Abstract
Background
Stereotactic radiosurgery (SRS) is an established treatment for brain metastases, yet little is known about SRS for neuroendocrine tumors given their unique natural history.
Objective
To determine outcomes and toxicity from SRS in patients with brain metastases arising from neuroendocrine tumors.
Methods
Thirty-three patients with brain metastases from neuroendocrine tumors who underwent SRS were retrospectively reviewed. Median age was 61 years and median Karnofsky performance status was 80. Primary sites were lung (87.9%), cervix (6.1%), esophagus (3%), and prostate (3%). Ten patients (30.3%) received upfront SRS, 7 of whom had neuroendocrine tumors other than small cell lung carcinoma. Kaplan-Meier survival and Cox regression analyses were performed to determine prognostic factors for survival.
Results
With median follow-up after SRS of 5.3 months, local and distant brain recurrence developed in 5 patients (16.7%) and 20 patients (66.7%), respectively. Median overall survival (OS) after SRS was 6.9 months. Patients with progressive disease per Response Assessment in Neuro-Oncology-Brain Metastases (RANO-BM) criteria at 4 to 6 weeks after SRS had shorter median time to developing recurrence at a distant site in the brain and shorter OS than patients without progressive disease: 1.4 months and 3.3 months vs 11.4 months and 12 months, respectively (both P < .001). Toxicity was more likely in lesions of small cell histology than in lesions of other neuroendocrine tumor histology, 15.7% vs 3.3% (P = .021). No cases of grade 3 to 5 necrosis occurred.
Conclusions
SRS is an effective treatment option for patients with brain metastases from neuroendocrine tumors with excellent local control despite slightly higher toxicity rates than expected. Progressive disease at 4 to 6 weeks after SRS portends a poor prognosis.
Keywords: brain metastases, Gamma Knife, neuroendocrine, stereotactic radiosurgery, small cell carcinoma
Neuroendocrine tumors can originate from any organ in the body and present with different clinical features depending on the primary site. Small cell lung carcinoma (SCLC) is recognized as highly aggressive with a poor prognosis,1–3 while extrapulmonary small cell carcinoma and other neuroendocrine tumors are considered different clinical entities due to their relatively lower metastatic potential.4–6
The brain is one of the most common metastatic sites in SCLC.7,8 Prophylactic cranial irradiation (PCI) reduces the incidence of brain metastases and improves survival in SCLC,7–13 but 14% to 43% of patients still develop intracranial tumors.7–10,12 With more frequent and advanced brain imaging as well as effective local and systemic treatments, the incidence of brain metastasis is increasing.14 Possible treatments include surgery, whole brain radiation (WBRT), and stereotactic radiosurgery (SRS). Surgery may not be appropriate in the setting of multiple brain metastases, and some patients cannot receive additional WBRT. Thus, local treatment using highly conformal SRS is an option for these patients, allowing tumor dose escalation for local control while minimizing dose to the normal brain.
Because these tumors have a high propensity for multiple metastases, the utility of focal radiation is debated. It is also unclear if patients with neuroendocrine tumors other than SCLC should be treated with WBRT upfront or if they can be treated with initial SRS without compromising neurological and survival outcomes. Due to the rarity of brain metastasis from neuroendocrine tumors, there are few case reports on SRS treatment in these patients and no specific treatment guidelines have been documented.15–17 Thus, we performed this study to determine treatment outcomes and toxicity from SRS in patients with brain metastases from neuroendocrine tumors.
Materials and Methods
Patient Selection
We retrospectively reviewed 33 patients with brain metastases from neuroendocrine tumors from any primary site consecutively treated with Gamma Knife radiosurgery at our institution between August 2009 and February 2014. All patients underwent contrast-enhanced magnetic resonance imaging (MRI) for the diagnosis and evaluation of brain metastases. Informed consent was waived as this study was approved by the institutional review board as a retrospective study.
Radiosurgical Treatment
A total of 147 lesions were treated with the Leksell Gamma Knife (Perfexion model). MRI was the standard imaging technique for the initial evaluation and treatment planning in every patient. Using a 1.5 T GE Healthcare (Milwaukee, Wisconsin) MRI machine following a stereotactic head frame fixation on the day of SRS, axial postcontrast 3-dimensional fast spoiled gradient echo (3D FSPGR) images (1-mm-slice thickness, no spacing) were obtained. The target volume was defined as the contrast-enhancing lesion without margin. No clinical target volume or planning target volume was used. SRS dose was prescribed according to RTOG 90-05: 20 to 24 Gy for lesions up to 20 mm in diameter, 18 Gy for lesions 21 to 30 mm in diameter, and 15 Gy for lesions 31 to 40 mm in diameter.
SRS was performed as one of the following: 1) salvage treatment in patients who received PCI initially and developed brain metastases (post PCI group); 2) salvage treatment after brain failure in patients who received prior WBRT for brain metastasis (post WBRT group); or 3) initial treatment in patients with limited brain metastasis (upfront SRS group).
Treatment Response Assessment
During the follow-up period, clinical examination and a contrast-enhanced MRI were performed 4 to 6 weeks after SRS treatment and every 2 to 3 months thereafter. Recent criteria proposed by The Response Assessment in Neuro-Oncology Brain Metastases (RANO-BM) working group classifies response as complete response, partial response, stable disease, or progressive disease.18 Patients were evaluated for SRS response using the RANO-BM criteria at first follow-up 4 to 6 weeks after SRS. Criteria for progressive disease included any of the following: at least a 20% increase in the sum of the longest diameters of central nervous system (CNS) target lesions, unequivocal progression of existing enhancing non-target CNS lesions, new lesion(s), unequivocal progression of existing tumor-related non-enhancing (T2/FLAIR) CNS lesions, or worsening clinical status. For cases where imaging changes at 4 to 6 weeks were equivocal, follow-up scans were used to confirm the nature of the changes. If tumor progression was confirmed on subsequent scans, then the date of progression was recorded as the date of the MRI at 4 to 6 weeks after SRS. Local recurrence was defined as a lesion reappearing within 1 cm from the original lesion whereas distant brain recurrence was defined as a metachronous remote metastasis in an area that contained no previous tumor. Toxicities including hemorrhage, necrosis, and edema requiring steroids were evaluated by MRI and clinical follow-up. Necrosis was graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0.
Statistical Analysis
Measures of association in frequency tables were assessed with Fisher’s exact test and the equality of means for continuous variables was assessed using the t test. Survival time was calculated from the date of SRS to the occurrence of the considered event using the Kaplan-Meier method.19 The log-rank test was used to assess the equality of survival across groups. Predictors of survival and distant brain recurrence were assessed using the Cox regression analysis. All factors with a P value of ≤.25 on univariate analysis were included in the multivariate analysis, with each factor eliminated in a step-wise manner until the most significant variables were identified. The Wald test was used to assess the role of covariates in the model. Logistic regression analysis was used to examine the influence of patient, tumor, and other factors on the occurrence of an event. All tests were two-sided and a P value of less than .05 was considered statistically significant. Statistical analyses were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL) and Stata/MP 14.0 (StataCorp, College Station, TX).
Results
Baseline patient and disease characteristics are shown in Table 1. At initial diagnosis, 22 patients presented with metastatic disease: 3 patients had brain metastases only, 14 patients had extracranial metastases only, and 5 patients had brain and extracranial metastases.
Table 1.
Baseline Characteristics Classified by Treatment Group
|
All patients
(N = 33) |
Post-PCI
Group (n = 11) |
Post-WBRT
Group (n = 12) |
Upfront SRS
Group (n = 10) |
P value | |
|---|---|---|---|---|---|
| Age, median (range) | 61 (30–76) y | 65 (53–76) y | 62 (45–75) y | 48 (30–62) y | <.001 |
| KPS, median | 80 (60–90) | 80 (70–90) | 80 (60–90) | 90 (80–90) | .081 |
| Sex | .281 | ||||
| Male | 18 (54.5%) | 4 (36.4%) | 7 (58.3%) | 7 (70%) | |
| Female | 15 (45.5%) | 7 (63.6%) | 5 (41.7%) | 3 (30%) | |
| Race | .051 | ||||
| Caucasian | 25 (75.7%) | 10 (90.9%) | 7 (58.3%) | 8 (80%) | |
| Black | 3 (9.1%) | 0 | 3 (25%) | 0 | |
| Hispanic | 3 (9.1%) | 1 (9.1%) | 0 | 2 (20%) | |
| Asian | 2 (6.1%) | 0 | 2 (16.7%) | 0 | |
| Primary site | .047 | ||||
| Lung | 29 (87.9%) | 11 (100%) | 11 (91.7%) | 7 (70%) | |
| Cervix | 2 (6.1%) | 0 | 0 | 2 (20%) | |
| Esophagus | 1 (3.0%) | 0 | 0 | 1 (10%) | |
| Prostate | 1 (3.0%) | 0 | 1 (8.3%) | 0 | |
| Primary histology | .006 | ||||
| Small cell | 23 (69.7%) | 10 (90.9%) | 10 (83.3%) | 3 (30%) | |
| Other NETs | 10 (30.3%) | 1 (9.1%) | 2 (16.7%) | 7 (70%) | |
| Baseline RPA41 | .164 | ||||
| RPA class I | 13 (39.4%) | 2 (18.2%) | 5 (41.7%) | 6 (60%) | |
| RPA class II | 19 (57.6%) | 9 (81.8%) | 6 (50%) | 4 (40%) | |
| RPA class III | 1 (3.0%) | 0 | 1 (8.3%) | 0 | |
| Baseline DS-GPA42 | .032 | ||||
| 0–1.0 | 4 (12.1%) | 1 (9.1%) | 2 (16.7%) | 1 (10%) | |
| 1.5–2.5 | 23 (69.7%) | 10 (90.9%) | 9 (75%) | 4 (40%) | |
| 3.0 | 2 (6.1%) | 0 | 1 (8.3%) | 1 (10%) | |
| 3.5–4.0 | 4 (12.1%) | 0 | 0 | 4 (40%) | |
| Baseline SIR43 | .312 | ||||
| 4–7 | 25 (75.8%) | 10 (90.9%) | 9 (75%) | 6 (60%) | |
| 8–10 | 8 (24.2%) | 1 (9.1%) | 3 (25%) | 4 (40%) | |
| Active extracranial metastasis at diagnosis of brain metastasis | 11 (33.3%) | 3 (27.3%) | 4 (33.3%) | 4 (40%) | .899 |
| Median number of brain metastatic lesions (range) | 3 (1–24) | 3 (1–8) | 3 (1–24) | 3 (1–10) | .603 |
| Median interval between NET diagnosis and brain metastasis diagnosis, months (range) | 8.2 (0–33.3) | 14.2 (8.2–33.3) | 5.5 (0–17.8) | 6.4 (0–31) | .017 |
Abbreviation: DS-GPA, disease-specific grade prognostic assessment; KPS, Karnofsky performance status; PCI, prophylactic cranial irradiation; NETs, neuroendocrine tumors; RPA, recursive partitioning analysis; SIR, score index for radiosurgery; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy; y, years.
Prior to SRS, 11 patients had PCI to a median dose of 25 Gy in 10 fractions, 12 patients had WBRT to a median dose of 30 Gy in 10 fractions, and 10 patients had no cranial radiation. Of 10 patients in the upfront SRS group, 7 had neuroendocrine tumors other than small cell carcinoma, 1 had small cell carcinoma of the cervix, and 2 had SCLC with an asymptomatic solitary brain metastasis. The median interval between cranial irradiation and SRS was 10 months in the post PCI group and 8.2 months in the post WBRT group.
Prior to SRS, 6 patients underwent surgical resection of their brain metastases due to mass effect. Four of these patients received delayed SRS after experiencing a tumor bed recurrence. The other 2 patients underwent planned SRS after surgery; one of these patients developed a tumor bed recurrence at the time of SRS and one did not. Four of these 6 patients subsequently developed distant brain metastases but not local recurrences.
SRS Treatment
The median prescription dose was 20 Gy (range, 12–24 Gy) in one fraction. All lesions had 100% coverage with a median prescription isodose line of 50% (range, 45%–88%). The median number of brain metastases treated with SRS per patient was 3 (range, 1–24). The mean tumor volume was 1414 mm3 (range, 3–27100 mm3).
Treatment Response and Patterns of Failure
Median follow-up time after SRS was 5.3 months (range, 0.5–52.9 months) for all patients and 16.5 months (range, 9.9–54.9 months) for the 3 patients alive at last follow up. Follow-up with clinical and MRI evaluations was available in 30 patients. For 131 lesions treated in these 30 patients, the local tumor control rate (complete response, partial response and stable disease) was 99.2% at 4 to 6 weeks after SRS. Of 30 evaluable patients, 19 patients had complete response, partial response or stable disease and 11 patients had progressive disease per RANO-BM criteria at 4 to 6 weeks after SRS (Table 2). Of the 11 patients with progressive disease, 1 had local tumor progression and 10 had new distant brain metastasis.
Table 2.
Treatment Response, Pattern of Failure, and Toxicities Classified by Treatment Group
| All (n = 30) | Post-PCI group (n = 10) | Post-WBRT group (n = 10) | Upfront SRS group (n = 10) | P value | |
|---|---|---|---|---|---|
| Patterns of response (RANO-BM) at 4 to 6 weeks after SRS | |||||
| Complete response | 6 (20%) | 1 (10%) | 0 | 5 (50%) | .027 |
| Partial response | 10 (33.3%) | 2 (20%) | 5 (50%) | 3 (30%) | .573 |
| Stable disease | 3 (10%) | 2 (20%) | 1 (10%) | 0 | .492 |
| Progressive disease | 11 (36.7%) | 5 (50%) | 4 (40%) | 2 (20%) | .510 |
| Patterns of failure in long-term follow-up | |||||
| Local recurrence | 5 (16.7%) | 1 (10%) | 1 (10%) | 3 (30%) | .574 |
| Distant brain recurrence | 20 (66.7%) | 6 (60%) | 6 (60%) | 8 (80%) | .649 |
| Leptomeningeal recurrence | 2 (6.7%) | 0 | 0 | 2 (20%) | .310 |
| Toxicity | |||||
| Overall toxicity * | 8 (26.7%) | 3 (30%) | 3 (30%) | 2 (20%) | 1.000 |
| Hemorrhage | 1 (3.3%) | 0 | 1 (10%) | 0 | 1.000 |
| Radiation necrosis | 6 (20%) | 2 (20%) | 2 (20%) | 2 (20%) | 1.000 |
| Symptomatic edema | 5 (16.7%) | 3 (30%) | 2 (20%) | 0 | .321 |
Abbreviation: PCI, prophylactic cranial irradiation; RANO-BM, Response Assessment in Neuro-Oncology Brain Metastases; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy.
*Some patients experienced more than one toxicity.
With longer follow-up, local recurrence developed in 5 patients: 1 in the post-PCI group, 1 in the post-WBRT group, and 3 in the upfront SRS group (Table 2). Median time from SRS to local recurrence was not reached in post-PCI and post-WBRT group and was 20.5 months (range, 1.4–27.1 months) in the upfront SRS group (P = .91).
Twenty patients (66.7%) developed distant brain metastases with a median time of 3.5 months (range, 1–27.1 months); 6 patients in each of the post-PCI (60%) and WBRT groups (60%) and 8 patients (80%) in the upfront SRS group (P = .65), with a median time of 3.1 months (range, 1–24.9 months), 10.7 months (range, 1–12.4 months), and 3.7 months (range, 1.4–38 months), respectively (P = .76). The complete response rate at 4 to 6 weeks was significantly higher in the upfront SRS groups, at 50%, compared with 10% in the post-PCI group and 0% in the post-WBRT group (P = .03). When classified by histological subtype, the complete response rate was significantly higher for patients with neuroendocrine tumors other than small cell carcinoma, at 50%, compared with 5% for patients with small cell carcinoma (P = .01). Treatment response and patterns of failure are shown in Table 2.
Salvage WBRT was delivered to 4 patients: 2 patients who developed numerous distant brain recurrences after PCI and SRS and 2 patients after upfront SRS. Salvage SRS was combined with WBRT in 1 patient in the upfront SRS group who developed limited small-volume distant brain recurrence 7 months after initial SRS. Salvage surgery was performed in 1 patient who had suspected disease progression but surgical pathology revealed treatment effect. No patient had leptomeningeal disease prior to SRS; leptomeningeal disease developed in 2 patients who received upfront SRS at 3.5 months after SRS and was managed with salvage WBRT.
Platinum-based chemotherapy was administered prior to SRS in 30 patients and after SRS in 9 patients. Thirty of 33 patients (90.9%) died by the time of analysis. Ten patients died from progressive neurological disease, 10 patients died from progressive systemic disease, and the remaining 10 patients died from unknown causes.
Toxicities
Overall, toxicity was observed in 8 patients (26.7%), including hemorrhage (3.3%), necrosis (20%), and edema requiring steroids (16.7%). Grade 1 or 2 radiation necrosis occurred in 1 (3.3%) and 5 (16.7%) patients, respectively. There were no cases of grade 3 or higher radiation necrosis. Two patients were asymptomatic but developed incidentally detected intralesional hemorrhage and necrosis on follow-up MRI that spontaneously resolved. Seven patients presented with clinical symptoms including fatigue (n = 3), headache (n = 2), altered mental status (n = 2), and neurological deficits (n = 4), which resolved after steroid administration. No difference in the toxicity rate was found between patients treated with prior radiation therapy compared to the upfront SRS groups. Toxicities observed for the different treatment groups are shown in Table 2.
When toxicity associated with individual lesions was analyzed, patients with small cell tumors experienced more overall toxicity than those with other neuroendocrine tumors: the overall toxicity for small cell lesions was 15.7% vs 3.3% for other neuroendocrine tumors (P = .02), with a trend toward a higher rate of radiation necrosis at 10% versus 1.7% (P = .07).
Considering the development of radiation necrosis after SRS, there was no difference in the baseline patient characteristics between those who experienced radiation necrosis (n = 6) and those who did not (n = 24). However, the tumor volume, prescription dose, and number of Gamma Knife radiosurgery shots were significantly different. The median tumor volume was significantly larger in the patients who experienced radiation necrosis at 5110 mm3 (range, 78–27100 mm3) compared to 339.5 mm3 (range, 3.8–8980 mm3) in the patients who did not. Consequently, lesions that developed radiation necrosis were treated with a lower median prescription dose, 16.5 Gy vs 20 Gy, and with a higher median number of Gamma Knife radiosurgery shots, 18.5 shots vs 3 shots (P < .001 for all).
Survival Outcomes
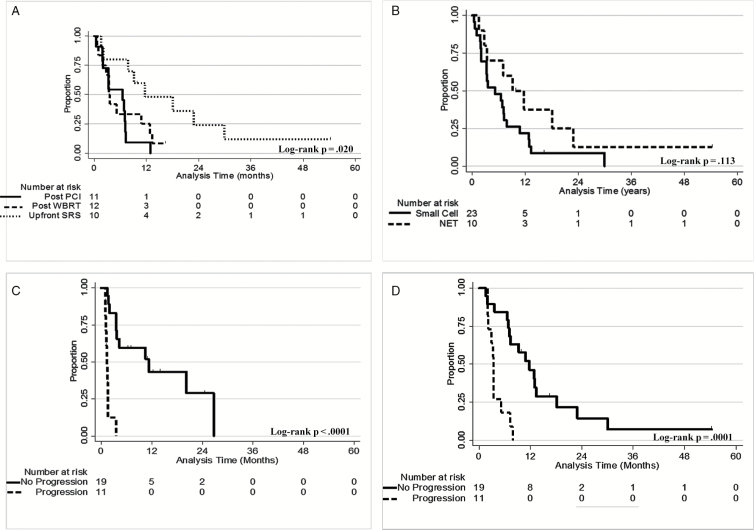
Median OS after SRS for the entire cohort was 6.9 months (range, 0.5–54.9 months). The longest median OS was in the upfront SRS group at 11.9 months (range, 1.6–54.9 months) compared to 6.6 months (range, 0.5–13.1 months) in the post-PCI group and 3.4 months (0.7–16.5 months) in the post-WBRT group (P = .02), as shown in Fig. 1A. Overall 6-month and 1-year OS were 54.5% and 26.7%, which were also highest in the upfront SRS group at 80% and 48%, respectively. Moreover, patients in this group also had the longest survival after their cancer diagnosis at 29 months compared with 19 months in the other two groups. Median OS of patients with small cell carcinoma was not significantly different from that of patients with other neuroendocrine tumors, 5.3 months (range, 0.5–30.4 months) vs 9.6 months (range, 1.6–54.9 months) (P = .11, Fig. 1B).
Fig. 1.
(A) Overall survival by treatment group. (B) Overall survival by histology. (C) Distant-brain-recurrence free survival by RANO-BM progression at 4 to 6 weeks after SRS. (D) Overall survival by RANO-BM progression at 4 to 6 weeks after SRS. Abbreviations: NET, neuroendocrine tumor; PCI, prophylactic cranial irradiation; RANO-BM, Response Assessment in Neuro-Oncology-Brain Metastases; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy.
Median local recurrence-free survival was not reached in the post-PCI and post WBRT-groups but was 20.5 months (range, 1.4–27.1 months) in the upfront SRS group. One-year local recurrence-free survival rates were 100% in the post-WBRT group, 75% in the post-PCI group, and 75% in the upfront SRS group. Median distant-brain-recurrence-free survival (DBRFS) after SRS was 3.5 months (range, 1–27.1 months) overall. Median DBRFS was 3.1 months (range, 1–24.9 months) in the post-PCI group, 10.7 months (range, 1–12.4 months) in the post-WBRT group, and 3.7 months (range, 1.4–38.3 months) in the upfront SRS group (P = .76). Overall, the DBRFS rate was 29.3% at 1 year.
When patients were classified according to RANO-BM response, both DBRFS and OS were significantly lower in patients who had progressive disease at 4 to 6 weeks after SRS. The median DBRFS and OS rates were 1.4 months and 3.3 months for patients with progressive disease compared with 11.4 months and 12 months for patients without progressive disease at 4 to 6 weeks after SRS, respectively (P < .001 both) (Fig. 1C and D).
Median OS from diagnosis of brain metastases was significantly longer in the post-WBRT group, 18 months (range, 4.1–35.2 months) compared with 7.4 months (range, 1.7–14.6 months) in the post-PCI group and 12.3 months (range, 1.9–56 months) in the upfront SRS group (P = .001). Considering histology, there was no difference in OS after diagnosis of brain metastases between small cell carcinoma and other neuroendocrine tumors (P = .40), but there was a trend toward higher OS of patients with tumors of pulmonary origin compared with extrapulmonary origin (13.8 vs 8.9 months, P = .06).
Overall median OS from cancer diagnosis was 25.4 months. This was significantly higher in the group of patients that developed radiation necrosis, 34.2 months (range, 27–56 months) vs 19.3 months (range, 8.6–42 months) in non-radiation necrosis group (P = .046). Otherwise, there was no statistically significant difference in OS from cancer diagnosis between treatment groups (P = .19), histologic subtypes (P = .87), or primary tumor site (P = .99).
Predictors of Outcomes
Univariate analyses demonstrated that upfront SRS was prognostic for better OS after SRS (P = .01) and that prior PCI (P = .047), prior chemotherapy (P = .04), a single course of SRS (P = .04), and RANO-BM progressive disease at 4 to 6 weeks (P < .001) were prognostic for worse OS after SRS. On multivariate analysis, RANO-BM progressive disease at 4 to 6 weeks after SRS was significantly predictive of worse OS and DBRFS (P < .001; hazard ratio [HR] = 8.36; 95% confidence interval [CI], 2.62–26.66 and P < 0.001; HR = 9.84; 95% CI, 2.82–34.33, respectively) (Tables 3 and 4).
Table 3.
Predictors of Overall Survival After Stereotactic Radiosurgery
| Univariate analysis | P value | Hazard ratio (95% CI) |
|---|---|---|
| Age (≥65 years) | .212 | 1.75 (1.00–1.07) |
| KPS (>70) | .733 | 1.19 (0.45–3.15) |
| Sex (male) | .837 | 1.00 (0.96–1.05) |
| Histology (NETs vs SCC) | .120 | 0.52 (0.23–1.19) |
| Extracranial disease (active) | .879 | 0.94 (0.43–2.06) |
| Initial brain metastases | .083 | 0.42 (0.16–1.12) |
| Number of brain metastasis (continuous variable) | .408 | 1.03 (0.95–1.12) |
| Prior PCI vs no prior PCI | .047 | 2.26 (1.01–5.07) |
| Prior WBRT vs no prior WBRT | .637 | 0.84 (0.41–1.73) |
| Prior chemotherapy | .035 | 8.87 (1.16–67.77) |
| Upfront SRS | .012 | 0.28 (0.11–0.76) |
| Post-SRS chemotherapy | .277 | 0.62 (0.27–1.46) |
| Single course SRS vs multiple courses of SRS | .043 | 2.78 (1.03–7.47) |
| RANO-BM progressive disease at 4 to 6 weeks after SRS | <.001 | 6.34 (2.3–17.25) |
| Local recurrence | .191 | 0.49 (0.17–1.43) |
| Distant brain recurrence | .398 | 0.71 (0.32–1.58) |
| Multivariate analysis | P value | Hazard ratio (95%CI) |
| Age (≥65 years) | .178 | 2.05 (0.72–5.82) |
| Histology (NETs vs. SCC) | .230 | 1.84 (0.68–5.00) |
| Initial brain metastases | .131 | 0.40 (0.12–1.32) |
| Upfront SRS | .064 | 0.33 (0.10–1.07) |
| RANO-BM progressive disease at 4 to 6 weeks after SRS | <.001 | 8.36 (2.62–26.66) |
Abbreviation: KPS, Karnofsky performance status; NETs, neuroendocrine tumors; PCI, prophylactic cranial irradiation; RANO-BM, Response Assessment in Neuro-Oncology Brain Metastases; SCC, small cell carcinoma; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy.
Table 4.
Predictors of Distant-brain recurrence-free Survival
| Univariate analysis | P value | Hazard ratio (95% CI) |
|---|---|---|
| Age (≥65 years) | .702 | 0.78 (0.23–2.72) |
| KPS (>70) | .924 | 0.95 (0.31–2.89) |
| Sex (male) | .942 | 0.97 (0.39–2.39) |
| Histology (NETs vs. SCC) | .988 | 0.99 (0.39–2.53) |
| Extracranial disease (active) | .581 | 1.32 (0.50–3.48) |
| Initial brain metastases | .276 | 1.68 (0.66–4.30) |
| Number of brain metastases (continuous variable) | .005 | 1.15 (1.05–1.27) |
| Prior PCI vs no prior PCI | .602 | 1.30 (0.49–3.44) |
| Prior WBRT vs no prior WBRT | .995 | 1.0 (0.40–2.48) |
| Prior chemotherapy | .854 | 0.89 (0.26–3.09) |
| Upfront SRS | .618 | 0.79 (0.31–2.02) |
| Post-SRS chemotherapy | .918 | 1.05 (0.41–2.71) |
| Single course SRS vs multiple courses of SRS | .397 | 0.67 (0.26–1.70) |
| RANO-BM progressive disease at 4 to 6 weeks after SRS | <.001 | 11.53 (3.60–36.91) |
| Local recurrence | .702 | 0.81 (0.27–2.45) |
| Distant brain recurrence | — | — |
| Multivariate analysis | P value | Hazard ratio (95% CI) |
| Age (≥65 years) | .987 | 0.99 (0.27–3.67) |
| Histology (NETs vs SCC) | .659 | 0.78 (0.25–2.40) |
| Number of brain metastases (continuous variable) | .065 | 1.11 (0.99–1.25) |
| RANO-BM progressive disease at 4 to 6 weeks after SRS | <.001 | 9.84 (2.82–34.33) |
Abbreviation: KPS, Karnofsky performance status; NETs, neuroendocrine tumors; PCI, prophylactic cranial irradiation; RANO-BM, Response Assessment in Neuro-Oncology Brain Metastases; SCC, small cell carcinoma; SRS, stereotactic radiosurgery; WBRT, whole brain radiation.
Discussion
SRS can be performed as primary or salvage treatment for patients with brain metastases from neuroendocrine tumors with good outcomes. Toxicity, including radiation necrosis, was more likely to occur in patients with small cell histology rather than other neuroendocrine tumors. RANO-BM progressive disease at 4 to 6 weeks after SRS was significantly predictive of worse OS and DBRFS.
The risk of brain metastasis from SCLC ranges from 25% to 65% and can be as high as 18% at the time of diagnosis,7,8 whereas the incidence is only 1.5% to 5.9% in patients with non-SCLC neuroendocrine tumors.20,21A recent meta-analysis confirmed that PCI significantly reduces the incidence of brain metastasis at 1 year with a pooled relative risk of 0.45 (95% CI, 0.35–0.58) as well as providing a survival benefit with a pooled relative risk of 0.87 (95% CI, 0.79–0.97).13 This supports the importance of PCI in patients with SCLC but not other neuroendocrine tumors.4,22
Reirradiation with WBRT was the historic mainstay of treatment after PCI and improved symptoms in 27% to 80% of patients with limited median survival of 2 to 5.2 months and time to progression of 2.6 to 2.8 months.23–28 More recently, several studies have established the role of SRS in patients with SCLC, both as salvage and upfront treatment, with local control rates of 54% to 96.4% and distant brain control rate of 22.4% to 77.8% at 1 year with median OS of 3 to 9.1 months, as shown in Table 5.29–40 Median time to distant brain recurrence ranged from 3 to 7 months, similar to our study.
Table 5.
Treatment Outcomes of Small Cell Lung Carcinoma/ Neuroendocrine Tumor Patients With Brain Metastases Treated With SRS
| Study | Year | No. of patients* / lesions | Median No. of brain metastases (range) | Sequence of SRS | Median dose (Gy) | 1-year LRFS | 1-year DBRFS | MS after SRS | ||
|---|---|---|---|---|---|---|---|---|---|---|
| After PCI | After WBRT | Upfront | ||||||||
| Primary small cell lung carcinoma | ||||||||||
| Serizawa33 | 2002 | 34 (total 245) | 4.6 (1–10) | — | — | 100% | 21 | 94.5% | — | 9.1 mo |
| Wegner34 | 2011 | 44 / 128 | 1 (1–14) | 27.3% | 54.5% | 18.2% | 18 | 86% | 39% | 9 mo |
| Jo30 | 2011 | 50 / 202 | 4 (1–15) | 22% | 54% | 24% | 17.4 | 70.3% | 70.3% | 6.3 mo |
| Harris29 | 2012 | 51 | 2–4 (1–5) | 31.4% | 68.6% | — | 18 | 57% | 42% | 5.9 mo |
| Olson18 | 2012 | 27 | 2 (1–6) | 30% | 70% | — | 20.5 | 76.5% | 40% | 3 mo |
| Grandhi38 | 2012 | 5 (total 61) | 13.2 (10–28) | — | 75.4% | 24.6% | 16 | 58.3% | 22.4% | 4 mo |
| Kuremsky31 | 2013 | 31 / 271 | 2 | 83.9% | — | 16.1% | 20 | 54% | 37% | 5.9 mo |
| Nakazaki32 | 2013 | 44 / 473 | 5 (1–36) | 22.7% | 77.3% | — | 20 | 96.4% | 42.9% | 5.8 mo |
| Yomo35 | 2014 | 41 / 121 | 2 (1–10) | — | — | 100% | 20 | 86% | 56% | 8.1 mo |
| Yomo36 | 2015 | 70 / 292 | 2 (1–21) | 10% | 22.9% | 67.1% | 20 | 77% | 53% | 7.8 mo |
| Primary small cell carcinoma of cervix | ||||||||||
| Chung39 | 2013 | 3 (total 13) | 5.7 (1–16) | — | 33.3% | 66.7% | 14 | 66.7% | 77.8% | 4.6 mo |
| Mixed patient population | ||||||||||
| Our study | 2015 | 33 / 147 | 3 (1–24) | 33.3% | 36.4% | 30.3% | 20 | 82.5% | 29.3% | 6.9 mo |
Abbreviation: DBRFS, distant-brain recurrence-free survival; LRFS, local recurrence-free survival; MS, median survival; PCI, prophylactic cranial irradiation; SRS, stereotactic radiosurgery; WBRT, whole brain radiation therapy.
* Number of patients with small cell carcinoma/total number of patients in study.
The efficacy of SRS as upfront treatment in patients with brain metastases from SCLC has been discussed in several studies. Serizawa et al34 studied 245 patients with 2374 brain metastasis from lung cancers, in which 34 patients had SCLC. Overall, median age was 65.5 years and 79.4% of patients had active extracranial disease. Local control was 94.5% at 1 year and median survival was 9.1 months. Recently, Yomo et al36 reported on SRS as upfront treatment in patients with brain metastases from SCLC in 41 patients with 121 lesions. The median age was 69 years and 61% of patients had active extracranial disease. They demonstrated a 1-year local-recurrence-free survival rate of 86% and a median survival time of 8.1 months. In our study, the local control rate in the upfront SRS group was comparable with these trials with a slightly increased OS. This is likely due to the younger age of our patient population (median age of 48 years), non-SCLC neuroendocrine tumor histology, and the lower rate of uncontrolled extracranial disease at the time of SRS (33.3%).
The rate of radiation necrosis in our patients was higher than expected but no differences were found between the treatment groups. Overall, 5 patients (16.7%) experienced symptomatic radiation necrosis requiring steroids, compared with 1.8% to 6% in other trials of SRS in SCLC despite similar SRS doses.29,31,36
The limitations of this study include the small number of patients and its retrospective nature. Although patients treated with upfront SRS had better OS, 11.9 months, compared with 8.1 to 9.1 months in other upfront SRS studies,33,35 patients in this group were young and had an excellent performance status. Moreover, patients with neuroendocrine tumors other than SCLC were more likely to receive upfront SRS, as shown in Table 1. Another drawback is the short follow-up time due to limited survival from disease. The strength of this study is the use of MRI as the standard imaging modality for diagnosis, treatment, and follow-up, as well as the uniform radiosurgery technique, with all patients treated over a time period of 5 years. Patients in our study were diagnosed accurately and promptly with brain metastases and evaluated for treatment response and toxicity using the most recent criteria. Furthermore, our series is unique in including neuroendocrine tumors and small cell carcinoma from any primary site.
Conclusion
SRS is an effective option as initial and salvage treatment for patients with brain metastases from NETs with excellent local control despite slightly higher rates of toxicity than expected. RANO-BM progressive disease at 4 to 6 weeks after SRS was a significant predictor for worse OS and DBRFS.
Disclosure of funding
None.
Conflicts of Interest. None.
References
- 1. Klimstra DS, Modlin IR, Coppola D, et al. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas. 2010;39(6):707–712. [DOI] [PubMed] [Google Scholar]
- 2. Rekhtman N. Neuroendocrine tumors of the lung: an update. Arch Pathol Lab Med. 2010;134(11):1628–1638. [DOI] [PubMed] [Google Scholar]
- 3. Pamela K. Carcinoid and neuroendocrine tumors: building on success. J Clin Oncol. 2015;33(16):1855–1863. [DOI] [PubMed] [Google Scholar]
- 4. Walenkamp AM, Sonke GS, Sleijfer DT. Clinical and therapeutic aspects of extrapulmonary small cell carcinoma. Cancer Treat Rev. 2009;35(3):228–236. [DOI] [PubMed] [Google Scholar]
- 5. Maiuri F, Cappabianca P, Del Basso De Caro M, et al. Single brain metastases of carcinoid tumors. J Neurooncol. 2004;66(3):327–332. [DOI] [PubMed] [Google Scholar]
- 6. Burzawa J, Gonzales N, Frumovitz M. Challenges in the diagnosis and management of cervical neuroendocrine carcinoma. Expert Rev Anticancer Ther. 2015;15(7):805–810. [DOI] [PubMed] [Google Scholar]
- 7. Seute T, Leffers P, ten Velde GP, et al. Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer. 2004;100(4):801–806. [DOI] [PubMed] [Google Scholar]
- 8. Sas-Korczyńska B, Korzeniowski S, Wójcik E. Comparison of the effectiveness of “late” and “early” prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. Strahlenther Onkol. 2010;186(6):315–319. [DOI] [PubMed] [Google Scholar]
- 9. Arriagada R, Le Chevalier T, Rivière A, et al. Patterns of failure after prophylactic cranial irradiation in small-cell lung cancer: analysis of 505 randomized patients. Ann Oncol. 2002;13(5):748–754. [DOI] [PubMed] [Google Scholar]
- 10. Aupérin A, Arriagada R, Pignon JP, et al. Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic Cranial Irradiation Overview Collaborative Group. N Engl J Med. 1999;341(7):476–484. [DOI] [PubMed] [Google Scholar]
- 11. Prophylactic Cranial Irradiation Overview Collaborative Group. Cranial irradiation for preventing brain metastases of small cell lung cancer in patients in complete remission. Cochrane Database Syst Rev. 2000; (4):CD002805. [DOI] [PubMed] [Google Scholar]
- 12. Slotman B, Faivre-Finn C, Kramer G, et al. ; EORTC Radiation Oncology Group and Lung Cancer Group. Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med. 2007;357(7):664–672. [DOI] [PubMed] [Google Scholar]
- 13. Zhang W, Jiang W, Luan L, et al. Prophylactic cranial irradiation for patients with small-cell lung cancer: a systematic review of the literature with meta-analysis. BMC Cancer. 2014;14:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Seute T, Leffers P, ten Velde GP, et al. Detection of brain metastases from small cell lung cancer: consequences of changing imaging techniques (CT versus MRI). Cancer. 2008;112(8):1827–1834. [DOI] [PubMed] [Google Scholar]
- 15. Huang MC, Lee LS, Ho DM, et al. A metastatic pituitary carcinoid tumor successfully treated with gamma knife radiosurgery. Zhonghua Yi Xue Za Zhi (Taipei). 2001;64(7):414–418. [PubMed] [Google Scholar]
- 16. Nakamura Y, Shimokawa S, Ishibe R, et al. Pulmonary carcinoid found in a patient who presented with initial symptoms of brain metastasis: report of a case. Surg Today. 2001;31(6):510–512. [DOI] [PubMed] [Google Scholar]
- 17. Mallory GW, Fang S, Giannini C, et al. Brain carcinoid metastases: outcomes and prognostic factors. J Neurosurg. 2013;118(4):889–895. [DOI] [PubMed] [Google Scholar]
- 18. Lin NU, Lee EQ, Aoyama H, et al. ; Response Assessment in Neuro-Oncology (RANO) group. Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol. 2015;16(6):e270–e278. [DOI] [PubMed] [Google Scholar]
- 19. Kaplan EL, Meier P. Nonparametric-estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 20. Patchell RA, Posner JB. Neurologic complications of carcinoid. Neurology. 1986;36(6):745–749. [DOI] [PubMed] [Google Scholar]
- 21. Hlatky R, Suki D, Sawaya R. Carcinoid metastasis to the brain. Cancer. 2004;101(11):2605–2613. [DOI] [PubMed] [Google Scholar]
- 22. Pavel M, Grossman A, Arnold R, et al. ; Palma de Mallorca Consensus Conference Participants. ENETS consensus guidelines for the management of brain, cardiac and ovarian metastases from neuroendocrine tumors. Neuroendocrinology. 2010;91(4):326–332. [DOI] [PubMed] [Google Scholar]
- 23. Cooper JS, Steinfeld AD, Lerch IA. Cerebral metastases: value of reirradiation in selected patients. Radiology. 1990;174(3 Pt 1):883–885. [DOI] [PubMed] [Google Scholar]
- 24. Hazuka MB, Kinzie JJ. Brain metastases: results and effects of re-irradiation. Int J Radiat Oncol Biol Phys. 1988;15(2):433–437. [DOI] [PubMed] [Google Scholar]
- 25. Sadikov E, Bezjak A, Yi QL, et al. Value of whole brain re-irradiation for brain metastases—single centre experience. Clin Oncol (R Coll Radiol). 2007;19(7):532–538. [DOI] [PubMed] [Google Scholar]
- 26. Son CH, Jimenez R, Niemierko A, et al. Outcomes after whole brain reirradiation in patients with brain metastases. Int J Radiat Oncol Biol Phys. 2012;82(2):e167–e172. [DOI] [PubMed] [Google Scholar]
- 27. Wong WW, Schild SE, Sawyer TE, et al. Analysis of outcome in patients reirradiated for brain metastases. Int J Radiat Oncol Biol Phys. 1996;34(3):585–590. [DOI] [PubMed] [Google Scholar]
- 28. Postmus PE, Haaxma-Reiche H, Gregor A, et al. Brain-only metastases of small cell lung cancer; efficacy of whole brain radiotherapy. An EORTC phase II study. Radiother Oncol. 1998;46(1):29–32. [DOI] [PubMed] [Google Scholar]
- 29. Harris S, Chan MD, Lovato JF, et al. Gamma knife stereotactic radiosurgery as salvage therapy after failure of whole-brain radiotherapy in patients with small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2012;83(1):e53–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jo KW, Kong DS, Lim DH, et al. The role of radiosurgery in patients with brain metastasis from small cell lung carcinoma. J Korean Neurosurg Soc. 2011;50(2):99–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kuremsky JG, Urbanic JJ, Petty WJ, et al. Tumor histology predicts patterns of failure and survival in patients with brain metastases from lung cancer treated with gamma knife radiosurgery. Neurosurgery. 2013;73(4):641–647; discussion 647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nakazaki K, Higuchi Y, Nagano O, et al. Efficacy and limitations of salvage gamma knife radiosurgery for brain metastases of small-cell lung cancer after whole-brain radiotherapy. Acta Neurochir (Wien). 2013;155(1):107–113; discussion 113. [DOI] [PubMed] [Google Scholar]
- 33. Olson AC, Wegner RE, Rwigema JC, et al. Clinical outcomes of reirradiation of brain metastases from small cell lung cancer with Cyberknife stereotactic radiosurgery. J Cancer Res Ther. 2012;8(3):411–416. [DOI] [PubMed] [Google Scholar]
- 34. Serizawa T, Ono J, Iichi T, et al. Gamma knife radiosurgery for metastatic brain tumors from lung cancer: a comparison between small cell and non-small cell carcinoma. J Neurosurg. 2002;97(5 Suppl):484–488. [DOI] [PubMed] [Google Scholar]
- 35. Wegner RE, Olson AC, Kondziolka D, et al. Stereotactic radiosurgery for patients with brain metastases from small cell lung cancer. Int J Radiat Oncol Biol Phys. 2011;81(3):e21–e27. [DOI] [PubMed] [Google Scholar]
- 36. Yomo S, Hayashi M. Upfront stereotactic radiosurgery in patients with brain metastases from small cell lung cancer: retrospective analysis of 41 patients. Radiat Oncol. 2014;9:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yomo S, Hayashi M. Is stereotactic radiosurgery a rational treatment option for brain metastases from small cell lung cancer? A retrospective analysis of 70 consecutive patients. BMC Cancer. 2015;15:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sheehan J, Kondziolka D, Flickinger J, et al. Radiosurgery for patients with recurrent small cell lung carcinoma metastatic to the brain: outcomes and prognostic factors. J Neurosurg. 2005;102(Suppl):247–254. [DOI] [PubMed] [Google Scholar]
- 39. Grandhi R, Kondziolka D, Panczykowski D, et al. Stereotactic radiosurgery using the Leksell Gamma Knife Perfexion unit in the management of patients with 10 or more brain metastases. J Neurosurg. 2012;117(2):237–245. [DOI] [PubMed] [Google Scholar]
- 40. Chung SB, Jo KI, Seol HJ, et al. Radiosurgery to palliate symptoms in brain metastases from uterine cervix cancer. Acta Neurochir (Wien). 2013;155(3):399–405. [DOI] [PubMed] [Google Scholar]
- 41. Videtic GM, Adelstein DJ, Mekhail TM, et al. Validation of the RTOG recursive partitioning analysis (RPA) classification for small-cell lung cancer-only brain metastases. Int J Radiat Oncol Biol Phys. 2007;67(1):240–243. [DOI] [PubMed] [Google Scholar]
- 42. Sperduto PW, Chao ST, Sneed PK, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4259 patients. Int J Radiat Oncol Biol Phys. 2010;77(3):655–661. [DOI] [PubMed] [Google Scholar]
- 43. Weltman E, Salvajoli JV, Brandt RA, et al. Radiosurgery for brain metastases: a score index for predicting prognosis. Int J Radiat Oncol Biol Phys. 2000;46(5):1155–1161. [DOI] [PubMed] [Google Scholar]