Abstract
Background
Studies have suggested that women are biologically different and that female gender itself is independently associated with poor clinical outcome after an acute myocardial infarction (AMI).
Hypothesis
We analyzed data from the Korean Acute Myocardial Infarction Registry (KAMIR) to assess gender differences in in‐hospital outcomes post ST‐segment elevation myocardial infarction (STEMI).
Methods
Between November 2005 and July 2007, 4037 patients who were admitted with STEMI to 41 facilities were registered into the KAMIR database; patients admitted within 72 hours of symptom onset were selected and included in this study.
Results
The proportion of patients who had reperfusion therapy within 12 hours from chest pain onset was lower in women. Women had higher rates of in‐hospital mortality (8.6% vs 3.2%, P < .01), noncardiac death (1.5% vs 0.4%, P < .01), cardiac death (7.1% vs 2.8%, P < .01), and stroke (1.2% vs 0.5%, P < .05) than men. Multivariate logistic regression analysis identified age, previous angina, hypertension, a Killip class ≥ II, a left ventricular ejection fraction (LVEF) < 40%, and a thrombolysis in myocardial infarction flow (TIMI) grade ≤ 3 after angioplasty as independent risk factors for in‐hospital death for all patients; however, female gender itself was not an independent risk factor.
Conclusions
The results of this study show that although women have a higher in‐hospital mortality than men, female gender itself is not an independent risk factor for in‐hospital mortality. Copyright © 2010 Wiley Periodicals, Inc.
Introduction
Ischemic heart disease is the leading cause of death worldwide. The prevalence of coronary artery disease is increasing and becoming a major cause of morbidity and mortality in Korea.1 Acute myocardial infarction (AMI) continues to be a major public health problem in the industrialized world. Recently, the Korean Acute Myocardial Infarction Registry (KAMIR) study, a nationwide, multicenter study, was initiated to analyze the clinical characteristics of AMI in the Korean population. The current study was designed, based on data obtained from the KAMIR study, to elucidate gender differences among Korean AMI patients.
A gender gap has been suggested to be present in coronary artery disease severity, percutaneous coronary intervention (PCI) outcomes, and short‐term mortality among patients with acute myocardial infarction (AMI).2, 3, 4, 5 One of the contributing factors to poorer outcomes in women is that women receive reperfusion therapy less often than men, which results in a higher incidence of severe myocardial necrosis.6, 7 In addition, women have other risk factors that contribute to a poorer outcome.6, 7, 8 However, some studies have shown similar outcomes between genders after adjustment for other risk factors. One report suggested that the overall mortality is not different between genders, but that the timing and mechanism underlying AMI are different.9
The purpose of the present study was to determine and compare in‐hospital outcomes after ST‐segment elevation myocardial infarction (STEMI) and independent predictors of these outcomes in women and men.
Methods
This study is based on a database collected by the KAMIR National Registry Study. KAMIR is a prospective, multicenter registry study designed to characterize the clinical features and prognosis of AMI in Korean patients. All 41 cardiology centers in Korea were invited to participate in the KAMIR study. At participating sites, consecutive patients admitted with AMI were asked to register to be part of this study. Patients at all centers were eligible for thrombolytic therapy, and PCI was available for all acute STEMI patients. All treatment strategies including reperfusion therapy modality and medications were chosen at the discretion of the attending physicians.
Patients
From November 2005 to July 2007, 4037 consecutive patients were admitted to 41 cardiovascular facilities due to an acute STEMI within 72 hours after symptom onset. All patients were divided into 2 groups according to gender and were compared with regard to baseline clinical characteristics, angiographic findings, treatment modalities, and in‐hospital outcomes. Among these patients, 1083 (27%) were women and 2954 (73%) were men.
The study protocol has been reviewed and approved by the institutional review boards of the participating centers.
Data Registry
Detailed data were obtained on patients' demographics, treatment in the emergency room, catheterization findings, and clinical outcome during their hospital stay. Data was collected at each institution; a study coordinator or doctor entered the data into a password‐protected, web‐based, computerized database program provided by the KAMIR committee. Data coordinators attended meetings at least twice yearly for education; in addition, they reviewed and discussed the study protocol.
Definitions
ST‐segment elevation myocardial infarction was diagnosed by a cardiologist in a patient with ≥ 2 of the following criteria: (1) typical chest pain lasting > 30 minutes; (2) development of pathological Q waves or ST‐segment and T‐wave changes in more than 2 ECG leads; and (3) the typical increase and decrease of serum creatinine kinase levels 2× the upper limit of normal. Hypertension was defined as known hypertension or blood pressure (BP) ≥ 140/90 mm Hg based on the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure VII guidelines.10 The diagnosis of diabetes mellitus was based on fasting plasma glucose levels ≥ 126 mg per dL (7.0 mmol per L) or 2‐hour postprandial plasma glucose (2 hr PPG) readings ≥ 200 mg per dL (11.1 mmol per L). Metabolic syndrome was defined according to the Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)11 since, cut off values for the definition of obesity in Asian populations have been revised and criteria for metabolic syndrome modified.12 Metabolic syndrome was diagnosed if 3 or more of the following criteria were satisfied: (1) obesity, defined by a abdominal circumference > 90 cm in men or > 80 cm in women; (2) hypertriglyceridemia if the triglyceride level was ≥ 150 mg/dL; (3) low high‐density lipoprotein cholesterol < 40 mg/dL in men or < 50 mg/dL in women; (4) hypertension, defined as known hypertension or a BP ≥ 130/85 mm Hg;, and (5) dysglycemia, defined as known diabetes or a fasting plasma glucose ≥ 110 mg/dL. Dyslipidemia was defined as a fasting total cholesterol concentration of ≥ 200 mg/dL, a fasting triglyceride concentration of ≥ 200 mg/dL, or the use of treatment with medication for dyslipidemia.
In‐hospital mortality included death from any cause, cardiac and noncardiac, that occurred before discharge. Cardiogenic shock was defined as a systolic blood pressure < 90 mm Hg for at least 10 minutes with evidence of poor tissue perfusion. Cardiac death was defined as mortality directly related to: (1) cardiogenic shock or congestive heart failure; (2) mechanical complications such as free wall and ventricular septal wall rupture; and (3) sudden arrhythmic death. Noncardiac deaths, such as sepsis and pneumonia, were included in the in‐hospital deaths.
Statistical Analysis
Data were expressed as proportions or mean value ± SD. Differences in categorical variables between the 2 groups were analyzed by the χ2 test and differences in continuous variables were analyzed by the 2‐tailed unpaired t test. Multivariate logistic regression analysis was used to determine independent predictors of in‐hospital mortality. Statistical significance was defined as a P value of <.05. Data were analyzed with the use of SPSS 12.0 for Windows software (SPSS Inc., Chicago, IL).
Results
Baseline Characteristics
Differences in demographics, medical history, clinical characteristics, and reperfusion therapy are shown in Table 1. Women were significantly older than the men at the time of their AMI (72 ± 10 vs 61 ± 13 years, P < .001); more than half of the women patients were older than 70. In addition, women were more likely to have metabolic syndrome, previous angina, stroke, hypertension, diabetes, and dyslipidemia. Among men, there was a higher percentage of smokers and had higher peak creatinine kinase‐MB levels. Because of the AMI, women were significantly more likely to have a higher incidence of a Killip class ≥ II and cardiogenic shock on admission.
Table 1.
Patient Baseline Characteristics
| Women (n = 1083) | Men (n = 2954) | P Value | |
|---|---|---|---|
| Age, years | 72.1 ± 9.7 | 60.7 ± 12.5 | <.001 |
| BMI, kg/m2 | 23.5 ± 3.6 | 24.1 ± 3.1 | <.001 |
| Metabolic syndrome | 751 (69.3%) | 1332 (45.1%) | <.001 |
| Previous angina | 70 (6.5%) | 126 (4.3%) | .004 |
| Previous MI | 31 (2.9%) | 107 (3.6%) | .239 |
| Previous CABG | 3 (0.3%) | 15 (0.5%) | .330 |
| Previous PCI | 30 (2.8%) | 128 (4.3%) | .023 |
| Stroke | 80 (7.4%) | 159 (5.4%) | .017 |
| Diabetes | 333 (31.4%) | 667 (23.1%) | <.001 |
| Hypertension | 640 (59.7%) | 1168 (40.2%) | <.001 |
| Smoking | 159 (14.7%) | 1738 (58.8%) | <.001 |
| Dyslipidemia | 560 (51.7%) | 1306 (44.2%) | <.001 |
| MI location | |||
| Anterior | 549 (53.6%) | 1528 (54.4%) | .911 |
| Inferior | 425 (41.5%) | 1143 (40.7%) | |
| Lateral | 36 (3.5%) | 105 (3.7%) | |
| Posterior | 14 (1.4%) | 33 (1.2%) | |
| Peak CK‐MB, ng/mL | 1485 ± 1671 | 2022 ± 2435 | <.001 |
| Killip class ≥ II on admission | 361 (34.7%) | 661 (23.2%) | <.001 |
| Cardiogenic shock on admission | 92 (8.5%) | 144 (4.9%) | <.001 |
| IABP | 63 (5.8%) | 127 (4.3%) | .044 |
| LVEF, % | 49.77 ± 12.518 | 50.37 ± 11.923 | .192 |
Abbreviations: BMI = body mass index; CABG = coronary artery bypass graft surgery; IABP = intra‐aortic balloon pump; LVEF = left ventricular ejection fraction; MI = myocardial infarction; PCI = percutaneous coronary intervention
Revascularization Time and Methods
The percentages of patients who visited the emergency room within 12 hours after chest pain onset or who were treated by reperfusion therapy within 12 hours of symptom onset were higher among men than among women. During their admission, reperfusion or revascularization therapy was performed in 86.3% of women and 90.9% of men (P < .001). Men received thrombolytic therapy more frequently than women did. There was no significant difference in the frequencies of primary PCI between women and men (Table 2). There were no significant differences in the proportions of use of medical treatment with glycoprotein IIb/IIIa inhibitors, aspirin, clopidogrel, β‐blockers, and angiotensin‐converting enzyme inhibitors.
Table 2.
Revascularization Time and Methods
| Women (n = 1083) | Men (n = 2954) | P Value | |
|---|---|---|---|
| Chest pain to ER visit < 12 hrs | 822 (75.9%) | 2404 (81.4%) | <.001 |
| Door to needle time, min | 86.51 ± 90.06 | 74.80 ± 73.59 | .230 |
| Door to balloon time, min | 177.29 ± 336.31 | 207.55 ± 652.548 | .143 |
| Chest pain to reperfusion Tx < 12 hrs | 597 (55.1%) | 1866 (63.2%) | <.001 |
| Any reperfusion Tx before discharge | 935 (86.3%) | 2685 (90.9%) | <.001 |
| Thrombolytic Tx | 108 (10.1%) | 404 (13.9%) | .002 |
| PCI (%) | |||
| Primary PCI | 661 (61.0%) | 1873 (63.4%) | .167 |
| Rescue PCI after thrombolysis | 38 (3.5%) | 113 (3.8%) | .639 |
| Rescue PCI after conservative Tx | 31 (2.9%) | 76 (2.6%) | .612 |
| Delayed PCI | 165 (15.2%) | 505 (17.1 %) | .159 |
| CABG | 20 (1.9%) | 38 (1.3%) | .192 |
Abbreviations: CABG = coronary artery bypass graft surgery; ER = emergency room; PCI = percutaneous coronary intervention; Tx = therapy
Figure 1.
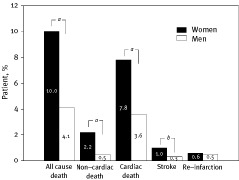
The rates of in‐hospital cardiovascular events in women and men. a P < .001 compared with the men. b P < .05 compared with the men
Coronary Angiographic Findings
The extent of coronary artery stenosis was more severe in men than in women. The most common infarct‐related artery was the left anterior descending coronary artery and there was no difference in its distribution between women and men. After coronary intervention, a thrombolysis in myocardial infarction flow (TIMI) of grade 3 was achieved in 89.4% of women and 93.0% of men (P = .001; Table 3).
Table 3.
Coronary Angiographic Findings
| Women (n = 895) | Men (n = 2567) | P Value | |
|---|---|---|---|
| Number of diseased vessels | |||
| LMT, complex | 12 (1.5) | 40 (1.6%) | .004 |
| LMT, isolated | 4 (0.5) | 9 (0.4%) | |
| 1 | 370 (41.9) | 1230 (48.5%) | |
| 2 | 278 (31.4) | 759 (29.9%) | |
| 3 | 219 (24.8) | 497 (19.6%) | |
| Infarct‐related artery | |||
| LAD | 458 (51.8%) | 1319 (52.0%) | .281 |
| LCX | 75 (8.5%) | 258 (10.2%) | |
| RCA | 345 (39.0%) | 930 (36.7%) | |
| LMT | 7 (0.8%) | 30 (1.2%) | |
| TIMI flow grade 0 at initial angiography | 478 (53.4%) | 1324 (51.6%) | .345 |
| Final TIMI flow grade 3 | 776 (89.4%) | 2299 (93.0%) | .001 |
Abbreviations: LAD = left anterior descending coronary artery; LCX = left circumflex artery; LMT = left main trunk; LMT complex = coronary artery stenosis on left main trunk and other major coronary arteries; RCA = right coronary artery; TIMI = thrombolysis in acute myocardial infarction
In‐Hospital Outcomes
All in‐hospital cardiovascular events are summarized in the Figure. During hospitalization, 189 deaths (4.7%) were recorded. The overall mortality rate during hospitalization was 8.6% in women and 3.2% in men (P < .001). The frequencies of both cardiac and noncardiac deaths were higher in women than in men (P < .001). There were similar frequencies of reinfarction during hospitalization in both men and women. However, a higher proportion of women patients had a stroke during hospitalization (1.2% vs 0.5%, P = .012).
Predictors of In‐hospital Death
Multivariate stepwise logistic regression models identified the predictors of in‐hospital death. Among all patients, age, previous angina, hypertension, a Killip class ≥ II, and left ventricular ejection fraction (LVEF) < 40% were identified as independent risk factors. A TIMI flow of grade 3 after coronary intervention was a negative predictor (Table 4).
Table 4.
Independent Predictors of In‐hospital Death in All Patients
| Variable | OR (95% CI) | P Value |
|---|---|---|
| Age | 1.06 (1.027–1.094) | <.001 |
| Sex, female | 1.36 (0.690–2.660) | .378 |
| Metabolic syndrome | 0.99 (0.507–1.935) | .978 |
| Previous angina | 2.57 (1.067–6.186) | .035 |
| Stroke | 1.04 (0.378–2.840) | .946 |
| Smoking | 0.82 (0.402–1.688) | .596 |
| Hypertension | 1.96 (1.016–3.792) | .045 |
| Diabetes mellitus | 1.41 (0.767–2.609) | .267 |
| Dyslipidemia | 0.68 (0.373–1.244) | .211 |
| Killip class ≥II | 3.22 (1.779–5.828) | <.001 |
| Anterior wall MI | 1.03 (0.557–1.893) | .932 |
| LVEF < 40% | 3.95 (2.133–7.309) | <.001 |
| Reperfusion therapy < 12 hr | 0.42 (0.169–1.055) | .065 |
| TIMI flow grade 3 after PCI | 0.32 (0.160–0.649) | .002 |
Abbreviations: CI = confidence interval; LVEF = left ventricular ejection fraction; MI = myocardial infarction; OR = odds ratio; PCI = percutaneous coronary intervention; TIMI = thrombolysis in myocardial infarction
Discussion
The outcome of AMI in men and women has been the object of debate in numerous studies. In this study, we found different clinical features and higher in‐hospital mortality in women compared to men after an AMI. However, after adjustment for confounding factors, female gender was not an independent predictor of in‐hospital mortality.
The physiological concentration of female sex hormones is thought to slow the progression of atherosclerosis.13 Therefore, gender differences in ischemic heart disease are not appreciated until after the age of 70 in women; this suggests that the antiatherogenic effects associated with female gender decrease and disappear by about 20 years after menopause.14 Consistent with the findings of other studies, the most striking difference between genders in this study, with regard to the clinical risk profile, was age; women were older by an average of 11 years.15,16 Therefore, women had a higher incidence of age‐associated risk factors such as diabetes and hypertension. Advanced age in women is commonly associated with many comorbidities in addition to diabetes and hypertension. Thus, for women there was limited use of thrombolytic therapy and invasive procedures.17
A number of studies have suggested gender differences in morbidity and mortality following an acute myocardial infarction.5,8 Although there are a few studies that did not find a gender difference in clinical outcomes,16,18 some studies have attributed the gender differences in outcome to less aggressive treatment of women compared to men.8 In this study, we found significant gender differences in the incidence of cardiac and noncardiac in‐hospital mortality. Explanations for why the female gender was associated with a poorer prognosis are needed. The frequency of hospital visits within the time frame eligible for reperfusion therapy (<12 h after the onset of chest pain) was higher in men than in women. In addition, women tended to present with more serious angiographic and clinical findings, such as cardiogenic shock and a Killip class ≥ II than did men. The percentages of men with early reperfusion or late revascularization therapy were higher than those in women. The thrombolytic therapy in men accounted for most of this difference. Older patients report chest pain more commonly with atypical symptoms such as nausea, vomiting, dyspnea, and abdominal symptoms.19, 20, 21 These atypical symptoms may delay a hospital visit in women having an MI and also delay reperfusion therapy. This may cause the resulting gender disparity in hospital arrival time and early treatment. In addition, treatment with proven cardioprotective drugs such as aspirin, heparin, and β‐blockers is less common in women.22 Furthermore, thrombolytic therapy, percutaneous transluminal coronary angioplasty, and coronary artery bypass surgery are performed less often in women.22
Does female gender itself increase mortality after an AMI? From the multivariate logistic regression analysis, age, previous angina, hypertension, a Killip class ≥ II, an LVEF < 40%, and a TIMI flow ≤ grade 3 after angioplasty were identified as independent risk factors for in‐hospital death; however, female gender itself was not an independent risk factor. These findings are explained by the observation that highly significant prognostic factors such as Killip class, left ventricular function, and TIMI flow of grade 3 after angioplasty were worse in women than in men.
Taken together the results of this study showed that women with an acute STEMI had different risk factors and a higher in‐hospital mortality than men. However, female gender itself was not an independent risk factor for in‐hospital mortality. Further study is needed to determine the reasons for these gender differences and to develop management protocols to improve patient outcomes.
Participating investigators for the Korean Acute Myocardial Infarction Registry (KAMIR) Study Group: Young Jo Kim MD, Myung Ho Jeong MD, Chong Jin Kim MD, Myeong Chan Cho MD, Young Keun Ahn MD, Jong Hyun Kim MD, Shung Chull Chae MD, Seung Ho Hur MD, In Whan Seong MD, Taek Jong Hong MD, Dong Hoon Choi MD, Jei Keon Chae MD, Jae Young Rhew MD, Doo Il Kim MD, In Ho Chae MD, Jung Han Yoon MD, Bon Kwon Koo MD, Byung Ok Kim MD, Myoung Yong Lee MD, Kee Sik Kim MD, Jin Yong Hwang MD, Seok Kyu Oh MD, Nae Hee Lee MD, Kyoung Tae Jeong MD, Seung Jea Tahk MD, Jang Ho Bae MD, Seung Woon Rha MD, Keum Soo Park MD, Kyoo Rok Han MD, Tae Hoon Ahn MD, Moo Hyun Kim MD, Ju Young Yang MD, Chong Yun Rhim MD, Hyeon Cheol Gwon MD, Seong Wook Park MD, Young Youp Koh MD, Seung Jae Joo MD, Soo Joong Kim MD, Dong Kyu Jin MD, Jin Man Cho MD, Jeong Gwan Cho MD, Wook Sung Chung MD, Yang Soo Jang MD, Ki Bae Seung MD, and Seung Jung Park MD.
References
- 1. Hong JS, Kang HC, Lee SH, Kim J. Long‐term trend in the incidence of acute myocardial infarction in Korea: 1997–2007. Korean Circ J. 2009; 39(11): 467–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Presbitero P, Carcagni A. Gender differences in the outcome of interventional cardiac procedures. Ital Heart J 2003; 4(8): 522–527. [PubMed] [Google Scholar]
- 3. Oe K, Shimizu M, Ino H, et al. Effects of gender on the number of diseased vessels and clinical outcome in Japanese patients with acute coronary syndrome. Circ J 2002; 66(5): 435–440. [DOI] [PubMed] [Google Scholar]
- 4. Cheng CI, Yeh KH, Chang HW, et al. Comparison of baseline characteristics, clinical features, angiographic results, and early outcomes in men vs women with acute myocardial infarction undergoing primary coronary intervention. Chest 2004; 126(1): 47–53. [DOI] [PubMed] [Google Scholar]
- 5. Zubaid M, Rashed WA, Thalib L, Suresh CG. Differences in thrombolytic treatment and in‐hospital mortality between women and men after acute myocardial infarction. Jpn Heart J 2001; 42(6): 669–676. [DOI] [PubMed] [Google Scholar]
- 6. Kanamasa K, Ishikawa K, Hayashi T, et al. Increased cardiac mortality in women compared with men in patients with acute myocardial infarction. Intern Med 2004; 43(10): 911–918. [DOI] [PubMed] [Google Scholar]
- 7. Hollenbeak CS, Weisman CS, Rossi M, Ettinger SM. Gender disparities in percutaneous coronary interventions for acute myocardial infarction in Pennsylvania. Med Care 2006; 44(1): 24–30. [DOI] [PubMed] [Google Scholar]
- 8. Heer T, Schiele R, Schneider S, et al. Gender differences in acute myocardial infarction in the era of reperfusion (the MITRA registry). Am J Cardiol 2002; 89(5): 511–517. [DOI] [PubMed] [Google Scholar]
- 9. Andreotti F, Conti E, Lanza GA, Crea F. Sex, survival bias, and mortality following acute myocardial infarction. Ital Heart J 2003; 4(8): 508–510. [PubMed] [Google Scholar]
- 10. Mancia G, Grassi G, Joint National Committee VII and European Society of Hypertension/European Society of Cardiology guidelines for evaluating and treating hypertension: a two‐way road? J Am Soc Nephrol 2005; 16(suppl 1): S74–77. [DOI] [PubMed] [Google Scholar]
- 11. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106(25): 3143–3421. [PubMed] [Google Scholar]
- 12. Ko GT, Cockram CS, Chow CC, et al. High prevalence of metabolic syndrome in Hong Kong Chinese—comparison of three diagnostic criteria. Diabetes Res Clin Pract 2005; 69(2): 160–168. [DOI] [PubMed] [Google Scholar]
- 13. Hayashi T, Jayachandran M, Sumi D, et al. Physiological concentration of 17beta‐estradiol retards the progression of severe atherosclerosis induced by a high‐cholesterol diet plus balloon catheter injury: role of NO. Arterioscler Thromb Vasc Biol 2000; 20(6): 1613–1621. [DOI] [PubMed] [Google Scholar]
- 14. Gorodeski GI. Impact of the menopause on the epidemiology and risk factors of coronary artery heart disease in women. Exp Gerontol 1994; 29(3–4): 357–375. [DOI] [PubMed] [Google Scholar]
- 15. Stone GW, Grines CL, Browne KF, et al. Comparison of in‐hospital outcome in men versus women treated by either thrombolytic therapy or primary coronary angioplasty for acute myocardial infarction. Am J Cardiol 1995; 75(15): 987–992. [DOI] [PubMed] [Google Scholar]
- 16. Kosuge M, Kimura K, Kojima S, et al. Sex differences in early mortality of patients undergoing primary stenting for acute myocardial infarction. Circ J 2006; 70(3): 217–221. [DOI] [PubMed] [Google Scholar]
- 17. Grazia Modena M. Acute myocardial infarction—are women different? Int J Clin Pract 2005; 59(1): 2–5. [DOI] [PubMed] [Google Scholar]
- 18. Heer T, Gitt AK, Juenger C, et al. Gender differences in acute non‐ST‐segment elevation myocardial infarction. Am J Cardiol 2006; 98(2): 160–166. [DOI] [PubMed] [Google Scholar]
- 19. Herlitz J, Bang A, Karlson BW, Hartford M. Is there a gender difference in aetiology of chest pain and symptoms associated with acute myocardial infarction? Eur J Emerg Med 1999; 6(4): 311–315. [DOI] [PubMed] [Google Scholar]
- 20. Goldberg R, Goff D, Cooper L, et al. Age and sex differences in presentation of symptoms among patients with acute coronary disease: the REACT Trial. Rapid Early Action for Coronary Treatment. Coron Artery Dis 2000; 11(5): 399–407. [DOI] [PubMed] [Google Scholar]
- 21. Milner KA, Funk M, Richards S, et al. Gender differences in symptom presentation associated with coronary heart disease. Am J Cardiol 1999; 84(4): 396–399. [DOI] [PubMed] [Google Scholar]
- 22. Chandra NC, Ziegelstein RC, Rogers WJ, et al. Observations of the treatment of women in the United States with myocardial infarction: a report from the National Registry of Myocardial Infarction‐I. Arch Intern Med 1998; 158(9): 981–988. [DOI] [PubMed] [Google Scholar]


