16 experts in infectious diseases and the management of patients with influenza. In addition, the Pediatric Infectious Diseases Society, the American Academy of Pediatrics, the American College of Emergency Physicians, the Society for Healthcare Epidemiology of America, and the American College of Obstetricians and Gynecologists provided representatives with specific expertise in pediatrics, emergency medicine, healthcare epidemiology, and obstetrics and gynecology.
Disclosure and Management of Potential Conflicts of Interest
All prospective panelists were required to disclose any actual, potential, or perceived conflicts of interest (COI) prior to inclusion in the panel. The disclosures were used to categorize the panelists as (i) cleared for full participation, (ii) allowed to participate with recusal from certain aspects of guidelines development, or (iii) disqualified from participation. The co-chairs remained free of any financial COI during the entire guidelines development process, which meant avoidance of any relationship with pharmaceutical or device companies with products in development or being marketed for influenza or pneumonia. Furthermore, all panelists were precluded from participating in any marketing-related activities (eg, lectures or advisory boards directly funded by a pharmaceutical or device company with interests related to the guideline subject[s]). Panelists were required to disclose to the IDSA and the chairs any new activities that had the potential to be viewed as a COI prior to engaging in the activity. Assignments of panelists to specific clinical questions were made as to minimize any COI concerns. At the beginning of each meeting, whether face-to-face or by telecom-ference, panelists were required to disclose any new potential COI or prior relevant COI to the subject matter to be discussed.
Clinical Questions and Evidence Review
Following approval by the IDSAs Standards and Practice Guideline Committee (SPGC), an initial list of clinical questions was developed by the panel based on the 2009 guidelines and clinical problems requiring guidance. The panel committee prioritized the clinical questions and divided them into subgroups based on diagnostics, treatment, and prevention and control. Each of these subgroups was addressed by its dedicated subcommittee.
Two health science librarians designed literature searches to address each of the questions. Searches were limited to studies performed between January 2009 and March 2014 and published in English. Databases searched included PubMed/Medline, Embase, and the Cochrane Database for Systematic Reviews. The searches focused on human studies and, while not an exhaustive list, included such search terms as “influenza” or “influenza and virus,” “influenza and infection,” “influenza and treatment,” “influenza and prophylaxis,” “influenza and chemoprophylaxis,” and “influenza and outbreak.” A subsequent literature search was developed and updated through July 2017. To supplement the librarians’ electronic searches, panelists also contacted experts and conducted updated literature searches, examined reviews of conference proceedings, manually checked reference lists, and examined regulatory agency websites for relevant articles published through January 2018. While the optimal “gold standard” randomized controlled trial evidence was often not available, the aim was to ensure that the guidelines panel considered the most up-to-date evidence to address the clinical questions within its scope. For both the initial and the updated evidence search, the titles and abstracts of identified citations were screened, and potentially relevant citations were subjected to a full-text review, using predefined inclusion and exclusion criteria. Where necessary, screening of retrieved articles was conducted in duplicate and independently. Panel judgments were made throughout the guidelines based on consensus.
Development of Clinical Recommendations
Formal evidence summaries for specific treatment and chemoprophylaxis questions were prepared by the panel members. The current guideline development process included a systematic weighting of the quality of the evidence and the grade of recommendations based upon the US Public Health Service Grading System (Table 1) for ranking recommendations in clinical guidelines as utilized in the previous 2009 guidelines [17]. The adopted grading system as per Table 1 ranged from the optimal category and grade for a recommendation of “A-I” (which meant that the panel judged that there was good evidence to support a recommendation for [should always be offered] or against [should never be offered] use, and evidence emerged from >1 properly conducted randomized controlled trial) to the lowest category and grade, which was “C-III” (meaning that there was poor evidence to support a recommendation and the judgment was based on evidence from opinions of respected authorities, as well as based on clinical experience, descriptive studies, or reports of expert committees). The summaries of study evidence were discussed and reviewed by panel committee members, and judgments were made based on the emerging evidence coupled to clinical expertise and experience. The analyses were completed in parallel with drafting of updated recommendations. Once the analyses were completed, recommendations were reviewed and revised as appropriate by the panel.
The panel had 4 face-to-face meetings and conducted teleconferences over 5 years. All members of the panel participated in the preparation of the guidelines and approved the final recommendations. Feedback was obtained from external peer reviewers. The Pediatric Infectious Diseases Society, the Society for Healthcare Epidemiology of America, and the American College of Obstetricians and Gynecologists reviewed and endorsed the guideline. The IDSA SPGC and the IDSA Board of Directors reviewed and approved the guidelines prior to dissemination.
Revision Dates
At annual intervals, the SPGC will determine the need for revisions to the guideline based on an examination of current literature evidence and the likelihood that any new data will have an impact on the recommendations. If necessary, the entire expert panel will be reconvened to discuss potential changes. Any revision to the guideline will be submitted for review and approval to the IDSA SPGC and Board of Directors.
BACKGROUND
Definitions
“Influenza season” refers to the surveillance period when influenza activity typically occurs, such as during October through May, in the United States. “Influenza activity” is defined as the circulation of seasonal influenza A and B viruses among persons in the local community. “High influenza activity” is defined as increased circulation of seasonal influenza A and B viruses, such as peak weeks of circulation of seasonal influenza A and B viruses during the colder fall, winter, and spring months in the United States. “Low influenza activity” is defined as low or lack of circulation of seasonal influenza A and B viruses, such as during the warm summer months in the United States. “Acute respiratory illness” is defined as infection of either the upper or lower respiratory tract with respiratory symptoms, with or without fever. “Influenza-like illness” (ILI) is defined as acute respiratory illness with fever and either cough or sore throat. “Influenza” refers to symptomatic illness caused by seasonal influenza A or B virus infection. “Respiratory distress” is defined as difficulty in breathing that is usually associated with an increased respiratory rate and use of accessory muscles of breathing. “Laboratory-confirmed influenza” is defined as acute respiratory illness with laboratory testing evidence of influenza virus infection.
Scope
The scope of the guidelines pertains to diagnostic testing and treatment of illness caused by infection with influenza A and B viruses circulating among humans during seasonal epidemics and does not address asymptomatic infections. The guidelines also address diagnostic testing and use of antivirals for management of institutional influenza outbreaks. Background information about signs and symptoms of influenza, complications, groups considered to be at high risk of complications, and influenza tests are included in the next section. The guidelines do not address sporadic infections with influenza C virus, and do not address sporadic human infections with novel influenza A viruses of animal origin.
Seasonal Influenza Background Information
Influenza is caused by infection of the respiratory tract with influenza A, B, or C viruses. Seasonal epidemics of influenza A and B viruses occur each fall, winter, and spring in the United States, while influenza C virus infections occur sporadically. Seasonal influenza A or B virus infections can cause a wide range of manifestations, from asymptomatic infection, uncomplicated illness with or without fever (Table 2), to complications that may result in severe disease (Table 3). One study estimated that during 2010–2016, the seasonal incidence of symptomatic influenza among all ages in the United States was approximately 8% and varied from 3% to 11% [1]. Most people recover from influenza without sequelae, but some persons are considered to be at increased risk for severe and fatal influenza, including children aged <5 years (but especially <2 years), adults aged ≥65 years, pregnant and postpartum women, people with certain chronic medical conditions including pulmonary, cardiac, and metabolic disease, people with immunosuppression, people with extreme obesity, residents of nursing homes, and American Indians and Alaska Natives [2–8] (Table 4). Elderly persons have the highest mortality rates attributable to influenza [8]. Among the high-risk groups, persons considered to be at very high risk of complications from influenza include those who are severely immunocompromised (eg, hematopoietic stem cell transplant [HSCT] recipients).
Table 2.
Signs and Symptoms of Uncomplicated Influenzaa
| General | Head, Eyes, Ears, Nose, Throat | Neuromuscular | Gastrointestinalb | Pulmonary |
|---|---|---|---|---|
| Feverc,d | Headache | Myalgia, arthralgia | Abdominal pain | Nonproductive cough |
| Chills | Nasal congestiond | Weakness | Vomiting | Pleuritic chest pain |
| Malaise | Rhinorrhead | Chest pain | Diarrhead | |
| Fatigue | Sore throat/hoarseness |
Adapted from Jani AA, Uyeki TM. Chapter 46. Influenza. In: Emergency management of infectious diseases. 2nd ed. Chin RL, ed. Cambridge, UK: Cambridge University Press, 2018.
Abrupt onset of respiratory and systematic signs and symptoms, with or without fever.
Gastrointestinal symptoms vary with age: Diarrhea is more common among infants, young children, and school-aged children; abdominal pain may be present among school-aged children; vomiting may be present among adults.
Fever can be age-specific: High fever or fever alone may be the only sign in infants and young children; fever may be absent or low grade in infants and the elderly.
Fever, nasal congestion, rhinorrhea, and diarrhea may be present among infants and young children.
Table 4.
Persons Who Are at High Risk of Complications From Influenza
| Persons at High Risk of Complications |
| Children aged <5 years, and especially aged <2 years |
| Adults aged >65 years |
| Persons with chronic pulmonary (including asthma), cardiovascular (except hypertension alone), renal, hepatic, hematologic (including sickle cell disease), or metabolic disorders (including diabetes mellitus) or neurologic and neurodevelopment conditions (including disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability [mental retardation], moderate to severe developmental delay, muscular dystrophy, or spinal cord injury) |
| Persons with immunosuppression, including that caused by medications or by HIV infectiona |
| Women who are pregnant or postpartum (within 2 weeks after delivery) |
| Children and adolescents through 18 years who are receiving aspirin- or salicylate-containing medications and who might be at risk for experiencing Reye syndrome after influenza virus infection |
| American Indian/Alaska Native peopleb |
| Persons with extreme obesity (ie, body mass index ≥40 kg/m2) |
| Residents of nursing homes and other chronic care facilities |
Adapted from Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2017–18 influenza season. MMWR Recomm Rep 2017; 66:1–20.
Abbreviation: HIV, human immunodeficiency virus.
Persons with the highest risk for complications are those who are severely immunocompromised (eg, hematopoietic stem cell transplant recipients).
American Indian/Alaska Native persons are included because of their documented higher rates of influenza-related mortality. Also, 30% of fatal American Indian/Alaska Native influenza cases would not have been classified as high risk during the 2009 H1N1 pandemic using other criteria. MMWR 2009; 58:1341–44.
During the 2010–2016 influenza seasons, seasonal influenza epidemics were associated with an estimated 4.3–16.7 million medical visits, 140 000–710 000 hospitalizations, and 12 000–56 000 respiratory and circulatory deaths each year in the United States [9]. A recent modeling study estimated a range of 291 243–645 832 seasonal influenza-associated respiratory deaths occurring annually worldwide [10]. Substantial practice variation exists in the diagnosis and treatment of influenza [21–23]. Appropriate diagnosis of influenza and timely use of antiviral medications may decrease unnecessary testing for other etiologies and associated empiric antibiotic use [11, 12], duration of symptoms, hospitalization, the need for critical care, and mortality [13–16].
Influenza vaccine effectiveness varies by age, host immune status, and the match between circulating and vaccine virus strains [24]. Because influenza vaccine effectiveness is widely variable, ranging from very low to approximately 40%−60% in well-matched seasons (https://www.cdc.gov/flu/professionals/vaccination/effec-tiveness-studies.htm) [25], a history of current season influenza vaccination does not exclude a diagnosis of influenza.
Typical signs and symptoms of uncomplicated influenza are listed in Table 2. However, atypical presentations of influenza virus infection, with or without fever, should also be considered along with the patient’s underlying health and immune function (eg, fever without source in infants; new-onset neurologic signs and symptoms [seizures, altered mental status], more commonly in infants and young children, but possible in adults; new-onset cardiovascular events [heart failure, myocardial infarction or ischemia, cerebrovascular accident] in adults; and exacerbation of chronic medical conditions, with or with-out fever [particularly cardiac, pulmonary, or neurologic disease], more commonly in adults than in children) (Table 5). Influenza should also be considered in children and adults with pneumonia, and those with severe, complicated, or progressive (worsening) acute respiratory illness, but with no documented alternative diagnosis, and those with an epidemiological link to case(s) of influenza or an influenza outbreak year-round (Table 5).
Table 5.
Groups in Whom to Consider a Diagnosis Of Influenzaa
| When to Consider a Diagnosis of Influenza | Symptom and Group |
|---|---|
| During influenza activity | Acute onset of respiratory symptoms, with or without fever (all ages) |
| • Pneumonia (all ages) | |
| • Acute exacerbation of underlying chronic lung disease (eg, chronic obstructive pulmonary disease, asthma), with or without fever (all ages) | |
| • Fever without an obvious source (infants, young children) | |
| • New-onset neurologic signs and symptoms (eg, seizures, altered mental status), with or without fever (infants, young children) | |
| • Exacerbation or new onset of cardiovascular events (eg, heart failure, myocardial infarction or ischemia, cerebrovascular accident in adults) or altered mental status, with or without fever (all ages) | |
| • Severe, complicated, or progressive (worsening) acute respiratory illness, without an alternative diagnosis (all ages) | |
| • Hospitalized patients who develop new onset of acute respiratory symptoms, with or without fever (all ages) | |
| Year-round | Acute onset of respiratory symptoms, with or without fever, especially those at high risk for influenza complications who are epidemiologically linked to recent influenza cases or outbreaks (all ages) |
| • Healthcare personnel caring for influenza patients | |
| • Healthcare personnel, residents, or visitors to an institution experiencing an influenza outbreak | |
| • Close contacts of persons with suspected influenza (household or a congregate setting, such as daycare, school, or healthcare facility) | |
| • Travelers who returned recently from areas where influenza viruses may be circulating | |
| • Organized tour group participants | |
| • Participants in international mass gatherings | |
| • Summer camp attendees | |
| • Cruise or military ship passengers |
A diagnosis of influenza should be considered regardless of current season influenza vaccination because influenza vaccine effectiveness is variable.
Influenza is associated with a variety of signs and symptoms that may vary by age, underlying chronic disease, complications, host immune status, and influenza virus type or influenza A virus subtype. Abrupt onset of fever with cough is most predictive of uncomplicated influenza in adult outpatients, with a sensitivity of >70% during the influenza season [26–29]. A retrospective, cross-sectional study in a single urban US emergency department found that the best predictive model for identifying influenza for all ages consisted of cough (diagnostic odds ratio [DOR], 5.87), fever (DOR, 4.49), rhinorrhea (DOR, 1.98), and myalgias (DOR, 1.44) [30]. In a prospective systematic sampling study, fever (temperature ≥38°C) and cough were significantly associated with reverse-transcription polymerase chain reaction (RT-PCR)-confirmed influenza [29]. A prospective study of adults aged 28–50 years across 2 influenza seasons in Taiwan reported that fever and cough had the best sensitivity (86%), while fever, cough, and sneezing had the best specificity (77%) for influenza [31].
While the abrupt onset of fever with cough is a good indicator of influenza, signs and symptoms may vary for patients with different underlying conditions. In a retrospective study of clinical predictors of influenza in hospitalized patients, fever with cough or sore throat had a sensitivity of 43% for patients without asthma, and only 21% for asthmatic patients [32]. A prospective study of >500 influenza patients in North Carolina reported that emergency department patients commonly reported cough, nasal congestion, fever, fatigue/malaise, headache, poor appetite, sore throat, and myalgias/muscle aches, whereas hospitalized patients reported shortness of breath and wheezing [33].
Infants and young children with influenza may not always have fever and may present with a wide range of signs and symptoms [34], making an influenza diagnosis more difficult [29]. Infants and young children may present with fever and suspected sepsis [35, 36]. Diarrhea can occur in up to 28% of infants and young children with influenza [37–39]. A prospective study found that fever >38°C, chills, headache, malaise, and sore eyes were significantly associated with a positive RT-PCR test result for influenza virus in children younger than 15 years [29]. Fever (≥38°C), headache, cough, and absence of abnormal breathing sounds in pediatric patients had a positive predictive value of 57.1% [29]. In a retrospective, cross-sectional study, adding rhinorrhea to the fever and cough case definition achieved a better balance between sensitivity (85%) and specificity (47%) among children aged <5 years [30]. In another prospective study among pediatric outpatients aged ≤13 years with respiratory infections, fever was the only reliable predictor of culture-confirmed influenza virus infection [40].
Influenza is an important cause of community-acquired pneumonia in adults [41]. Invasive bacterial coinfection may occur (with Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes [group A streptococci], and others) [42–45]. Secondary bacterial pneumonia due to methicillin-resistant S. aureus (MRSA) is becoming more prevalent and has been a more common finding in recent pediatric influenza-associated deaths [42, 46–48].
Influenza virus infection of the respiratory tract can result in severe nonpulmonary complications (eg, myocarditis [42, 49], rhabdomyolysis [50–61], encephalitis [53–57], and hypovolemic shock with hyperthermia or hypothermia [46, 58–62]). Myocarditis and encephalitis were the most frequently described extrapulmonary complications associated with influenza in adults in a recent comprehensive review [63]. Exacerbation of chronic disease (eg, coronary artery disease, chronic pulmonary disease, asthma, heart failure) with influenza virus infection can result in severe illness [49, 63–69]. Influenza can trigger acute myocardial infarction [70].
Elderly persons with influenza may present without fever and milder systemic symptoms than younger patients, but with higher frequencies of altered mental status [71–75]. Data from a prospective surveillance study indicated that in patients aged ≥65 years hospitalized with acute cardiopulmonary illnesses, the clinical symptoms of cough and/or sore throat combined with a lowered oral temperature threshold (≥37.3°C or 99.0°F) increased sensitivity and specificity of influenza diagnosis [76]. Another prospective study found that cough (odds ratio [OR], 6.4; 95% confidence interval [CI], 3.2–13.0) and feverishness and/or triage temperature ≥37.2°C (OR, 3.0; 95% CI, 2.0–4.7) were most predictive of influenza among adults aged ≥60 years in the emergency departments of 6 hospitals [77].
Immunocompromised patients may also present without typical findings of influenza. In a study of adult transplant patients, the CDC criteria of ILI, defined as fever and either cough or sore throat, were poorly predictive of RT-PCR-positive cases [78]. In a report of an influenza outbreak in an ambulatory stem cell transplant center, only 7% had signs and symptoms that met the CDC ILI definition; only a minority had fever [79].
Nosocomial acquisition of influenza is a consideration in persons who experience an onset of fever 48 hours or more after hospital admission during the influenza season [80–84]. However, any hospitalized patient may be in the incubation period for influenza virus infection when admitted and become symptomatic during the first few days of hospitalization for other illnesses or injuries. During influenza season, even in the absence of fever, the presence of new onset or worsening or unexplained cough in a hospitalized patient should prompt testing for influenza [32].
In a 2015 prospective study among 504 hospitalized or emergency department patients with laboratory-confirmed influenza, only 29% were clinically diagnosed with influenza [33]. Certain factors made an influenza diagnosis more likely, including having a high-risk condition, being in an inpatient setting, and not having a bacterial infection diagnosis. In the same study of laboratory-confirmed influenza patients, receiving a diagnosis of bacterial infection decreased the likelihood of an influenza diagnosis by 3-fold [33].
During low influenza activity (eg, summer months in the United States), a diagnosis of influenza should be considered for ill international travelers or their ill contacts [85–88] because influenza viruses circulate year-round among persons living in the tropics and during winter periods in temperate climates of the Southern Hemisphere [89, 90]. In addition, influenza should be considered in persons with acute febrile respiratory symptoms who have recently spent time in settings linked to an influenza outbreak. These may include organized tour groups [91], international mass gatherings [92–94], summer camps [95, 96], cruise ships [87, 91, 97–101], and military ships [102].
Clinicians should consider novel influenza A virus infection in the differential diagnosis in travelers who have recently returned from countries affected by poultry outbreaks of avian influenza and who have febrile respiratory symptoms and a recent history of direct or close exposure to poultry (well-appearing, sick or dead birds, or visiting a live poultry market [103, 104]). If novel influenza A virus infection is suspected, clinicians should seek prompt consultation with the local and state health departments for possible testing for novel influenza A virus infection, with laboratory confirmation at the CDC. Updated information on avian influenza is available at the CDC’s avian influenza website [19] and the World Health Organization’s (WHO) avian influenza website [105]. Novel influenza A virus infection should also be suspected in persons with febrile respiratory illness and a history of recent direct or close contact with pigs, such as at animal exhibits at agricultural fairs [106, 107]. Swine influenza A viruses are endemic among pigs worldwide, including the United States. Human infection with swine influenza A viruses is referred to as “variant virus infection.” Updated information on variant influenza virus infections is available at the CDC’s variant influenza viruses website [20].
Influenza testing should be performed when the results are anticipated to influence clinical management (impact decision to initiate antiviral therapy, other diagnostic testing, antibiotic use, or IPC measures) or public health response (eg, outbreak identification and interventions). The decision to test is related to the level of suspicion for influenza, local influenza activity, and the sensitivity and specificity of available influenza tests. The appropriate respiratory tract specimen to collect depends upon the approved specimens for the specific influenza test used, patient acceptability, and disease severity. The choice of influenza test depends upon the clinical setting and test performance (Table 6). Clinicians should be aware of the prevalence of influenza viruses among the patient population being tested to help inform the pretest probability of influenza, understand the limitations of influenza tests, and properly interpret the results, particularly negative results (Table 7). Molecular assays that detect influenza virus nucleic acids have the best performance characteristics. Detection of influenza viruses in respiratory specimens by molecular assays is suggestive, but cannot confirm, that infectious virus is present; only isolation of influenza viruses by viral culture can confirm that viable virus is present. A wide range of influenza tests is available for diagnostic purposes:
Rapid influenza molecular assays are a relatively new kind of highly sensitive molecular point-of-care influenza diagnostic test for rapid (15–30 minutes) detection of influenza A and B viral RNA in respiratory specimens, with higher sensitivity than rapid influenza diagnostic tests (RIDTs) that detect influenza viral antigens.
RT-PCR is a highly sensitive and highly specific testing modality for detection of influenza A and B viral RNA in respiratory specimens, though the results may take 4–6 hours or more once testing is started, and RT-PCR may not be available at all clinical sites. Some of the newer cartridge-based RT-PCR assays can yield results in 60–80 minutes. RT-PCR can be useful as a confirmatory test and identify influenza virus types and influenza A virus subtypes.
Multiplex RT-PCR assays target a panel of microorganisms using multiplex RT-PCR. Multiplex respiratory pathogen panels range from narrow, targeting influenza A and B viral and RSV RNA, to broad, targeting more than a dozen respiratory viruses and other pathogens in respiratory specimens. Turnaround times to results range from 1 to 8 hours. These assays are preferred for immunocompromised patients and may be useful for other hospitalized patients.
Immunofluorescence assays include direct fluorescent anti-body or indirect fluorescent antibody staining for influenza virus antigen detection. They have higher sensitivity than RIDTs, but lower sensitivity and specificity compared with viral isolation in cell culture or RT-PCR. Results are available within 2–4 hours after specimen submission. Performance of these assays depends heavily on laboratory expertise and the quality of the specimen collected (ie, specimens must include respiratory epithelium cells; requires a florescent microscope and an experienced laboratory technician).
RIDTs can identify influenza A and B viral nucleoprotein antigens in respiratory specimens and rapidly (<15 minutes) provide results. Most are approved for bedside and office use. Compared with other types of tests (eg, RT-PCR), RIDTs are significantly less sensitive than other methods (false-negative results are not uncommon). RIDTs that utilize analyzer devices generally have higher sensitivity to detect influenza viral antigens than RIDTs without analyzer devices but have lower sensitivity than rapid molecular assays.
Table 7.
Interpretation of Influenza Testing Results on Respiratory Specimens
| Test and Characteristics | Low Influenza Activitya | High Influenza Activityb | ||
|---|---|---|---|---|
| Rapid influenza diagnostic test (antigen detection: immunoassay or immunofluorescence assay) • Low to moderate sensitivity • High specificity ➢ Should not be used for testing of patients with progressive illness and hospitalized patients |
Negative result NPV is high: ➢ Likely to be a true-negative result if an upper respiratory tract specimen was collected <4 days after illness onset ➢ If epidemiologically linked to an influenza outbreak, consider confirming with molecular assay |
Positive result PPV is low: ➢ Likely to be a false-positive result ➢ Confirm with molecular assay |
Negative result NPV is low: ➢ May be a false-negative result, especially if upper respiratory tract specimen was collected >4 days after illness onset, cannot exclude influenza virus infection ➢ Do not withhold antiviral treatment if clinically indicated ➢ Confirm with molecular assay |
Positive result PPV is high: ➢ Likely to be a true-positive result |
| Molecular assay (nucleic acid detection: rapid molecular assayc, multiplex PCR, RT-PCR) • High sensitivity • Very high specificity ➢ Can be used for both outpatients and hospitalized patients ➢ RT-PCR assays should be used for hospitalized patients |
Negative result NPV is high: ➢ Very likely to be a true-negative result, especially if an upper respiratory tract specimen was collected <4 days after illness onset |
Positive result PPV is low: ➢ False-positive result is possible |
Negative result NPV is low: ➢ May be a true-negative result in a patient without lower respiratory tract disease ➢ Consider potential for a false-negative result, especially if an upper respiratory tract specimen was collected in a hospitalized patient ➢ For hospitalized patients on mechanical ventilation who tested negative on upper respiratory tract specimens, collect lower respiratory tract specimens (endotracheal aspirate, BAL fluid) for testing |
Positive result PPV is high: ➢ Likely to be a true-positive result |
Abbreviations: BAL, bronchoalveolar lavage; NPV, negative predictive value; PCR, polymerase chain reaction; PPV, positive predictive value; RT-PCR, reverse-transcription polymerase chain reaction.
Low influenza activity refers to periods when influenza viruses are not known to be circulating or are only sporadically detected among the patient population being tested, such as during the summer months in the United States.
High influenza activity refers to periods when influenza viruses are known to be circulating among the patient population being tested, such as during the winter months in the United States.
Rapid molecular assays may have lower sensitivity and specificity compared to other molecular assays (eg, RT-PCR).
Additional tests are available and may have utility under certain circumstances (eg, institutional outbreaks), but are generally not useful for clinical diagnostic purposes. These include:
Viral culture of respiratory specimens, using standard cell culture and shell vial culture, can provide specific information regarding circulating strains and subtypes of seasonal influenza A viruses and influenza B virus strains for public health purposes, especially to inform influenza vaccine strain selection, and is important during both low and high influenza activity. However, because results are not available in a timely manner, viral culture cannot inform clinical management of influenza patients, but can confirm negative test results from RIDTs and immunofluorescence assays, such as during an institutional outbreak, and to provide influenza virus isolates for further characterization.
Serologic testing results from a single serum specimen cannot be reliably interpreted, and collection of paired (acute/ convalescent) sera 2–3 weeks apart are needed for serological testing. Therefore, serologic testing cannot inform clinical management of influenza patients, but could be useful for seroepidemiology studies.
Recently, the US Food and Drug Administration (FDA) reclassified RIDTs from class I to class II devices, which requires approved tests to meet higher standards for clinical sensitivity and specificity. Most RIDTs and some rapid molecular assays are Clinical Laboratory Improvement Amendments (CLIA) “waived” tests that can be performed in clinical settings or by any clinical laboratory with a CLIA Certificate of Waiver. As the field of approved influenza diagnostics is dynamic, clinicians should consult the CDC website for information on FDA-cleared tests (https://www.cdc.gov/flu/professionals/diagnosis/index.htm).
To properly interpret test results, clinicians should understand the limitations of diagnostic tests with lower sensitivities to detect influenza viruses (eg, immunofluorescence assays, rapid antigen tests) and influenza activity among the population being tested. Antiviral treatment, when indicated, should not be delayed until the results of diagnostic testing are available for persons at high risk of complications, those with progressive disease, or patients being admitted to hospital. Interpretation of test results depends on multiple factors, including the level of influenza activity in the population being tested, pretest probability, whether influenza viruses are actively replicating or have recently infected the person being tested, the time from illness onset to specimen collection, the source and quality of respiratory specimen(s), the characteristics of a test, and whether proper procedures were used for specimen collection, transport, and testing [108]. Interpretation of test results relies on the positive and negative predictive values of a test, which are influenced primarily by the prevalence of influenza viruses in the population tested and on the sensitivity and specificity of the test to detect influenza virus infection vs a “gold standard” test such as RT-PCR assay results [108, 109]. The sensitivity and specificity of an influenza test are fixed parameters, whereas the prevalence of circulating influenza viruses (level of influenza activity) changes over time with influenza activity (eg, in the United States, high influenza activity can occur during the fall, winter, and spring, whereas low influenza activity occurs during the summer).
Multiple studies have reported that rapid influenza diagnostic tests (antigen detection) have low to moderate sensitivity. One meta-analysis of observational studies of rapid influenza antigen testing of respiratory tract specimens (mostly upper respiratory tract specimens) compared to molecular assays or viral culture reported that rapid influenza antigen tests had moderate sensitivity (62%) and high specificity (98%) among all ages [110]. These studies were predominantly among out-patients with uncomplicated influenza. Sensitivity of rapid influenza antigen tests was lower in adults (approximately 54%) than children (approximately 67%), and lower for detection of influenza B viruses than for influenza A viruses [110]. An updated meta-analysis of observational studies of rapid influenza antigen tests reported pooled sensitivities of 54% and 53% to detect influenza A and influenza B virus antigens, respectively, and pooled specificities of 99%, compared with RT-PCR [111]. Low sensitivity to detect influenza A(H1N1)pdm09 virus was reported for some rapid antigen tests [112]. Other studies reported higher sensitivities for detection of influenza A(H3N2) than for A(H1N1)pdm09 and influenza B viruses compared with RT-PCR [113, 114]. One meta-analysis of observational studies of rapid influenza antigen tests to detect A(H1N1) pdm09 virus reported a sensitivity of 51% and specificity of 98% compared with RT-PCR [115]. One comparative study reported variability in the analytical sensitivity of different rapid influenza antigen tests to detect dilutions of influenza viruses [116]. Use of an analyzer device for rapid influenza diagnostic tests to detect influenza viral antigens (immunoassay or immunofluorescence assay) had moderately high pooled sensitivity (80% and 77%) compared with RT-PCR [111]. Higher sensitivity to detect influenza viruses in respiratory specimens has been reported for one rapid molecular assay (isothermal nucleic acid amplification) than for rapid antigen detection tests [117–119], and a meta-analysis of rapid molecular assays reported pooled sensitivities of 92% and 95% for detection of influenza A and B viruses, respectively, and pooled specificities of 99% [111].
The timing and site of respiratory specimen collection can affect influenza testing results. The sensitivity of influenza screening assays such as rapid diagnostic tests is somewhat higher when respiratory specimens are collected within 48–72 hours of illness onset due to reduction in influenza viral shedding after this period [120]. RT-PCR is more likely to still be positive later in illness. Viral shedding is more prolonged in infants, young children, and immunocompromised patients. Testing of lower respiratory tract specimens by RT-PCR in critically ill patients with respiratory failure can yield higher detection of influenza viruses compared with upper respiratory tract specimens [121, 122].
The high specificity among most influenza screening tests and molecular assays indicates that the frequency of false-positive results is generally very low, especially when influenza activity is high in the patient population tested. The potential for a false-positive result is higher when influenza activity is very low (eg, when influenza viruses are not circulating among the population tested such as during summer months) for a patient without a known influenza epidemiological link (exposure to a person with influenza in areas where influenza activity is high [eg, opposite hemisphere or to tropical/subtropical areas] or to an influenza outbreak). A positive influenza test result in a person without known exposure to influenza during low influenza periods (low positive predictive value) could be a false positive. Collection of additional respiratory specimens for testing of influenza viruses by molecular assays should be considered for outpatients who are at high risk for influenza complications and hospitalized patients with suspected influenza, and antiviral treatment should be started promptly while molecular assay results are pending.
Persons who receive live attenuated influenza virus vaccine for intranasal administration can shed influenza vaccine virus strains in the upper respiratory tract for up to 7 days after intranasal vaccination and can test positive during this period [123–125]. Clinicians should also consider that a positive influenza test result does not exclude bacterial coinfection, and evaluation of the potential need for antibiotics, especially in patients with pneumonia, should be considered.
The choice of an antiviral drug for treatment or chemoprophylaxis should be based on the approved and recommended ages, route of administration, whether contraindications exist for the use of a particular product, and knowledge of antiviral resistance patterns. Antiviral resistance information is available in the weekly CDC influenza surveillance report (https://www.cdc.gov/flu/weekly/index.htm), and the latest information about approved antivirals is available on the CDC website (http://www.cdc.gov/flu/professionals/index.htm).
The risk of influenza-associated complications is not identical among all high-risk persons, and antiviral chemoprophylaxis is likely to have the greatest benefit among those at highest risk of influenza complications and death, particularly if influenza vaccination is contraindicated or not expected to be effective (eg, severely immunocompromised persons). If antiviral chemoprophylaxis is given to close contacts of high-risk persons while awaiting an immune response to influenza vaccination, it should be continued for 2 weeks after vaccination until an immune response is expected (6 weeks for children aged 6 months to <9 years not previously vaccinated and who require 2 doses). Antiviral chemoprophylaxis should not be given for 2 weeks after administration of live attenuated influenza virus vaccine. If pos-texposure antiviral chemoprophylaxis is administered, it should be given within 48 hours of exposure to a person with influenza.
DIAGNOSIS
Which Patients Should Be Tested for Influenza?
Recommendations
Outpatients (including emergency department patients).
-
1During influenza activity (defined as the circulation of seasonal influenza A and B viruses among persons in the local community) (see Figure 1):
- Clinicians should test for influenza in immunocompromised and high-risk patients who present with influenza-like illness, pneumonia, or nonspecific respiratory illness (eg, cough without fever) if the testing result will influence clinical management (A-III).
- Clinicians should test for influenza in patients who present with acute onset of respiratory symptoms with or without fever, and either exacerbation of chronic medical conditions (eg, asthma, chronic obstructive pulmonary heart disease [COPD], heart failure) or known complications of influenza (eg, pneumonia) if the testing result will influence clinical management (A-III) (see Table 3).
- Clinicians can consider influenza testing for patients not at high risk for influenza complications who present with influenza-like illness, pneumonia, or nonspecific respiratory illness (eg, cough without fever) and who are likely to be discharged home if the results might influence antiviral treatment decisions or reduce use of unnecessary antibiotics, further diagnostic testing, and time in the emergency department, or if the results might influence antiviral treatment or chemoprophylaxis decisions for high-risk household contacts (see recommendations 40–42) (C-III).
-
2During low influenza activity without any link to an influenza outbreak:
- Clinicians can consider influenza testing in patients with acute, febrile respiratory tract illness, especially for immunocompromised and high-risk patients (B-III).
Hospitalized Patients.
-
3During influenza activity:
- Clinicians should test for influenza on admission in all patients requiring hospitalization with acute respiratory illness, including pneumonia, with or without fever (A-II).
- Clinicians should test for influenza on admission in all patients with acute worsening of chronic cardiopulmonary disease (eg, COPD, asthma, coronary artery disease, or congestive heart failure), as influenza can be associated with exacerbation of underlying conditions (A-III).
- Clinicians should test for influenza on admission in all patients who are immunocompromised or at high risk of complications and present with acute onset of respiratory symptoms with or without fever, as the manifestations of influenza in such patients are frequently less characteristic than in immunocompetent individuals (A-III).
- Clinicians should test for influenza in all patients who, while hospitalized, develop acute onset of respiratory symptoms with or without fever, or respiratory distress, without a clear alternative diagnosis (A-III).
-
4During periods of low influenza activity:
- Clinicians should test for influenza on admission in all patients requiring hospitalization with acute respiratory illness, with or without fever, who have an epidemiological link to a person diagnosed with influenza, an influenza outbreak or outbreak of acute febrile respiratory illness of uncertain cause, or who recently traveled from an area with known influenza activity (A-II).
- Clinicians can consider testing for influenza in patients with acute, febrile respiratory tract illness, especially children and adults who are immunocompromised or at high risk of complications, or if the results might influence antiviral treatment or chemoprophylaxis decisions for high-risk household contacts (see recommendations 41–43) (B-III).
Evidence Summary
Although clinical diagnosis during influenza outbreaks has reasonable sensitivity and specificity, laboratory testing should be performed when the results may influence clinical management or infection prevention and control decisions. During periods of high influenza activity, influenza is typically diagnosed based on presenting illness signs and symptoms. Cough and fever provide the most predictive signs and symptoms when influenza viruses are circulating in the community [126]. However, influenza may be clinically indistinguishable from illness caused by other infectious etiologies (including bacterial and other viral infections such as respiratory syncytial virus, parainfluenza virus, human metapneumovirus, and adenovirus) [127]. Various case definitions and scoring systems designed to predict the likelihood of influenza have low specificity and predictability [30, 128–133].
An algorithmic approach may help optimize the use of influenza testing (Figure 1). If influenza testing of high-risk outpatients with suspected influenza to confirm influenza is not feasible, or if testing will not change clinical management decisions, a clinical diagnosis of influenza without testing can support empiric antiviral treatment decisions. Influenza testing is recommended for all hospitalized patients during influenza season with acute respiratory illness including pneumonia, respiratory failure, or exacerbation of a chronic condition (eg, asthma, coronary artery disease, COPD) [65–67] and for immunocompromised patients with any of the above or nonspecific respiratory symptoms or unexplained fever [134]. Influenza testing can help inform management and IPC measures in hospitalized patients. A test confirming influenza may reduce the unnecessary use of antibiotics (especially if the procalcitonin level is low, suggesting that bacterial infection is unlikely) and improve antibiotic stewardship. Also, influenza testing can be helpful in hospitalized patients to reduce unnecessary antiviral therapy if a highly sensitive influenza test (eg, molecular assay) does not confirm influenza (especially when another microbial etiology is identified).
One randomized clinical trial (RCT), performed at medical wards of 2 teaching hospitals in the United Kingdom, found no evidence that RT-PCR testing for influenza influenced antibiotic prescribing or clinical outcome in adult patients; however, few study patients with RT-PCR-confirmed influenza were prescribed antiviral treatment [135]. The authors suggested this was in part due to the length of illness prior to admission (>48 hours) or unfamiliarity by physicians with RT-PCR. In contrast, several observational studies have reported benefits of influenza testing. In a retrospective study of data from the National Hospital Ambulatory Medical Care Survey, influenza testing resulted in fewer ancillary and other diagnostic tests (ie, chest radiography, blood culture, urinalysis, complete blood count) and more frequent use of antivirals [136]. Another study reported that rapid influenza diagnostic testing resulted in early receipt of antiviral treatment as compared with relying on the presence of risk factors alone [137]. In a retrospective study, rapid influenza testing led to a significant reduction in antibiotic use among hospitalized adults [12]. A study from 2 hospitals in Belgium during the 2015 influenza season reported that use of a rapid molecular assay in emergency departments helped avoid 10.7% of hospitalizations, 46.4% of antibiotic prescriptions, and 42.9% of additional investigations for influenza-positive patients, and helped facilitate prescription of oseltamivir and patient isolation [138]. In a prospective trial in the United Kingdom, use of a rapid multiplex polymerase chain reaction (PCR) test in patients hospitalized with acute respiratory illness increased appropriate use of anti-virals for patients with laboratory-confirmed influenza from 65% to 91% and decreased length of hospital stay by 1 day [139]. Use of a rapid RT-PCR-based influenza assay decreased unnecessary antiviral use among adult patients hospitalized for acute respiratory tract infection who tested negative for influenza [140].
A randomized controlled trial using a rapid influenza antigen test in a pediatric emergency department demonstrated that among young children with febrile acute respiratory illness, rapid testing resulted in fewer diagnostic tests, fewer antibiotic prescriptions, and decreased length of stay in the emergency department [11]. Use of a respiratory viral panel test for children admitted to the hospital with an acute respiratory tract illness resulted in shorter time to diagnosis, duration of antibiotic use, and length of inpatient stay [141]. One study used a decision analytic model to compare costs of care and outcomes using 4 different strategies for influenza testing in children (rapid multiplex PCR; traditional RT-PCR; direct-fluorescent antibody staining; and rapid antigen tests). Despite the increased cost, when considering the potential to reduce inappropriate antibiotic use and other costs of care, the most effective test was rapid multiplex PCR [142]. Other studies have reported that a confirmatory influenza test result reduced the use of unnecessary antibiotics and patient waiting time in outpatient clinics and emergency departments [136, 143–145].
Laboratory testing is important for immunocompromised patients since the manifestations of influenza virus infection in such patients are frequently less characteristic than in immunocompetent patients.
What Specimen(s) Should Be Collected When Testing Patients for Influenza?
Recommendations
-
5Clinicians should collect upper respiratory tract specimens from outpatients for influenza testing as soon after illness onset as possible, preferably within 4 days of symptom onset (A-II).
- Nasopharyngeal (NP) specimens should be collected over other upper respiratory tract specimens to increase detection of influenza viruses (A-II).
- If NP specimens are not available, nasal and throat swab specimens should be collected and combined together for influenza testing over single specimens from either site (particularly over throat swabs) to increase detection of influenza viruses (A-II).
- Mid-turbinate nasal swab specimens should be collected over throat swab specimens to increase detection of influenza viruses (A-II).
- Flocked swab specimens should be collected over non-flocked swab specimens to improve detection of influenza viruses (A-II).
-
6
Clinicians should collect NP (optimally, as for outpatients), mid-turbinate nasal, or combined nasal-throat specimens from hospitalized patients without severe lower respiratory tract disease for influenza testing as soon as possible (A-II).
-
7
Clinicians should collect endotracheal aspirate or broncho-alveolar lavage (BAL) fluid specimens from hospitalized patients with respiratory failure receiving mechanical ventilation, including patients with negative influenza testing results on upper respiratory tract specimens, for influenza testing as soon as possible (A-II).
-
8
Clinicians should not collect or routinely test specimens for influenza from nonrespiratory sites such as blood, plasma, serum, cerebrospinal fluid (CSF), urine, and stool (A-III).
-
9
Clinicians should not collect serum specimens, including single or paired sera, for serological diagnosis of seasonal influenza virus infection for clinical management purposes (A-III).
Evidence Summary
In most persons, infectious influenza virus levels in the upper respiratory tract of persons with uncomplicated influenza peak during the first 1–2 days after illness onset, and decline to undetectable levels within a week [146, 147]. Collection of upper respiratory tract specimens from immunocompetent outpatients with influenza >3–4 days after illness onset may yield negative results because of substantially decreased influenza viral shedding, especially in older children and adults. Influenza viruses might be detectable in upper respiratory tract specimens for longer periods in some patients, particularly when molecular assays are used. Infants and young children and adults hospitalized with severe lower respiratory tract illness often shed influenza viruses for ≥1 week. Immunocompromised patients may have prolonged influenza virus replication and shed infectious influenza viruses for weeks to months, even when asymptomatic or without fever [134, 148].
The appropriate respiratory tract specimen to collect depends upon which influenza test is used and patient acceptability. Prospective evaluation of clinical specimens in patients with influenza A(H1N1)pdm09, A(H1N1), or A(H3N2) virus infections documented that the highest viral load and best sensitivity are obtained from NP aspirate, followed by nasal or NP swab, and then throat swab specimens [149]. NP aspirate specimens are acceptable for multiple types of influenza tests [150], but are more cumbersome to obtain and less well tolerated by patients. Similar sensitivity in detecting respiratory viruses has been demonstrated for mid-turbinate nasal swab specimens compared with NP swabs [151]. For molecular assays, NP or mid-turbinate nasal swab specimens are the preferred upper respiratory tract specimens. However, mid-turbinate swabs may not be approved for all assays or accepted by all laboratories. Oropharyngeal specimens (eg, throat swabs) generally have a lower yield for detection of seasonal influenza viruses [152], but may still produce positive results, especially when molecular assays are used. Testing sputum specimens by RT-PCR can increase the detection of influenza viral RNA over combined nasal and throat swabs [153–155].
Some influenza diagnostic assays have been tested and FDA approved for respiratory specimens collected from specific sites, although published studies have utilized other respiratory specimens such as combined specimens or lower respiratory tract specimens. Clinicians should check both the approved clinical specimens for a specific assay and what specimens are accepted by clinical laboratories before collecting specimens. Some assays (eg, a few rapid influenza diagnostic tests) require the exact swab supplied with the test being used. Use of a flocked nasal swab (with fibers projecting outward) may increase the detection of influenza viruses over a nonflocked swab and have a similar yield as NP aspirate [156].
Testing of a combined specimen (a nasal swab and a throat swab placed together) can be used to increase test sensitivity over testing each swab separately. Testing combined specimens from 3 sites (combined nasal and throat swabs plus a nasal aspirate) was more sensitive for detecting influenza A(H1N1) pdm09 virus than any single sample [157]. Paired nasal-throat swabs are similar in sensitivity to NP aspirates in children when evaluated by molecular assay and are more readily tolerated [158]. Addition of a throat swab to a nasal specimen using molecular testing has been shown to slightly increase recovery of influenza viruses in pediatric patients in some studies [159], but not in others [160]. For the detection of influenza viruses by nonmolecular assays, combined specimens or NP aspirates should be considered. In the hospitalized patient, the use of flocked mid-turbinate nasal swabs, combined nasal plus throat swabs, or NP aspirates is recommended.
In critically ill patients with respiratory failure who are receiving mechanical ventilation, a lower respiratory tract specimen (endotracheal aspirate or BAL fluid) should be obtained for influenza testing. Lower respiratory tract specimens have much higher sensitivity for detection of influenza viruses in critically ill patients because influenza virus shedding may be lower or have stopped in the upper respiratory tract, whereas influenza viral replication in the lower respiratory tract may be higher and prolonged [121, 122, 161–163].
Seasonal influenza viruses infect the respiratory tract and typically are not associated with viremia. Influenza viral RNA has rarely been detected in blood, although detection in severely immunosuppressed persons and critically ill patients with influenza has been reported, but whether this represents viremia is unclear [164–166]. A large autopsy series of 100 fatal cases found no evidence of extrapulmonary influenza A(H1N1) pdm09 virus infection [167]. Therefore, except for research purposes or for special patient populations, there is no diagnostic utility to routinely collect whole blood, plasma, or serum specimens for seasonal influenza virus testing by any assay.
The pathogenesis of influenza-associated neurologic complications (including encephalopathy, encephalitis, acute disseminated encephalomyelitis, cerebral vascular accident, Guillain-Barré syndrome) is complex and may be related to inflammation of the nervous system caused by cytokine dysregulation triggered by influenza virus infection of the respiratory tract [168, 169]. Therefore, CSF testing for influenza for suspected seasonal influenza-associated central nervous system disease is not routinely recommended. Clinicians should test respiratory specimens for influenza if influenza-associated neurologic complications are suspected.
Renal failure can occur in critically ill influenza patients [63, 170, 171] but does not represent kidney infection, and evidence of seasonal influenza viruses has very rarely been reported in urine [172]; therefore, collection of urine for influenza testing is not recommended.
Influenza viral RNA or infectious virus has rarely been detected in stool, and such detection is of unknown clinical importance [38, 173–175]; therefore, testing of stool for influenza viruses is not recommended.
For serological diagnosis of seasonal influenza virus infection, paired acute and convalescent serum specimens must be collected and tested together, and cannot inform clinical management. There is no validated immunoglobulin M assay or other available serologic assay to diagnose seasonal influenza virus infection in a single serum specimen. Therefore, single serum or paired sera specimens should not be collected for influenza serology except for research purposes.
What Test(s) Should Be Used to Diagnose Influenza?
Recommendations
-
10
Clinicians should use rapid molecular assays (ie, nucleic acid amplification tests) over RIDTs in outpatients to improve detection of influenza virus infection (A-II) (see Table 6).
-
11
Clinicians should use reverse-transcription polymerase chain reaction (RT-PCR) or other molecular assays over other influenza tests in hospitalized patients to improve detection of influenza virus infection (A-II) (see Table 6).
-
12
Clinicians should use multiplex RT-PCR assays targeting a panel of respiratory pathogens, including influenza viruses, in hospitalized immunocompromised patients (A-III).
-
13
Clinicians can consider using multiplex RT-PCR assays targeting a panel of respiratory pathogens, including influenza viruses, in hospitalized patients who are not immunocompromised if it might influence care (eg, aid in isolation decisions, reduce other testing or antibiotic use) (B-III).
-
14
Clinicians should not use immunofluorescence assays for influenza virus antigen detection in hospitalized patients except when more sensitive molecular assays are not available (A-II), and follow-up testing with RT-PCR or other molecular assays should be performed to confirm negative immunofluorescence test results (A-III).
-
15
Clinicians should not use RIDTs in hospitalized patients except when more sensitive molecular assays are not available (A-II), and follow-up testing with RT-PCR or other molecular assays should be performed to confirm negative RIDT results (A-II).
-
16
Clinicians should not use viral culture for initial or primary diagnosis of influenza because results will not be available in a timely manner to inform clinical management (A-III), but viral culture can be considered to confirm negative test results from RIDTs and immunofluorescence assays, such as during an institutional outbreak, and to provide isolates for further characterization (C-II).
-
17
Clinicians should not use serologic testing for diagnosis of influenza because results from a single serum specimen cannot be reliably interpreted, and collection of paired (acute/convalescent) sera 2–3 weeks apart are needed for serological testing (A-III).
Evidence Summary
There are multiple options for influenza diagnostic and confirmatory testing [108]. The ideal diagnostic test should produce rapid, accurate results with high sensitivity and high specificity to detect influenza viruses in respiratory specimens at reasonable cost. Each test has strengths and weaknesses and a thoughtful diagnostic approach is important (see information on influenza testing and clinical algorithms available on the CDC website: https://www.cdc.gov/flu/professionals/diagnosis/index.htm).
Rapid influenza molecular assays that detect influenza viral RNA utilizing different nucleic acid amplification technologies have recently been approved by the FDA. These rapid molecular assays generally have moderately high to high sensitivity (66%−99%) and high specificity (55%−99%), depending upon the virus type, compared with RT-PCR assays [111, 117, 176–184]. In some studies, sensitivity and specificity of rapid molecular assays were reported to be slightly lower for influenza B viruses than for influenza A viruses.
RT-PCR assays, whether real-time or multiplex, are highly sensitive and highly specific nucleic acid amplification tests for detection of influenza viral RNA. RT-PCR assays produce results in significantly less time than viral culture and are frequently used as a confirmatory test [126]. There are multiple assays approved by the FDA. These assays are also useful for testing individuals with suspected influenza during low influenza periods. Some commercially available molecular assays can distinguish between influenza A virus subtypes. Molecular techniques for influenza diagnosis continue to advance; additional and updated information is available at the CDC’s influenza website (http://www.cdc.gov/flu/professionals/diagnosis/index.htm).
Immunofluorescence assays require laboratory expertise and a fluorescent microscope, and take longer to produce results than RIDTs, rapid molecular assays, and some RT-PCR assays, but have generally better sensitivity and specificity than RIDTs [185, 186]. However, some immunofluorescence assays may be part of a respiratory panel and thus useful for the identification of other respiratory viruses.
RIDTs are primarily point-of-care immunoassays; one test is an immunofluorescent assay. RIDTs have utility in community- and hospital-based outpatient settings because of their rapid processing times. Some RIDTs utilize an analyzer device for standardizing results and improving test sensitivity to detect influenza viral antigens [111]. However, the sensitivities for RIDTs range from very low to moderate (ie, approximately 10%−70%), often yielding false-negative results, while specificities are high (ie, approximately 90%−99%), compared with RT-PCR or viral culture [110, 111, 115, 116, 187]. Therefore, RIDTs are not recommended for use in hospitalized patients with suspected influenza, and rapid influenza molecular assays may be a better alternative in outpatient settings.
TREATMENT
Which Patients With Suspected or Confirmed Influenza Should Be Treated With Antivirals?
Recommendations
-
18Clinicians should start antiviral treatment as soon as possible for adults and children with documented or suspected influenza, irrespective of influenza vaccination history, who meet the following criteria:
- Persons of any age who are hospitalized with influenza, regardless of illness duration prior to hospitalization (A-II).
- Outpatients of any age with severe or progressive illness, regardless of illness duration (A-III).
- Outpatients who are at high risk of complications from influenza, including those with chronic medical conditions and immunocompromised patients (A-II).
- Children younger than 2 years and adults aged ≥65 years (A-III).
- Pregnant women and those within 2 weeks postpartum (A-III).
-
19Clinicians can consider antiviral treatment for adults and children who are not at high risk of influenza complications, with documented or suspected influenza, irrespective of influenza vaccination history, who are either:
- Outpatients with illness onset ≤2 days before presentation (C-I).
- Symptomatic outpatients who are household contacts of persons who are at high risk of developing complications from influenza, particularly those who are severely immunocompromised (C-III).
- Symptomatic healthcare providers who routinely care for patients who are at high risk of developing complications from influenza, particularly those who are severely immunocompromised (C-III).
Evidence Summary
Influenza can result in a wide range of clinical signs, symptoms, and complications of variable severity, from self-limited upper respiratory tract illness, to life-threatening illness with respiratory failure and prolonged respiratory tract influenza virus replication. The clinical and virologic impact of NAI antiviral treatment of influenza is dependent on several factors: immune status of the host, underlying medical conditions, age, virus type or influenza A virus subtype, and illness duration and severity when antiviral treatment is started [13, 16, 188–199]. The relevant study population to assess clinical benefit of NAI treatment is patients with laboratory-confirmed influenza (intention-to-treat-infected). There is no evidence that NAIs have benefit for ill patients with-out influenza virus infection. Therefore, in studies of NAI treatment of patients with nonspecific ILI without documentation of influenza virus infection (intention-to-treat), clinical outcomes are biased toward lower efficacy or effectiveness [14] than in studies of treatment of laboratory-confirmed influenza.
Most RCTs of NAI treatment of outpatients with seasonal influenza were conducted before 2009, whereas most observational studies of NAI treatment were done during or after the 2009 H1N1 pandemic. Systematic reviews and meta-analyses of RCTs of early NAI treatment in generally healthy outpatients with uncomplicated laboratory-confirmed influenza reported clinical benefit in reducing illness duration in children and adults, and in reducing risk of hospitalization in adults [194, 200]. A meta-analysis of observational data for high-risk pediatric and adult outpatients with laboratory-confirmed influenza reported that NAI treatment reduced the risk of hospitalization for any cause [201]. Survival benefit of NAI treatment of hospitalized adult patients with laboratory-confirmed influenza was reported by one systematic review of the published systematic reviews of observational studies [202] and 2 meta-analyses of observational studies [13, 16], but not in another meta-analysis [203].
Randomized placebo-controlled clinical trials that established the efficacy of NAIs in reducing the duration of fever and symptoms by approximately 1–2 days were conducted among mostly non-high-risk adult and pediatric outpatients with uncomplicated laboratory-confirmed influenza, enrolled within 36–48 hours of illness onset [188–191, 204–206]. Greater clinical benefit was reported when NAI treatment was started very early; in both adults and children, NAI treatment started within 6 hours of illness onset reduced symptoms by about 4 days [26, 197, 207]. Systematic reviews and meta-analyses of RCTs indicate that early initiation (within 2 days of illness onset) of antiviral treatment can reduce the duration of fever and symptoms, especially in nonasthmatic children; decrease the risk of otitis media in children; and reduce the risk of lower respiratory tract complications requiring antibiotics and of hospitalization in adults [14, 194, 200].
Because high-risk outpatients with suspected or confirmed influenza are recommended for prompt antiviral treatment, placebo-controlled studies are generally not possible in many countries, and the benefits of antiviral therapy in different highrisk groups to reduce complications have not been reported in completed prospective, randomized, placebo-controlled trials. However, an individual patient data meta-analysis of >3000 outpatients at high risk for complications with laboratory-confirmed influenza reported that NAI treatment significantly reduced the likelihood of hospital admission [201].
There are no fully enrolled prospective, randomized, placebo-controlled trials of oral oseltamivir or inhaled zanamivir in hospitalized influenza patients. A pooled meta-analysis of observational studies with individual-level data from >29 000 hospitalized patients (86% with laboratory-confirmed influenza, 14% clinically diagnosed with influenza) reported survival benefit of NAI treatment (primarily oseltamivir) in adults compared with no treatment, with significantly greater survival benefit with early (within 2 days of illness onset) compared with later initiation (>2 days after onset) of NAI treatment [16]. This study also reported that NAI treatment (including started >2 days after onset) vs no treatment had significant survival benefit in critically ill adults and in pregnant and postpartum women with influenza [16]. In contrast, when mortality was analyzed as the endpoint for children aged <16 years hospitalized with influenza, the meta-analysis reported that early vs later initiation of NAI treatment, and early initiation vs no treatment, did not have significant survival benefit, although the low number of deaths limited statistical power [16, 195]. Other observational studies of hospitalized influenza patients have reported that NAI treatment shortened the duration of hospitalization and reduced the risk of mechanical ventilation in children [196, 208], and improved survival in adults [199].
The majority of observational studies, individual patient-level pooled analyses, and meta-analyses of patients with laboratory-confirmed influenza have reported clinical benefit of NAI treatment (primarily oral oseltamivir) among hospitalized patients, including persons at high risk for influenza complications (Table 4), including when NAI treatment was started >48 hours after illness onset [13, 15, 16, 192–196, 198, 199, 209, 210]. However, a small number of observational studies and one meta-analysis of observational studies of hospitalized influenza patients reported that NAI treatment did not have survival benefit [203, 211, 212]. In studies showing a benefit, the greatest clinical benefit was reported when antiviral treatment was started within 2 days of illness onset, but benefit was noted even when treatment was started in most patients 4–5 days and up to 7 days after illness onset [15, 16, 193, 199, 209].
Although prompt antiviral treatment is recommended for high-risk outpatients with suspected or confirmed influenza, a study of high-risk persons during 2011–2016 reported that of those who presented to outpatient care within 2 days of onset of acute respiratory illness symptoms, only 15% were prescribed antiviral treatment, including 37% with RT-PCR-confirmed influenza [213]. In this study, 40% of high-risk persons presented for medical care within 2 days of illness onset. Another study reported that while the proportion of hospitalized influenza patients who received antiviral treatment increased during 2010–2011 to 2014–2015, the percentage was higher in adults than children, and only 56% were treated on the day of admission [214]. A study of hospitalized pediatric influenza patients reported that the proportion that received antiviral treatment increased from 20% to 69% overall during 2007–2015, but varied from 42% to 90% among 46 hospitals during 2014–2015 [23]. Because the clinical benefit of NAI treatment is greatest the earlier that treatment is initiated, we recommend starting empiric antiviral treatment as soon as possible without waiting for influenza testing results when patients with suspected influenza are being admitted to the hospital.
Early antiviral treatment of influenza in outpatients reduces the likelihood of antibiotic use for physician-diagnosed complications and may reduce secondary bacterial coinfection (otitis media, pneumonia) [13, 191, 194, 200, 215]. Thus, antiviral treatment of influenza has the potential to decrease medical care costs and antibiotic-attributable adverse events, and potentially decrease bacterial resistance to antibiotics. Well-described risk factors for influenza complications allow clinicians to target patients who are most likely to benefit from prompt antiviral treatment of influenza (Table 4) [134, 170, 208, 216–221].
Data from the 2009 H1N1 pandemic highlighted the impact of A(H1N1)pdm09 virus infection on pregnant and postpartum women [222–224]. While risk of severe morbidity and mortality from influenza occurs throughout pregnancy, these risks are higher in the second and third trimesters [225–227]. During the 2009 H1N1 pandemic, of 30 maternal deaths in the United States, 7.1% occurred in the first trimester; 26.8% in the second trimester, and 64.3% in the third trimester [3]. One meta-analysis of seasonal and pandemic influenza studies reported that increased influenza-associated mortality risk occurs in the third trimester compared to the first or second trimesters, but also extends 4 weeks postpartum [228]. The etiology for this increase in disease severity may reflect normal physiologic changes of pregnancy including an altered immune system, decreased lung capacity as the uterus grows, increased heart rate and oxygen consumption, and increased colloid oncotic pressure.
Maternal morbidity associated with influenza includes a greater risk for hospitalization, intensive care unit (ICU) admission, and adult respiratory distress syndrome [3, 209, 229–233]. Some studies reported that influenza during pregnancy may lead to preterm labor and small for gestational age infants [224, 234–240]. However, other studies of infants born to women who had laboratory-confirmed influenza during pregnancy have not shown higher rates of prematurity, preterm labor, low birth weight, or lower Apgar scores compared with infants born to uninfected women [230, 241, 242]. One meta-analysis reported an association of maternal influenza to congenital birth defects including neural tube and heart defects [243]. In addition, influenza during pregnancy can precipitate spontaneous abortion [244, 245]. A study of the 2009 H1N1 pandemic in California reported that pregnant and postpartum women who received antiviral treatment >2 days after presentation were more likely to be admitted to the ICU or die compared to those treated ≤2 days after presentation [209]. A meta-analysis of data from hospitalized patients with A(H1N1)pdm09 virus infection worldwide reported that pregnant and postpartum women treated with NAIs within 2 days of admission were 20% less likely to die compared to those treated later [16].
Annual influenza vaccination can prevent influenza, but influenza vaccine effectiveness has ranged from low to moderate in preventing medically attended outpatient visits and hospitalizations, and may have lower effectiveness in immunocompromised patients, who may also experience prolonged influenza viral replication [134]. A history of current season influenza vaccination does not exclude a diagnosis of influenza in either immunocompetent or immunocompromised patients. Therefore, antiviral treatment should be initiated as soon as possible in hospitalized patients, high-risk persons, and those with severe or progressive disease if influenza is suspected, irrespective of receipt of influenza vaccine.
No primary studies exist of the effectiveness of antiviral treatment of uncomplicated influenza in a non-high-risk person to prevent influenza in a household contact who is at high risk for influenza complications, including immunocompromised persons. However, data from a prospective, randomized, placebo-controlled trial in Bangladesh to assess the impact of antiviral treatment of an index case on household spread of influenza documented a small but significant decrease in the number of secondary cases [246]. Retrospective observational studies have suggested benefit of antiviral treatment in reducing transmission to household contacts [247, 248]. Therefore, early antiviral treatment of persons with uncomplicated influenza who have household members that are immunocompromised is recommended to provide potential benefit in reducing the risk of influenza in the household contacts. See recommendations 40–42 and Evidence summary for discussion of the role of postexposure prophylaxis in high-risk patients who are close contacts of influenza patients.
For Patients Who Are Recommended to Receive Antiviral Treatment for Suspected or Confirmed Influenza, Which Antiviral Should Be Prescribed, at What Dosing, and for What Duration?
Recommendations
-
20
Clinicians should start antiviral treatment as soon as possible with a single NAI (either oral oseltamivir, inhaled zanamivir, or intravenous peramivir) and not use a combination of NAIs (A-1).
-
21
Clinicians should not routinely use higher doses of FDA-approved NAI drugs for the treatment of seasonal influenza (A-II).
-
22
Clinicians should treat uncomplicated influenza in otherwise healthy ambulatory patients for 5 days with oral oseltamivir or inhaled zanamivir, or a single dose of intravenous peramivir (A-1).
-
23
Clinicians can consider longer duration of antiviral treatment for patients with a documented or suspected immunocompromising condition or patients requiring hospitalization for severe lower respiratory tract disease (especially pneumonia or acute respiratory distress syndrome [ARDS]), as influenza viral replication is often protracted (C-III).
Evidence Summary
Clinicians should maintain familiarity with local patterns of influenza activity in their communities throughout influenza season. Current and frequently updated information on antiviral resistance and approved antivirals is available on the CDC’s influenza website (http://www.cdc.gov/flu).
Based on seasonal influenza virus susceptibility patterns observed through virologic surveillance from 2009 through 2017, the use of an NAI is recommended—either oral oseltamivir, inhaled zanamivir, or intravenous (IV) peramivir for early treatment of uncomplicated influenza in pediatric and adult patients. Therapy should be started as soon as possible and generally should not be delayed while awaiting influenza test results.
The adamantane influenza antiviral agents, with activity only against susceptible influenza A viruses, are not recommended for treatment of influenza A given documented high levels of adamantane resistance among circulating influenza A viruses in recent years [249, 250].
Risks and benefits may differ between specific antiviral agents for various patient populations based on age, underlying medical conditions, immune function, severity of illness, and different influenza virus strains. Comparative prospective, controlled data on outcomes with different antiviral agents do not exist for most of these risk groups and conditions. One superiority-design RCT without a placebo arm did not demonstrate superiority of investigational IV zanamivir to oral oseltamivir in hospitalized patients with laboratory-confirmed influenza [251]. One RCT of monotherapy with oral oseltamivir or inhaled zanamivir compared with combination oral oseltamivir plus inhaled zanamivir treatment or placebo in adult outpatients with lab oratory-confirmed influenza reported that oral oseltamivir demonstrated both significant reduction in viral shedding at day 2 of treatment and significant reduction in the median time to resolution of illness symptoms compared with inhaled zanamivir [252]. In addition, oral oseltamivir had both significant virologic and clinical benefit compared with combination oseltamivir-zanamivir treatment, whereas the oseltamivir-zanamivir combination treatment had significant virologic, but not significant clinical, benefit compared with inhaled zanamivir [252]. One RCT reported that combination oral therapy with oseltamivir, amantadine, and ribavirin resulted in a significant but modest reduction in influenza viral shedding at treatment day 3, but was not associated with significant reduction in multiple clinical endpoints compared with oseltamivir monotherapy in adult outpatients with laboratory-confirmed influenza [253]. Based upon available evidence, recommendations are provided below for specific antiviral agents, route, dosing, and duration of therapy.
Oseltamivir treatment is associated with gastrointestinal symptoms. Meta-analyses of RCTs among outpatients with lab oratory-confirmed influenza reported that oseltamivir treatment vs placebo was significantly associated with vomiting (relative risk [RR], 1.63) in children [200] and nausea (RR, 1.6; risk difference, 3.7%) and vomiting (RR, 2.43; risk difference, 4.7%) in adults [194]. Similar findings were reported in a systematic review of oseltamivir RCTs in children and adults [254]. No significant differences were found in any serious adverse events or study withdrawal due to adverse events in these pediatric and adult RCTs [194, 200]. Although post-marketing reports of severe abnormal behavior in adolescents with influenza after starting oseltamivir treatment have been reported primarily in Japan, no differences in the estimated incidence of life-threatening abnormal behavior were identified among patients treated with 4 different NAIs, including oseltamivir, in Japan [255]. Another study that utilized national medical claims data reported that the estimated risk of severe abnormal behavior was lower for Japanese children prescribed oseltamivir than those who were not prescribed an NAI [256]. A case-crossover analysis of administrative data found no association with suicide for oseltamivir exposure or influenza diagnosis [257]. A self-controlled case series study in Japan could not exclude the possibility that severe abnormal behavior was induced by influenza [258]. A meta-analysis of RCTs of inhaled zanamivir treatment reported no evidence of an increase in reported adverse events vs placebo in children or adults [259]. A combined analysis of data from one phase 2 RCT and one phase 3 RCT of peramivir treatment reported that the frequency of adverse events was similar to placebo [260].
Dosing and Duration
Adults
Drug dosing is standardized for oral oseltamivir and inhaled zanamivir (Table 8). Oseltamivir phosphate is metabolized to the active metabolite oseltamivir carboxylate by hepatic esterases and renally excreted; dosage adjustment for oseltamivir is indicated for reduced renal function. Zanamivir is administered as an orally inhaled powder, concentrated in the respiratory tract with limited systemic absorption that is excreted unchanged by the kidneys. Duration of therapy with oseltamivir and zanamivir for ambulatory adults with uncomplicated influenza is 5 days. In ambulatory adults with uncomplicated influenza, peramivir administered as a single IV dose is an alternative, but is costlier. In hospitalized adults, oseltamivir is the preferred antiviral drug because data are very limited on inhaled zanamivir in severely ill influenza patients.
Table 8.
Antiviral Agents and Dosing Recommendations for Treatment and Chemoprophylaxis of Influenza
| Antiviral Agents and Age Group | Treatment Dosing | Chemoprophylaxis Dosing |
|---|---|---|
| Oseltamivir | ||
| Adults | 75 mg twice daily | 75 mg once daily |
| Pregnancy (any trimester)a | 75 mg twice dailyb | 75 mg once dailyb |
| Children (1 year or older) ≤15 kg | 30 mg twice daily | 30 mg once daily |
| Children >15–23 kg | 45 mg twice daily | 45 mg once daily |
| Children >23–40 kg | 60 mg twice daily | 60 mg once daily |
| Children >40 kg | 75 mg twice daily | 75 mg once daily |
| Infants 9–11 months | 3.5 mg/kg per dose twice dailyc | 3.5 mg/kg per dose once dailyc |
| 3 mg/kg per dose twice dailyc | 3 mg/kg per dose once dailyc | |
| Term infants 0–8 months | 3 mg/kg per dose twice daily | 3 mg/kg per dose once daily if ≥3 months; not recommended for infants <3 months unless the situation is judged critical due to lack of safety and efficacy data |
| Preterm infants | See details in footnotea | No data |
| Zanamivir | ||
| Adults | 10 mg (two 5-mg inhalations), twice daily | 10 mg (two 5-mg inhalations), once daily |
| Children (≥7 years) | 10 mg (two 5-mg inhalations), twice daily | 10 mg (two 5-mg inhalations), once daily |
| Peramivird | ||
| Adults | 600 mg intravenous infusion once, given over 15–30 minutes | NA |
| Children (2—12 years) | One 12 mg/kg dose, up to 600 mg maximum, intravenous, given over 15–30 minutes | NA |
| Children (13–17 years) | 600 mg intravenous infusion once, given over 15–30 minutes | NA |
Antiviral resistance information is available in the weekly Centers for Disease Control and Prevention (CDC) influenza surveillance report: https://wwwcdc.gov/flu/weekly/index.htm. Abbreviation: NA, not applicable.
The weight-based dosing recommendation for preterm infants is lower than for term infants. Preterm infants may have lower clearance of oseltamivir because of immature renal function, and doses recommended for full-term infants may lead to very high drug concentrations in this age group. Limited data from the National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group provide the basis for dosing preterm infants using their postmenstrual age (ie, gestational age + chronological age): 1.0 mg/kg per dose, orally, twice daily, for those <38 weeks postmenstrual age; 1.5 mg/kg per dose, orally, twice daily, for those 38–40 weeks postmenstrual age; 3.0 mg/kg per dose, orally, twice daily, for those >40 weeks postmenstrual age. For extremely premature infants (<28 weeks), please consult a pediatric infectious diseases physician (Committee on Infectious Diseases. Recommendations for prevention and control of influenza in children, 2017–2018. Pediatrics 2018; 141. pii:e20173535).
Based on pharmacokinetic data in pregnancy, regardless of trimester, a dose of 105 mg twice daily was predicted to provide the effective exposure provided to nonpregnant adults Some experts recommend 150 mg twice daily for severe illness in pregnant women. Optimal dosing for prophylaxis in pregnant women is unknown.
The American Academy of Pediatrics recommends 3.5 mg/kg per dose twice daily; CDC and US Food and Drug Administration (FDA)-approved dosing is 3 mg/kg per dose twice daily for children aged 9–11 months.
Approved for early treatment of uncomplicated influenza in outpatients. If used off-label for treatment of hospitalized patients, repeated once-daily dosing can be considered, although data are very limited.
Modifications in Special Populations
Pediatrics
Oseltamivir (tablets or oral suspension formulation) may be administered to all pediatric age groups with influenza, including premature infants [216]. Duration of therapy for ambulatory children with uncomplicated influenza is 5 days. Dosing is based upon age and weight; however, the FDA has not reviewed data on safety and efficacy of oseltamivir in neonates <2 weeks of age. Although only limited pharmacokinetic data are available for oseltamivir in neonates and premature infants, 3 mg/kg/ dose twice daily has been used in some studies, although one open-label adaptive design study reported that doses of 3.5 mg/ kg were needed to produce drug exposures approaching the efficacious exposure levels in adults [261, 262]. One study that utilized a pharmacokinetic model based upon data from samples collected from neonates treated with oseltamivir suggested use of lower oseltamivir doses in premature (1 mg/kg) and term infants (2 mg/kg) [263]. Documented increased morbidity and mortality of influenza in newborn and very young infants should be balanced by the anticipated benefits of therapy given the available limited pharmacokinetics and safety data in this very young population [6]. Zanamivir (inhalation) is FDA-approved for treatment of uncomplicated influenza in children aged ≥7 years. Dosing and duration of uncomplicated influenza is the same for all pediatric age groups (2 inhalations twice daily for 5 days).
Peramivir is the only FDA-approved IV antiviral drug and is approved for early treatment of uncomplicated influenza in outpatients aged ≥2 years. Peramivir single-dose pharmacokinetics were studied in children ranging in age from ≥28 days to <16 years during the 2009 H1N1 pandemic [264], and infants and children were treated on a compassionate use basis [265]. For infants and children with influenza who cannot tolerate oral therapy, IV peramivir can be considered. Intravenous zanami-vir has been evaluated in adults [251] and children [266], but is not FDA approved and is not currently available.
Geriatrics
There are no published randomized controlled clinical trials of antiviral treatment of influenza in geriatric populations. Since some elderly individuals may not be able to correctly use the inhaler device to effectively deliver zanamivir, caution should be used in prescribing inhaled zanamivir in patients with cognitive or physical limitations [267].
Pregnancy
Influenza may be associated with increased risk of adverse out-comes to the fetus and an increased risk of maternal complications and death. Observational studies suggest that early antiviral treatment provides improved clinical outcomes compared with no therapy or late initiation of antiviral treatment in hospitalized pregnant women with influenza [16, 209, 268]. However, no randomized, prospective, controlled trials of antiviral treatment in pregnant or postpartum women have been conducted to date. Oseltamivir is preferred for treatment of influenza in pregnant women over inhaled zanamivir because of concerns about lower lung volumes resulting in reduced drug distribution and concerns about bronchospasm. Oseltamivir is also preferred over IV peramivir because of the dearth of pharmacokinetic or safety data for peramivir in pregnant women [222]. Pharmacokinetic studies of oseltamivir comparing pregnant and nonpregnant women found that pregnant women have a lower systemic exposure of oseltamivir carboxylate due to increased renal filtration and secretion [269]. Based on pharmacokinetic modeling, a 30% dose increase of oseltamivir phosphate was estimated to be needed to attain comparable systemic exposure of oseltamivir carboxylate to nonpregnant women (105 mg once daily for prophylaxis and 105 mg twice daily for treatment) [270]. Therefore, higher dosing of oseltamivir can be considered, especially for pregnant women who are hospitalized with influenza complications, although there are no safety data supporting higher doses in pregnancy. Any potential benefit of higher oseltamivir dosing should be weighed against the severity of disease and the potential for unknown toxicities, and this is best done in the context of a study. The lower systemic exposure might also compromise the effectiveness of once-daily oseltamivir chemoprophylaxis.
Both oseltamivir phosphate and the metabolite oseltamivir carboxylate have been demonstrated to cross the placenta [271–276]. The safety of oseltamivir during pregnancy has been evaluated in several cohort studies and there is no evidence that oseltamivir causes harm to women or their babies [275–278]. Although oseltamivir carboxylate is detectable at low concentrations in the breastmilk of lactating women who received oseltamivir [276], the benefits of oseltamivir treatment of influenza in the mother outweigh any potential risk of exposure in the infant. There is no need to discontinue breastfeeding due to the use of oral oseltamivir.
The safety of inhaled zanamivir has been evaluated in small cohort studies, which showed no harm to pregnant women and their exposed babies [279–281]. Systemic exposure is lower in pregnancy with inhaled zanamivir than oseltamivir, and has been recommended by some experts when chemoprophylaxis of influenza is prescribed for pregnant women [222]. Zanamivir is detectable at low concentrations in breastmilk of lactating women who received inhaled zanamivir [276]. There is no need to discontinue breastfeeding due to the use of inhaled zanamivir.
There are very limited data on the safety or effectiveness of IV peramivir in pregnancy [265, 282–284]. There are also very limited data on the safety or effectiveness of the investigational drug IV zanamivir in pregnancy [285, 286]. No recommendation can be made about the use of IV peramivir or IV zanamivir in pregnant women with influenza at this time. No information is available on the use of peramivir during breastfeeding.
Immunocompromised Patients
Influenza viral replication in the respiratory tract, including asymptomatic shedding, can be prolonged, and emergence of resistant variants during or after antiviral treatment can occur more frequently in immunocompromised patients than in immunocompetent patients [134, 287–289]. There are limited data to define the optimal duration of therapy for influenza in immunocompromised patients, but retrospectively collected data suggest that treatment can safely extend to 10 days or longer. Rebound in influenza viral replication has been observed in some patients treated for 5 days, and longer duration of treatment is advisable if the disease course is severe and influenza viral RNA remains detectable. There are no data to support the use of higher doses of oseltamivir in this population. Early initiation of antiviral therapy is associated with the best outcomes [290], although clinical benefit has been reported when starting treatment >48 hours after symptom onset [291, 292].
Critical Illness
Antiviral treatment should be started as soon as possible for critically ill patients with suspected or lab oratory-confirmed influenza. Although the benefits of therapy are greatest if therapy is started within 48 hours of illness onset, there is evidence of clinical benefit with later initiation of therapy in critically ill adults [16]. Although critically ill patients may have a variety of complications that alter drug absorption and excretion (ie, altered gastrointestinal motility, renal dysfunction), most studies suggest that oral oseltamivir, when administered by nasogastric tube, results in adequate drug exposures [293]. For patients requiring extracorporeal membrane oxygenation, data suggest that no dosage adjustment of oseltamivir is needed, although dose reduction is generally needed for patients on continuous renal replacement therapy [294, 295]. Nebulization of the commercial formulation of zanamivir containing lactose should be avoided in intubated patients, given documented severe and fatal complications reported with this mode of administration [296, 297]. Patients with significant hypoxemia who are not receiving mechanical ventilation may not be able to reliably use the disk inhaler device needed to effectively deliver inhaled zanamivir.
Adequate studies have not been conducted to define which patients may benefit from therapy with an IV antiviral medication. Intravenous peramivir can be considered if there are contraindications to enteric administration of oseltamivir or if adequate bioavailability is in question. Of note, IV peramivir given once daily to hospitalized adults and children aged ≥7 years, in addition to standard of care, failed to show superiority vs placebo [298], although enrollment criteria did not exclude patients based on duration of illness. If IV peramivir is used for hospitalized patients, consideration should be given to administering a multiday dosing regimen, although the optimal regimen is unknown.
Prolonged viral replication and shedding in the upper and lower respiratory tracts may occur in critically ill patients with influenza viral pneumonia [161, 299]. Given the possibility of clinical deterioration following an initial clinical response if antivirals are stopped prior to a substantial antiviral effect, continuing antiviral treatment may be beneficial beyond 5 days, but the appropriate treatment duration has not been defined. Virologic testing in patients with a prolonged clinical course may help guide duration of antiviral treatment. Most studies have failed to demonstrate a benefit of higher doses of oseltamivir, including one RCT in hospitalized children and adults, and nonrandomized studies in hospitalized and critically ill adults [300].
Obese Populations
The volume of distribution of the metabolite oseltamivir carboxylate is not significantly different in nonobese and obese patients, and obese (including extremely obese) patients appear to have similar plasma levels as nonobese patients. This suggests standard oseltamivir dosing irrespective of weight in adults [301, 302].
Patients With Underlying Lung Disease
Because of the potential for exacerbation of reactive airway disease in influenza patients with COPD, asthma, or bronchospasm, noninhaled antiviral treatment may be safer in these individuals, although controlled studies are not available. One placebo-controlled RCT of inhaled zanamivir in influenza patients with mild to moderate asthma or COPD found adequate tolerance and symptom benefit [303]. If inhaled zan-amivir is used, bronchodilators should be readily available in case bronchospasm occurs [304].
In a Patient With Suspected or Confirmed Influenza, When Should Bacterial Coinfection of the Upper or Lower Respiratory Tract Be Considered, Investigated, and Treated?
Recommendations
-
24
Clinicians should investigate and empirically treat bacterial coinfection in patients with suspected or laboratory-confirmed influenza who present initially with severe disease (extensive pneumonia, respiratory failure, hypotension, and fever), in addition to antiviral treatment for influenza (A-II).
-
25
Clinicians should investigate and empirically treat bacterial coinfection in patients who deteriorate after initial improvement, particularly in those treated with antivirals (A-III).
-
26
Clinicians can consider investigating bacterial coinfection in patients who fail to improve after 3–5 days of antiviral treatment (C-III).
Evidence Summary
Several respiratory syndromes can be associated with either bacterial or viral pathogen infections or coinfections, including community-acquired pneumonia, sinusitis, pharyngitis, and acute otitis media. Respiratory viral infection, including influenza virus infection, can be difficult to distinguish from bacterial infection. The patient’s age, underlying medical conditions, clinical signs and symptoms, disease severity, time of the year, and known circulation of respiratory viruses in the community are important considerations for clinical management. Bacterial coinfection with influenza virus infection can be present at the time of medical evaluation or may develop later and manifest with clinical deterioration. Lower respiratory tract bacterial coinfection with influenza carries significant morbidity [122, 305, 306]. Some investigators have attributed the majority of deaths during the 1918 H1N1 pandemic to bacterial coinfection [307]. Bacterial coinfection contributed to critical and fatal illness during the 2009 H1N1 pandemic [122, 167, 308–310]. It is likely that the risk of pneumonia with bacterial coinfection varies by influenza virus strain [307, 310].
Streptococcus pneumoniae is the most common bacterial coinfection associated with influenza and pneumonia [310–314], but S. aureus, including methicillin-resistant strains [48, 315–317], and S. pyogenes coinfections have also been reported in patients with pneumonia and influenza [167, 318, 319]. Early antiviral treatment of influenza can reduce the risk of otitis media in young children and the need for antibiotic therapy for lower respiratory tract complications [189, 191, 194]. For additional guidance, see IDSA guidelines on the management of community-acquired pneumonia, S. aureus infections, and rhinosinusitis.
Guidance for the diagnosis and treatment of bacterial infection among several special populations is available, including guidance for the management of neonatal bacterial sepsis [320], sepsis among pregnant woman, infections among solid organ transplant recipients [321], and patients with human immunodeficiency virus infection (see guidelines for prevention and treatment of opportunistic infections: https://aidsinfo.nih.gov). Guidance for hospitalized patients to assess and treat those at risk of hospital-acquired bacterial pneumonia and ventilator-associated pneumonia has also been published [322–324]. Given the higher incidence of S. aureus infections, including MRSA among patients with severe pneumonia complicating influenza, agents with activity against MRSA should be included in the empiric treatment regimen for critically ill patients. There are no data to support the safety or efficacy of antibiotic chemoprophylaxis to prevent bacterial complications in patients with influenza.
Unfortunately, there are few tools or diagnostic strategies that reliably differentiate influenza virus infection alone from influenza and bacterial coinfection. Procalcitonin (PCT) and C-reactive protein (CRP) have both been used in an attempt to differentiate between bacterial and viral pneumonia. Very low levels of PCT, but not low levels of CRP, have high negative predictive value for bacterial infection, although clinical judgement is indicated [305, 309, 325]. One systematic review and meta-analysis reported that PCT tests have high sensitivity, particularly for ICU patients, but low specificity to identify bacterial coinfection in influenza patients [326]. The diagnostic value for PCT to exclude bacterial coinfection among influenza patients was reasonably high in this study [326]. One meta-analysis of data from patients with acute respiratory infections enrolled in 26 RCTs reported that procalcitonin-guided antibiotic treatment reduced 30-day mortality, antibiotic exposures, and antibiotic-related adverse effects [327].
If a Patient With Influenza Does Not Demonstrate Clinical Improvement With Antiviral Treatment or Demonstrates Clinical Deterioration During or After Treatment, What Additional Testing and Therapy Should Be Considered?
Recommendation
-
27
Clinicians should investigate other causes besides influenza virus infection in influenza patients who fail to improve or deteriorate despite antiviral treatment (A-III).
Evidence Summary
There are limited data to inform when clinical response to antiviral treatment can be expected in patients with influenza. In patients who do not demonstrate clinical improvement after at least 2–3 days of antiviral treatment, especially when treatment is initiated early in the clinical course, consideration should be given to potential alternative explanations. Development of complications should also be considered in patients with clinical deterioration (Table 9). However, lack of clinical improvement while receiving adequate antiviral treatment can occur in severely ill patients with influenza. Evaluation and management should be individualized. Specific guidance on evaluation and management of specific problems is beyond the scope of these guidelines.
Table 9.
List of Differential Diagnoses to Consider for Patients With Influenza Who Do Not Improve or Have Clinical Deterioration With Antiviral Treatmenta
| Differential Diagnoses | Supportive Tests and Clinical Clues |
|---|---|
| Inadequate NAI exposure | Inadequate antiviral dosing (oral, IV, inhaled) Inadequate bioavailability: • For oral administration (vomiting, poor compliance, esterase deficiency in converting oseltamivir phosphate to oseltamivir carboxylate) • For inhaled administration (inadequate delivery to sites of infection, poorly tolerated or poor compliance) Late initiation of NAI treatment relative to illness onset or after severe illness has occurred, with ongoing viral replication, including in the lower respiratory tract |
| Extrapulmonary complications of influenza virus infection of the respiratory tract: • Encephalopathy or encephalitis • Myocarditis, pericarditis • Myositis, rhabdomyolysis |
No other etiology identified to explain findings associated with current influenza virus infection of the upper or lower respiratory tract |
| Postinfluenza immune-mediated neurologic complications • Encephalitis or ADEM • Guillain-Barré syndrome |
No other etiology identified to explain neurologic findings associated with recent influenza virus infection of the upper or lower respiratory tract |
| Community-acquired bacterial coinfection with influenza (eg, pneumonia, otitis media, sinusitis, tracheitis, meningitis, toxic shock syndrome) | Clinical indicators, imaging studies, laboratory markers (eg, CRP procalcitionin), bacterial cultures or specific tests from sterile sites and upper/lower respiratory tract, current and prior antibiotic exposure history. Bacterial meningitis can occur during influenza virus infection or after influenza has resolved. |
| Community-acquired viral coinfection with influenza (eg, RSV, HMPV, adenovirus) | Multiple viruses can be detected by multiplex respiratory viral PCR testing. |
| Hospital-acquired infectionb (bacterial, viral, fungal), DIC, septic shock | • Ventilator-associated pneumonia • Healthcare-associated pneumonia • Catheter-related bloodstream infection • Catheter-associated UTI |
| NAI-resistant influenza virus infection | Persistent virus detection during or after NAI therapyc; detection of molecular marker(s) associated with NAI resistance; or notification of community circulation of NAI-resistant viruses (testing per guidance) |
| Respiratory failure, ARDS with influenza | Lower respiratory tract complications can occur without bacterial coinfection. Respiratory failure and ARDS can occur with or without bacterial coinfection of the lower respiratory tract |
| Multiorgan dysfunction or failure (respiratory failure, acute kidney injury, or renal failure), DIC, septic shock | Clinical indicators, imaging studies, laboratory markers (eg, CRP) |
| Cardiovascular event: MI, angina, arrhythmias | Clinical indicators, imaging studies, laboratory markers |
| Pulmonary event: poor control of underlying comorbid condition (eg, COPD, heart failure), pulmonary embolism | Clinical indicators, imaging studies |
| Cerebrovascular events: CVA | Imaging studies, neurological assessment |
| Immune deficiency with inadequate antiviral response (eg, chemotherapy or other immunosuppression, pregnancy) | Clinical history and appropriate laboratory tests |
| Reye syndrome | Hyperammonemia, hypoglycemia, fatty liver, altered mental status (especially if the patient received salicylates or was on long-term aspirin therapy) |
| Immunocompromised host-specific syndromes | Rejection, hemolytic uremic syndrome, sirolimus pneumonitis/serositis |
Abbreviations: ADEM, acute disseminated encephalomyelitis; ARDS, acute respiratory distress syndrome; CRP C-reactive protein; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; DIC, disseminated intravascular coagulation; HMPV, human metapneumovirus; IV, intravenous; MI, myocardial infarction; NAI, neuraminidase inhibitor; PCR, polymerase chain reaction; RSV, respiratory syncytial virus; UTI, urinary tract infection.
If an obvious alternative source is not identified, consider other sites of infection (eg, aspiration in neurologically impaired, endocarditis, Clostridium difficile colitis)
Nosocomial influenza virus infection can complicate other conditions requiring hospitalization.
Persistent detection of influenza viral RNA after antiviral treatment does not necessarily indicate that antiviral-resistant virus infection is present.
There are some patient population-specific issues to consider:
Pediatric populations: Influenza morbidity and hospitalization rates are much higher in children aged <2 years than in older children and young adults, likely due to the immature immune system in young children and lack of previous exposure and immunity to circulating influenza viruses [328, 329]. Extrapulmonary complications of influenza such as myocarditis, myositis, and encephalitis can occur in previously healthy children.
Pregnant women: Metabolism of oseltamivir is increased in pregnancy, reducing exposure to oseltamivir carboxylate by 30% compared to nonpregnant women [269, 270]. Some experts have suggested consideration of higher oseltamivir dosing. Deterioration to respiratory failure and ARDS in pregnant women with influenza may necessitate emergency cesarean delivery in the ICU [234].
Immunocompromised patients: Lung transplant and HSCT recipients may be more susceptible to development of influenza viral pneumonia, in addition to bacterial and fungal coinfections. Management should include involvement of an infectious diseases physician competent in infectious diseases in transplant recipients, if available. Data on colonizing respiratory tract flora in lung transplant patients should help to inform empiric antibiotic coverage. Immunosuppressed patients, especially HSCT patients, who are treated with NAIs are more likely to experience emergence of antiviral resistance during or after therapy in part due to a poor host response, with prolonged influenza virus replication [134]. However, prolonged replication of influenza viruses in the respiratory tract can occur in such patients without emergence of antiviral resistance. Antiviral resistance is discussed in the next section. Clinicians should be aware that adverse events associated with immunosuppressive agents may result in clinical deterioration in severely immunosuppressed patients. For example, pneumonitis has been reported with multiple immunosuppressive drugs, including in patients receiving mammalian target of rapamycin (mTOR) inhibitors such as sirolimus or everolimus [330, 331].
When Should Testing Be Done for Infection With an Antiviral-resistant Influenza Virus?
Recommendations
-
28Influenza NAI resistance testing can be considered for:
- Patients who develop laboratory-confirmed influenza while on or immediately after NAI chemoprophylaxis (C-III).
- Patients with an immunocompromising condition and evidence of persistent influenza viral replication (eg, after 7–10 days, demonstrated by persistently positive RT-PCR or viral culture results) and remain ill during or after NAI treatment (B-III).
- Patients with laboratory-confirmed influenza who inadvertently received subtherapeutic NAI dosing and remain ill (C-III).
- Patients with severe influenza who do not improve with NAI treatment and have evidence of persistent influenza viral replication (eg, after 7–10 days) (C-II).
-
29
Clinicians should remain informed on current CDC and WHO surveillance data on the frequency and geographic distribution of NAI-resistant influenza viruses during influenza season, and with the latest CDC antiviral treatment recommendations (A-III).
Evidence Summary
Influenza virus resistance to NAI drugs is detected infrequently in clinically significant situations [246]. A patient may be infected with NAI-resistant influenza virus circulating in the community, or resistance may develop during therapy. In the first situation, the patient will not respond to appropriate therapy, and in the second, clinical deterioration may occur following an initial response. The emergence of NAI resistance during antiviral chemoprophylaxis or treatment has been reported uncommonly in immunocompetent patients [189, 246, 332–334]. In contrast, NAI resistance has been reported among severely immunocompromised patients more frequently than immunocompetent patients during prolonged influenza viral replication and antiviral treatment, and after postexposure antiviral chemoprophylaxis [289, 335–342]. Patients who received subtherapeutic NAI dosing and who remain ill with laboratory-confirmed influenza might be at increased risk of emergence of NAI-resistant virus, although the risk is likely higher in severely immunocompromised patients. While some studies have suggested that young children with uncomplicated influenza may also be at higher risk for the emergence of drug resistance during or after NAI use based on molecular detection methods, presumably due to longer viral shedding, no effect on illness resolution has been reported [246, 333, 334, 343].
If there is clinical suspicion of antiviral resistance as the cause of failure to improve or clinical deterioration, it is critical to consider a change in NAI treatment and to perform testing to confirm the presence of continued viral replication and to document resistance. NAI resistance can vary among influenza viruses and the specific NAI being used. The most commonly detected molecular marker of resistance is the H275Y substitution in viral neuraminidase in A(H1N1)pdm09 and other N1-containing influenza A viruses, which confers highly reduced susceptibility to oseltamivir and reduced susceptibility to peramivir while maintaining susceptibility to zanamivir [344, 345]. Less common molecular markers of resistance that have been reported include the E119E/V and R292K substitutions in the neuraminidase of A(H3N2) and avian influenza A(H7N9) viruses, which confer highly reduced susceptibility to oseltamivir [250, 346]. R292K confers reduced susceptibility to all licensed NAIs, much greater for oseltamivir than zanamivir, and should prompt consultation with an infectious disease specialist. Currently, only testing for the H275Y marker in A(H1N1)pdm09 viruses is available commercially. Comprehensive testing for molecular markers associated with NAI resistance requires specialized assays that may be available at some public health and academic laboratories.
In general, influenza patients who were treated with oseltamivir and are suspected of developing oseltamivir resistance should be switched to inhaled zanamivir, unless contraindicated. Inhaled zanamivir is FDA approved for children aged ≥5 years for chemoprophylaxis and ≥7 years for treatment, but there are limited options for treating oseltamivir-resistant virus. Clinicians should evaluate the ability to reliably use inhaled zanamivir in children 5–7 years old. Consultation should be sought with an expert on management of patients with antiviral-resistant influenza virus infection.
There are no randomized trials to inform the optimal management of patients infected with influenza viruses with resistance to NAIs. Two studies conducted during 2008–2009 when H275Y H1N1 virus variants (oseltamivir resistant, but amantadine and zanamivir susceptible) circulated in the community suggested that treatment with zanamivir or a related drug, lani-namivir, had superior clinical outcomes compared to oseltamivir [347, 348]. Most of the available clinical data from patients with resistant virus infections that emerged during treatment are derived from case reports and case series in which patients on oseltamivir treatment were switched to other antivirals often late in the clinical course of their illness [285, 286, 340, 349–353]. The best outcomes appear to be associated with early change in antiviral therapy to an agent with in vitro activity against the oseltamivir-resistant influenza virus. Combination antiviral therapy with 2 or more active agents with different mechanisms of action is an investigational approach that may reduce the development of additional de novo resistance in immunocompromised patients and other patients at higher risk for the emergence of resistant viruses during or after therapy [354, 355]. Use of convalescent plasma or intravenous immunoglobulin (IVIg) that contains neutralizing antibodies [356, 357], as well as other antiviral agents (eg, polymerase inhibitors baloxavir marboxil, pimodivir, favipiravir), are under investigation.
Community Circulation of Antiviral-Resistant Influenza Viruses
Currently, circulation of NAI-resistant influenza viruses is rare, although limited community circulation of oseltamivir-resistant A(H1N1)pdm09 viruses has been reported in several countries [358–360]. The CDC and WHO perform ongoing assessment of the antiviral susceptibility of circulating influenza viruses [349]; updated summaries of US data are available at https://www.cdc.gov/flu/weekly/summary.htm. If circulation of NAI- resistant influenza viruses increases in prevalence, updated guidance will be available from the CDC.
Should Adjunctive Therapy Be Administered to Patients With Suspected or Confirmed Influenza?
Recommendations
-
30
Clinicians should not administer corticosteroid adjunctive therapy for the treatment of adults or children with suspected or confirmed seasonal influenza, influenza-associated pneumonia, respiratory failure, or ARDS, unless clinically indicated for other reasons (A-III).
-
31
Clinicians should not routinely administer immunomodulation using immunoglobulin preparations such as IVIg for treatment of adults or children with suspected or confirmed seasonal influenza (A-III).
Evidence Summary
Corticosteroid Therapy
While current evidence is limited, corticosteroid treatment of influenza patients should be avoided unless clinically indicated for other reasons (eg, exacerbation of asthma, COPD, low-dose hydrocortisone for adrenal insufficiency or refractory septic shock), as the risks of corticosteroid treatment are not balanced by a documented clinical benefit in the treatment of influenza [361]. For those who require corticosteroid therapy, systematically collected data on clinical and virologic response to antiviral therapy from randomized prospective trials are not available; these patients may not respond to antiviral treatment as expected in otherwise healthy populations.
Data from randomized controlled clinical trials of corticosteroid treatment of influenza patients are not available. One RCT of corticosteroid treatment of mechanically ventilated adults with influenza A(H1N1)pdm09 virus infection did not complete enrollment [362]. One RCT of hydrocortisone treatment of mechanically ventilated adults with septic shock of multiple infectious etiologies reported no significant difference in 90-day morality vs placebo [363]. Two meta-analyses of methodologically weaker observational studies (including concurrent antiviral treatment for most patients) reported that despite the limitations of the included studies, corticosteroid treatment of hospitalized influenza patients appeared to be associated with increased mortality, but firm conclusions were not possible due to lack of information on dosing, or indication for corticosteroid treatment [364, 365]. An additional meta-analysis of published observational studies suggested that not only was mortality increased, but also nosocomial bacterial infection, duration of mechanical ventilation, and ICU stay were greater in corticosteroid-treated patients (patient ages not reported) with suspected or confirmed influenza [366].
Most observational studies of corticosteroid treatment of hospitalized patients have been reported in adults [199, 367, 368]. One observational study reported that early corticosteroid treatment (within 72 hours of illness onset) of patients with influenza A(H1N1)pdm09 virus infection was associated with increased mortality [369]. In 2 observational studies that utilized propensity scoring to adjust for confounding by treatment assignment, corticosteroid treatment of critically ill adults with influenza A(H1N1)pdm09 virus infection was associated with longer duration of mechanical ventilation and increased mortality [367, 368]. One observational study of critically ill children with influenza A(H1N1)pdm09 virus infection reported that those who received high-dose corticosteroids had an elevated risk of death compared to those not treated with high-dose corticosteroids [308].
One large retrospective observational study not included in any meta-analyses reported data for 607 adults hospitalized with influenza A(H1N1)pdm09 in 51 Canadian ICUs [370]. In-hospital mortality was significantly higher in patients treated with corticosteroids in crude and multivariable analyses; however, further analyses using propensity scoring matching, and adjusting for time-dependent between-group differences during ICU admission, did not demonstrate significant differences in mortality between patients treated with and without corticosteroids, demonstrating the need to control for covariates that may impact survival [370]. Another large observational study, not included in any meta-analyses, of 2141 adolescents and adults hospitalized with influenza A(H1N1)pdm09 viral pneumonia in China used propensity score-matched case-control analysis. Low- to moderate-dose (25–150 mg/day methylprednisolone or equivalent), but not higher-dose, corticosteroid treatment was associated with lower 30-day mortality compared with no treatment (adjusted hazard ratio [aHR], 0.64; 95% CI, .43–.96; P = .033) [371]. In patients with mild or worse hypoxemia (partial pressure of arterial oxygen/fraction of inspired oxygen [PaO2/FIO2] <300 mm Hg), low-to moderate-dose, but not high-dose, corticosteroid treatment significantly reduced 30-day and 60-day mortality [371]. However, in patients with mild disease (PaO2/FIO2 ≥300 mm Hg), corticosteroid treatment was not associated with survival benefit, and was associated with higher 60-day mortality.
A case-control study from China analyzed corticosteroid use in hospitalized adults with avian influenza A(H7N9) virus infection from 84 cities within 16 provinces using propensity score matching with multivariable Cox regression [372]. Mortality at 60 days was higher in patients who received corticosteroids compared with those who did not (aHR, 1.98; 95% CI, 1.03–3.79; P = .04). In this study, a subgroup analysis demonstrated that patients who received high doses (>150 mg/ day methylprednisolone or equivalent) had much higher 30-day and 60-day mortality than those who received no steroid therapy (P = .031 and P = .002, respectively) [372]. There was no significant impact on mortality for patients who received low to moderate doses of corticosteroids compared with matched controls without corticosteroid treatment.
Multiple observational studies have reported that corticosteroid treatment was associated with prolonged influenza viral shedding [373–375], including A(H7N9) viral shedding and emergence of antiviral resistance [346], and secondary bacterial and invasive fungal coinfections [199, 376–378].
Passive Immunotherapy
Immunotherapy with plasma, immune serum globulin, or IVIg can result in immune-modulating as well as virus neutralizing activity. Following infection, influenza virus strain-specific antiviral activity is present in convalescent plasma of immunocompetent persons. During the 2009 H1N1 pandemic, a prospective cohort study in Hong Kong reported that treatment with convalescent plasma containing virus-specific neutralizing antibodies reduced respiratory tract A(H1N1)pdm09 viral load, serum cytokine response, and mortality compared with untreated patients [379]. In a multicenter, prospective, double-blind, randomized controlled trial of hyperimmune IVIg for severe illness with influenza A(H1N1)pdm09 virus infection (17 received hyperimmune IVIg from persons who recovered from laboratory-confirmed influenza A(H1N1)pdm09 virus infection, 18 received IVIg created from donors prior to the pandemic as a control group), hyperimmune IVIg treatment was associated with significant reduction in respiratory tract viral load and mortality [357]. An open-label multicenter RCT of convalescent or postimmunization plasma (containing variable concentrations of hemagglutinin inhibition antibodies) treatment plus standard care vs standard care alone in hospitalized children and adults with laboratory-confirmed influenza did not find significant clinical benefit or antiviral effects, but convalescent plasma was well-tolerated, and a phase 3 trial is under way [380].
Additional research from randomized controlled trials to confirm these findings and to assess the contributions of immunomodulation vs antiviral activity are needed before recommendations can be made for administration of convalescent plasma, IVIg, or other immunoglobulin preparations to patients with severe influenza.
Other Immunomodulatory Agents
Studies of other drugs with immune-modulating activity, such as the hydroxy-methylglutaryl-coenzyme A reductase inhibitors (statins), have been proposed as adjunctive therapy for influenza, but no prospective data are available on which to make recommendations [381]. An open-label, randomized controlled trial of oseltamivir and azithromycin vs oseltamivir alone for treatment of adults hospitalized with laboratory-confirmed influenza in Hong Kong reported that oseltamivir and azithromycin treatment significantly reduced several proinflammatory cytokines compared with oseltamivir alone [382]. One open-label randomized controlled trial of a combination of clarithromycin, naproxen, and oseltamivir vs oseltamivir alone for early treatment of elderly patients hospitalized with laboratory-confirmed influenza reported that the combination significantly reduced 30-day mortality [383]. Further randomized controlled trials of adjunctive macrolide antibiotic treatment and nonsteroidal anti-inflammatory drugs are needed before recommendations can be made.
ANTIVIRAL CHEMOPROPHYLAXIS IN COMMUNITY SETTINGS
Who Should Be Considered for Antiviral Chemoprophylaxis to Prevent Influenza in the Absence of Exposure or an Institutional Outbreak (Preexposure Chemoprophylaxis)?
Recommendations
Antiviral drugs should not be used for routine or widespread chemoprophylaxis outside of institutional outbreaks; antiviral chemoprophylaxis can be considered in certain situations:
-
32
Clinicians can consider antiviral chemoprophylaxis for the duration of the influenza season for adults and children aged ≥3 months who are at very high risk of developing complications from influenza and for whom influenza vaccination is contraindicated, unavailable, or expected to have low effectiveness (eg, persons who are significantly immunocompromised) (C-II).
-
33
Clinicians can consider antiviral chemoprophylaxis for the duration of the influenza season for adults and children aged ≥3 months who have the highest risk of influenza-associated complications, such as recipients of HSCT in the first 6–12 months posttransplant and lung transplant recipients (B-II).
-
34
Clinicians can consider short-term antiviral chemoprophylaxis in conjunction with prompt administration of inactivated influenza vaccine for unvaccinated adults and children aged ≥3 months who are at high risk of developing complications from influenza in whom influenza vaccination is expected to be effective (but not yet administered) when influenza activity has been detected in the community (C-II).
-
35
Clinicians can consider short-term antiviral chemoprophylaxis for unvaccinated adults, including healthcare personnel, and for children aged ≥3 months who are in close contact with persons at high risk of developing influenza complications during periods of influenza activity when influenza vaccination is contraindicated or unavailable and these high-risk persons are unable to take antiviral chemoprophylaxis (C-III).
-
36
Clinicians can consider educating patients and parents of patients to arrange for early empiric initiation of antiviral treatment as an alternative to antiviral chemoprophylaxis (C-III).
Which Antiviral Drugs Should Be Used for Preexposure Chemoprophylaxis for Influenza?
Recommendation
-
37
Clinicians should use an NAI (oral oseltamivir or inhaled zanamivir) if preexposure chemoprophylaxis for influenza is administered rather than an adamantane antiviral (A-II).
What Is the Duration of Preexposure Antiviral Chemoprophylaxis to Prevent Influenza?
Recommendations
-
38
Clinicians should administer preexposure antiviral chemoprophylaxis for adults and children aged ≥3 months who are at very high risk of developing complications from influenza (eg, severely immunocompromised persons such as HSCT recipients) and for whom influenza vaccination is contraindicated, unavailable, or expected to have low effectiveness, as soon as influenza activity is detected in the community and continued for the duration of community influenza activity (A-II).
-
39
Clinicians should test for influenza and switch to antiviral treatment dosing in persons receiving preexposure antiviral chemoprophylaxis who become symptomatic, preferably with an antiviral drug with a different resistance profile if not contraindicated (A-II).
Which Asymptomatic Persons Exposed to Influenza Should Be Considered for Postexposure Antiviral Chemoprophylaxis in a Noninstitutional Setting?
Recommendations
-
40
Clinicians can consider postexposure antiviral chemoprophylaxis for asymptomatic adults and children aged ≥3 months who are at very high risk of developing complications from influenza (eg, severely immunocompromised persons) and for whom influenza vaccination is contraindicated, unavailable, or expected to have low effectiveness after household exposure to influenza (C-II).
-
41
Clinicians can consider postexposure antiviral chemoprophylaxis (in conjunction with influenza vaccination) for adults and children aged ≥3 months who are unvaccinated and are household contacts of a person at very high risk of complications from influenza (eg, severely immunocompromised persons), after household exposure to influenza (C-II).
-
42
Clinicians can consider educating patients and arranging for early empiric initiation of antiviral treatment as an alternative to postexposure antiviral chemoprophylaxis (C-III).
When Should Postexposure Antiviral Chemoprophylaxis Be Started?
Recommendations
-
43
If chemoprophylaxis is given, clinicians should administer postexposure antiviral chemoprophylaxis as soon as possible after exposure, ideally no later than 48 hours after exposure (A-III).
-
44
Clinicians should not administer once-daily postexposure antiviral chemoprophylaxis if >48 hours has elapsed since exposure. Full-dose empiric antiviral treatment should be initiated as soon as symptoms occur, if treatment is indicated (A-III).
How Long Should Postexposure Antiviral Chemoprophylaxis Be Given?
Recommendations
-
45
Clinicians should administer postexposure antiviral chemoprophylaxis in a nonoutbreak setting for 7 days after the most recent exposure to a close contact with influenza (A-III).
-
46
Clinicians should test for influenza and switch to antiviral treatment dosing in persons receiving postexposure antiviral chemoprophylaxis who become symptomatic, preferably with an antiviral drug with a different resistance profile if not contraindicated (A-III).
Which Antiviral Drugs Should Be Used for Postexposure Chemoprophylaxis?
Recommendation
-
47
Clinicians should administer an NAI (inhaled zanamivir or oral oseltamivir) if postexposure chemoprophylaxis for influenza is given, rather than an adamantane antiviral (A-II).
Evidence Summary
Nine randomized controlled clinical trials [206, 384–391] and 2 meta-analyses [392, 393] have demonstrated that preexposure or postexposure antiviral chemoprophylaxis with an NAI (oral oseltamivir or inhaled zanamivir) decreases the likelihood of developing symptomatic laboratory-confirmed influenza. Three of these randomized trials evaluated preexposure NAI chemoprophylaxis. In one study, oral oseltamivir was 74% effective (95% CI, 53%−88%; attack rate, 4.8% vs 1.3%) in preventing symptomatic laboratory-confirmed influenza when given to predominantly healthy unvaccinated adults for 42 days [384]. In another, inhaled zanamivir given for 28 days was 84% effective (95% CI, 55%−94%; attack rate, 3.4% vs 0.5%) for symptomatic laboratory-confirmed influenza and 67% effective (95% CI, 39%−83%) against laboratory-confirmed influenza meeting a strict case definition [385]. Among 3363 adults and adolescents at high risk of influenza complications, inhaled zanamivir for 28 days was 83% effective (95% CI, 56%−93%) at preventing symptomatic laboratory-confirmed influenza [391].
A single study evaluated oseltamivir chemoprophylaxis for 12 weeks in solid organ and HSCT recipients. There was no significant difference in the primary endpoint, laboratory-confirmed clinical influenza, in the intent-to-treat population (2.9% vs 2.1%; 95% CI, −2.3 to 4.1; efficacy, 28%); a borderline significant benefit was detected in a secondary analysis using RT-PCR and excluding patients who were RT-PCR positive at study entry (3.0% vs 0.04%; 95% CI, .1–5.7; efficacy, 86%) [394].
Oseltamivir chemoprophylaxis is associated with a modest increase in upper gastrointestinal symptoms; 12% and 15% when used once or twice daily respectively, significantly more frequent than among placebo recipients (5%) [384]. The rate of reported adverse events among patients using inhaled zanamivir for extended chemoprophylaxis was not different than among those using a placebo inhaler [384]. A study of extended (16 weeks) oral oseltamivir or inhaled zanamivir chemoprophylaxis vs placebo among Thai healthcare personnel reported no significant differences in adverse events and no withdrawals by drug recipients [395].
When considering whether to use extended antiviral chemoprophylaxis during seasonal influenza epidemics, it is important to appreciate that absolute risk reductions were modest and the number needed to treat (NNT) in studies conducted to date were high. This varied with influenza vaccine use and severity of seasonal influenza epidemics. Oseltamivir chemoprophylaxis given once or twice daily vs placebo for 6 weeks reduced laboratory-confirmed influenza by 3.5% in an unvaccinated adult population (from 4.8% to 1.3%; NNT to prevent one case of laboratory-confirmed symptomatic influenza, 29) [384]. Zanamivir chemoprophylaxis for 6 weeks vs placebo in unvaccinated adults resulted in a 3% reduction in laboratory-confirmed influenza with fever (3.4% to 0.5%; NNT, 33) [385], and a 1.2% reduction when used for 28 days vs placebo in high-risk adolescents and adults (1.4% to 0.2%; NNT, 83] [391]. The risk of severe complications and death from influenza varies significantly among groups at high risk for complications, so the expected benefit in preventing severe complications varies. The risk of death from influenza is highest among HSCT and lung transplant patients [396, 397]. Decisions on extended duration of antiviral chemoprophylaxis for severely immunocompromised patients such as HSCT recipients should consider issues such as the potential for emergence of antiviral-resistant influenza viruses as well as tolerability and absorption issues for those with gastrointestinal graft-vs-host disease.
Several studies have evaluated the efficacy of postexposure antiviral chemoprophylaxis for household members after influenza diagnosis in a household member [386–390]. Two trials evaluated oseltamivir; one included adolescents aged ≥13 years and adults [388], and the other included children aged >1 year as well as adults [390]. The pooled efficacy against laboratory-confirmed symptomatic influenza was 81% (95% CI, 55%- 92%) [398]. A subgroup analysis of the efficacy in children demonstrated 64% efficacy (95% CI, 16%−85%) [390]. Three trials evaluated postexposure antiviral chemoprophylaxis with inhaled zanamivir; 2 included children older than 5 years and adults [387, 389], and one trial was restricted to persons aged 13–65 years [386]. All showed statistically significant protection; the pooled estimate of efficacy against laboratory-confirmed symptomatic influenza for the 3 trials was 79% (95% CI, 67%−87%) [398]. Absolute risk reductions were modest. Data on the ability of postexposure antiviral chemoprophylaxis to prevent serious complications of influenza are not available, although reductions in symptomatic influenza cases would be expected to also reduce the risk of complications. To reduce the risk of subtherapeutic dosing if influenza virus infection has occurred following exposure, antiviral treatment (twice-daily dosing) rather than once-daily chemoprophylaxis dosing has been recommended by some experts, particularly in immunocompromised patients, when postexposure antiviral chemoprophylaxis is indicated. This may also be appropriate if >48 hours has elapsed since exposure, as the patient may already have infection established, warranting full-dose therapy. No studies have adequately evaluated this strategy. Decisions on whether to administer postexposure antiviral chemoprophylaxis should consider the nature of the exposure, the exposed person’s risk of developing complications from influenza, the ability to promptly administer antiviral therapy if symptoms develop, advice from public health authorities, and clinical judgment.
Although older studies demonstrated efficacy of adamantanes (amantadine and rimantadine) for chemoprophylaxis, the use of adamantanes is not recommended because of widespread adamantane resistance among circulating influenza A viruses [249, 399, 400], the inherent resistance of influenza B viruses to adamantanes, and the rapid emergence and transmission of adamantane-resistant influenza A viruses during adamantane treatment. NAI resistance remains relatively uncommon in currently circulating influenza virus strains. However, during the 2008–2009 season, an oseltamivir-resistant H1N1 virus strain (susceptible to both adamantane and zanamivir) became the predominant circulating strain worldwide [401, 402]. Since then, sporadic cases and clusters of oseltamivir-resistant influenza A(H1N1)pdm09 virus infection have been detected annually [399, 403–405]. The development of oseltamivir resistance during chemoprophylaxis has been reported, usually with the H275Y mutation, with limited ongoing transmission of resistant virus [96, 336, 358, 406]. Thus, if a patient develops influenza during oseltamivir chemoprophylaxis, inhaled zanamivir can be considered for treatment if there are no contraindications.
The decision to use antiviral chemoprophylaxis must balance the knowledge of the prevalence of antiviral resistance among circulating influenza viruses (see http://www.cdc.gov/flu/pro-fessionals/index.htm), risk of emergence of resistance, risk of severe complications of influenza, the potential for side effects, and the ability to initiate early therapy for influenza. Influenza vaccination is the primary tool to prevent influenza. Antiviral chemoprophylaxis is not a substitute for influenza vaccination. Educating patients and arranging for early empiric initiation of antiviral therapy if influenza symptoms develop may be an effective alternative to postexposure antiviral chemoprophylaxis, but studies comparing these 2 approaches have not been conducted.
INSTITUTIONAL OUTBREAK CONTROL
When Is There Sufficient Evidence of an Influenza Outbreak in a Long-term Care Facility or Hospital to Trigger Implementation of Control Measures Among Exposed Residents or Patients and Healthcare Personnel to Prevent Additional Cases of Influenza?
Recommendations
-
48
Active surveillance for additional cases should be implemented as soon as possible when one healthcare-associated laboratory-confirmed influenza case is identified in a hospital or one case of laboratory-confirmed influenza is identified in a long-term care facility (A-III).
-
49
Outbreak control measures should be implemented as soon as possible, including antiviral chemoprophylaxis of residents/patients, and active surveillance for new cases, when 2 cases of healthcare-associated laboratory-confirmed influenza are identified within 72 hours of each other in residents or patients of the same ward or unit (A-III).
-
50
Implementation of outbreak control measures can be considered as soon as possible if one or more residents or patients has suspected healthcare-associated influenza and results of influenza molecular testing are not available on the day of specimen collection (B-III).
Evidence Summary
Data are limited to inform recommendations regarding when an influenza outbreak should be declared in a long-term care facility or hospital, and on the effectiveness of interventions to prevent or control institutional influenza outbreaks. Observational studies have used different definitions for declaring an influenza outbreak on a single ward, including (i) 2 cases of ILI with one laboratory-confirmed influenza case, over a 3-day period, or 3 ILI cases with one laboratory-confirmed influenza case, over a 7-day period; (ii) 2 cases of acute respiratory illness occurring in 48 hours; (iii) 10% of residents on a nursing unit with acute respiratory illness in a 7-day period with influenza virus isolated from a resident in the facility; and (iv) 2 cases of laboratory-confirmed influenza occurring in a 5-day period [407–413].
Early detection of influenza outbreaks in long-term care facilities and hospitals is important because influenza virus transmission can occur rapidly, with high attack rates [412–418], and because the risk of complications and mortality from influenza is higher than in other high-risk groups for frail older adults, severely disabled persons of any age, and immunocompromised patients [79, 419–423]. However, early detection of influenza is often difficult because severely handicapped persons and frail older adults may not present with typical influenza signs and symptoms [90] and because many residents with neurocognitive impairment or dementia may not be able to describe or complain of symptoms. The difficulty of identifying influenza in residents of long-term care facilities means that undetected cases may be present coincident with the detection of the first confirmed influenza case.
Although laboratory testing of additional suspected cases is the most definitive means to confirm an outbreak, waiting for laboratory testing results may delay outbreak control measures. A negative result of an influenza test with low to moderate sensitivity may be falsely negative and does not exclude a diagnosis of influenza; therefore, use of highly sensitive molecular assays is recommended for influenza testing. When the results of influenza molecular testing will not be available until the next day, outbreak control measures should be instituted when a single laboratory-confirmed case of influenza is accompanied by influenza activity in the community and by 2 or more other residents with symptoms compatible with influenza.
There are no data available that provide an estimate of how often a single identified laboratory-confirmed influenza case represents the start of an influenza outbreak. Evidence from several observational studies demonstrates that higher influenza vaccination coverage is associated with a lower risk of influenza outbreaks [424–429]. Although no other factors have been demonstrated to be associated with the risk of outbreaks, biological plausibility and expert opinion suggest that volume and patterns of air flow, degree of crowding in rooms or public areas, the effectiveness of policies excluding ill visitors and ill staff, and the ability to reduce interresident and staff contact in response to a single identified influenza case may all influence whether introduction of a single case of influenza will result in an outbreak [430]. These factors should be considered when judging whether a single confirmed influenza case represents the beginning of an outbreak. The ability to rapidly identify other cases—the combination of a sensitive surveillance case definition and use of RT-PCR testing of upper respiratory tract specimens for laboratory diagnosis—can reduce the risk that additional, undetected influenza cases are present at the time the first case is diagnosed and help to ensure early detection of influenza virus transmission if an outbreak has started [431].
The identification of one healthcare-associated laboratory-confirmed influenza virus infection in a long-term care resident should prompt a careful review to identify other undiagnosed cases, as well as an assessment of the likelihood of influenza virus transmission and the need to institute outbreak control measures. Staff at facilities with low influenza vaccination coverage among staff and/or residents, lack of surveillance for acute respiratory illness in residents, <6 air changes per hour, many multibed shared rooms, crowded dining and activity rooms, and multiple frequent visitors who are not adequately screened for illness symptoms should consider early and rapid implementation of outbreak control measures after a single laboratory-confirmed influenza case.
Hospital units with longer length-of-stay patients (eg, rehabilitation units, transplant units) and skilled nursing facilities are relatively closed environments with high-risk patient populations and are similar to long-term care facilities for the elderly [417, 432, 433]. The threshold for declaring an outbreak in hospital units with longer-stay patients should be the same as that in long-term care facilities for the elderly. One pertinent difference to note is the challenge associated with identifying whether cases of influenza with onset within 72–96 hours of hospital admission are acquired in the hospital vs community acquired with onset after admission, because the incubation period for influenza ranges from 1 to 4 days.
Which Residents/Patients Should Be Considered to Have Influenza and Be Treated With Antivirals During an Influenza Outbreak in a Long-term Care Facility or Hospital?
Recommendations
-
51
When an influenza outbreak has been identified in a long-term care facility or hospital, influenza testing should be done for any resident/patient with one or more acute respiratory symptoms, with or without fever, or any of the following without respiratory symptoms: temperature elevation or reduction, or behavioral change (A-III).
-
52
Empiric antiviral treatment should be administered as soon as possible to any resident or patient with suspected influenza during an influenza outbreak, without waiting for the results of influenza diagnostic testing (A-III).
Evidence Summary
Ascertainment of influenza symptoms may be challenging in residents or patients with developmental disabilities, with severe neurologic impairment or dementia, or who are nonverbal. Older adults may not always mount a fever with influenza, and behavioral change may be the only sign of influenza virus infection in some frail elderly persons [76]. Hospitalized children and adults with chronic illness who develop nosocomial influenza may not initially manifest typical influenza signs and symptoms [434, 435]. Therefore, during an institutional influenza outbreak, there should be a low threshold for suspecting influenza and initiating antiviral treatment without waiting for the results of influenza molecular testing. Although early antiviral treatment of persons with influenza may reduce the risk of influenza virus transmission to exposed close contacts, the magnitude of this effect is unknown, and therefore other control measures also should be implemented as soon as possible (Table 10). Since not all persons who receive a 5-day antiviral treatment course without laboratory confirmation of influenza actually had influenza virus infection or can mount an immune response, antiviral chemoprophylaxis should be resumed after treatment is completed if chemoprophylaxis is continued for ongoing influenza exposures of other residents on their unit/ward.
Table 10.
Control Measures for Managing Institutional Influenza Outbreaks
| Level | Control Measures |
|---|---|
| Resident level | • Identify and isolate all ill residents or patients with suspected or laboratory-confirmed influenza; encourage ill residents to stay in their rooms as much as possible • Ask ill residents or patients with suspected or laboratory-confirmed influenza to wear facemasks when out of their rooms • Promptly identify influenza virus infection in residents and initiate antiviral treatment in suspected or confirmed influenza cases as soon as possible • Encourage and facilitate frequent hand washing • Educate residents or patients and their families on respiratory etiquette • Arrange beds in rooms housing >1 resident to maximize distance between the heads of beds to at least 2 meters or approximately 6 feet • Once an influenza outbreak is declared (when 2 cases of laboratory-confirmed influenza are identified within 72 hours of each other in residents or patients of the same ward or unit), start empiric antiviral treatment of newly symptomatic residents with a neuraminidase inhibitor as soon as possible |
| Ward/unit level | • Implement droplet precautions when providing care for ill residents or patients, in addition to standard precautions already in place regardless of symptoms. • Cohort ill residents by rooming together, or in group activities such as dining or recreation • Post signs diverting nonessential visits • Minimize or restrict staff working on affected wards from working on nonaffected wards • Post signs to remind staff and visitors to wash hands, wear facemasks, and to adhere to standard, contact, and droplet precautions when entering rooms of ill residents or patients • Add distance between individuals during mealtimes and activities, eg, eating just outside of or in their rooms rather than a common dining area • Keep residents on their wards; prohibit or, as feasible, limit and do not overlap movement of residents of affected wards to nonaffected wards or common areas • Once an outbreak is declared, administer empiric antiviral chemoprophylaxis with a neuraminidase inhibitor as soon as possible to asymptomatic exposed residents on the affected ward or unit • Close affected wards to new admissions • Once an influenza outbreak is declared, consider whether to offer empiric antiviral chemoprophylaxis with a neuraminidase inhibitor to unvaccinated staff on the affected ward/unit, including staff with influenza vaccine contraindications or immunocompromised staff (who are expected to have poor immune response to vaccination) for the duration of the outbreak • If there is substantial antigenic drift between circulating influenza viruses and influenza vaccine virus strains, consider whether to extend empiric antiviral chemoprophylaxis with a neuraminidase inhibitor to all staff on the affected ward/unit with an influenza outbreak, regardless of influenza vaccination status |
| Building level | • Cohorting of ill persons if isolation or nursing unit-level cohorting is not possible at the building level in multibuilding facilities • Once an influenza outbreak is declared, consider whether to offer empiric neuraminidase inhibitor chemoprophylaxis and treatment to all staff working in buildings with residents having new respiratory illness, not just on the affected unit(s)/ward(s) |
| Institution level | • Have annual influenza vaccination programs in place for residents or patients and healthcare personnel • Have policies and procedures for identification and management of an influenza outbreak, including occupational health aspects (eg, which staff should receive antiviral treatment or chemoprophylaxis, be referred for influenza testing and antiviral treatment; policies for sick leave and return to work) • Have mechanisms in place for rapid collection and handling of respiratory specimens from ill residents or patients and healthcare personnel for influenza testing, preferably by molecular assays. If influenza molecular assays are negative, test specimens for other respiratory pathogens, since noninfluenza respiratory viruses and bacteria infections have also been associated with respiratory disease outbreaks in healthcare and long-term care facilities; the nonpharmaceutical control measures apply to these as well • Implement active daily surveillance for any new respiratory illness (eg, fever, increased work of breathing, coughing, or sneezing) among residents or patients and staff. Respiratory symptoms, even without fever, should trigger suspicion for influenza, especially in elderly individuals. Nonrespiratory manifestations, such as altered mental status, may also be a sign of influenza virus infection in elderly patients • Collect respiratory specimens for influenza testing (preferably by molecular assay such as RT-PCR, if available) from all new symptomatic residents or patients to facilitate identification of the end of the outbreak and inform the extent (units or wards affected) and duration of outbreak control interventions. • Any ill staff who develop respiratory symptoms should don a facemask and promptly be excluded from the facility and, if indicated, be offered or referred for empiric antiviral treatment or have influenza testing performed. Institute a policy where ill staff do not return to work until afebrile >24 hours without antipyretic treatment and with improvement in respiratory symptoms or no earlier than 5 days after illness onset, because lack of fever does not necessarily mean lack of infectiousness • Post and display information about influenza illness signs and symptoms, facility policies related to influenza prevention and control, influenza vaccine recommendations, outbreak activity, and precautions for visitors and staff • Have procedures in place to actively screen all visitors for any illness signs and symptoms, and prohibit anyone with any illness from visiting • Offer influenza vaccination to unvaccinated staff members and residents or patients, and oseltamivir chemoprophylaxis to staff for 14 days after influenza vaccination. If influenza vaccine is not available, antiviral chemoprophylaxis can be offered to all unvaccinated staff for the duration of an institutional outbreak • Notify local public health authorities as soon as possible of a suspected or confirmed influenza outbreak |
When an institutional influenza outbreak is recognized, it is very likely that some exposed residents or patients are already incubating influenza virus infection coincident with the initiation of antiviral chemoprophylaxis. Additionally, antiviral chemoprophylaxis is not completely effective in preventing influenza, and some persons receiving antiviral chemoprophylaxis can develop influenza [393, 435]. Persons receiving antiviral chemoprophylaxis who develop any signs or symptoms of influenza should be switched to receive antiviral treatment dosing.
Antiviral chemoprophylaxis (once daily) rather than treatment dosing (twice daily) given to persons with asymptomatic influenza virus infection might theoretically increase the risk of selection for antiviral-resistant influenza viruses. However, the risk for developing NAI antiviral resistance is low except in severely immunocompromised persons, who can have prolonged and asymptomatic influenza virus replication [134]. Because some exposed persons can have asymptomatic or sub-clinical influenza virus infection, consideration can be given to using antivirals for chemoprophylaxis at the daily treatment dosing (twice daily with renal dose adjustment if indicated) to exposed residents or patients instead of antiviral chemoprophylaxis dosing (once daily) during outbreaks of influenza in long-term care facilities or healthcare facilities, including in immunosuppressed exposed patients [437, 438]. In this situation, antiviral treatment dosing should be continued for a full treatment course (twice daily) for 5 days before reducing to the recommended chemoprophylaxis dosing (once daily) until the outbreak is declared over.
To Control an Influenza Outbreak in a Long-term Care Facility or Hospital, Should Antiviral Chemoprophylaxis Be Administered to Exposed Residents/Patients?
Recommendation
-
53
Antiviral chemoprophylaxis should be administered as soon as possible to all exposed residents or patients who do not have suspected or laboratory-confirmed influenza regardless of influenza vaccination history, in addition to implementation of all other recommended influenza out-break control measures, when an influenza outbreak has been identified in a long-term care facility or hospital (A-III).
During an Influenza Outbreak at a Long-term Care Facility, Should Antiviral Chemoprophylaxis Be Administered to Residents Only on Affected Units or to All Residents in the Facility?
Recommendation
-
54
Antiviral chemoprophylaxis should be administered to residents on outbreak-affected units, in addition to implementing active daily surveillance for new influenza cases throughout the facility (A-II).
Evidence Summary
Residents of long-term care facilities and hospitalized patients are at high risk for complications of influenza, even if vaccinated, because influenza vaccine effectiveness may be low, particularly in elderly persons. Influenza vaccine should be administered to all healthcare personnel each season, as vaccine is more likely to be immunogenic in healthcare personnel compared with residents. Several RCTs of antiviral chemoprophylaxis have been conducted among long-term care residents. Two RCTs of inhaled zanamivir for postexposure chemoprophylaxis have reported efficacy in reducing laboratory-confirmed influenza in elderly long-term care residents with high influenza vaccine coverage in the United States [409] and in an unvaccinated population in Lithuania [439]. One RCT of oseltamivir chemoprophylaxis for 10 days vs placebo in frail elderly patients in long-term care facility units after a single laboratory-confirmed case of influenza over 4 seasons in the Netherlands did not find a significant benefit; however, this study was underpowered due to fewer influenza outbreaks than expected [440]. In a cluster randomized trial over 3 seasons in Australia comparing oseltamivir treatment of symptomatic persons and provision of oseltamivir chemoprophylaxis for elderly long-term care residents and staff, researchers found that chemoprophylaxis reduced the influenza attack rate among residents compared with treatment of symptomatic persons [407]. One multicountry RCT of oseltamivir chemoprophylaxis vs placebo for 6 weeks in vaccinated residents reported high efficacy in preventing influenza outbreaks in nursing homes [441].
Multiple observational studies have reported effectiveness of oseltamivir chemoprophylaxis in controlling influenza out-breaks in long-term care facilities [410, 442–444]. One retro-spective analysis of surveillance and administrative data on influenza outbreaks in long-term care facilities over 2 seasons in Alberta, Canada, reported that a 1-day delay in administering oseltamivir chemoprophylaxis among residents was associated with an increase of 2.2 days (95% CI, 1.37–3.06) in outbreak duration after the intervention [443].
However, a retrospective observational study of routinely collected influenza outbreak data in aged care facilities in 3 local health districts in Australia reported no difference in outbreak duration, attack rates, hospitalization, or case fatality between residents of facilities where antiviral chemoprophylaxis (oral oseltamivir) was routinely recommended compared with facilities where antiviral treatment, but not routine antiviral chemoprophylaxis, was recommended [444].
Data on the effectiveness of antiviral chemoprophylaxis for controlling influenza outbreaks in hospitals are limited. The use of oseltamivir or zanamivir chemoprophylaxis of exposed patients has been described in neonates, older children, and adults in conjunction with other interventions to control nosocomial influenza outbreaks [445–448]. Decisions about antiviral chemoprophylaxis should consider the anticipated severity of illness, risk of complications, and mortality associated with influenza in the population at risk, and on the ability to implement control measures, including isolation and spatial separation of susceptible individuals from each other. Decisions about the choice of antivirals and whether to utilize chemoprophylaxis vs treatment dosing should be carefully considered for control of influenza outbreaks in units with immunocompromised and immunosuppressed patients because such patients can have prolonged influenza viral replication with emergence and nosocomial transmission of antiviral-resistant influenza virus strains [352, 449].
There are very limited data to inform the use of antiviral chemoprophylaxis beyond affected units during influenza out-breaks in long-term care facilities. One observational study reported that outbreak duration was the shortest when oseltamivir chemoprophylaxis was administered to all residents of one nursing home vs only for exposed residents at another nursing home or not used at a third nursing home [410]. There are no published data to quantify the risk of influenza virus transmission among different wards of a long-term care facility. Some factors that can facilitate influenza virus transmission among different units and buildings include the amount of mixing by shared staff, sharing circulating air or patient care equipment, and the duration of resident interaction such as in common rooms for shared meals or other group activities. The risk of wider influenza virus transmission likely increases as the number of influenza cases increases and as the time extends between onset of the first cases, recognition of the outbreak, and implementation of interventions.
Decisions on whether to widen antiviral chemoprophylaxis should consider the potential for influenza virus transmission between different wards and buildings of the facility and balance the risk of complications associated with additional cases of influenza in residents against the cost and adverse consequences of antiviral chemoprophylaxis. Use of antiviral chemoprophylaxis limited to an individual affected ward is reasonable if the number of influenza cases is small when the outbreak is declared, and if the affected ward’s residents and staff had limited contact with those of other wards before the outbreak was declared. This approach is also reasonable if residents and staff can be effectively separated from other wards or buildings after the outbreak is declared. Active daily surveillance for new influenza cases, with influenza testing for suspected cases, should be enhanced throughout the entire facility as soon as an outbreak is declared on any one ward. Finding influenza virus transmission on a second ward should prompt consideration of facility-wide antiviral chemoprophylaxis, as considerable experience by subject matter experts in this scenario has demonstrated eventual emergence of further influenza virus transmission to multiple units within the facility when implementation of facility-wide antiviral chemoprophylaxis is not implemented.
Use of antiviral chemoprophylaxis might be considered along with other control measures for influenza outbreaks in other institutional settings among persons generally not at high risk for complications from influenza, such as in dormitories at boarding schools, universities, and summer camps. However, in populations with lower risk of influenza complications, the benefits of prevention with antivirals may be marginal. As such, considerable uncertainty remains about how, when, and for whom antiviral chemoprophylaxis should be used for these other institutional settings.
Which Healthcare Personnel Should Receive Antiviral Chemoprophylaxis During an Institutional Outbreak?
Recommendations
-
55
Clinicians can consider antiviral chemoprophylaxis for unvaccinated staff, including those for whom chemoprophylaxis may be indicated based upon underlying conditions of the staff or their household members (see recommendations 41–43) for the duration of the outbreak (C-III).
-
56
Clinicians can consider antiviral chemoprophylaxis for staff who receive inactivated influenza vaccine during an institutional influenza outbreak for 14 days postvaccination (C-III).
-
57
Clinicians can consider antiviral chemoprophylaxis for staff regardless of influenza vaccination status to reduce the risk of short staffing in facilities and wards where clinical staff are limited and to reduce staff reluctance to care for patients with suspected influenza (C-III).
Evidence Summary
There are no data available to address the effectiveness of antiviral chemoprophylaxis of staff to control institutional influenza outbreaks in residents or patients, or to guide whether, when, and which staff should be considered for antiviral chemoprophylaxis. Observational studies have described the use of antiviral chemoprophylaxis of staff in addition to exposed residents [450–452], and some randomized controlled trials for antiviral chemoprophylaxis of residents also offered chemoprophylaxis to staff [409, 430].
Factors to consider when deciding whether to offer antiviral chemoprophylaxis include: (i) staff can serve as sources of influenza virus transmission to residents; (ii) staff absenteeism for respiratory illness will impact workforce available for care of facility residents; and (iii) staff could be infected with influenza viruses from ill residents or patients. Antiviral chemoprophylaxis in vaccinated staff may be less beneficial to institutional outbreak control than use in unvaccinated staff if vaccine is not available. Many facilities cannot afford to have several ill staff absent from work, and increased staff demands at the time of outbreak declaration may make it challenging for referral to a primary care provider to prescribe antiviral chemoprophylaxis. Therefore, facility medical directors should plan for prescribing antivirals (including renal dosing adjustments if needed) by facility physicians vs referral to external providers.
All healthcare personnel should receive annual influenza vaccination [453]. During influenza outbreaks, influenza vaccine should be offered to unvaccinated staff throughout the facility, and antiviral chemoprophylaxis can be offered for 14 days postvaccination (until protective antibodies have developed). If influenza vaccine is not available, antiviral chemoprophylaxis can be offered to all unvaccinated staff. Antiviral chemoprophylaxis can also be offered to unvaccinated staff with vaccine contraindications and to immunocompromised staff (who are expected to have poor immune response to vaccination) for the duration of an institutional outbreak.
The importance of limiting staff absenteeism for outbreak control and maintaining quality of patient and resident care during the outbreak should be assessed and incorporated into decisions about antiviral chemoprophylaxis of staff. Especially during seasons in which influenza vaccine effectiveness is low, consideration can be given to administration of antiviral chemoprophylaxis to vaccinated staff for the duration of an outbreak.
Effective isolation and control of outbreaks can be challenging and may require different strategies. Facility medical directors should consider consultation from public health experts.
How Long Should Antiviral Chemoprophylaxis Be Given to Residents During an Influenza Outbreak in a Long-term Care Facility?
Recommendation
-
58
Clinicians should administer antiviral chemoprophylaxis for 14 days and continue for at least 7 days after the onset of symptoms in the last case identified during an institutional influenza outbreak (A-III).
Evidence Summary
One older randomized trial conducted during 1991–1995 reported that antiviral chemoprophylaxis with amantadine or rimantadine for 14 days (and for 7 days after the last confirmed influenza case) was sufficient to control influenza A outbreaks compared to 21 days (and for 7 days after the last confirmed influenza case) [454]. No randomized trials have been conducted to assess the duration of NAI chemoprophylaxis to control influenza outbreaks in long-term care facilities. One observational study described successful use of oseltamivir chemoprophylaxis to control 5 influenza outbreaks in long-term care residents after use of amantadine failed to contain the outbreaks [442]. Other studies have described the use of oseltamivir or zanamivir chemoprophylaxis for 7–14 days [407–410, 439, 440, 451, 454].
The incubation period for influenza is believed to be typically 1–3 days, up to 4 days, with a mean serial interval (time from illness onset of the index case to illness onset of a secondary case, such as in household transmission studies) of approximately 2–3 days in most persons [455]. Influenza A(H1N1) pdm09 viral RNA can be detected for approximately 4–7 days after onset of symptoms in most persons (although influenza virus is recoverable in viral culture for shorter periods), and immunosuppressed, hospitalized and critically ill patients can have prolonged influenza viral shedding [455]. Two recent household studies suggested that influenza A(H1N1)pdm09 virus transmission was substantially reduced >3 days after onset of symptoms [456], but another study reported that more than one-third of patients had A(H1N1)pdm09 viral RNA detected at 7 days after illness onset [457]. While data are limited on the optimal duration of antiviral chemoprophylaxis to control institutional influenza outbreaks, the CDC recommends that antiviral chemoprophylaxis should be administered initially for 14 days, and if surveillance indicates that new cases continue to occur, chemoprophylaxis should be continued until 7 days after the last case has been identified [458].
Research Gaps
Following global consultations with multiple stakeholders, the WHO posted a comprehensive influenza research agenda in 2009 that addressed research gaps including surveillance, the animal-human interface, novel influenza A virus infections, transmission, vaccines and other prevention strategies, diagnostics, disease pathogenesis, antivirals, and clinical management. During 2016–2017, some IDSA panelists worked with international experts on reviewing advances in the field and updating this research agenda. Specific issues of interest to IDSA are included in the WHO Research Agenda, Stream 4: optimizing the treatment of patients (available at http://www.who.int/influenza/resources/research/Stream_4_BD_final_GIP.pdf?ua=1).
New Developments After Guideline Finalization
Baloxavir marboxil is a cap-dependent endonuclease inhibitor that was approved by the FDA for treatment of acute uncomplicated influenza in patients aged ≥12 years who have been symptomatic for no more than 48 hours. As FDA approval occurred after finalization of these guidelines, the panel was unable to make recommendations on use of baloxavir. In a phase 3 randomized controlled trial of baloxavir, oseltamivir, and placebo in 1066 otherwise healthy patients aged 12–64 years with uncomplicated influenza for no more than 48 hours, a single dose of baloxavir significantly shortened the median time to alleviation of symptoms by 26.5 hours compared with placebo (P < .001) [459]. There was no difference in clinical benefit for a single dose of baloxavir compared with 5 days of twice-daily oseltamivir [459]. Baloxavir was well tolerated, with no difference in adverse events compared with oseltamivir or placebo. The median duration of infectious virus detection in upper respiratory tract specimens was significantly shorter for baloxavir compared with oseltamivir (24 vs 72 hours, respectively; P < .001) [459]. However, 10% of the baloxavir recipients with paired sequenced samples had emergence of viral escape mutants with reduced drug susceptibility, and most of these patients had infectious virus detected 5 days after treatment and longer duration of symptoms than in baloxavir recipients without these mutations [459].
The results of a phase 3, randomized controlled trial of balox-avir, oseltamivir, and placebo in 1163 patients aged ≥12 years, with at least one high-risk medical condition and uncomplicated influenza for no more than 48 hours were presented after finalization of these guidelines. In this study, a single dose of baloxavir reduced the median time to improvement of symptoms by 29.1 hours compared with placebo (P < .0001), but was not significantly different than 5 days of twice-daily oseltamivir [460]. In patients with influenza B, baloxavir significantly reduced the median time to improvement of symptoms by 26 hours compared with placebo (P < .0138) and 27 hours compared with oseltamivir (P < .0251) [460]. Baloxavir significantly reduced systemic antibiotic use and influenza-related complications compared with placebo [460].
Multiple influenza diagnostics and therapeutics are in advanced development, and new influenza tests, antiviral medications, and other therapeutics might be approved by the FDA after publication of these guidelines. Clinicians should consult the CDC webpages for the latest information on approved influenza tests (https://www.cdc.gov/flu/professionals/diagnosis/index.htm) and approved antivirals (https://www.cdc.gov/flu/professionals/antivirals/index.htm).
Acknowledgments.
The expert panel expresses its gratitude for thoughtful external reviews of an earlier version by Drs John Beigel, Arnold Monto, and Ruth Lynfield. The panel thanks Vita Washington and Rebecca Goldwater for their guidance and assistance in preparation of the manuscript; Peggy Cruse for her assistance with systematic literature searches; and Valery Lavergne for her guidance and support during the development of the guidelines.
Financial support. Support for these guidelines was provided by the Infectious Diseases Society of America.
Footnotes
It is important to realize that guidelines cannot always account for individual variationamong patients. They are not intended to supplant physician judgment with respect to particular patients or special clinical situations. IDSA considers adherence to these guidelines to be voluntary, with the ultimate determination regarding their application to be made by the physician in the light of a patient’s individual circumstances. While IDSA makes every effort to present accurate and reliable information, the information provided in these guidelines is “as is” without any warranty of accuracy, reliability, or otherwise, either express or implied. Neither IDSA nor its officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with these guidelines or reliance on the information presented. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Disclaimer. While IDSA makes every effort to present accurate and reliable information, the information provided in these guidelines is “as is” without any warranty of accuracy, reliability, or otherwise, either express or implied. Neither IDSA nor its officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with these guidelines or reliance on the information presented. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Potential conflicts of interest. The following list is a reflection of what has been reported to the IDSA. To provide thorough transparency, the IDSA requires full disclosure of all relationships, regardless of relevancy to the guideline topic. Evaluation of such relationships as potential conflicts of interest (COI) is determined by a review process that includes assessment by the Standards and Practice Guidelines Committee (SPGC) Chair, the SPGC liaison to the development panel and the Board of Directors (BOD) liaison to the SPGC, and if necessary, the COI Task Force of the BOD. This assessment of disclosed relationships for possible COI will be based on the relative weight of the financial relationship (ie, monetary amount) and the relevance of the relationship (ie, the degree to which an association might reasonably be interpreted by an independent observer as related to the topic or recommendation of consideration). The reader of these guidelines should be mindful of this when the list of disclosures is reviewed. H. H. B. reports grants from the New York State Department of Health and personal fees from Current Opinion in Pediatrics, Shire Human Genetic Therapies, the Harvard School of Public Health, and the American Academy of Pediatrics (AAP); H. H. B. is a member of the Advisory Committee on Immunization Practices at CDC; is an ex-officio member of the Committee on Infectious Diseases at AAP; and is an editor of the Red Book Online at AAP. J. A. E. reports personal fees from Sanofi Pasteur, Gilead, and the Bill & Melinda Gates Foundation and grants from Gilead, Chimerix, Novavax, the Bill & Melinda Gates Foundation, Alios/Janssen, and MedImmune, out-side the submitted work. T. M. F. reports personal fees from bioMerieux, Curetis AG, GlaxoSmithKline, Melinta, Meji Seika Pharma Co, Merck & Co, MotifBio, Nabriva, Paratek, and Shionogi, during the conduct of the study. S. G. reports grants, personal fees, and nonfinancial support from Sanofi and Seqirus; personal fees from Merck, Pfizer, Longevoron, Janssen, GSK, and the Gerontological Society of America; and grants from the National Institutes of Health (NIH), CDC, and Janssen. F. G. H. reports personal fees from the World Health Organization and the University of Alabama Antiviral Drug Discovery and Development Consortium; fees to the University of Virginia for serving on data safety monitoring boards for Celltrion, GSK, and Vaccitech; donations to a non-profit orphanage and school for consulting from PREP Biopharm and Sequiris; travel support and donations to a non-profit orphanage and school for consulting from Shionogi; and noncompensated consulting for various companies engaged in developing influenza therapeutics or vaccines (CoCrystal, Farmak, Genentech/Roche, GSK, Janssen, MedImmune, Medivector/ FujiFilm, Regeneron, resTORbio, SAB Biotherapeutics, Vir, and Visterra). J. M. H. reports personal fees from Pfizer; nonfinancial support from Global Blood Therapeutics; and grants from the NIH, Fogarty International Center, the Health Resources and Services Administration, the Centers for Medicare and Medicaid, and the Maryland Institute of Emergency Medical System Services, outside the submitted work. M. G. I. reports grants from Janssen and Emergent BioSolutions; personal fees from Celltrion, Genentech/ Roche, Medi Vector, Seqirus, VirBio, Alios, Biota, Crucell, Janssen, and NexBio, during the conduct of the study; and reimbursement for serving on a data safety monitoring board from GlaxoSmithKline. B. L. J. reports grants from Pfizer, Gilead, and the Canadian Institutes of Health Research (CIHR); and contracts for nosocomial infection surveillance from the Public Health Agency of Canada, outside the submitted work. A. M. reports grants and other from Crucell, Sanofi Pasteur, and GlaxoSmithKline; and grants from CIHR and the Ontario Workplace Safety Insurance Board, out-side the submitted work. L. E. R. served as a consultant to the Vaccines and Medications in Pregnancy Surveillance System; served as a speaker for the American College of Obstetricians and Gynecologists; served as a contributor for UpToDate; served as a consultant to Johns Hopkins University; reports grants from the Bill & Melinda Gates Foundation; and provided expert testimony for Ficks and Connolly, for Wiggins and Dana, LLP, and for McAloon & Friedman. A. T. P. reports grants from the National Institute of Allergy and Infectious Diseases (NIAID)/NIH, NIAID/Biofire, and the CDC; other from Antimicrobial Therapy Inc; and personal fees from WebMD and Johnson & Johnson, outside the submitted work. All other authors report no potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis 2018; 66:1511–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poehling KA, Edwards KM, Weinberg GA, et al. ; New Vaccine Surveillance Network. The underrecognized burden of influenza in young children. N Engl J Med 2006; 355:31–40. [DOI] [PubMed] [Google Scholar]
- 3.Siston AM, Rasmussen SA, Honein MA, et al. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA 2010; 303:1517–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou H, Thompson WW, Viboud CG, et al. Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis 2012; 54:1427–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson WW, Moore MR, Weintraub E, et al. Estimating influenza-associated deaths in the United States. Am J Public Health 2009; 99(Suppl 2):S225–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine 2007; 25:5086–96. [DOI] [PubMed] [Google Scholar]
- 7.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA 2004; 292:1333–40. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Estimates of deaths associated with seasonal influenza—United States, 1976–2007. MMWR Morb Mortal Wkly Rep 2010; 59:1057–62. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Disease Burden of Influenza. Available at: https://www.cdc.gov/flu/about/burden/index.html Accessed on November 8, 2018.
- 10.Iuliano AD, Roguski KM, Chang HH, et al. ; Global Seasonal Influenza-Associated Mortality Collaborator Network. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet 2018; 391:1285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonner AB, Monroe KW, Talley LI, Klasner AE, Kimberlin DW. Impact of the rapid diagnosis of influenza on physician decision-making and patient management in the pediatric emergency department: results of a randomized, prospective, controlled trial. Pediatrics 2003; 112:363–7. [DOI] [PubMed] [Google Scholar]
- 12.Falsey AR, Murata Y, Walsh EE. Impact of rapid diagnosis on management of adults hospitalized with influenza. Arch Intern Med 2007; 167:354–60. [DOI] [PubMed] [Google Scholar]
- 13.Hsu J, Santesso N, Mustafa R, et al. Antivirals for treatment of influenza: a systematic review and meta-analysis of observational studies. Ann Intern Med 2012; 156:512–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jefferson T, Jones MA, Doshi P, et al. Neuraminidase inhibitors for preventing and treating influenza in healthy adults and children. Cochrane Database Syst Rev 2014; CD008965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muthuri SG, Myles PR, Venkatesan S, Leonardi-Bee J, Nguyen-Van-Tam JS. Impact of neuraminidase inhibitor treatment on outcomes of public health importance during the 2009–2010 influenza A(H1N1) pandemic: a systematic review and meta-analysis in hospitalized patients. J Infect Dis 2013; 207:553–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muthuri SG, Venkatesan S, Myles PR, et al. ; PRIDE Consortium Investigators. Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza A H1N1pdm09 virus infection: a meta-analysis of individual participant data. Lancet Respir Med 2014; 2:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harper SA, Bradley JS, Englund JA, et al. ; Expert Panel of the Infectious Diseases Society of America. Seasonal influenza in adults and children-diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2009; 48:1003–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Prevention strategies for seasonal influenza in healthcare settings: guidelines and recommendations. Available at: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm. Accessed 30 September 2018.
- 19.Centers for Disease Control and Prevention. Avian influenza: information for health professionals and laboratorians. Available at: https://www.cdc.gov/flu/avi-anflu/healthprofessionals.htm. Accessed 30 September 2018.
- 20.Centers for Disease Control and Prevention. Interim guidance for clinicians on human infections with variant influenza viruses. Available at: https://www.cdc.gov/flu/swineflu/interim-guidance-variant-flu.htm. Accessed 30 September 2018.
- 21.Lindegren ML, Griffin MR, Williams JV, et al. Antiviral treatment among older adults hospitalized with influenza, 2006–2012. PLoS One 2015; 10:e0121952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Havers F, Thaker S, Clippard JR, et al. Use of influenza antiviral agents by ambulatory care clinicians during the 2012–2013 influenza season. Clin Infect Dis 2014; 59:774–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stockmann C, Byington CL, Pavia AT, et al. Limited and variable use of antivirals for children hospitalized with influenza. JAMA Pediatr 2017; 171:299–301. [DOI] [PubMed] [Google Scholar]
- 24.Nichol KL, Treanor JJ. Vaccines for seasonal and pandemic influenza. J Infect Dis 2006; 194(Suppl 2):S111–8. [DOI] [PubMed] [Google Scholar]
- 25.Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis 2012; 12:36–44. [DOI] [PubMed] [Google Scholar]
- 26.Boivin G, Goyette N, Hardy I, Aoki F, Wagner A, Trottier S. Rapid antiviral effect of inhaled zanamivir in the treatment of naturally occurring influenza in other-wise healthy adults. J Infect Dis 2000; 181:1471–4. [DOI] [PubMed] [Google Scholar]
- 27.Call SA, Vollenweider MA, Hornung CA, Simel DL, McKinney WP. Does this patient have influenza? JAMA 2005; 293:987–97. [DOI] [PubMed] [Google Scholar]
- 28.Monto AS, Gravenstein S, Elliott M, Colopy M, Schweinle J. Clinical signs and symptoms predicting influenza infection. Arch Intern Med 2000; 160:3243–7. [DOI] [PubMed] [Google Scholar]
- 29.SoČan M, Prosenc K, Nagode M. Differences in clinical predictors of influenza in adults and children with influenza-like illness. Cent Eur J Med 2010; 5:41–8. [Google Scholar]
- 30.Shah SC, Rumoro DP, Hallock MM, et al. Clinical predictors for laboratory-confirmed influenza infections: exploring case definitions for influenza-like illness. Infect Control Hosp Epidemiol 2015; 36:241–8. [DOI] [PubMed] [Google Scholar]
- 31.Yang JH, Huang PY, Shie SS, et al. Predictive symptoms and signs of laboratory-confirmed influenza: a prospective surveillance study of two metropolitan areas in Taiwan. Medicine (Baltimore) 2015; 94:e1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Babcock HM, Merz LR, Dubberke ER, Fraser VJ. Case-control study of clinical features of influenza in hospitalized patients. Infect Control Hosp Epidemiol 2008; 29:921–6. [DOI] [PubMed] [Google Scholar]
- 33.Miller MR, Peters TR, Suerken CK, Snively BM, Poehling KA. Predictors of influnza diagnosis among patients with laboratory-confirmed influenza. J Infect Dis 2015; 212:1604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glezen WP, Taber LH, Frank AL, Gruber WC, Piedra PA. Influenza virus infections in infants. Pediatr Infect Dis J 1997; 16:1065–8. [DOI] [PubMed] [Google Scholar]
- 35.Quach C, Piché-Walker L, Platt R, Moore D. Risk factors associated with severe influenza infections in childhood: implication for vaccine strategy. Pediatrics 2003; 112:e197–201. [DOI] [PubMed] [Google Scholar]
- 36.Rojo JC, Ruiz-Contreras J, Fernández MB, Marín MA, Folgueira L. Influenza-related hospitalizations in children younger than three years of age. Pediatr Infect Dis J 2006; 25:596–601. [DOI] [PubMed] [Google Scholar]
- 37.Wang YH, Huang YC, Chang LY, et al. Clinical characteristics of children with influenza A virus infection requiring hospitalization. J Microbiol Immunol Infect 2003; 36:111–6. [PubMed] [Google Scholar]
- 38.Wootton SH, Scheifele DW, Mak A, Petric M, Skowronski DM. Detection of human influenza virus in the stool of children. Pediatr Infect Dis J 2006; 25:1194–5. [DOI] [PubMed] [Google Scholar]
- 39.Meury S, Zeller S, Heininger U. Comparison of clinical characteristics of influenza and respiratory syncytial virus infection in hospitalised children and adolescents. Eur J Pediatr 2004; 163:359–63. [DOI] [PubMed] [Google Scholar]
- 40.Heinonen S, Peltola V, Silvennoinen H, Vahlberg T, Heikkinen T. Signs and symptoms predicting influenza in children: a matched case-control analysis of prospectively collected clinical data. Eur J Clin Microbiol Infect Dis 2012; 31:1569–74. [DOI] [PubMed] [Google Scholar]
- 41.Jain S, Self WH, Wunderink RG, et al. ; CDC EPIC Study Team. Community- acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med 2015; 373:415–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guarner J, Paddock CD, Shieh WJ, et al. Histopathologic and immunohistochemical features of fatal influenza virus infection in children during the 2003–2004 season. Clin Infect Dis 2006; 43:132–40. [DOI] [PubMed] [Google Scholar]
- 43.Brundage JF. Interactions between influenza and bacterial respiratory pathogens: implications for pandemic preparedness. Lancet Infect Dis 2006; 6:303–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hageman JC, Uyeki TM, Francis JS, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003–04 influenza season. Emerg Infect Dis 2006; 12:894–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peltola VT, McCullers JA. Respiratory viruses predisposing to bacterial infections: role of neuraminidase. Pediatr Infect Dis J 2004; 23:S87–97. [DOI] [PubMed] [Google Scholar]
- 46.Bhat N, Wright JG, Broder KR, et al. Influenza-associated deaths among children in the United States, 2003–2004. N Engl J Med 2005; 353:2559–67. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Severe methicillin-resistant Staphylococcus aureus community-acquired pneumonia associated with influenza—Louisiana and Georgia, December 2006-January 2007. MMWR Morb Mortal Wkly Rep 2007; 56:325–9. [PubMed] [Google Scholar]
- 48.Finelli L, Fiore A, Dhara R, et al. Influenza-associated pediatric mortality in the United States: increase of Staphylococcus aureus coinfection. Pediatrics 2008; 122:805–11. [DOI] [PubMed] [Google Scholar]
- 49.Mamas MA, Fraser D, Neyses L. Cardiovascular manifestations associated with influenza virus infection. Int J Cardiol 2008; 130:304–9. [DOI] [PubMed] [Google Scholar]
- 50.Abe M, Higuchi T, Okada K, Kaizu K, Matsumoto K. Clinical study of influenza-associated rhabdomyolysis with acute renal failure. Clin Nephrol 2006; 66:166–70. [DOI] [PubMed] [Google Scholar]
- 51.Annerstedt M, Herlitz H, Molne J, Oldfors A, Westberg G. Rhabdomyolysis and acute renal failure associated with influenza virus type A. Scand J Urol Nephrol 1999; 33:260–4. [DOI] [PubMed] [Google Scholar]
- 52.Naderi ASA, Palmer BF. Rhabdomyolysis and acute renal failure associated with influenza virus type B infection. Am J Med Sci 2006; 332:88–9. [DOI] [PubMed] [Google Scholar]
- 53.Maricich SM, Neul JL, Lotze TE, et al. Neurologic complications associated with influenza A in children during the 2003–2004 influenza season in Houston, Texas. Pediatrics 2004; 114:e626–33. [DOI] [PubMed] [Google Scholar]
- 54.Morishima T, Togashi T, Yokota S, et al. ; Collaborative Study Group on Influenza-Associated Encephalopathy in Japan. Encephalitis and encephalopathy associated with an influenza epidemic in Japan. Clin Infect Dis 2002; 35:512–7. [DOI] [PubMed] [Google Scholar]
- 55.Nagao T, Morishima T, Kimura H, et al. Prognostic factors in influenza-associated encephalopathy. Pediatr Infect Dis J 2008; 27:384–9. [DOI] [PubMed] [Google Scholar]
- 56.Newland JG, Laurich VM, Rosenquist AW, et al. Neurologic complications in children hospitalized with influenza: characteristics, incidence, and risk factors. J Pediatr 2007; 150:306–10. [DOI] [PubMed] [Google Scholar]
- 57.Steininger C, Popow-Kraupp T, Laferl H, et al. Acute encephalopathy associated with influenza A virus infection. Clin Infect Dis 2003; 36:567–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chang LY, Lee PI, Lin YJ, Chiu HH, Huang LM, Lee CY. Influenza B virus infection associated with shock in a two-month-old infant. J Formos Med Assoc 1996; 95:703–5. [PubMed] [Google Scholar]
- 59.Conway EE Jr, Haber RS, Gumprecht J, Singer LP. Toxic shock syndrome following influenza A in a child. Crit Care Med 1991; 19:123–5. [DOI] [PubMed] [Google Scholar]
- 60.MacDonald KL, Osterholm MT, Hedberg CW, et al. Toxic shock syndrome. A newly recognized complication of influenza and influenza-like illness. JAMA 1987; 257:1053–8. [DOI] [PubMed] [Google Scholar]
- 61.Sharkey R, Mulloy E, O’Neill G, Walker F, O’Neill S. Toxic shock syndrome following influenza A infection. Intensive Care Med 1999; 25:335–6. [DOI] [PubMed] [Google Scholar]
- 62.Tolan RW Jr. Toxic shock syndrome complicating influenza A in a child: case report and review. Clin Infect Dis 1993; 17:43–5. [DOI] [PubMed] [Google Scholar]
- 63.Sellers SA, Hagan RS, Hayden FG, Fischer WA 2nd. The hidden burden of influenza: a review of the extra-pulmonary complications of influenza infection. Influenza Other Respir Viruses 2017; 11:372–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Warren-Gash C, Bhaskaran K, Hayward A, et al. Circulating influenza virus, climatic factors, and acute myocardial infarction: a time series study in England and Wales and Hong Kong. J Infect Dis 2011; 203:1710–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR. Acute myocardial infarction and influenza: a meta-analysis of case-control studies. Heart 2015; 101:1738–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Varkey JB, Varkey B. Viral infections in patients with chronic obstructive pulmonary disease. Curr Opin Pulm Med 2008; 14:89–94. [DOI] [PubMed] [Google Scholar]
- 67.Dawood FS, Kamimoto L, D’Mello TA, et al. Children with asthma hospitalized with seasonal or pandemic influenza, 2003–2009. Pediatrics 2011; 128:e27–32. [DOI] [PubMed] [Google Scholar]
- 68.Mamas MA, Nair S, Fraser D. Cardiac tamponade and heart failure as a presentation of influenza. Exp Clin Cardiol 2007; 12:214–6. [PMC free article] [PubMed] [Google Scholar]
- 69.Miller EK, Griffin MR, Edwards KM, et al. ; New Vaccine Surveillance Network. Influenza burden for children with asthma. Pediatrics 2008; 121:1–8. [DOI] [PubMed] [Google Scholar]
- 70.Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 2018; 378:345–53. [DOI] [PubMed] [Google Scholar]
- 71.Babcock HM, Merz LR, Fraser VJ. Is influenza an influenza-like illness? Clinical presentation of influenza in hospitalized patients. Infect Control Hosp Epidemiol 2006; 27:266–70. [DOI] [PubMed] [Google Scholar]
- 72.Govaert TM, Dinant GJ, Aretz K, Knottnerus JA. The predictive value of influenza symptomatology in elderly people. Fam Pract 1998; 15:16–22. [DOI] [PubMed] [Google Scholar]
- 73.Monmany J, Rabella N, Margall N, Domingo P, Gich I, Vázquez G. Unmasking influenza virus infection in patients attended to in the emergency department. Infection 2004; 32:89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nicholson KG, Kent J, Hammersley V, Cancio E. Acute viral infections of upper respiratory tract in elderly people living in the community: comparative, prospective, population based study of disease burden. BMJ 1997; 315:1060–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Walsh EE, Cox C, Falsey AR. Clinical features of influenza A virus infection in older hospitalized persons. J Am Geriatr Soc 2002; 50:1498–503. [DOI] [PubMed] [Google Scholar]
- 76.Falsey AR, Baran A, Walsh EE. Should clinical case definitions of influenza in hospitalized older adults include fever? Influenza Other Respir Viruses 2015; 9(Suppl 1):23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lam PP, Coleman BL, Green K, et al. Predictors of influenza among older adults in the emergency department. BMC Infect Dis 2016; 16:615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Claus JA, Hodowanec AC, Singh K. Poor positive predictive value of influenza-like illness criteria in adult transplant patients: a case for multiplex respiratory virus PCR testing. Clin Transplant 2015; 29:938–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Apewokin S, Vyas K, Lester LK, et al. Influenza A outbreak in an ambulatory stem cell transplant center. Open Forum Infect Dis 2014; 1:ofu050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Horcajada JP, Pumarola T, Martínez JA, et al. A nosocomial outbreak of influenza during a period without influenza epidemic activity. Eur Respir J 2003; 21:303–7. [DOI] [PubMed] [Google Scholar]
- 81.Leekha S, Zitterkopf NL, Espy MJ, Smith TF, Thompson RL, Sampathkumar P. Duration of influenza A virus shedding in hospitalized patients and implications for infection control. Infect Control Hosp Epidemiol 2007; 28:1071–6. [DOI] [PubMed] [Google Scholar]
- 82.Sagrera X, Ginovart G, Raspall F, et al. Outbreaks of influenza A virus infection in neonatal intensive care units. Pediatr Infect Dis J 2002; 21:196–200. [DOI] [PubMed] [Google Scholar]
- 83.Salgado CD, Farr BM, Hall KK, Hayden FG. Influenza in the acute hospital setting. Lancet Infect Dis 2002; 2:145–55. [DOI] [PubMed] [Google Scholar]
- 84.Sartor C, Zandotti C, Romain F, et al. Disruption of services in an internal medicine unit due to a nosocomial influenza outbreak. Infect Control Hosp Epidemiol 2002; 23:615–9. [DOI] [PubMed] [Google Scholar]
- 85.Camps M, Vilella A, Marcos MA, et al. Incidence of respiratory viruses among travelers with a febrile syndrome returning from tropical and subtropical areas. J Med Virol 2008; 80:711–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Luna LK, Panning M, Grywna K, Pfefferle S, Drosten C. Spectrum of viruses and atypical bacteria in intercontinental air travelers with symptoms of acute respiratory infection. J Infect Dis 2007; 195:675–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Miller JM, Tam TW, Maloney S, et al. Cruise ships: high-risk passengers and the global spread of new influenza viruses. Clin Infect Dis 2000; 31:433–8. [DOI] [PubMed] [Google Scholar]
- 88.Mutsch M, Tavernini M, Marx A, et al. Influenza virus infection in travelers to tropical and subtropical countries. Clin Infect Dis 2005; 40:1282–7. [DOI] [PubMed] [Google Scholar]
- 89.Hirve S, Newman LP, Paget J, et al. Influenza seasonality in the tropics and sub-tropics—when to vaccinate? PLoS One 2016; 11:e0153003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Azziz Baumgartner E, Dao CN, Nasreen S, et al. Seasonality, timing, and climate drivers of influenza activity worldwide. J Infect Dis 2012; 206:838–46. [DOI] [PubMed] [Google Scholar]
- 91.Uyeki TM, Zane SB, Bodnar UR, et al. ; Alaska/Yukon Territory Respiratory Outbreak Investigation Team. Large summertime influenza A outbreak among tourists in Alaska and the Yukon Territory. Clin Infect Dis 2003; 36:1095–102. [DOI] [PubMed] [Google Scholar]
- 92.Gautret P, Steffen R. Communicable diseases as health risks at mass gatherings other than Hajj: what is the evidence? Int J Infect Dis 2016; 47:46–52. [DOI] [PubMed] [Google Scholar]
- 93.Alqahtani AS, Alfelali M, Arbon P, Booy R, Rashid H. Burden of vaccine preventable diseases at large events. Vaccine 2015; 33:6552–63. [DOI] [PubMed] [Google Scholar]
- 94.Al-Tawfiq JA, Memish ZA. Mass gatherings and infectious diseases: prevention, detection, and control. Infect Dis Clin North Am 2012; 26:725–37. [DOI] [PubMed] [Google Scholar]
- 95.Morrison C, Maurtua-Neumann P, Myint MT, Drury SS, Begue RE. Pandemic (H1N1) 2009 outbreak at camp for children with hematologic and oncologic conditions. Emerg Infect Dis 2011; 17:87–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Centers for Disease Control and Prevention. Oseltamivir-resistant 2009 pandemic influenza A (H1N1) virus infection in two summer campers receiving prophylaxis—North Carolina, 2009. MMWR Morb Mortal Wkly Rep 2009; 58:969–72. [PubMed] [Google Scholar]
- 97.Millman AJ, Kornylo Duong K, Lafond K, Green NM, Lippold SA, Jhung MA. Influenza outbreaks among passengers and crew on two cruise ships: a recent account of preparedness and response to an ever-present challenge. J Travel Med 2015; 22:306–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fernandes EG, de Souza PB, de Oliveira ME, et al. Influenza B outbreak on a cruise ship off the Sao Paulo Coast, Brazil. J Travel Med 2014; 21:298–303. [DOI] [PubMed] [Google Scholar]
- 99.Ward KA, Armstrong P, McAnulty JM, Iwasenko JM, Dwyer DE. Outbreaks of pandemic (H1N1) 2009 and seasonal influenza A (H3N2) on cruise ship. Emerg Infect Dis 2010; 16:1731–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Brotherton JM, Delpech VC, Gilbert GL, Hatzi S, Paraskevopoulos PD, McAnulty JM; Cruise Ship Outbreak Investigation Team. A large outbreak of influenza A and B on a cruise ship causing widespread morbidity. Epidemiol Infect 2003; 130:263–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Centers for Disease Control and Prevention. Influenza B virus outbreak on a cruise ship—Northern Europe, 2000. MMWR Morb Mortal Wkly Rep 2001; 50:137–40. [PubMed] [Google Scholar]
- 102.Centers for Disease Control and Prevention. Outbreak of 2009 pandemic influenza A (H1N1) on a Peruvian Navy ship—June-July 2009. MMWR Morb Mortal Wkly Rep 2010; 59:162–5. [PubMed] [Google Scholar]
- 103.Zhou L, Ren R, Ou J, et al. Risk factors for influenza A(H7N9) disease in China, a matched case control study, October 2014 to April 2015. Open Forum Infect Dis 2016; 3:ofw182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhou L, Liao Q, Dong L, et al. Risk factors for human illness with avian influenza A (H5N1) virus infection in China. J Infect Dis 2009; 199:1726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.World Health Organization. Avian influenza in humans. Available at: http://www.who.int/influenza/human_animal_interface/avian_influenza/en/. Accessed September 30, 2018
- 106.Jhung MA, Epperson S, Biggerstaff M, et al. Outbreak of variant influenza A(H3N2) virus in the United States. Clin Infect Dis 2013; 57:1703–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Greenbaum A, Quinn C, Bailer J, et al. Investigation of an outbreak of variant influenza A(H3N2) virus infection associated with an agricultural fair—Ohio, August 2012. J Infect Dis 2015; 212:1592–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Uyeki TM. Influenza diagnosis and treatment in children: a review of studies on clinically useful tests and antiviral treatment for influenza. Pediatr Infect Dis J 2003; 22:164–77. [DOI] [PubMed] [Google Scholar]
- 109.Grijalva CG, Poehling KA, Edwards KM, et al. Accuracy and interpretation of rapid influenza tests in children. Pediatrics 2007; 119:e6–11. [DOI] [PubMed] [Google Scholar]
- 110.Chartrand C, Leeflang MM, Minion J, Brewer T, Pai M. Accuracy of rapid influenza diagnostic tests: a meta-analysis. Ann Intern Med 2012; 156:500–11. [DOI] [PubMed] [Google Scholar]
- 111.Merckx J, Wali R, Schiller I, et al. Diagnostic accuracy of novel and traditional rapid tests for influenza infection compared with reverse transcriptase polymerase chain reaction: a systematic review and meta-analysis. Ann Intern Med 2017; 167:394–409. [DOI] [PubMed] [Google Scholar]
- 112.Centers for Disease Control and Prevention. Evaluation of rapid influenza diagnostic tests for detection of novel influenza A (H1N1) virus—United States, 2009. MMWR Morb Mortal Wkly Rep 2009; 58:826–9. [PubMed] [Google Scholar]
- 113.Busson L, Hallin M, Thomas I, De Foor M, Vandenberg O. Evaluation of 3 rapid influenza diagnostic tests during the 2012–2013 epidemic: influences of subtype and viral load. Diagn Microbiol Infect Dis 2014; 80:287–91. [DOI] [PubMed] [Google Scholar]
- 114.Chan KH, Chan KM, Ho YL, et al. Quantitative analysis of four rapid antigen assays for detection of pandemic H1N1 2009 compared with seasonal H1N1 and H3N2 influenza A viruses on nasopharyngeal aspirates from patients with influenza. J Virol Methods 2012; 186:184–8. [DOI] [PubMed] [Google Scholar]
- 115.Chu H, Lofgren ET, Halloran ME, Kuan PF, Hudgens M, Cole SR. Performance of rapid influenza H1N1 diagnostic tests: a meta-analysis. Influenza Other Respir Viruses 2012; 6:80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Centers for Disease Control and Prevention. Evaluation of 11 commercially available rapid influenza diagnostic tests—United States, 2011–2012. MMWR Morb Mortal Wkly Rep 2012; 61:873–6. [PubMed] [Google Scholar]
- 117.Hazelton B, Gray T, Ho J, Ratnamohan VM, Dwyer DE, Kok J. Detection of influenza A and B with the Alere ™ i influenza A & B: a novel isothermal nucleic acid amplification assay. Influenza Other Respir Viruses 2015; 9:151–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Beckmann C, Hirsch HH. Diagnostic performance of near-patient testing for influenza. J Clin Virol 2015; 67:43–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bell JJ, Selvarangan R. Evaluation of the Alere i influenza A&B nucleic acid amplification test by use of respiratory specimens collected in viral transport medium. J Clin Microbiol 2014; 52:3992–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lee CS, Lee JH, Kim CH. Time-dependent sensitivity of a rapid antigen test in patients with 2009 H1N1 influenza. J Clin Microbiol 2011; 49:1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Blyth CC, Iredell JR, Dwyer DE. Rapid-test sensitivity for novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med 2009; 361:2493. [DOI] [PubMed] [Google Scholar]
- 122.Rice TW, Rubinson L, Uyeki TM, et al. Critical illness from 2009 pandemic influenza A virus and bacterial coinfection in the United States. Crit Care Med 2012; 40:1487–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ali T, Scott N, Kallas W, et al. Detection of influenza antigen with rapid antibody-based tests after intranasal influenza vaccination (FluMist). Clin Infect Dis 2004; 38:760–2. [DOI] [PubMed] [Google Scholar]
- 124.Block SL, Yogev R, Hayden FG, Ambrose CS, Zeng W, Walker RE. Shedding and immunogenicity of live attenuated influenza vaccine virus in subjects 5–49 years of age. Vaccine 2008; 26:4940–6. [DOI] [PubMed] [Google Scholar]
- 125.Vesikari T, Karvonen A, Korhonen T, et al. ; CAIV-T Transmission Study Group. A randomized, double-blind study of the safety, transmissibility and phenotypic and genotypic stability of cold-adapted influenza virus vaccine. Pediatr Infect Dis J 2006; 25:590–5. [DOI] [PubMed] [Google Scholar]
- 126.Zambon M, Hays J, Webster A, Newman R, Keene O. Diagnosis of influenza in the community: relationship of clinical diagnosis to confirmed virological, serologic, or molecular detection of influenza. Arch Intern Med 2001; 161:2116–22. [DOI] [PubMed] [Google Scholar]
- 127.Huijskens EG, Koopmans M, Palmen FM, van Erkel AJ, Mulder PG, Rossen JW. The value of signs and symptoms in differentiating between bacterial, viral and mixed aetiology in patients with community-acquired pneumonia. J Med Microbiol 2014; 63:441–52. [DOI] [PubMed] [Google Scholar]
- 128.Ranjan P, Kumari A, Das R, Gupta L, Singh SK, Yadav M. Evaluation of clinical features scoring system as screening tool for influenza A (H1N1) in epidemic situations. J Postgrad Med 2012; 58:265–9. [DOI] [PubMed] [Google Scholar]
- 129.Keijzers GB, Vossen CN, Zhang P, et al. Predicting influenza A and 2009 H1N1 influenza in patients admitted to hospital with acute respiratory illness. Emerg Med J 2011; 28:500–6. [DOI] [PubMed] [Google Scholar]
- 130.Hirve S, Chadha M, Lele P, et al. Performance of case definitions used for influenza surveillance among hospitalized patients in a rural area of India. Bull World Health Organ 2012; 90:804–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lee VJ, Yap J, Cook AR, et al. A clinical diagnostic model for predicting influenza among young adult military personnel with febrile respiratory illness in Singapore. PLoS One 2011; 6:e17468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Padin DS, Faix D, Brodine S, et al. Retrospective analysis of demographic and clinical factors associated with etiology of febrile respiratory illness among US military basic trainees. BMC Infect Dis 2014; 14:576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mahony AA, Cheng AC, Olsen KL, et al. Diagnosing swine flu: the inaccuracy of case definitions during the 2009 pandemic, an attempt at refinement, and the implications for future planning. Influenza Other Respir Viruses 2013; 7:403–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Memoli MJ, Athota R, Reed S, et al. The natural history of influenza infection in the severely immunocompromised vs nonimmunocompromised hosts. Clin Infect Dis 2014; 58:214–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nicholson KG, Abrams KR, Batham S, et al. Randomised controlled trial and health economic evaluation of the impact of diagnostic testing for influenza, respiratory syncytial virus and Streptococcus pneumoniae infection on the management of acute admissions in the elderly and high-risk 18- to 64-year-olds. Health Technol Assess 2014; 18:1–274, vii-viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Blaschke AJ, Shapiro DJ, Pavia AT, et al. A national study of the impact of rapid influenza testing on clinical care in the emergency department. J Pediatric Infect Dis Soc 2014; 3:112–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Suryaprasad A, Redd JT, Ricks PM, et al. Effect of rapid influenza diagnostic testing on antiviral treatment decisions for patients with influenza-like illness: southwestern U.S., May-December 2009. Public Health Rep 2014; 129:322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Busson L, Mahadeb B, De Foor M, Vandenberg O, Hallin M. Contribution of a rapid influenza diagnostic test to manage hospitalized patients with suspected influenza. Diagn Microbiol Infect Dis 2017; 87:238–42. [DOI] [PubMed] [Google Scholar]
- 139.Brendish NJ, Malachira AK, Armstrong L, et al. Routine molecular point-of-care testing for respiratory viruses in adults presenting to hospital with acute respiratory illness (ResPOC): a pragmatic, open-label, randomised controlled trial. Lancet Respir Med 2017; 5:401–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chu HY, Englund JA, Huang D, et al. Impact of rapid influenza PCR testing on hospitalization and antiviral use: a retrospective cohort study. J Med Virol 2015; 87:2021–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rogers BB, Shankar P, Jerris RC, et al. Impact of a rapid respiratory panel test on patient outcomes. Arch Pathol Lab Med 2015; 139:636–41. [DOI] [PubMed] [Google Scholar]
- 142.Nelson RE, Stockmann C, Hersh AL, et al. Economic analysis of rapid and sensitive polymerase chain reaction testing in the emergency department for influenza infections in children. Pediatr Infect Dis J 2015; 34:577–82. [DOI] [PubMed] [Google Scholar]
- 143.Tillekeratne LG, Bodinayake CK, Nagahawatte A, et al. Use of rapid influenza testing to reduce antibiotic prescriptions among outpatients with influenza-like illness in southern Sri Lanka. Am J Trop Med Hyg 2015; 93:1031–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Soto M, Sampietro-Colom L, Vilella A, et al. Economic impact of a new rapid PCR assay for detecting influenza virus in an emergency department and hospitalized patients. PLoS One 2016; 11:e0146620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Green DA, Hitoaliaj L, Kotansky B, Campbell SM, Peaper DR. Clinical utility of on-demand multiplex respiratory pathogen testing among adult outpatients. J Clin Microbiol 2016; 54:2950–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ip DKM, Lau LLH, Chan KH, et al. The dynamic relationship between clinical symptomatology and viral shedding in naturally acquired seasonal and pandemic influenza virus infections. Clin Infect Dis 2016; 62:431–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lau LL, Cowling BJ, Fang VJ, et al. Viral shedding and clinical illness in naturally acquired influenza virus infections. J Infect Dis 2010; 201:1509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Weinstock DM, Gubareva LV, Zuccotti G. Prolonged shedding of multidrug-resistant influenza A virus in an immunocompromised patient. N Engl J Med 2003; 348:867–8. [DOI] [PubMed] [Google Scholar]
- 149.Ngaosuwankul N, Noisumdaeng P, Komolsiri P, et al. Influenza A viral loads in respiratory samples collected from patients infected with pandemic H1N1, seasonal H1N1 and H3N2 viruses. Virol J 2010; 7:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sung RY, Chan PK, Choi KC, et al. Comparative study of nasopharyngeal aspirate and nasal swab specimens for diagnosis of acute viral respiratory infection. J Clin Microbiol 2008; 46:3073–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Grijalva CG, Griffin MR, Edwards KM, et al. Concordance between RT-PCR- based detection of respiratory viruses from nasal swabs collected for viral testing and nasopharyngeal swabs collected for bacterial testing. J Clin Virol 2014; 60:309–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Robinson JL, Lee BE, Kothapalli S, Craig WR, Fox JD. Use of throat swab or saliva specimens for detection of respiratory viruses in children. Clin Infect Dis 2008; 46:e61–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Branche AR, Walsh EE, Formica MA, Falsey AR. Detection of respiratory viruses in sputum from adults by use of automated multiplex PCR. J Clin Microbiol 2014; 52:3590–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Falsey AR, Formica MA, Walsh EE. Yield of sputum for viral detection by reverse transcriptase PCR in adults hospitalized with respiratory illness. J Clin Microbiol 2012; 50:21–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Falsey AR, Formica MA, Walsh EE. Simple method for combining sputum and nasal samples for virus detection by reverse transcriptase PCR. J Clin Microbiol 2012; 50:2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hansen KB, Westin J, Andersson LM, Lindh M, Widell A, Nilsson AC. Flocked nasal swab versus nasopharyngeal aspirate in adult emergency room patients: similar multiplex PCR respiratory pathogen results and patient discomfort. Infect Dis (Lond) 2016; 48:246–50. [DOI] [PubMed] [Google Scholar]
- 157.de la Tabla VO, Masia M, Antequera P, et al. Comparison of combined nose- throat swabs with nasopharyngeal aspirates for detection of pandemic influenza A/H1N1 2009 virus by real-time reverse transcriptase PCR. J Clin Microbiol 2010; 48:3492–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Lambert SB, Whiley DM, O’Neill NT, et al. Comparing nose-throat swabs and nasopharyngeal aspirates collected from children with symptoms for respiratory virus identification using real-time polymerase chain reaction. Pediatrics 2008; 122:e615–20. [DOI] [PubMed] [Google Scholar]
- 159.Hammitt LL, Kazungu S, Welch S, et al. Added value of an oropharyngeal swab in detection of viruses in children hospitalized with lower respiratory tract infection. J Clin Microbiol 2011; 49:2318–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Dawood FS, Jara J, Estripeaut D, et al. What is the added benefit of oropharyngeal swabs compared to nasal swabs alone for respiratory virus detection in hospitalized children aged <10 years? J Infect Dis 2015; 212:1600–3. [DOI] [PubMed] [Google Scholar]
- 161.Lee N, Chan PK, Wong CK, et al. Viral clearance and inflammatory response patterns in adults hospitalized for pandemic 2009 influenza A(H1N1) virus pneumonia. Antivir Ther 2011; 16:237–47. [DOI] [PubMed] [Google Scholar]
- 162.López Roa P, Rodríguez-Sánchez B, Catalán P, et al. Diagnosis of influenza in intensive care units: lower respiratory tract samples are better than nose-throat swabs. Am J Respir Crit Care Med 2012; 186:929–30. [DOI] [PubMed] [Google Scholar]
- 163.Reddy KP, Bajwa EK, Parker RA, Onderdonk AB, Walensky RP. Relationship between upper respiratory tract influenza test result and clinical outcomes among critically ill influenza patients. Open Forum Infect Dis 2016; 3:ofw023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Tse H, To KK, Wen X, et al. Clinical and virological factors associated with viremia in pandemic influenza A/H1N1/2009 virus infection. PLoS One 2011; 6:e22534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wootton SH, Aguilera EA, Wanger A, et al. Detection of NH1N1 influenza virus in nonrespiratory sites among children. Pediatr Infect Dis J 2014; 33:95–6. [DOI] [PubMed] [Google Scholar]
- 166.Choi SM, Xie H, Campbell AP, et al. Influenza viral RNA detection in blood as a marker to predict disease severity in hematopoietic cell transplant recipients. J Infect Dis 2012; 206:1872–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Shieh WJ, Blau DM, Denison AM, et al. 2009 pandemic influenza A (H1N1): pathology and pathogenesis of 100 fatal cases in the United States. Am J Pathol 2010; 177:166–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mizuguchi M Influenza encephalopathy and related neuropsychiatric syndromes. Influenza Other Respir Viruses 2013; 7(Suppl 3):67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lyon JB, Remigio C, Milligan T, Deline C. Acute necrotizing encephalopathy in a child with H1N1 influenza infection. Pediatr Radiol 2010; 40:200–5. [DOI] [PubMed] [Google Scholar]
- 170.Bautista E, Chotpitayasunondh T, et al. ; Writing Committee of the WHO Consultation on Clinical Aspects of Pandemic (H1N1) 2009 Influenza. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med 2010; 362:1708–19. [DOI] [PubMed] [Google Scholar]
- 171.Bagshaw SM, Sood MM, Long J, Fowler RA, Adhikari NK; Canadian Critical Care Trials Group H1N1 Collaborative. Acute kidney injury among critically ill patients with pandemic H1N1 influenza A in Canada: cohort study. BMC Nephrol 2013; 14:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.To KK, Chan KH, Li IW, et al. Viral load in patients infected with pandemic H1N1 2009 influenza A virus. J Med Virol 2010; 82:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Dilantika C, Sedyaningsih ER, Kasper MR, et al. Influenza virus infection among pediatric patients reporting diarrhea and influenza-like illness. BMC Infect Dis 2010; 10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chan MC, Lee N, Chan PK, Leung TF, Sung JJ. Fecal detection of influenza A virus in patients with concurrent respiratory and gastrointestinal symptoms. J Clin Virol 2009; 45:208–11. [DOI] [PubMed] [Google Scholar]
- 175.Pinsky BA, Mix S, Rowe J, Ikemoto S, Baron EJ. Long-term shedding of influenza A virus in stool of immunocompromised child. Emerg Infect Dis 2010; 16:1165–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bell J, Bonner A, Cohen DM, et al. Multicenter clinical evaluation of the novel Alere™ i Influenza A&B isothermal nucleic acid amplification test. J Clin Virol 2014; 61:81–6. [DOI] [PubMed] [Google Scholar]
- 177.Binnicker MJ, Espy MJ, Irish CL, Vetter EA. Direct detection of influenza A and B viruses in less than 20 minutes using a commercially available rapid PCR assay. J Clin Microbiol 2015; 53:2353–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chapin KC, Flores-Cortez EJ. Performance of the molecular Alere i influenza A&B test compared to that of the xpert flu A/B assay. J Clin Microbiol 2015; 53:706–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Chen L, Tian Y, Chen S, Liesenfeld O. Performance of the Cobas(®) influenza A/B assay for rapid PCR-based detection of influenza compared to prodesse ProFlu+ and viral culture. Eur J Microbiol Immunol (Bp) 2015; 5:236–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Chiarella FC, Culebras E, Fuentes-Ferrer ME, Picazo JJ. Evaluation of the Alere i Influenza A&B assay for rapid identification of influenza A and influenza B viruses. J Med Microbiol 2016; 65:456–61. [DOI] [PubMed] [Google Scholar]
- 181.Jokela P, Vuorinen T, Waris M, Manninen R. Performance of the Alere i influenza A&B assay and mariPOC test for the rapid detection of influenza A and B viruses. J Clin Virol 2015; 70:72–6. [DOI] [PubMed] [Google Scholar]
- 182.Nie S, Roth RB, Stiles J, et al. Evaluation of Alere i influenza A&B for rapid detection of influenza viruses A and B. J Clin Microbiol 2014; 52:3339–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Nguyen Van JC, Camelena F, Dahoun M, et al. Prospective evaluation of the Alere i Influenza A&B nucleic acid amplification versus Xpert Flu/RSV. Diagn Microbiol Infect Dis 2016; 85:19–22. [DOI] [PubMed] [Google Scholar]
- 184.Chen JH, Lam HY, Yip CC, et al. Evaluation of the molecular Xpert Xpress Flu/ RSV assay vs. Alere i Influenza A & B assay for rapid detection of influenza viruses. Diagn Microbiol Infect Dis 2018; 90:177–80. [DOI] [PubMed] [Google Scholar]
- 185.Nutter S, Cheung M, Adler-Shohet FC, Krusel K, Vogel K, Meyers H. Evaluation of indirect fluorescent antibody assays compared to rapid influenza diagnostic tests for the detection of pandemic influenza A (H1N1) pdm09. PLoS One 2012; 7:e33097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Sadeghi CD, Aebi C, Gorgievski-Hrisoho M, Muhlemann K, Barbani MT. Twelve years’ detection of respiratory viruses by immunofluorescence in hospitalised children: impact of the introduction of a new respiratory picornavirus assay. BMC Infect Dis 2011; 11:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Peci A, Winter AL, King EC, Blair J, Gubbay JB. Performance of rapid influenza diagnostic testing in outbreak settings. J Clin Microbiol 2014; 52:4309–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Hayden FG, Osterhaus AD, Treanor JJ, et al. Efficacy and safety of the neuraminidase inhibitor zanamivir in the treatment of influenza virus infections. GG167 Influenza Study Group. N Engl J Med 1997; 337:874–80. [DOI] [PubMed] [Google Scholar]
- 189.Treanor JJ, Hayden FG, Vrooman PS, et al. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: a randomized controlled trial. US Oral Neuraminidase Study Group. JAMA 2000; 283:1016–24. [DOI] [PubMed] [Google Scholar]
- 190.Nicholson KG, Aoki FY, Osterhaus AD, et al. Efficacy and safety of oseltamivir in treatment of acute influenza: a randomised controlled trial. Neuraminidase Inhibitor Flu Treatment Investigator Group. Lancet 2000; 355:1845–50. [DOI] [PubMed] [Google Scholar]
- 191.Whitley RJ, Hayden FG, Reisinger KS, et al. Oral oseltamivir treatment of influenza in children. Pediatr Infect Dis J 2001; 20:127–33. [DOI] [PubMed] [Google Scholar]
- 192.Louie JK, Yang S, Acosta M, et al. Treatment with neuraminidase inhibitors for critically ill patients with influenza A (H1N1)pdm09. Clin Infect Dis 2012; 55:1198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Louie JK, Yang S, Samuel MC, Uyeki TM, Schechter R. Neuraminidase inhibitors for critically ill children with influenza. Pediatrics 2013; 132:e1539–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Dobson J, Whitley RJ, Pocock S, Monto AS. Oseltamivir treatment for influenza in adults: a meta-analysis of randomised controlled trials. Lancet 2015; 385:1729–37. [DOI] [PubMed] [Google Scholar]
- 195.Yang SG, Cao B, Liang LR, et al. ; National Influenza A Pandemic (H1N1) 2009 Clinical Investigation Group of China. Antiviral therapy and outcomes of patients with pneumonia caused by influenza A pandemic (H1N1) virus. PLoS One 2012; 7:e29652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Coffin SE, Leckerman K, Keren R, Hall M, Localio R, Zaoutis TE. Oseltamivir shortens hospital stays of critically ill children hospitalized with seasonal influenza: a retrospective cohort study. Pediatr Infect Dis J 2011; 30:962–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Heinonen S, Silvennoinen H, Lehtinen P, et al. Early oseltamivir treatment of influenza in children 1–3 years of age: a randomized controlled trial. Clin Infect Dis 2010; 51:887–94. [DOI] [PubMed] [Google Scholar]
- 198.Chowell G, Viboud C, Simonsen L, et al. Impact of antiviral treatment and hospital admission delay on risk of death associated with 2009 A/H1N1 pandemic influenza in Mexico. BMC Infect Dis 2012; 12:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Lee N, Leo YS, Cao B, et al. Neuraminidase inhibitors, superinfection and corticosteroids affect survival of influenza patients. Eur Respir J 2015; 45:1642–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Malosh RE, Martin ET, Heikkinen T, Brooks WA, Whitley RJ, Monto AS. Efficacy and safety of oseltamivir in children: systematic review and individual patient data meta-analysis of randomized controlled trials. Clin Infect Dis 2018; 66:1492–500. [DOI] [PubMed] [Google Scholar]
- 201.Venkatesan S, Myles PR, Leonardi-Bee J, et al. Impact of outpatient neuraminidase inhibitor treatment in patients infected with influenza A(H1N1)pdm09 at high risk of hospitalization: an individual participant data metaanalysis. Clin Infect Dis 2017; 64:1328–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Doll MK, Winters N, Boikos C, Kraicer-Melamed H, Gore G, Quach C. Safety and effectiveness of neuraminidase inhibitors for influenza treatment, prophylaxis, and outbreak control: a systematic review of systematic reviews and/or meta-analyses. J Antimicrob Chemother 2017; 72:2990–3007. [DOI] [PubMed] [Google Scholar]
- 203.Heneghan CJ, Onakpoya I, Jones MA, et al. Neuraminidase inhibitors for influenza: a systematic review and meta-analysis of regulatory and mortality data. Health Technol Assess 2016; 20:1–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Monto AS, Webster A, Keene O. Randomized, placebo-controlled studies of inhaled zanamivir in the treatment of influenza A and B: pooled efficacy analysis. J Antimicrob Chemother 1999; 44(Suppl B):23–9. [DOI] [PubMed] [Google Scholar]
- 205.Hedrick JA, Barzilai A, Behre U, et al. Zanamivir for treatment of symptomatic influenza A and B infection in children five to twelve years of age: a randomized controlled trial. Pediatr Infect Dis J 2000; 19:410–7. [DOI] [PubMed] [Google Scholar]
- 206.Hayden FG, Treanor JJ, Fritz RS, et al. Use of the oral neuraminidase inhibitor oseltamivir in experimental human influenza: randomized controlled trials for prevention and treatment. JAMA 1999; 282:1240–6. [DOI] [PubMed] [Google Scholar]
- 207.Aoki FY, Macleod MD, Paggiaro P, et al. ; IMPACT Study Group. Early administration of oral oseltamivir increases the benefits of influenza treatment. J Antimicrob Chemother 2003; 51:123–9. [DOI] [PubMed] [Google Scholar]
- 208.Eriksson CO, Graham DA, Uyeki TM, Randolph AG. Risk factors for mechanical ventilation in U.S. children hospitalized with seasonal influenza and 2009 pandemic influenza A. Pediatr Crit Care Med 2012; 13:625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Louie JK, Acosta M, Jamieson DJ, Honein MA; California Pandemic (H1N1) Working Group. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med 2010; 362:27–35. [DOI] [PubMed] [Google Scholar]
- 210.Wang CB, Chiu ML, Lin PC, et al. Prompt oseltamivir therapy reduces medical care and mortality for patients with influenza infection: an Asian population cohort study. Medicine (Baltimore) 2015; 94:e1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Choi SH, Kim T, Park KH, Kwak YG, Chung JW, Lee MS. Early administration of neuraminidase inhibitors in adult patients hospitalized for influenza does not benefit survival: a retrospective cohort study. Eur J Clin Microbiol Infect Dis 2017; 36:1673–7. [DOI] [PubMed] [Google Scholar]
- 212.Wolkewitz M, Schumacher M. Neuraminidase inhibitors and hospital mortality in British patients with H1N1 influenza A: a re-analysis of observational data. PLoS One 2016; 11:e0160430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Stewart RJ, Flannery B, Chung JR, et al. Influenza antiviral prescribing for outpatients with an acute respiratory illness and at high risk for influenza-associated complications during 5 influenza seasons—United States, 2011–2016. Clin Infect Dis 2018; 66:1035–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Appiah GD, Chaves SS, Kirley PD, et al. Increased antiviral treatment among hospitalized children and adults with laboratory-confirmed influenza, 2010–2015. Clin Infect Dis 2017; 64:364–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Qiu S, Shen Y, Pan H, Wang J, Zhang Q. Effectiveness and safety of oseltamivir for treating influenza: an updated meta-analysis of clinical trials. Infect Dis (Lond) 2015; 47:808–19. [DOI] [PubMed] [Google Scholar]
- 216.Committee On Infectious Diseases. Recommendations for prevention and control of influenza in children, 2018–2019. Pediatrics 2018; 142. doi: 10.1542/peds.2018-2367. [DOI] [PubMed] [Google Scholar]
- 217.Lynfield R, Davey R, Dwyer DE, et al. ; INSIGHT Influenza Study Group. Outcomes of influenza A(H1N1)pdm09 virus infection: results from two international cohort studies. PLoS One 2014; 9:e101785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Yu H, Feng Z, Uyeki TM, et al. Risk factors for severe illness with 2009 pandemic influenza A (H1N1) virus infection in China. Clin Infect Dis 2011; 52:457–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Louie JK, Acosta M, Winter K, et al. ; California Pandemic (H1N1) Working Group. Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA 2009; 302:1896–902. [DOI] [PubMed] [Google Scholar]
- 220.Dominguez-Cherit G, Lapinsky SE, Macias AE, et al. Critically ill patients with 2009 influenza A(H1N1) in Mexico. JAMA 2009; 302:1880–7. [DOI] [PubMed] [Google Scholar]
- 221.Chemaly RF, Torres HA, Aguilera EA, et al. Neuraminidase inhibitors improve outcome of patients with leukemia and influenza: an observational study. Clin Infect Dis 2007; 44:964–7. [DOI] [PubMed] [Google Scholar]
- 222.Rasmussen SA, Jamieson DJ, Uyeki TM. Effects of influenza on pregnant women and infants. Am J Obstet Gynecol 2012; 207:S3–8. [DOI] [PubMed] [Google Scholar]
- 223.Rasmussen SA, Kissin DM, Yeung LF, et al. Preparing for influenza after 2009 H1N1: special considerations for pregnant women and newborns. Am J Obstet Gynecol 2011; 204(6 Suppl 1):S13–20. [DOI] [PubMed] [Google Scholar]
- 224.Rasmussen SA, Power ML, Jamieson DJ, et al. Practices of obstetrician-gynecol-ogists regarding nonvaccine-related public health recommendations during the 2009 H1N1 influenza pandemic. Am J Obstet Gynecol 2012; 207:294.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Freeman DW, Barno A. Deaths from Asian influenza associated with pregnancy. Am J Obstet Gynecol 1959; 78:1172–5. [DOI] [PubMed] [Google Scholar]
- 226.Hardy JM, Azarowicz EN, Mannini A, Medearis DN Jr, Cooke RE. The effect of Asian influenza on the outcome of pregnancy, Baltimore, 1957–1958. Am J Public Health Nations Health 1961; 51:1182–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Jamieson DJ, Honein MA, Rasmussen SA, et al. ; Novel Influenza A (H1N1) Pregnancy Working Group. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 2009; 374:451–8. [DOI] [PubMed] [Google Scholar]
- 228.Mertz D, Kim TH, Johnstone J, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ 2013; 347:f5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Neuzil KM, Reed GW, Mitchel EF, Simonsen L, Griffin MR. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol 1998; 148:1094–102. [DOI] [PubMed] [Google Scholar]
- 230.Irving WL, James DK, Stephenson T, et al. Influenza virus infection in the second and third trimesters of pregnancy: a clinical and seroepidemiological study. BJOG 2000; 107:1282–9. [DOI] [PubMed] [Google Scholar]
- 231.Cox S, Posner SF, McPheeters M, Jamieson DJ, Kourtis AP, Meikle S. Hospitalizations with respiratory illness among pregnant women during influenza season. Obstet Gynecol 2006; 107:1315–22. [DOI] [PubMed] [Google Scholar]
- 232.Louie JK, Salibay CJ, Kang M, Glenn-Finer RE, Murray EL, Jamieson DJ. Pregnancy and severe influenza infection in the 2013–2014 influenza season. Obstet Gynecol 2015; 125:184–92. [DOI] [PubMed] [Google Scholar]
- 233.Nair P, Davies AR, Beca J, et al. Extracorporeal membrane oxygenation for severe ARDS in pregnant and postpartum women during the 2009 H1N1 pandemic. Intensive Care Med 2011; 37:648–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Mosby LG, Rasmussen SA, Jamieson DJ. 2009 pandemic influenza A (H1N1) in pregnancy: a systematic review of the literature. Am J Obstet Gynecol 2011; 205:10–8. [DOI] [PubMed] [Google Scholar]
- 235.Bloom-Feshbach K, Simonsen L, Viboud C, et al. Natality decline and miscarriages associated with the 1918 influenza pandemic: the Scandinavian and United States experiences. J Infect Dis 2011; 204:1157–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.McNeil SA, Dodds LA, Fell DB, et al. Effect of respiratory hospitalization during pregnancy on infant outcomes. Am J Obstet Gynecol 2011; 204:S54–7. [DOI] [PubMed] [Google Scholar]
- 237.Mendez-Figueroa H, Raker C, Anderson BL. Neonatal characteristics and out-comes of pregnancies complicated by influenza infection during the 2009 pandemic. Am J Obstet Gynecol 2011; 204(6 Suppl 1):S58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Yates L, Pierce M, Stephens S, et al. Influenza A/H1N1v in pregnancy: an investigation of the characteristics and management of affected women and the relationship to pregnancy outcomes for mother and infant. Health Technol Assess 2010; 14:109–82. [DOI] [PubMed] [Google Scholar]
- 239.Håberg SE, Trogstad L, Gunnes N, et al. Risk of fetal death after pandemic influenza virus infection or vaccination. N Engl J Med 2013; 368:333–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Naresh A, Fisher BM, Hoppe KK, et al. A multicenter cohort study of pregnancy outcomes among women with laboratory-confirmed H1N1 influenza. J Perinatol 2013; 33:939–43. [DOI] [PubMed] [Google Scholar]
- 241.Griffiths PD, Ronalds CJ, Heath RB. A prospective study of influenza infections during pregnancy. J Epidemiol Community Health 1980; 34:124–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Hartert TV, Neuzil KM, Shintani AK, et al. Maternal morbidity and perinatal out-comes among pregnant women with respiratory hospitalizations during influenza season. Am J Obstet Gynecol 2003; 189:1705–12. [DOI] [PubMed] [Google Scholar]
- 243.Luteijn JM, Brown MJ, Dolk H. Influenza and congenital anomalies: a systematic review and meta-analysis. Hum Reprod 2014; 29:809–23. [DOI] [PubMed] [Google Scholar]
- 244.Oluyomi-Obi T, Avery L, Schneider C, et al. Perinatal and maternal outcomes in critically ill obstetrics patients with pandemic H1N1 influenza A. J Obstet Gynaecol Can 2010; 32:443–7. [DOI] [PubMed] [Google Scholar]
- 245.Ellington SR, Hartman LK, Acosta M, et al. Pandemic 2009 influenza A (H1N1) in 71 critically ill pregnant women in California. Am J Obstet Gynecol 2011; 204(6 Suppl 1):S21–30. [DOI] [PubMed] [Google Scholar]
- 246.Fry AM, Goswami D, Nahar K, et al. Effects of oseltamivir treatment of index patients with influenza on secondary household illness in an urban setting in Bangladesh: secondary analysis of a randomised, placebo-controlled trial. Lancet Infect Dis 2015; 15:654–62. [DOI] [PubMed] [Google Scholar]
- 247.Ng S, Cowling BJ, Fang VJ, et al. Effects of oseltamivir treatment on duration of clinical illness and viral shedding and household transmission of influenza virus. Clin Infect Dis 2010; 50:707–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Nishiura H, Oshitani H. Household transmission of influenza (H1N1–2009) in Japan: age-specificity and reduction of household transmission risk by zanamivir treatment. J Int Med Res 2011; 39:619–28. [DOI] [PubMed] [Google Scholar]
- 249.Bright RA, Shay DK, Shu B, Cox NJ, Klimov AI. Adamantane resistance among influenza A viruses isolated early during the 2005–2006 influenza season in the United States. JAMA 2006; 295:891–4. [DOI] [PubMed] [Google Scholar]
- 250.Nguyen HT, Fry AM, Gubareva LV. Neuraminidase inhibitor resistance in influenza viruses and laboratory testing methods. Antivir Ther 2012; 17:159–73. [DOI] [PubMed] [Google Scholar]
- 251.Marty FM, Vidal-Puigserver J, Clark C, et al. Intravenous zanamivir or oral oseltamivir for hospitalised patients with influenza: an international, randomised, double-blind, double-dummy, phase 3 trial. Lancet Respir Med 2017; 5:135–46. [DOI] [PubMed] [Google Scholar]
- 252.Duval X, van der Werf S, Blanchon T, et al. ; Bivir Study Group. Efficacy of oseltamivir-zanamivir combination compared to each monotherapy for seasonal influenza: a randomized placebo-controlled trial. PLoS Med 2010; 7:e1000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Beigel JH, Bao Y, Beeler J, et al. ; IRC003 Study Team. Oseltamivir, amantadine, and ribavirin combination antiviral therapy versus oseltamivir monotherapy for the treatment of influenza: a multicentre, double-blind, randomised phase 2 trial. Lancet Infect Dis 2017; 17:1255–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Jefferson T, Jones M, Doshi P, Spencer EA, Onakpoya I, Heneghan CJ. Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments. BMJ 2014; 348:g2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Nakamura Y, Sugawara T, Ohkusa Y, et al. Life-threatening abnormal behavior incidence in 10–19 year old patients administered neuraminidase inhibitors. PLoS One 2015; 10:e0129712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Nakamura Y, Sugawara T, Ohkusa Y, et al. Severe abnormal behavior incidence after administration of neuraminidase inhibitors using the national database of medical claims. J Infect Chemother 2018; 24:177–81. [DOI] [PubMed] [Google Scholar]
- 257.Harrington R, Adimadhyam S, Lee TA, Schumock GT, Antoon JW. The relationship between oseltamivir and suicide in pediatric patients. Ann Fam Med 2018; 16:145–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Fukushima W, Ozasa K, Okumura A, et al. Oseltamivir use and severe abnormal behavior in Japanese children and adolescents with influenza: is a self-controlled case series study applicable? Vaccine 2017; 35:4817–24. [DOI] [PubMed] [Google Scholar]
- 259.Heneghan CJ, Onakpoya I, Thompson M, Spencer EA, Jones M, Jefferson T. Zanamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments. BMJ 2014; 348:g2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Whitley R, Laughlin A, Carson S, et al. Single dose peramivir for the treatment of acute seasonal influenza: integrated analysis of efficacy and safety from two placebo-controlled trials. Antivir Ther 2015; 20:709–19. [DOI] [PubMed] [Google Scholar]
- 261.Acosta EP, Jester P, Gal P, et al. ; National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. Oseltamivir dosing for influenza infection in premature neonates. J Infect Dis 2010; 202:563–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Kimberlin DW, Acosta EP, Prichard MN, et al. ; National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. Oseltamivir pharmacokinetics, dosing, and resistance among children aged <2 years with influenza. J Infect Dis 2013; 207:709–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Standing JF, Nika A, Tsagris V, et al. Oseltamivir pharmacokinetics and clinical experience in neonates and infants during an outbreak of H1N1 influenza A virus infection in a neonatal intensive care unit. Antimicrob Agents Chemother 2012; 56:3833–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Sugaya N, Kohno S, Ishibashi T, Wajima T, Takahashi T. Efficacy, safety, and pharmacokinetics of intravenous peramivir in children with 2009 pandemic H1N1 influenza A virus infection. Antimicrob Agents Chemother 2012; 56:369–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Hernandez JE, Adiga R, Armstrong R, et al. Clinical experience in adults and children treated with intravenous peramivir for 2009 influenza A (H1N1) under an emergency IND program in the United States. Clin Infect Dis 2011; 52:695–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Bradley JS, Blumer JL, Romero JR, et al. Intravenous zanamivir in hospitalized patients with influenza. Pediatrics 2017; 140. doi: 10.1542/peds.2016-2727. [DOI] [PubMed] [Google Scholar]
- 267.Diggory P, Fernandez C, Humphrey A, Jones V, Murphy M. Comparison of elderly people’s technique in using two dry powder inhalers to deliver zanamivir: randomised controlled trial. BMJ 2001; 322:577–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Oboho IK, Reed C, Gargiullo P, et al. Benefit of Early Initiation of Influenza Antiviral Treatment to Pregnant Women Hospitalized With Laboratory-Confirmed Influenza. J Infect Dis 2016; 214:507–15. [DOI] [PubMed] [Google Scholar]
- 269.Beigi RH, Han K, Venkataramanan R, et al. ; Obstetric-Fetal Pharmacology Research Units Network. Pharmacokinetics of oseltamivir among pregnant and nonpregnant women. Am J Obstet Gynecol 2011; 204:S84–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Pillai VC, Han K, Beigi RH, et al. Population pharmacokinetics of oseltamivir in non-pregnant and pregnant women. Br J Clin Pharmacol 2015; 80:1042–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Huang H, Wang J, Li Q, et al. Transplacental transfer of oseltamivir phosphate and its metabolite oseltamivir carboxylate using the ex vivo human placenta perfusion model in Chinese Hans population. J Matern Fetal Neonatal Med 2017; 30:1288–92. [DOI] [PubMed] [Google Scholar]
- 272.Nanovskaya TN, Patrikeeva S, Zhan Y, Hankins GD, Ahmed MS. Transplacental transfer of oseltamivir carboxylate. J Matern Fetal Neonatal Med 2012; 25:2312–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Meijer WJ, Bruinse HW, van den Broek MP, Kromdijk W, Wensing AM. Oseltamivir and its active metabolite cross the placenta at significant levels. Clin Infect Dis 2012; 54:1676–7. [DOI] [PubMed] [Google Scholar]
- 274.Berveiller P, Mir O, Vinot C, et al. Transplacental transfer of oseltamivir and its metabolite using the human perfused placental cotyledon model. Am J Obstet Gynecol 2012; 206:92e1–6. [DOI] [PubMed] [Google Scholar]
- 275.Greer LG, Leff RD, Rogers VL, et al. Pharmacokinetics of oseltamivir according to trimester of pregnancy. Am J Obstet Gynecol 2011; 204:S89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Tanaka T, Nakajima K, Murashima A, Garcia-Bournissen F, Koren G, Ito S. Safety of neuraminidase inhibitors against novel influenza A (H1N1) in pregnant and breastfeeding women. CMAJ 2009; 181:55–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Dickey RP, Xiong X, Xie Y, Gee RE, Pridjian G. Effect of maternal height and weight on risk for preterm singleton and twin births resulting from IVF in the United States, 2008–2010. Am J Obstet Gynecol 2013; 209:349e1–6. [DOI] [PubMed] [Google Scholar]
- 278.Saito S, Minakami H, Nakai A, Unno N, Kubo T, Yoshimura Y. Outcomes of infants exposed to oseltamivir or zanamivir in utero during pandemic (H1N1) 2009. Am J Obstet Gynecol 2013; 209:130.e1–9. [DOI] [PubMed] [Google Scholar]
- 279.Dunstan HJ, Mill AC, Stephens S, Yates LM, Thomas SH. Pregnancy outcome following maternal use of zanamivir or oseltamivir during the 2009 influenza A/H1N1 pandemic: a national prospective surveillance study. BJOG 2014; 121:901–6. [DOI] [PubMed] [Google Scholar]
- 280.Xie HY, Yasseen AS III, Xie RH, et al. Infant outcomes among pregnant women who used oseltamivir for treatment of influenza during the H1N1 epidemic. Am J Obstet Gynecol 2013; 208:293e1–7. [DOI] [PubMed] [Google Scholar]
- 281.Beau AB, Hurault-Delarue C, Vial T, Montastruc JL, Damase-Michel C, Lacroix I. Safety of oseltamivir during pregnancy: a comparative study using the EFEMERIS database. BJOG 2014; 121:895–900. [DOI] [PubMed] [Google Scholar]
- 282.Sorbello A, Jones SC, Carter W, et al. Emergency use authorization for intravenous peramivir: evaluation of safety in the treatment of hospitalized patients infected with 2009 H1N1 influenza A virus. Clin Infect Dis 2012; 55:1–7. [DOI] [PubMed] [Google Scholar]
- 283.Louie JK, Yang S, Yen C, Acosta M, Schechter R, Uyeki TM. Use of intravenous peramivir for treatment of severe influenza A(H1N1)pdm09. PLoS One 2012; 7:e40261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Yu Y, Garg S, Yu PA, et al. Peramivir use for treatment of hospitalized patients with influenza A(H1N1)pdm09 under emergency use authorization, October 2009-June 2010. Clin Infect Dis 2012; 55:8–15. [DOI] [PubMed] [Google Scholar]
- 285.Chan-Tack KM, Kim C, Moruf A, Birnkrant DB. Clinical experience with intravenous zanamivir under an emergency IND program in the United States (2011–2014). Antivir Ther 2015; 20:561–4. [DOI] [PubMed] [Google Scholar]
- 286.Chan-Tack KM, Gao A, Himaya AC, et al. Clinical experience with intravenous zanamivir under an emergency investigational new drug program in the United States. J Infect Dis 2013; 207:196–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Renaud C, Boudreault AA, Kuypers J, et al. H275Y mutant pandemic (H1N1) 2009 virus in immunocompromised patients. Emerg Infect Dis 2011; 17:653–60; quiz 765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Shah DP, Ghantoji SS, Ariza-Heredia EJ, et al. Immunodeficiency scoring index to predict poor outcomes in hematopoietic cell transplant recipients with RSV infections. Blood 2014; 123:3263–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Graitcer SB, Gubareva L, Kamimoto L, et al. Characteristics of patients with oseltamivir-resistant pandemic (H1N1) 2009, United States. Emerg Infect Dis 2011; 17:255–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients [manuscript published online ahead of print 7 April 2018]. Clin Infect Dis 2018. doi: 10.1093/cid/ciy294. [DOI] [Google Scholar]
- 291.Kumar D, Michaels MG, Morris MI, et al. ; American Society of Transplantation H1N1 Collaborative Study Group. Outcomes from pandemic influenza A H1N1 infection in recipients of solid-organ transplants: a multicentre cohort study. Lancet Infect Dis 2010; 10:521–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Reid G, Huprikar S, Patel G, et al. A multicenter evaluation of pandemic influenza A/H1N1 in hematopoietic stem cell transplant recipients. Transpl Infect Dis 2013; 15:487–92. [DOI] [PubMed] [Google Scholar]
- 293.Ariano RE, Sitar DS, Zelenitsky SA, et al. Enteric absorption and pharmacokinetics of oseltamivir in critically ill patients with pandemic (H1N1) influenza. CMAJ 2010; 182:357–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Mulla H, Peek GJ, Harvey C, Westrope C, Kidy Z, Ramaiah R. Oseltamivir pharmacokinetics in critically ill adults receiving extracorporeal membrane oxygenation support. Anaesth Intensive Care 2013; 41:66–73. [DOI] [PubMed] [Google Scholar]
- 295.Flannery AH, Thompson Bastin ML. Oseltamivir dosing in critically ill patients with severe influenza. Ann Pharmacother 2014; 48:1011–8. [DOI] [PubMed] [Google Scholar]
- 296.Kiatboonsri S, Kiatboonsri C, Theerawit P. Fatal respiratory events caused by zan-amivir nebulization. Clin Infect Dis 2010; 50:620. [DOI] [PubMed] [Google Scholar]
- 297.Steel HM, Peppercorn AF. Fatal respiratory events caused by zanamivir nebulization. Clin Infect Dis 2010; 51:121. [DOI] [PubMed] [Google Scholar]
- 298.de Jong MD, Ison MG, Monto AS, et al. Evaluation of intravenous peramivir for treatment of influenza in hospitalized patients. Clin Infect Dis 2014; 59:e172–85. [DOI] [PubMed] [Google Scholar]
- 299.To KK, Hung IF, Li IW, et al. Delayed clearance of viral load and marked cytokine activation in severe cases of pandemic H1N1 2009 influenza virus infection. Clin Infect Dis 2010; 50:850–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Welch SC, Lam SW, Neuner EA, Bauer SR, Bass SN. High-dose versus standard dose oseltamivir for treatment of severe influenza in adult intensive care unit patients. Intensive Care Med 2015; 41:1365–6. [DOI] [PubMed] [Google Scholar]
- 301.Pai MP, Lodise TP Jr. Oseltamivir and oseltamivir carboxylate pharmacokinetics in obese adults: dose modification for weight is not necessary. Antimicrob Agents Chemother 2011; 55:5640–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Thorne-Humphrey LM, Goralski KB, Slayter KL, Hatchette TF, Johnston BL, McNeil SA; 2009 OPTIMO Study Group. Oseltamivir pharmacokinetics in morbid obesity (OPTIMO trial). J Antimicrob Chemother 2011; 66:2083–91. [DOI] [PubMed] [Google Scholar]
- 303.Murphy KR, Eivindson A, Pauksens K, et al. Efficacy and safety of inhaled zanam-ivir for the treatment of influenza in patients with asthma or chronic obstructive pulmonary disease: a double-blind, randomised, placebo-controlled, multicentre study. Clin Drug Invest 2000; 20:337–49. [Google Scholar]
- 304.Williamson JC, Pegram PS. Respiratory distress associated with zanamivir. N Engl J Med 2000; 342:661–2. [DOI] [PubMed] [Google Scholar]
- 305.Campigotto A, Mubareka S. Influenza-associated bacterial pneumonia; managing and controlling infection on two fronts. Expert Rev Anti Infect Ther 2015; 13:55–68. [DOI] [PubMed] [Google Scholar]
- 306.Metersky ML, Masterton RG, Lode H, File TM Jr, Babinchak T. Epidemiology, microbiology, and treatment considerations for bacterial pneumonia complicating influenza. Int J Infect Dis 2012; 16:e321–31. [DOI] [PubMed] [Google Scholar]
- 307.Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis 2008; 198:962–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Randolph AG, Vaughn F, Sullivan R, et al. Critically ill children during the 2009–2010 influenza pandemic in the United States. Pediatrics 2011; 128:e1450–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Pfister R, Kochanek M, Leygeber T, et al. Procalcitonin for diagnosis of bacterial pneumonia in critically ill patients during 2009 H1N1 influenza pandemic: a prospective cohort study, systematic review and individual patient data meta-analysis. Crit Care 2014; 18:R44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.McCullers JA. Do specific virus-bacteria pairings drive clinical outcomes of pneumonia? Clin Microbiol Infect 2013; 19:113–8. [DOI] [PubMed] [Google Scholar]
- 311.Reichert T, Chowell G, McCullers JA. The age distribution of mortality due to influenza: pandemic and peri-pandemic. BMC Med 2012; 10:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Alymova IV, Samarasinghe A, Vogel P, Green AM, Weinlich R, McCullers JA. A novel cytotoxic sequence contributes to influenza A viral protein PB1-F2 pathogenicity and predisposition to secondary bacterial infection. J Virol 2014; 88:503–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.McCullers JA. The co-pathogenesis of influenza viruses with bacteria in the lung. Nat Rev Microbiol 2014; 12:252–62. [DOI] [PubMed] [Google Scholar]
- 314.Smith AM, McCullers JA. Secondary bacterial infections in influenza virus infection pathogenesis. Curr Top Microbiol Immunol 2014; 385:327–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Dawood FS, Chaves SS, Perez A, et al. Complications and associated bacterial coinfections among children hospitalized with seasonal or pandemic influenza, United States, 2003–2010. J Infect Dis 2014; 209:686–94. [DOI] [PubMed] [Google Scholar]
- 316.Kallen AJ, Reed C, Patton M, Arnold KE, Finelli L, Hageman J. Staphylococcus aureus community-onset pneumonia in patients admitted to children’s hospitals during autumn and winter of 2006–2007. Epidemiol Infect 2010; 138:666–72. [DOI] [PubMed] [Google Scholar]
- 317.Reed C, Kallen AJ, Patton M, et al. Infection with community-onset Staphylococcus aureus and influenza virus in hospitalized children. Pediatr Infect Dis J 2009; 28:572–6. [DOI] [PubMed] [Google Scholar]
- 318.Jean C, Louie JK, Glaser CA, et al. Invasive group A streptococcal infection concurrent with 2009 H1N1 influenza. Clin Infect Dis 2010; 50:e59–62. [DOI] [PubMed] [Google Scholar]
- 319.Allard R, Couillard M, Pilon P, Kafka M, Bedard L. Invasive bacterial infections following influenza: a time-series analysis in Montreal, Canada, 1996–2008. Influenza Other Respir Viruses 2012; 6:268–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Polin RA; Committee on Fetus and Newborn. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics 2012; 129:1006–15. [DOI] [PubMed] [Google Scholar]
- 321.Annual data report of the US Organ Procurement and Transplantation Network (OPTN) and the scientific registry of transplant recipients (SRTR) preface. Am J Transplant 2013; 13(Suppl 1):1–7. [DOI] [PubMed] [Google Scholar]
- 322.Nair GB, Niederman MS. Ventilator-associated pneumonia: present understanding and ongoing debates. Intensive Care Med 2015; 41:34–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Kollef MH, Morrow LE, Baughman RP, et al. Health care-associated pneumonia (HCAP): a critical appraisal to improve identification, management, and outcomes—proceedings of the HCAP Summit. Clin Infect Dis 2008; 46(Suppl 4):S296–334; quiz 335–8. [DOI] [PubMed] [Google Scholar]
- 324.Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 2016; 63:e61–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Stockmann C, Ampofo K, Killpack J, et al. Procalcitonin accurately identifies hospitalized children with low risk of bacterial community-acquired pneumonia. J Pediatric Infect Dis Soc 2018; 7:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Wu MH, Lin CC, Huang SL, et al. Can procalcitonin tests aid in identifying bacterial infections associated with influenza pneumonia? A systematic review and meta-analysis. Influenza Other Respir Viruses 2013; 7:349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Schuetz P, Wirz Y, Sager R, et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: a patient level meta-analysis. Lancet Infect Dis 2018; 18:95–107. [DOI] [PubMed] [Google Scholar]
- 328.Izurieta HS, Thompson WW, Kramarz P, et al. Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 2000; 342:232–9. [DOI] [PubMed] [Google Scholar]
- 329.Poehling KA, Edwards KM, Griffin MR, et al. The burden of influenza in young children, 2004–2009. Pediatrics 2013; 131:207–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Takada T, Mikami A, Kitamura N, et al. Efficacy and safety of long-term sirolimus therapy for Asian patients with lymphangioleiomyomatosis. Ann Am Thorac Soc 2016; 13:1912–22. [DOI] [PubMed] [Google Scholar]
- 331.Nishino M, Boswell EN, Hatabu H, Ghobrial IM, Ramaiya NH. Drug-related pneumonitis during mammalian target of rapamycin inhibitor therapy: radiographic pattern-based approach in Waldenstrom macroglobulinemia as a paradigm. Oncologist 2015; 20:1077–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Centers for Disease Control and Prevention. Oseltamivir-resistant novel influenza A (H1N1) virus infection in two immunosuppressed patients—Seattle, Washington, 2009. MMWR Morb Mortal Wkly Rep 2009; 58:893–6. [PubMed] [Google Scholar]
- 333.Whitley RJ, Boucher CA, Lina B, et al. Global assessment of resistance to neuraminidase inhibitors, 2008–2011: the Influenza Resistance Information Study (IRIS). Clin Infect Dis 2013; 56:1197–205. [DOI] [PubMed] [Google Scholar]
- 334.Stephenson I, Democratis J, Lackenby A, et al. Neuraminidase inhibitor resistance after oseltamivir treatment of acute influenza A and B in children. Clin Infect Dis 2009; 48:389–96. [DOI] [PubMed] [Google Scholar]
- 335.Baz M, Abed Y, McDonald J, Boivin G. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin Infect Dis 2006; 43:1555–61. [DOI] [PubMed] [Google Scholar]
- 336.Baz M, Abed Y, Papenburg J, Bouhy X, Hamelin ME, Boivin G. Emergence of oseltamivir-resistant pandemic H1N1 virus during prophylaxis. N Engl J Med 2009; 361:2296–7. [DOI] [PubMed] [Google Scholar]
- 337.Escuret V, Collins PJ, Casalegno JS, et al. A novel I221L substitution in neuraminidase confers high-level resistance to oseltamivir in influenza B viruses. J Infect Dis 2014; 210:1260–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Gubareva LV, Matrosovich MN, Brenner MK, Bethell RC, Webster RG. Evidence for zanamivir resistance in an immunocompromised child infected with influenza B virus. J Infect Dis 1998; 178:1257–62. [DOI] [PubMed] [Google Scholar]
- 339.Ison MG, Gubareva LV, Atmar RL, Treanor J, Hayden FG. Recovery of drug-resistant influenza virus from immunocompromised patients: a case series. J Infect Dis 2006; 193:760–4. [DOI] [PubMed] [Google Scholar]
- 340.Tamura D, DeBiasi RL, Okomo-Adhiambo M, et al. Emergence of multidrug-resistant influenza A(H1N1)pdm09 virus variants in an immunocompromised child treated with oseltamivir and zanamivir. J Infect Dis 2015; 212:1209–13. [DOI] [PubMed] [Google Scholar]
- 341.Rocha E, Cox NJ, Black RA, Harmon MW, Harrison CJ, Kendal AP. Antigenic and genetic variation in influenza A (H1N1) virus isolates recovered from a persistently infected immunodeficient child. J Virol 1991; 65:2340–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Calatayud L, Lackenby A, Reynolds A, et al. Oseltamivir-resistant pandemic (H1N1) 2009 virus infection in England and Scotland, 2009–2010. Emerg Infect Dis 2011; 17:1807–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Kiso M, Mitamura K, Sakai-Tagawa Y, et al. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 2004; 364:759–65. [DOI] [PubMed] [Google Scholar]
- 344.Hurt AC, Chotpitayasunondh T, Cox NJ, et al. Antiviral resistance during the 2009 influenza A H1N1 pandemic: public health, laboratory, and clinical perspectives. Lancet Infect Dis 2012; 12:240–8. [DOI] [PubMed] [Google Scholar]
- 345.Nguyen HT, Sheu TG, Mishin VP, Klimov AI, Gubareva LV. Assessment of pandemic and seasonal influenza A (H1N1) virus susceptibility to neuraminidase inhibitors in three enzyme activity inhibition assays. Antimicrob Agents Chemother 2010; 54:3671–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Hu Y, Lu S, Song Z, et al. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 2013; 381:2273–9. [DOI] [PubMed] [Google Scholar]
- 347.Kawai N, Ikematsu H, Iwaki N, et al. Comparison of the effectiveness of zanamivir and oseltamivir against influenza A/H1N1, A/H3N2, and B. Clin Infect Dis 2009; 48:996–7. [DOI] [PubMed] [Google Scholar]
- 348.Sugaya N, Ohashi Y. Long-acting neuraminidase inhibitor laninamivir octanoate (CS-8958) versus oseltamivir as treatment for children with influenza virus infection. Antimicrob Agents Chemother 2010; 54:2575–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Takashita E, Meijer A, Lackenby A, et al. Global update on the susceptibility of human influenza viruses to neuraminidase inhibitors, 2013–2014. Antiviral Res 2015; 117:27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Okomo-Adhiambo M, Fry AM, Su S, et al. ; 2013-14 US Influenza Antiviral Working Group. Oseltamivir-resistant influenza A(H1N1)pdm09 viruses, United States, 2013–14. Emerg Infect Dis 2015; 21:136–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Speers DJ, Williams SH, Pinder M, Moody HR, Hurt AC, Smith DW. Oseltamivir-resistant pandemic (H1N1) 2009 influenza in a severely ill patient: the first Australian case. Med J Aust 2010; 192:166–8. [DOI] [PubMed] [Google Scholar]
- 352.Dulek DE, Williams JV, Creech CB, et al. Use of intravenous zanamivir after development of oseltamivir resistance in a critically ill immunosuppressed child infected with 2009 pandemic influenza A (H1N1) virus. Clin Infect Dis 2010; 50:1493–6. [DOI] [PubMed] [Google Scholar]
- 353.Gaur AH, Bagga B, Barman S, et al. Intravenous zanamivir for oseltamivir-resist- ant 2009 H1N1 influenza. N Engl J Med 2010; 362:88–9. [DOI] [PubMed] [Google Scholar]
- 354.Hoopes JD, Driebe EM, Kelley E, et al. Triple combination antiviral drug (TCAD) composed of amantadine, oseltamivir, and ribavirin impedes the selection of drug-resistant influenza A virus. PLoS One 2011; 6:e29778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Ison MG, Gnann JW Jr, Nagy-Agren S, et al. ; NIAID Collaborative Antiviral Study Group. Safety and efficacy of nebulized zanamivir in hospitalized patients with serious influenza. Antivir Ther 2003; 8:183–90. [PubMed] [Google Scholar]
- 356.Luke TC, Kilbane EM, Jackson JL, Hoffman SL. Meta-analysis: convalescent blood products for Spanish influenza pneumonia: a future H5N1 treatment? Ann Intern Med 2006; 145:599–609. [DOI] [PubMed] [Google Scholar]
- 357.Hung IF, To KK, Lee CK, et al. Hyperimmune IV immunoglobulin treatment: a multicenter double-blind randomized controlled trial for patients with severe 2009 influenza A(H1N1) infection. Chest 2013; 144:464–73. [DOI] [PubMed] [Google Scholar]
- 358.Le QM, Wertheim HF, Tran ND, van Doorn HR, Nguyen TH, Horby P; Vietnam H1N1 Investigation Team. A community cluster of oseltamivir-resistant cases of 2009 H1N1 influenza. N Engl J Med 2010; 362:86–7. [DOI] [PubMed] [Google Scholar]
- 359.Hurt AC, Hardie K, Wilson NJ, et al. Community transmission of oseltamivir-re-sistant A(H1N1)pdm09 influenza. N Engl J Med 2011; 365:2541–2. [DOI] [PubMed] [Google Scholar]
- 360.Takashita E, Ejima M, Itoh R, et al. A community cluster of influenza A(H1N1) pdm09 virus exhibiting cross-resistance to oseltamivir and peramivir in Japan, November to December 2013. Euro Surveill 2014; 19. [DOI] [PubMed] [Google Scholar]
- 361.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 41:580–637. [DOI] [PubMed] [Google Scholar]
- 362.Annane D, Antona M, Lehmann B, et al. Designing and conducting a randomized trial for pandemic critical illness: the 2009 H1N1 influenza pandemic. Intensive Care Med 2012; 38:29–39. [DOI] [PubMed] [Google Scholar]
- 363.Venkatesh B, Finfer S, Myburgh J, Cohen J, Billot L. Long-term outcomes of the ADRENAL trial. N Engl J Med 2018; 378:1744–5. [DOI] [PubMed] [Google Scholar]
- 364.Rodrigo C, Leonardi-Bee J, Nguyen-Van-Tam JS, Lim WS. Effect of corticosteroid therapy on influenza-related mortality: a systematic review and meta-analysis. J Infect Dis 2015; 212:183–94. [DOI] [PubMed] [Google Scholar]
- 365.Zhang Y, Sun W, Svendsen ER, et al. Do corticosteroids reduce the mortality of influenza A (H1N1) infection? A meta-analysis. Crit Care 2015; 19:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Yang JW, Fan LC, Miao XY, et al. Corticosteroids for the treatment of human infection with influenza virus: a systematic review and meta-analysis. Clin Microbiol Infect 2015; 21:956–63. [DOI] [PubMed] [Google Scholar]
- 367.Brun-Buisson C, Richard JC, Mercat A, Thiébaut AC, Brochard L; REVA-SRLF A/ H1N1v 2009 Registry Group. Early corticosteroids in severe influenza A/H1N1 pneumonia and acute respiratory distress syndrome. Am J Respir Crit Care Med 2011; 183:1200–6. [DOI] [PubMed] [Google Scholar]
- 368.Kim SH, Hong SB, Yun SC, et al. Corticosteroid treatment in critically ill patients with pandemic influenza A/H1N1 2009 infection: analytic strategy using propensity scores. Am J Respir Crit Care Med 2011; 183:1207–14. [DOI] [PubMed] [Google Scholar]
- 369.Han K, Ma H, An X, et al. Early use of glucocorticoids was a risk factor for critical disease and death from pH1N1 infection. Clin Infect Dis 2011; 53:326–33. [DOI] [PubMed] [Google Scholar]
- 370.Delaney JW, Pinto R, Long J, et al. ; Canadian Critical Care Trials Group H1N1 Collaborative. The influence of corticosteroid treatment on the outcome of influenza A(H1N1pdm09)-related critical illness. Crit Care 2016; 20:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Li H, Yang SG, Gu L, et al. ; National Influenza A(H1N1)pdm09 Clinical Investigation Group of China. Effect of low-to-moderate-dose corticosteroids on mortality of hospitalized adolescents and adults with influenza A(H1N1)pdm09 viral pneumonia. Influenza Other Respir Viruses 2017; 11:345–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Cao B, Gao H, Zhou B, et al. Adjuvant corticosteroid treatment in adults with influenza A (H7N9) viral pneumonia. Crit Care Med 2016; 44:e318–28. [DOI] [PubMed] [Google Scholar]
- 373.Lee N, Cockram CS, Chan PK, Hui DS, Choi KW, Sung JJ. Antiviral treatment for patients hospitalized with severe influenza infection may affect clinical outcomes. Clin Infect Dis 2008; 46:1323–4. [DOI] [PubMed] [Google Scholar]
- 374.Giannella M, Alonso M, Garcia de Viedma D, et al. Prolonged viral shedding in pandemic influenza A(H1N1): clinical significance and viral load analysis in hospitalized patients. Clin Microbiol Infect 2011; 17:1160–5. [DOI] [PubMed] [Google Scholar]
- 375.Lee N, Chan PK, Hui DS, et al. Viral loads and duration of viral shedding in adult patients hospitalized with influenza. J Infect Dis 2009; 200:492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Linko R, Pettila V, Ruokonen E, et al. ; FINNH1N1-Study Group. Corticosteroid therapy in intensive care unit patients with PCR-confirmed influenza A(H1N1) infection in Finland. Acta Anaesthesiol Scand 2011; 55:971–9. [DOI] [PubMed] [Google Scholar]
- 377.Viasus D, Pano-Pardo JR, Cordero E, et al. Effect of immunomodulatory therapies in patients with pandemic influenza A (H1N1) 2009 complicated by pneumonia. J Infect 2011; 62:193–9. [DOI] [PubMed] [Google Scholar]
- 378.Martin-Loeches I, Lisboa T, Rhodes A, et al. ; ESICM H1N1 Registry Contributors. Use of early corticosteroid therapy on ICU admission in patients affected by severe pandemic (H1N1)v influenza A infection. Intensive Care Med 2011; 37:272–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Hung IF, To KK, Lee CK, et al. Convalescent plasma treatment reduced mortality in patients with severe pandemic influenza A (H1N1) 2009 virus infection. Clin Infect Dis 2011; 52:447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Beigel JH, Tebas P, Elie-Turenne MC, et al. ; IRC002 Study Team. Immune plasma for the treatment of severe influenza: an open-label, multicentre, phase 2 randomised study. Lancet Respir Med 2017; 5:500–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Fedson DS. Treating influenza with statins and other immunomodulatory agents. Antiviral Res 2013; 99:417–35. [DOI] [PubMed] [Google Scholar]
- 382.Lee N, Wong CK, Chan MCW, et al. Anti-inflammatory effects of adjunctive mac-rolide treatment in adults hospitalized with influenza: a randomized controlled trial. Antiviral Res 2017; 144:48–56. [DOI] [PubMed] [Google Scholar]
- 383.Hung IFN, To KKW, Chan JFW, et al. Efficacy of clarithromycin-naprox- en-oseltamivir combination in the treatment of patients hospitalized for influenza A(H3N2) infection: an open-label randomized, controlled, phase IIb/III trial. Chest 2017; 151:1069–80. [DOI] [PubMed] [Google Scholar]
- 384.Hayden FG, Atmar RL, Schilling M, et al. Use of the selective oral neuraminidase inhibitor oseltamivir to prevent influenza. N Engl J Med 1999; 341:1336–43. [DOI] [PubMed] [Google Scholar]
- 385.Monto AS, Robinson DP, Herlocher ML, Hinson JM Jr, Elliott MJ, Crisp A. Zanamivir in the prevention of influenza among healthy adults: a randomized controlled trial. JAMA 1999; 282:31–5. [DOI] [PubMed] [Google Scholar]
- 386.Kaiser L, Henry D, Flack NP, Keene O, Hayden FG. Short-term treatment with zanamivir to prevent influenza: results of a placebo-controlled study. Clin Infect Dis 2000; 30:587–9. [DOI] [PubMed] [Google Scholar]
- 387.Hayden FG, Gubareva LV, Monto AS, et al. ; Zanamivir Family Study Group. Inhaled zanamivir for the prevention of influenza in families. Zanamivir Family Study Group. N Engl J Med 2000; 343:1282–9. [DOI] [PubMed] [Google Scholar]
- 388.Welliver R, Monto AS, Carewicz O, et al. ; Oseltamivir Post Exposure Prophylaxis Investigator Group. Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. JAMA 2001; 285:748–54. [DOI] [PubMed] [Google Scholar]
- 389.Monto AS, Pichichero ME, Blanckenberg SJ, et al. Zanamivir prophylaxis: an effective strategy for the prevention of influenza types A and B within households. J Infect Dis 2002; 186:1582–8. [DOI] [PubMed] [Google Scholar]
- 390.Hayden FG, Belshe R, Villanueva C, et al. Management of influenza in households: a prospective, randomized comparison of oseltamivir treatment with or without postexposure prophylaxis. J Infect Dis 2004; 189:440–9. [DOI] [PubMed] [Google Scholar]
- 391.LaForce C, Man CY, Henderson FW, et al. Efficacy and safety of inhaled zan- amivir in the prevention of influenza in community-dwelling, high-risk adult and adolescent subjects: a 28-day, multicenter, randomized, double-blind, placebo-controlled trial. Clin Ther 2007; 29:1579–90; discussion 1577–8. [DOI] [PubMed] [Google Scholar]
- 392.Jefferson T, Jones M, Doshi P, Del Mar C. Neuraminidase inhibitors for preventing and treating influenza in healthy adults: systematic review and meta-analysis. BMJ 2009; 339:b5106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Okoli GN, Otete HE, Beck CR, Nguyen-Van-Tam JS. Use of neuraminidase inhibitors for rapid containment of influenza: a systematic review and meta-analysis of individual and household transmission studies. PLoS One 2014; 9:e113633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Ison MG, Szakaly P, Shapira MY, Krivan G, Nist A, Dutkowski R. Efficacy and safety of oral oseltamivir for influenza prophylaxis in transplant recipients. Antivir Ther 2012; 17:955–64. [DOI] [PubMed] [Google Scholar]
- 395.Anekthananon T, Pukrittayakamee S, Pukritayakamee S, et al. Oseltamivir and inhaled zanamivir as influenza prophylaxis in Thai health workers: a randomized, double-blind, placebo-controlled safety trial over 16 weeks. J Antimicrob Chemother 2013; 68:697–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Nichols WG, Guthrie KA, Corey L, Boeckh M. Influenza infections after hematopoietic stem cell transplantation: risk factors, mortality, and the effect of antiviral therapy. Clin Infect Dis 2004; 39:1300–6. [DOI] [PubMed] [Google Scholar]
- 397.Choi SM, Boudreault AA, Xie H, Englund JA, Corey L, Boeckh M. Differences in clinical outcomes after 2009 influenza A/H1N1 and seasonal influenza among hematopoietic cell transplant recipients. Blood 2011; 117:5050–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Jackson RJ, Cooper KL, Tappenden P, et al. Oseltamivir, zanamivir and amantadine in the prevention of influenza: a systematic review. J Infect 2011; 62:14–25. [DOI] [PubMed] [Google Scholar]
- 399.Cho HG, Choi JH, Kim WH, et al. High prevalence of amantadine-resistant influenza A virus isolated in Gyeonggi Province, South Korea, during 2005–2010. Arch Virol 2013; 158:241–5. [DOI] [PubMed] [Google Scholar]
- 400.Sheu TG, Fry AM, Garten RJ, et al. Dual resistance to adamantanes and oseltam-ivir among seasonal influenza A(H1N1) viruses: 2008–2010. J Infect Dis 2011; 203:13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Dharan NJ, Gubareva LV, Meyer JJ, et al. ; Oseltamivir-Resistance Working Group. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA 2009; 301:1034–41. [DOI] [PubMed] [Google Scholar]
- 402.Lackenby A, Hungnes O, Dudman SG, et al. Emergence of resistance to oseltam-ivir among influenza A(H1N1) viruses in Europe. Euro Surveill 2008; 13. [DOI] [PubMed] [Google Scholar]
- 403.Dapat C, Kondo H, Dapat IC, et al. Neuraminidase inhibitor susceptibility profile of pandemic and seasonal influenza viruses during the 2009–2010 and 2010–2011 influenza seasons in Japan. Antiviral Res 2013; 99:261–9. [DOI] [PubMed] [Google Scholar]
- 404.Garg S, Moore Z, Lee N, et al. A cluster of patients infected with I221V influenza b virus variants with reduced oseltamivir susceptibility—North Carolina and South Carolina, 2010–2011. J Infect Dis 2013; 207:966–73. [DOI] [PubMed] [Google Scholar]
- 405.Hurt AC. The epidemiology and spread of drug resistant human influenza viruses. Curr Opin Virol 2014; 8:22–9. [DOI] [PubMed] [Google Scholar]
- 406.Roussy JF, Abed Y, Bouhy X, Boivin G. Emergence of an oseltamivir-resistant influenza A/H3N2 virus in an elderly patient receiving a suboptimal dose of antiviral prophylaxis. J Clin Microbiol 2013; 51:4234–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Booy R, Lindley RI, Dwyer DE, et al. Treating and preventing influenza in aged care facilities: a cluster randomised controlled trial. PLoS One 2012; 7:e46509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Schilling M, Povinelli L, Krause P, et al. Efficacy of zanamivir for chemoprophylaxis of nursing home influenza outbreaks. Vaccine 1998; 16:1771–4. [DOI] [PubMed] [Google Scholar]
- 409.Gravenstein S, Drinka P, Osterweil D, et al. Inhaled zanamivir versus rimantadine for the control of influenza in a highly vaccinated long-term care population. J Am Med Dir Assoc 2005; 6:359–66. [DOI] [PubMed] [Google Scholar]
- 410.Gorisek Miksic N, Ursic T, Simonovic Z, et al. Oseltamivir prophylaxis in controlling influenza outbreak in nursing homes: a comparison between three different approaches. Infection 2015; 43:73–81. [DOI] [PubMed] [Google Scholar]
- 411.Monto AS, Rotthoff J, Teich E, et al. Detection and control of influenza outbreaks in well-vaccinated nursing home populations. Clin Infect Dis 2004; 39:459–64. [DOI] [PubMed] [Google Scholar]
- 412.Rainwater-Lovett K, Chun K, Lessler J. Influenza outbreak control practices and the effectiveness of interventions in long-term care facilities: a systematic review. Influenza Other Respir Viruses 2014; 8:74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Cheng HY, Chen WC, Chou YJ, Huang AS, Huang WT. Containing influenza outbreaks with antiviral use in long-term care facilities in Taiwan, 2008–2014. Influenza Other Respir Viruses 2018; 12:287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Gupta RK, Zhao H, Cooke M, et al. Public health responses to influenza in care homes: a questionnaire-based study of local health protection units. J Public Health (Oxf) 2007; 29:88–90. [DOI] [PubMed] [Google Scholar]
- 415.Utsumi M, Makimoto K, Quroshi N, Ashida N. Types of infectious outbreaks and their impact in elderly care facilities: a review of the literature. Age Ageing 2010; 39:299–305. [DOI] [PubMed] [Google Scholar]
- 416.Vaux S, Poujol I, Bonmarin I, Levy-Bruhl D, Desenclos JC. Surveillance of lower respiratory tract infections outbreaks in nursing homes in France. Eur J Epidemiol 2009; 24:149–55. [DOI] [PubMed] [Google Scholar]
- 417.Pagani L, Thomas Y, Huttner B, et al. Transmission and effect of multiple clusters of seasonal influenza in a Swiss geriatric hospital. J Am Geriatr Soc 2015; 63:739–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Taylor G, Mitchell R, McGeer A, et al. Healthcare-associated influenza in Canadian hospitals from 2006 to 2012. Infect Control Hosp Epidemiol 2014; 35:169–75. [DOI] [PubMed] [Google Scholar]
- 419.Sayers G, Igoe D, Carr M, et al. High morbidity and mortality associated with an outbreak of influenza A(H3N2) in a psycho-geriatric facility. Epidemiol Infect 2013; 141:357–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Naumova EN, Parisi SM, Castronovo D, Pandita M, Wenger J, Minihan P. Pneumonia and influenza hospitalizations in elderly people with dementia. J Am Geriatr Soc 2009; 57:2192–9. [DOI] [PubMed] [Google Scholar]
- 421.Chemaly RF, Shah DP, Boeckh MJ. Management of respiratory viral infections in hematopoietic cell transplant recipients and patients with hematologic malignancies. Clin Infect Dis 2014; 59(Suppl 5):S344–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Chan MC, Lee N, Ngai KL, et al. A “pre-seasonal” hospital outbreak of influenza pneumonia caused by the drift variant A/Victoria/361/2011-like H3N2 viruses, Hong Kong, 2011. J Clin Virol 2013; 56:219–25. [DOI] [PubMed] [Google Scholar]
- 423.McGeer AJ, Lee W, Loeb M, et al. Adverse effects of amantadine and oseltamivir used during respiratory outbreaks in a center for developmentally disabled adults. Infect Control Hosp Epidemiol 2004; 25:955–61. [DOI] [PubMed] [Google Scholar]
- 424.Lemaitre M, Meret T, Rothan-Tondeur M, et al. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc 2009; 57:1580–6. [DOI] [PubMed] [Google Scholar]
- 425.Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ 2006; 333:1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Pop-Vicas A, Rahman M, Gozalo PL, Gravenstein S, Mor V. Estimating the effect of influenza vaccination on nursing home residents’ morbidity and mortality. J Am Geriatr Soc 2015; 63:1798–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Patriarca PA, Weber JA, Parker RA, et al. Risk factors for outbreaks of influenza in nursing homes. A case-control study. Am J Epidemiol 1986; 124:114–9. [DOI] [PubMed] [Google Scholar]
- 428.Arden N, Monto AS, Ohmit SE. Vaccine use and the risk of outbreaks in a sample of nursing homes during an influenza epidemic. Am J Public Health 1995; 85:399–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Stevenson CG, McArthur MA, Naus M, Abraham E, McGeer AJ. Prevention of influenza and pneumococcal pneumonia in Canadian long-term care facilities: how are we doing? CMAJ 2001; 164:1413–9. [PMC free article] [PubMed] [Google Scholar]
- 430.Drinka PJ, Krause PF, Nest LJ, Goodman BM, Gravenstein S. Risk of acquiring influenza B in a nursing home from a culture-positive roommate. J Am Geriatr Soc 2005; 53:1437. [DOI] [PubMed] [Google Scholar]
- 431.Gooskens J, Swaan CM, Claas EC, Kroes AC. Rapid molecular detection of influenza outbreaks in nursing homes. J Clin Virol 2008; 41:7–12. [DOI] [PubMed] [Google Scholar]
- 432.Eibach D, Casalegno JS, Bouscambert M, et al. Routes of transmission during a nosocomial influenza A(H3N2) outbreak among geriatric patients and healthcare workers. J Hosp Infect 2014; 86:188–93. [DOI] [PubMed] [Google Scholar]
- 433.Andrieu AG, Paute J, Glomot L, Jarlier V, Belmin J. Nosocomial influenza out-break in a geriatrics department: effectiveness of preventive measures. Presse Med 2006; 35:1419–26. [DOI] [PubMed] [Google Scholar]
- 434.Khandaker G, Rashid H, Zurynski Y, et al. Nosocomial vs community-acquired pandemic influenza A (H1N1) 2009: a nested case-control study. J Hosp Infect 2012; 82:94–100. [DOI] [PubMed] [Google Scholar]
- 435.van den Dool C, Hak E, Wallinga J, van Loon AM, Lammers JW, Bonten MJ. Symptoms of influenza virus infection in hospitalized patients. Infect Control Hosp Epidemiol 2008; 29:314–9. [DOI] [PubMed] [Google Scholar]
- 436.Michiels B, Van Puyenbroeck K, Verhoeven V, Vermeire E, Coenen S. The value of neuraminidase inhibitors for the prevention and treatment of seasonal influenza: a systematic review of systematic reviews. PLoS One 2013; 8:e60348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Shijubo N, Yamada G, Takahashi M, Tokunoh T, Suzuki T, Abe S. Experience with oseltamivir in the control of nursing home influenza A outbreak. Intern Med 2002; 41:366–70. [DOI] [PubMed] [Google Scholar]
- 438.Buchbinder N, Dumesnil C, Pinquier D, et al. Pandemic A/H1N1/2009 influenza in a paediatric haematology and oncology unit: successful management of a sudden outbreak. J Hosp Infect 2011; 79:155–60. [DOI] [PubMed] [Google Scholar]
- 439.Ambrozaitis A, Gravenstein S, van Essen GA, et al. Inhaled zanamivir versus placebo for the prevention of influenza outbreaks in an unvaccinated long-term care population. J Am Med Dir Assoc 2005; 6:367–74. [DOI] [PubMed] [Google Scholar]
- 440.van der Sande MA, Meijer A, Sen-Kerpiclik F, et al. Effectiveness of post-exposition prophylaxis with oseltamivir in nursing homes: a randomised controlled trial over four seasons. Emerg Themes Epidemiol 2014; 11:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Peters PH Jr, Gravenstein S, Norwood P, et al. Long-term use of oseltamivir for the prophylaxis of influenza in a vaccinated frail older population. J Am Geriatr Soc 2001; 49:1025–31. [DOI] [PubMed] [Google Scholar]
- 442.Bowles SK, Lee W, Simor AE, et al. Use of oseltamivir during influenza outbreaks in Ontario nursing homes, 1999–2000. J Am Geriatr Soc 2002; 50:608–16. [DOI] [PubMed] [Google Scholar]
- 443.Ye M, Jacobs A, Khan MN, et al. Evaluation of the use of oseltamivir prophylaxis in the control of influenza outbreaks in long-term care facilities in Alberta, Canada: a retrospective provincial database analysis. BMJ Open 2016; 6:e011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Merritt T, Hope K, Butler M, et al. Effect of antiviral prophylaxis on influenza outbreaks in aged care facilities in three local health districts in New South Wales, Australia, 2014. Western Pac Surveill Response J 2016; 7:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Tsagris V, Nika A, Kyriakou D, et al. Influenza A/H1N1/2009 outbreak in a neonatal intensive care unit. J Hosp Infect 2012; 81:36–40. [DOI] [PubMed] [Google Scholar]
- 446.Pannaraj PS, Tam B, Akan D. Oseltamivir treatment and prophylaxis in a neonatal intensive care unit during a 2009 H1N1 influenza outbreak. J Perinatol 2011; 31:487–93. [DOI] [PubMed] [Google Scholar]
- 447.Shinjoh M, Takano Y, Takahashi T, Hasegawa N, Iwata S, Sugaya N. Postexposure prophylaxis for influenza in pediatric wards oseltamivir or zanamivir after rapid antigen detection. Pediatr Infect Dis J 2012; 31:1119–23. [DOI] [PubMed] [Google Scholar]
- 448.Higa F, Tateyama M, Tomishima M, et al. Role of neuraminidase inhibitor chemoprophylaxis in controlling nosocomial influenza: an observational study. Influenza Other Respir Viruses 2012; 6:299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Chen LF, Dailey NJ, Rao AK, et al. Cluster of oseltamivir-resistant 2009 pandemic influenza A (H1N1) virus infections on a hospital ward among immunocompromised patients—North Carolina, 2009. J Infect Dis 2011; 203:838–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.van der Sande MA, Ruijs WL, Meijer A, Cools HJ, van der Plas SM. Use of oseltamivir in Dutch nursing homes during the 2004–2005 influenza season. Vaccine 2006; 24:6664–9. [DOI] [PubMed] [Google Scholar]
- 451.Chang YM, Li WC, Huang CT, et al. Use of oseltamivir during an outbreak of influenza A in a long-term care facility in Taiwan. J Hosp Infect 2008; 68:83–7. [DOI] [PubMed] [Google Scholar]
- 452.Bush KA, McAnulty J, McPhie K, et al. ; Southern New South Wales Public Health Unit. Antiviral prophylaxis in the management of an influenza outbreak in an aged care facility. Commun Dis Intell Q Rep 2004; 28:396–400. [DOI] [PubMed] [Google Scholar]
- 453.Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recomm Rep 2018; 67:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Drinka PJ, Gravenstein S, Schilling M, Krause P, Miller BA, Shult P. Duration of antiviral prophylaxis during nursing home outbreaks of influenza A: a comparison of 2 protocols. Arch Intern Med 1998; 158:2155–9. [DOI] [PubMed] [Google Scholar]
- 455.Vink MA, Bootsma MC, Wallinga J. Serial intervals of respiratory infectious diseases: a systematic review and analysis. Am J Epidemiol 2014; 180:865–75. [DOI] [PubMed] [Google Scholar]
- 456.France AM, Jackson M, Schrag S, et al. Household transmission of 2009 influenza A (H1N1) virus after a school-based outbreak in New York City, April-May 2009. J Infect Dis 2010; 201:984–92. [DOI] [PubMed] [Google Scholar]
- 457.Ling LM, Chow AL, Lye DC, et al. Effects of early oseltamivir therapy on viral shedding in 2009 pandemic influenza A (H1N1) virus infection. Clin Infect Dis 2010; 50:963–9. [DOI] [PubMed] [Google Scholar]
- 458.Centers for Disease Control and Prevention. Influenza antiviral medications: summary for clinicians. Available at: https://www.cdc.gov/flu/professionals/anti-virals/summary-clinicians.htm. Accessed 8 November 2018.
- 459.Hayden FG, Sugaya N, Hirotsu N, et al. ; Baloxavir Marboxil Investigators Group. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med 2018; 379:913–23. [DOI] [PubMed] [Google Scholar]
- 460.Ison MG, Portsmouth S, Yoshida Y, et al. Phase 3 trial of baloxavir marboxil in high risk influenza patients (CAPSTONE-2 Study) Late breaker Abstract LB16. Presented on October 6, 2018 at ID Week 2018, San Francisco, CA: Open Forum Infectious Diseases, ofy209. Available at: https://academic.oup.com/ofid/advance-article/doi/10.1093/ofid/ofy209/5106888. Accessed 8 November 2018. [Google Scholar]


