Abstract
Introduction: Dysmenorrhea (period pain) is common and affects around three quarters of all young women under the age of 25. The majority of young women, for a variety of reasons, think of period pain as ‘normal’ and something to be managed or endured. This normalisation of pain often is reinforced by family and friends and results in young women using self-care strategies to manage their pain rather than seeking medical advice. This systematic review and meta-analysis examined observational studies reporting on the prevalence of different types of self-care, both pharmaceutical and non-pharmaceutical, self-rated effectiveness of self-care and the sources of information on menstruation in young women under 25 Methods: A search of Medline, PsychINFO, EMBASE and CINAHL in English was carried out from 1980 to December 2018. Studies that reported on menstrual self-care strategies in young women were included. Results: Nine hundred and forty-seven articles were screened. Twenty-four studies including 12,526 young women were eligible and included in the meta-analysis. Fifteen studies were from low, lower-middle or upper-middle-income countries (LMIC) and nine studies were from high income countries (HIC). Self-care was used by over half of all young women (55%, 95%CI 34.1–74.3) with both pharmaceutical (48%, 95%CI 40.0–57.0) and non-pharmaceutical (51.8%, 95%CI 31.3–71.7) options used. Paracetamol was the most common analgesic used (28.7%, 95%CI 19.6–39.9) but did not always provide sufficient pain relief in almost half of those using it. Contraceptive use was significantly higher (P<0.001) in HIC (22%) compared to LMIC (1%). Only 11% (95%CI 8.4–15.2) of young women reported seeing a medical doctor for their period pain. Conclusions: Self-care usage, both pharmaceutical and non-pharmaceutical, was common, but young women were not necessarily choosing the most effective options for pain management. High-quality information on self-care for period pain is urgently needed.
Introduction
Dysmenorrhea (period pain) is common and our recent meta-analysis shows dysmenorrhea affects around three quarters of all young women under the age of 25 worldwide[1]. Primary dysmenorrhea is defined as menstrual pain in the absence of underlying pathology [2, 3] and is the most common cause of dysmenorrhea in young women under the age of 25 [4]. In addition to painful cramps, many women with dysmenorrhea experience other menstrual related symptoms including back and thigh pain, headaches, diarrhoea, nausea and vomiting [5].
Dysmenorrhea or its associated symptoms often result in a reduction in classroom performance and increased absenteeism at school and tertiary education[1]. Despite this negative impact, most young women frame period pain as a normal part of being a woman[6], a common theme across varying geographic and ethnic boundaries[7, 8]. In addition, some countries such as Sri Lanka, Nigeria and India, have traditionally held strong taboos related to menstruation [9–11]. This in turn may impact how women manage their menstrual pain due to their beliefs and attitudes and/or a lack of accurate information[12].
In managing their period pain, many young women primarily use self-care. Self-care includes physical (e.g exercise, stretching or rest), pharmacological (e.g analgesic medication), non-pharmacological (e.g herbal medicine, heat) or psychological strategies (e.g prayer or meditation) that are usually undertaken by women themselves without seeking medical advice [13]. In the case of period pain these commonly include over the counter (OTC) analgesic medications (e.g. ibuprofen and paracetamol), rest and the application of heat [7, 8, 14–22]. Lack of satisfactory pain relief and effective medical interventions in primary dysmenorrhea leads to an uptake of self-care strategies by women[23]. Complementary medicine usage (such as herbal medicines or traditional remedies) is often a significant component of self-care[23, 24]. Many women already use various forms of complementary medicine to manage their menstrual pain in addition to, or instead of, pharmaceutical pain relief, due to a lack of perceived effectiveness[19, 22] or a dislike of using analgesic medication[25].
The implications of normalising menstrual pain in conjunction with a lack of understanding of effective self-care strategies may lead to poor pain management. Given the link between pain intensity and negative outcomes, such as absenteeism, at school, university or work [26] ensuring that young women have access to effective self-care such as non-steroidal anti-inflammatories (NSAIDs) [27], the contraceptive pill [2] or effective non-pharmaceutical methods such as exercise[28] and heat [13] is vital. It is currently unclear what self-care strategies young women worldwide are using, if they are finding them effective, and what sources of information they are accessing to help make those decisions.
The aim of this systematic review and meta-analysis was to determine the prevalence and type(s) of self-care used for dysmenorrhea, the sources of information on menstruation used by young women under 25, and to explore any possible differences in both self-care and sources of information between low to middle income (LMIC) and high income (HIC) countries.
Materials and methods
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (S2 File—PRISMA) guidelines were adhered to throughout this review [29].
Search strategy and selection criteria
A literature search was performed on Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Embase, and PsycINFO databases. All databases were searched from 1980 till 1 December 2018 using the following main keywords: ‘self-care,’ ‘management’, ‘symptoms’, ‘dysmennorhoea’ and ‘adolescen*’. The search and selection processes are outlined in Fig 1. The detailed search strategy is enclosed in S1 File. Only English language articles published in peer reviewed journals were included.
Fig 1. PRISMA flow diagram of the search and selection process.

Observational studies (including cohort, cross-sectional, and case-control studies) were included. Studies were eligible if they specified that the participants were either at school or university (even if age was not reported) or were recruited from the broader community and included those aged ≤25 years. Eligible studies were those that included data on self-management strategies. Self-management could include either pharmacological (such as analgesic medication or the contraceptive pill) or non-pharmacological strategies (such as rest or herbal medicine). Studies which reported on secondary dysmenorrhea only were excluded as these would not represent the true prevalence rate or impact of dysmenorrhea. Studies which only reported qualitative data were not eligible for inclusion.
Data extraction
Two authors (MA, KP) assessed eligibility, while three authors (MA, KP, MaD) extracted the data independently and any disagreements were resolved by discussion. Where data were missing or unclear, the study authors were contacted via email to request the data. Authors were contacted twice over a 6-week period, and if no response was received within that period, the data was marked as missing. A systematic tool for data extraction was developed to extract all relevant information from eligible studies.
Data were extracted on all of the following outcomes (if reported):
Prevalence of dysmenorrhea
Overall self-care usage (all categories)
Overall analgesic usage (all categories)
Usage of analgesics by category (Paracetamol, Ibuprofen and Other NSAIDs)
Perceived effectiveness of analgesics (both overall and by category)
Overall non-pharmacological self-care usage (all categories)
Usage of the most common categories of non-pharmacological self-care (heat, rest, exercise, herbal medicines)
Perceived effectiveness of non-pharmacological self-care (both overall and by category)
Number and type of consultation(s) with health professionals (both overall and by category)
Sources of information about menstruation (family, friends, medical professionals, teachers and the internet)
Study characteristics (location, demographics) were also extracted. Self-care usage, analgesic usage and non-pharmacological self-care were only included if overall figures were reported in studies (eg they were not assembled by adding together sub-categories (such as number using heat and number using exercise)) as these often-allowed multiple answers and would likely have given incorrect estimates. If effectiveness data was presented as a Likert scale (e.g. I think paracetamol helps my period pain) all positive scores (such as agree or most of the time) were considered as evidence of effectiveness while neutral and negative responses (such as no change or never) were considered as not showing evidence of effectiveness. Given the diversity of potential self-care approaches due to the cultural and geographic diversity of included studies, four common categories were chosen to allow a manageable analysis. This was based on a combination of our recent review of effective self-care in dysmenorrhea [13] as well as the authors expert opinion on common strategies. Rest included options such as laying down, having a nap and sleeping. Heat included hot baths, hot showers, heat packs or hot water bottles and herbal medicine included herbal teas, decoctions, pills or powders. Finally, if the type of medical or health professional was not specified, for example if women indicated they visited a clinic this was classified as ‘Visited Other Health Professional’ as there was insufficient data to determine the type of health professional seen.
Quality assessment
Quality assessment of the reporting of the included studies was performed independently and in duplicate by all authors with any disagreements resolved by a third party. The quality of reporting in each study was assessed using a condensed version of the STROBE guidelines that have been used in previous reviews [30, 31]. The modified guidelines contain thirteen questions which covered reporting on; selection methods, validity and reliability of measures, methods to deal with bias, sample sizes and conflicts of interest. Each author rated bias items as yes (bias present) or no/unclear (bias may be present).
Data synthesis and meta-analysis
A random-effects meta-analyses was conducted using Comprehensive Meta-Analysis software (Version 3). Data were pooled for each outcome where there were data from at least three independent studies.
A random effects model was used to account for expected heterogeneity between studies. Statistical heterogeneity between studies was quantified using Cochran’s Q and I2 statistic, both of which provide estimates of the degree of heterogeneity resulting from between-study variance, rather than by chance. Cochran's Q with p-value of <0.05 was classified as significant heterogeneity, and I2 of more than 75% was considered to indicate high level heterogeneity, I2 of 50%–75% as indicative of substantial heterogeneity, and an I2 of less than 40% as low heterogeneity.
Pre‐planned subgroup analyses were conducted to examine whether there was a difference in prevalence or impact in High income vs Low-Income, Lower-Middle-Income (LMIC) and Upper-Middle-Income (HIC) Economies (as classified by the World Bank[32]) due to differences in access to suitable medical and/or social support and between those at school and university/tertiary education to see if there were changes related to age or increased knowledge of menstruation. Sub-group analyses were conducted if there were a minimum of three studies for each sub-group.
Results
Nine hundred and forty-seven studies were returned by our searches after duplicate studies were removed. Fifty-three full text articles were screened. Twenty-nine studies were excluded after screening; 12 due to reporting only qualitative data, 16 for not reporting on the use of self-care or sources of menstrual knowledge and one for not reporting an age range in a community-based study, Twenty-four studies including 12,536 young women were included in the analysis. All studies were cross-sectional quantitative studies. Nine studies (6,275 young women) were from HIC and 15 studies (6,261 young women) from LMIC.
Four studies were undertaken in Nigeria[33–36], three in Australia[15, 37, 38] and Iran [39–41], two in Hong Kong [8, 22] and Mexico [14, 42], and one each in the USA [7], Taiwan [43], Sweden [44], Sri Lanka [45], Saudi Arabia [46], Malaysia [47], India [48], Ghana [49], Ethiopia [50] and Brazil [51]. Study publication dates ranged from 1985 to 2018. Mean ages at the time of the survey ranged from 13 [51] to 23 years old [49], with a median age of 19. Twelve studies did not report the mean age of the participants, but still met the inclusion criteria; ten were undertaken in schools, one at both school and university and one community study [37] reported a valid age range (14–19) but not the mean age. Fourteen studies reported on young women at school, six reported on young women at university or higher education, three recruited from a community population; one using online recruitment, one a mixture of online and postal and one where it was unclear, and one recruited from both school and university. Table 1 summarises the included studies.
Table 1. Characteristics of included studies.
| Study ID | Study Design | Country | Mean Age | Sample Size | Sample Population | Reports On |
|---|---|---|---|---|---|---|
| Abidoye (2012) | Cross-sectional quantitative | Nigeria | NR | 180 | School & University | • Overall Self-Care Usage • Analgesic/Pain Medication Use (Total) • Non-Pharma or Traditional Chinese Medicine Usage ○ Total ○ Rest ○ Heat |
| Abraham (1985) | Cross-sectional quantitative | Australia | NR Age range 15–19 years |
1377 | Community (unclear) | • Contraceptive Use • Sources of Advice: ○ Doctor ○ Friends ○ Teacher |
| Adinma (2008) | Cross-sectional quantitative | Nigeria | NR | 550 | School | • Analgesic/Pain Medication Use (Total) • Contraceptive Use • Non-Pharma or Traditional Chinese Medicine Usage ○ Total ○ Heat • Sources of Advice: ○ Doctor ○ Family ○ Friends ○ Teacher |
| Alsaleem (2018) | Cross-sectional quantitative | Saudi Arabia | 19.1 | 197 | University | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use: ○ Total ○ Other NSAID • Non-Pharma or Traditional Chinese Medicine Usage (Total) • Sources of Advice: ○ Doctor ○ Family ○ Friends ○ Teacher |
| Ameade (2018) | Cross-sectional quantitative | Ghana | 23 | 293 | University | • Prevalence of Dysmenorrhea • Overall Self-Care Usage • Analgesic/Pain Medication Use ○ Total ○ Paracetamol ○ Ibuprofen ○ Other NSAID • Non-Pharma or Traditional Chinese Medicine Usage: ○ Total ○ Herbal Medicine • Effectiveness of Analgesics (Total) • Sources of Advice: ○ Got Medical Advice (Total) ○ Family ○ Friends |
| Banikarim (2000) | Cross-sectional quantitative | USA | NR | 740 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Non-Pharma or Traditional Chinese Medicine Usage ○ Rest ○ Exercise ○ Herbal Medicine ○ Heat • Sources of Advice: ○ Doctor ○ Nurse |
| Chia (2013) | Cross-sectional quantitative | Hong Kong | 20.1 | 240 | University | • Prevalence of Dysmenorrhea • Overall Self-Care Usage • Analgesic/Pain Medication Use ○ Total ○ Paracetamol ○ Other NSAID • Non-Pharma or Traditional Chinese Medicine Usage (Total) • Effectiveness of Analgesics: ○ Paracetamol ○ Other NSAID • Effectiveness of Traditional Chinese Medicine (Total) • Sources of Advice (Got Medical Advice Total) |
| Chiou (2008) | Cross-sectional quantitative | Taiwan | 16.7 | 760 | University | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Non-Pharma or Traditional Chinese Medicine Usage ○ Rest ○ Exercise ○ Heat • Sources of Advice: ○ Doctor ○ Nurse ○ Family ○ Friends ○ Teacher |
| Devi (2014) | Cross-sectional quantitative | India | NR | 100 | School | • Analgesic/Pain Medication Use (Total) • Non-Pharma or Traditional Chinese Medicine Usage ○ Rest ○ Exercise • Sources of Advice: ○ Family ○ Friends |
| Ghaderi (2017) | Cross-sectional quantitative | Iran | 21.3 | 197 | University | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use ○ Total ○ Other NSAID • Non-Pharma or Traditional Chinese Medicine Usage (Total) • Sources of Advice: ○ Family ○ Friends ○ Internet |
| Hillen (1999) | Cross-sectional quantitative | Australia | NR | 388 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use ○ Total ○ Other NSAID • Contraceptive Use • Non-Pharma or Traditional Chinese Medicine Usage ○ Total ○ Herbal Medicine • Effectiveness of Analgesics: ○ Paracetamol ○ Other NSAID • Sources of Advice: ○ Doctor • Nurse |
| Moronkola (2006) | Cross-sectional quantitative | Mexico | NR | 120 | School | • Analgesic/Pain Medication Use: ○ Total ○ Paracetamol ○ Other NSAID |
| Ortiz (2009) | Cross-sectional quantitative | Mexico | NR | 1152 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use: ○ Paracetamol ○ Other NSAID • Effectiveness of Analgesics (Total) • Sources of Advice (Doctor) |
| Pitangui (2013) | Cross-sectional quantitative | Brazil | 13.65 | 218 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Sources of Advice: ○ Got Medical Advice (Total) ○ Teacher |
| Poureslami (2002) | Cross-sectional quantitative | Iran | NR | 250 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Sources of Advice (Got Medical Advice Total) |
| Rostami (2007) | Cross-sectional quantitative | Iran | NR | 660 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Sources of Advice (Doctor) |
| Saka (2018) | Cross-sectional quantitative | Nigeria | 15.2 | 400 | School | • Prevalence of Dysmenorrhea • Overall Self-Care Usage • Analgesic/Pain Medication Use ○ Paracetamol ○ Other NSAID • Non-Pharma or Traditional Chinese Medicine Usage (Total) • Sources of Advice: ○ Got Medical Advice (Total) ○ Family ○ Friends ○ Teacher |
| Söderman (2018) | Cross-sectional quantitative | Sweden | 16.2 | 1785 | Community (postal invitation with online collection) | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use ○ Total ○ Paracetamol ○ Ibuprofen • Contraceptive Use • Effectiveness of Analgesics (Total) • Sources of Advice: ○ Got Medical Advice (Total) ○ Doctor ○ Nurse |
| Subasinghe (2016) | Cross-sectional quantitative | Australia | 21.5 | 247 | Community (online) | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Contraceptive Use • Non-Pharma or Traditional Chinese Medicine Usage (Total) • Sources of Advice: ○ Got Medical Advice (Total) ○ Family |
| Sule (2007) | Cross-sectional quantitative | Nigeria | NR | 400 | School | • Prevalence of Dysmenorrhea • Overall Self-Care Usage ○ Total ○ Paracetamol ○ Other NSAID • Sources of Advice: ○ Family ○ Friends |
| Wijesiri (2013) | Cross-sectional quantitative | Sri Lanka | NR | 200 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use ○ Total ○ Paracetamol ○ Ibuprofen ○ Other NSAID • Non-Pharma or Traditional Chinese Medicine Usage ○ Rest ○ Exercise ○ Heat • Sources of Advice (Family) |
| Wong (2011) | Cross-sectional quantitative | Malaysia | 15.28 | 1295 | School | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use (Total) • Non-Pharma or Traditional Chinese Medicine Usage ○ Rest ○ Herbal Medicine ○ Heat • Sources of Advice: ○ Doctor ○ Family ○ Friends ○ Teacher |
| Wong (2015) | Cross-sectional quantitative | Hong Kong | 15.69 | 531 | School | • Analgesic/Pain Medication Use (Total) • Sources of Advice (Got Medical Advice Total) |
| Yesuf (2018) | Cross-sectional quantitative | Ethiopia | 20.5 | 246 | University | • Prevalence of Dysmenorrhea • Analgesic/Pain Medication Use ○ Total ○ Paracetamol ○ Ibuprofen ○ Other NSAID • Contraceptive Use • Non-Pharma or Traditional Chinese Medicine Usage: ○ Total ○ Rest • Sources of Advice (Doctor) |
STROBE assessment on reporting quality
The results of the STROBE assessment for the 24 studies are summarised in S1 Table. Twenty-three studies clearly reported their aim. Ten studies clearly reported their eligibility criteria, in addition one study reported the exclusion criteria only and one study reported very broad criteria. Thirteen studies used a form of random sampling. All 23 studies used questionnaires. Only five studies reported using validated measures, with three of these five studies lacking detail on how the measure was validated. Four studies reported a sample size calculation. Response rates ranged from 37% to 100%. Ten studies did not report response rates. Eight studies reported no conflict of interest, with one study reporting a potential conflict that was disclosed. The most common sources of bias were self-report bias, selection bias and responder bias, with recall bias also being present, but less common. Only two studies reported on methods used to minimise bias.
Prevalence of dysmenorrhea
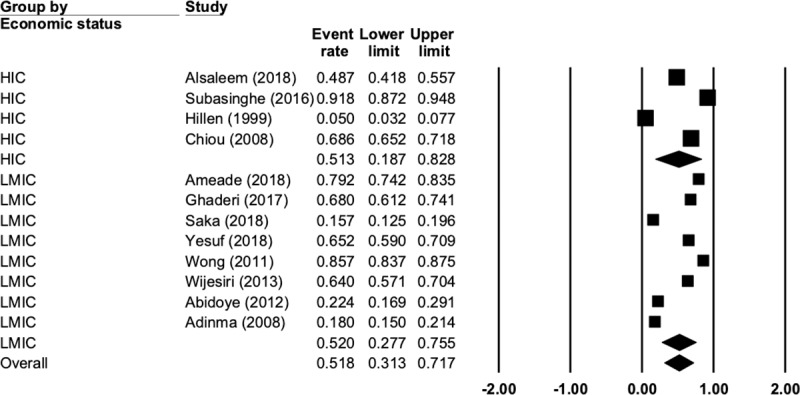
Overall prevalence rate for dysmenorrhea in the included studies was 78.5% (N = 18, n = 9668, 95% CI 73.7 to 82.7, Q = 718, P < 0.001, I2 = 97.6). When analysed by economic status, the prevalence of dysmenorrhea was higher in HIC countries at 81.7% (N = 7, n = 4357, 95% CI 75.2 to 86.8, Q = 124, P < 0.001, I2 = 95.1) than LMIC at 75.2% (N = 11, n = 5311, 95% CI 67.6 to 81.5, Q = 335, P < 0.001, I2 = 97.0), but this difference was not significant (p = 0.159). Fig 2 presents the complete data for this comparison.
Fig 2. Prevalence of dysmenorrhea by economic status.

Self-care usage
Only five studies reported on the overall rate of self-care usage. Self-care was used by 55% of women in the included studies (N = 5, n = 1513, 95% CI 34.1 to 74.3, Q = 216, P < 0.001, I2 = 98.1). There were not enough studies reporting on this outcome to perform subgroup analysis.
Pharmacological analgesia
Overall rates of pharmacological analgesia usage in the included studies was common, with just under half (48%) of women reporting using analgesics (N = 21, n = 9556, 95% CI 40.0 to 57.0, Q = 1246, P < 0.001, I2 = 98.3). Fig 3 presents the complete data for this comparison.
Fig 3. Pharmacological analgesia use.

There was no difference (p = 0.89) between analgesic usage in LMIC (48.7%, N = 13, n = 4709, 95% CI 38.9 to 58.6, Q = 475, P < 0.001, I2 = 98.4) and HIC (47.3%, N = 8, n = 4847, 95% CI 31.2 to 64.0, Q = 757, P < 0.001, I2 = 99.1). There was also no difference (p = 0.653) in the rates of analgesic usage in young women at school (43.1%) and university (48.9%).
When looking at specific classes of analgesics, paracetamol was the most common (28.7%) (N = 9, n = 4836, 95% CI 19.6 to 39.9, Q = 396, P < 0.001, I2 = 97.9), followed by other NSAIDS such a naproxen sodium (23.3%) (N = 11, n = 3833, 95% CI 16.3 to 32.3, Q = 311, P < 0.001, I2 = 96.7) and finally Ibuprofen (17.1%) (N = 4, n = 2524, 95% CI 6.3 to 38.8, Q = 172, P < 0.001, I2 = 98.2).
Three studies reported on the effectiveness of analgesic medication overall, where 31.5% of women reported that analgesic usage reduced their pain (N = 3, n = 3230, 95% CI 22.9 to 41.6, Q = 57, P < 0.001, I2 = 96.5). Two studies looked at the self-reported effectiveness of paracetamol (57.8%, N = 2, n = 628, 95% CI 53.9 to 61.7, Q = 0.54, P = 0.46, I2 = 0) and other NSAIDS (97.3% N = 2, n = 628, 95% CI 24.9 to 1.0, Q = 11, P = 0.001, I2 = 91).
Contraceptive use
Very few studies reported on contraceptive usage. In the six studies reporting on this, contraceptive usage was significantly higher (P<0.001) in HIC (22%, N = 4, n = 3797, 95% CI 11.0 to 39.3, Q = 268, P<0.001, I2 = 98) compared to LMIC (<1%, N = 2, n = 246, 95% CI 0.0 to 2.9, Q = 1.9, P = 0.165, I2 = 48).
Traditional, complementary or non-pharmacological interventions
Usage of complementary, traditional or non-pharmacological interventions to manage menstrual symptoms was common (51.8%, N = 12, n = 4913, 95% CI 31.3 to 71.7, Q = 1273, P < 0.001, I2 = 99.1). Fig 4 presents the complete data for this comparison. There was no difference (p = 0.974) between LMIC (52%, N = 8, n = 3361, 95% CI 27.7 to 75.5, Q = 970, P < 0.001, I2 = 99.2) and HIC (51%, N = 4, n = 1552, 95% CI 18.7 to 82.8, Q = 302, P < 0.001, I2 = 99.0).
Fig 4. Complementary, traditional or non-pharmacological interventions.
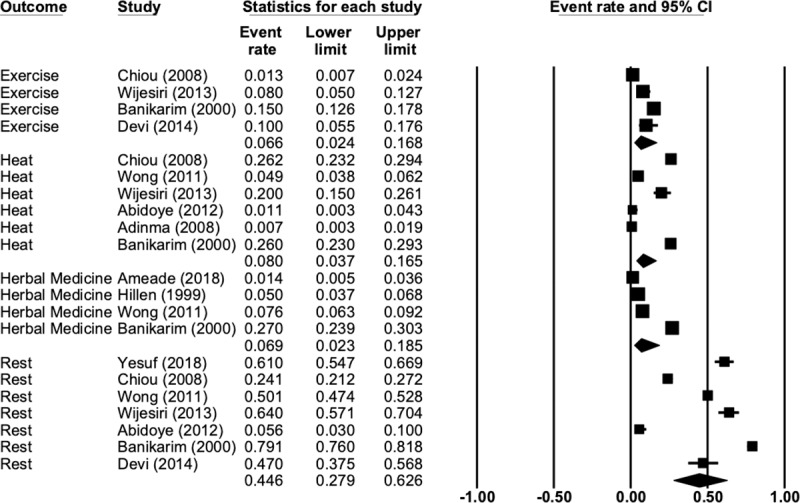
Rest was the most commonly used non-pharmacological intervention (44.6%) followed by heat (8%), herbal medicine or herbal teas (6.9%) and exercise (6.6%). Fig 5 presents the complete data for this comparison. There were not enough studies reporting on these outcomes to perform a subgroup analysis. There was only one study that reported on the effectiveness of these interventions, so no analysis was performed.
Fig 5. Traditional, complementary or non-pharmacological intervention comparison.
Medical consultations
Only 11% of women in the included studies reported visiting a medical doctor to discuss their period pain (N = 11, n = 9150, 95% CI 8.4 to 15.2, Q = 252, P<0.001, I2 = 96). There was no difference in consultation rates between HIC (10.7%, N = 6, n = 5247, 95% CI 6.4 to 17.3, Q = 178, P<0.001, I2 = 97) and LMIC (11.8%, N = 5, n = 3903, 95% CI 8.1 to 16.8, Q = 70, P<0.001, I2 = 94). Four studies, all performed in HIC, reported that 22% of young women reported visiting a nurse, usually at school (N = 4, n = 3673, 95% CI 11.1 to 38.8, Q = 263, P<0.001, I2 = 98). In addition, 15.1% of women in the included studies reported seeking medical attention or advice (such as visiting a clinic) but the studies did not specify what kind of health professional they saw (N = 8, n = 3924, 95% CI 10.2 to 21.8, Q = 203, P<0.001, I2 = 96).
Other sources of information
Outside of medical consultations the most common sources of information about menstrual symptoms was family (62.4%, N = 11, n = 4598, 95% CI 60.9 to 64.0, Q = 476, P<0.001, I2 = 97.9), friends (51.4%, N = 10, n = 5569, 95% CI 49.8 to 53.0, Q = 923, P<0.001, I2 = 99.0) and teachers/lecturers (22.8%, N = 7, n = 1377, 95% CI 21.5 to 24.1, Q = 306, P<0.001, I2 = 98.4). Only one study (n = 197) reported on the use of the internet (21.8%). There was no difference in rate of consulting these sources when comparing LMIC or HIC (all P>0.05). Young women at school (24.6%) were much more likely (P<0.001) to list teachers as a source of information on menstruation than those at university (3.6%).
Discussion
The overall rates of dysmenorrhea (78%) in the included studies were similar to our previous meta-analysis on worldwide prevalence rates (71.1%)[1]. The usage of self-care or self-management strategies was relatively common with just over half of women reporting using self-care. Both non-pharmacological strategies and analgesic usage were similarly prevalent. Family and friends, along with teachers were common sources of information and play a significant role in providing information about menstruation.
Overall, analgesic usage did not provide sufficient relief to the majority of women taking it. Common NSAIDs, such as ibuprofen, naproxen and aspirin, are all superior to placebo for pain relief in primary dysmenorrhea, and there does not appear to be one particular type that is superior to others[52]. Paracetamol was the most common type of analgesic used by women in the included studies. This is a concern as paracetamol does not appear to be any more effective than a placebo[53] and is significantly less effective than NSAIDs [52] in reducing menstrual pain. This may explain why those women taking NSAIDs reported a much higher level of effectiveness compared to paracetamol. In the absence of prior medical consultation, adolescent self-medication has shown to lead to less frequent doses being taken resulting in sub-optimal pain relief[18, 54]. This is a serious concern as higher pain levels are strongly correlated with greater academic disruption[45].
The low usage of the oral contraceptive pill in the included studies is surprising, given that population surveys have shown an inverse relationship between contraceptive usage and self-reported period pain[55–57] and the combined oral contraceptive (COC) is commonly recommended as a second line of treatment for primary dysmenorrhea if NSAIDs have been unsuccessful [5, 58]. The reasons for the lower usage in LMIC may be influenced by cultural or religious factors, especially in young or unmarried women due to concerns that the COC promotes sexual promiscuity [12, 59]. Usage of COC in HIC was significantly higher, but still considerably lower than using analgesics, even though many women reported lack of effective pain relief with analgesics. This may at least in part stem from women’s concerns around long-term health consequences of the COC, or due to side effects [60, 61].
Rest was the most common non-pharmacological self-management strategy, with exercise, heat and herbal medicine being used by less than one in ten young women in the included studies. Exercise, especially low intensity exercise such as stretching or yoga, and heat are both effective self-management strategies for primary dysmenorrhea [13] and may be a useful alternative or adjunct to analgesic medications, especially in women who do not respond to analgesics.
Knowledge of dysmenorrhea from non-medical sources, such as family, friends and teachers were common. The normality of period pain may be reinforced by speaking to female family members (such as mothers or sisters) and peers as it is very likely that they will have had period pain[19, 62]. The concept of having to endure menstrual pain and symptoms as an integral part of female life is common amongst women with dysmenorrhea[6, 63–65], with even medical students not visiting their doctor when having period pain [66]. This is consistent with the concept that women “assemble” an idea of a normal period from their own experiences[67]. This normalisation of pain is likely to be a contributing factor to the usage of self-care rather than seeking medical intervention, leading to the low rates of visiting health professionals seen in the included studies.
There are a number of strengths in this systematic review and meta-analysis. We searched for articles across a range of databases and used dual data extraction via a pre-specified data extraction form to ensure rigorous data collection. Decisions on how to determine a country’s status used the four tier World Bank system[32] rather than the more simplified ‘developing’ or ‘developed’ bipartite classification. There are a number of limitations that must be acknowledged. First, we did not search in languages other than English, so there may be a number of non-English language papers that were not included. Second, there were significant inconsistences in reporting between surveys, especially with respect to the types of self-care used. Many surveys reported the use of regionally specific brand names for medications. While these were classified where possible, often information was not available in English. This may have resulted in under reporting the usage of specific medication types. Finally, the number of individual non-pharmacological self-care categories was limited to those which are commonly used in western countries and may not have represented the diversity of different self-care measures in different areas.
Since most young women do not seek medical advice, it would be prudent to ensure that the sources of advice they do consult; family, friends and teachers, as well as the young women themselves are suitably equipped. This could be achieved via well designed educational interventions; either delivered face to face, online or as a mixture of these. Teachers, in an Australian context particularly Health and Physical Education (HPE) teachers, can provide an effective means of providing all children and young people with the menstrual health literacy needed to manage menstruation and menstrual symptoms. With such a significant uptake of self-care options, teachers need to ensure they are informed on a range of effective complementary, traditional or non-pharmacological interventions to manage menstrual symptoms. Ideally this education on effective self-care would be given either prior to or approximating menarche, before the concept of period pain being ‘normal’ and needing to be ‘endured’ is firmly established in young women.
Conclusions
Dysmenorrhea was common amongst young women, and the majority of self-care was undertaken without medical advice. Use of paracetamol, a less effective analgesic in treating period pain, was common compared to ibuprofen or other types of NSAIDs. Less than half of young women reported that they received satisfactory relief from analgesics in general. The use of the oral contraceptive pill was very low amongst young women in LMIC, likely due to cultural or religious beliefs around its use. Educational interventions which discuss the effective use of NSAIDs, and the incorporation of effective non-pharmacological management strategies, such as using exercise and heat, should be offered as these are likely to reduce the negative impact of dysmenorrhea on young women.
Supporting information
(PDF)
PRISMA Checklist.
(DOC)
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Armour M, Parry K, Manohar N, Holmes K, Ferfolja T, Curry C, et al. The Prevalence and Academic Impact of Dysmenorrhea in 21,573 Young Women: A Systematic Review and Meta-Analysis. J Womens Health (Larchmt). 2019. Epub 2019/06/07. 10.1089/jwh.2018.7615 . [DOI] [PubMed] [Google Scholar]
- 2.Wong CL, Farquhar C, Roberts H, Proctor M. Oral contraceptive pill for primary dysmenorrhoea. Cochrane Database Syst Rev. 2009;(4):CD002120 Epub 2009/10/13. 10.1002/14651858.CD002120.pub3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coco AS. Primary dysmenorrhea. Am Fam Physician. 1999;60(2):489–96. Epub 1999/08/28. . [PubMed] [Google Scholar]
- 4.French L. Dysmenorrhea in adolescents: diagnosis and treatment. Paediatr Drugs. 2008;10(1):1–7. Epub 2007/12/29. 10.2165/00148581-200810010-00001 . [DOI] [PubMed] [Google Scholar]
- 5.Proctor M, Farquhar C. Diagnosis and management of dysmenorrhoea. BMJ. 2006;332(7550):1134–8. Epub 2006/05/13. 10.1136/bmj.332.7550.1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armour M, Dahlen HG, Smith CA. More Than Needles: The Importance of Explanations and Self-Care Advice in Treating Primary Dysmenorrhea with Acupuncture. Evid Based Complement Alternat Med. 2016;2016:3467067 Epub 2016/06/01. 10.1155/2016/3467067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med. 2000;154(12):1226–9. Epub 2000/12/15. . [DOI] [PubMed] [Google Scholar]
- 8.Wong LP. Attitudes towards dysmenorrhoea, impact and treatment seeking among adolescent girls: A rural school‐based survey. Australian Journal of Rural Health. 2011;19(4):218–23. 10.1111/j.1440-1584.2011.01213.x [DOI] [PubMed] [Google Scholar]
- 9.Yagnik AS. Reframing menstruation in India: metamorphosis of the menstrual taboo with the changing media coverage. Health Care Women Int. 2014;35(6):617–33. Epub 2013/11/05. 10.1080/07399332.2013.838246 . [DOI] [PubMed] [Google Scholar]
- 10.Kumar A, Srivastava K. Cultural and social practices regarding menstruation among adolescent girls. Soc Work Public Health. 2011;26(6):594–604. Epub 2011/09/22. 10.1080/19371918.2010.525144 . [DOI] [PubMed] [Google Scholar]
- 11.Ssewanyana D, Bitanihirwe BKY. Menstrual hygiene management among adolescent girls in sub-Saharan Africa. Glob Health Promot. 2019;26(1):105–8. Epub 2017/05/10. 10.1177/1757975917694597 . [DOI] [PubMed] [Google Scholar]
- 12.Hawkey AJ, Ussher JM, Perz J, Metusela C. Experiences and Constructions of Menarche and Menstruation Among Migrant and Refugee Women. Qual Health Res. 2017;27(10):1473–90. Epub 2016/10/16. 10.1177/1049732316672639 . [DOI] [PubMed] [Google Scholar]
- 13.Armour M, Smith CA, Steel KA, Macmillan F. The effectiveness of self-care and lifestyle interventions in primary dysmenorrhea: a systematic review and meta-analysis. BMC Complement Altern Med. 2019;19(1):22 Epub 2019/01/19. 10.1186/s12906-019-2433-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ortiz MI, Rangel-Flores E, Carrillo-Alarcon LC, Veras-Godoy HA. Prevalence and impact of primary dysmenorrhea among Mexican high school students. Int J Gynecol Obstet. 2009;107(3):240–3. Epub 2009/09/01. 10.1016/j.ijgo.2009.07.031 . [DOI] [PubMed] [Google Scholar]
- 15.Hillen TI, Grbavac SL, Johnston PJ, Straton JA, Keogh JM. Primary dysmenorrhea in young Western Australian women: prevalence, impact, and knowledge of treatment. J Adolesc Health. 1999;25(1):40–5. Epub 1999/07/27. 10.1016/s1054-139x(98)00147-5 . [DOI] [PubMed] [Google Scholar]
- 16.Johnson J. Level of knowledge among adolescent girls regarding effective treatment for dysmenorrhea. J Adolesc Health Care. 1988;9(5):398–402. Epub 1988/09/01. . [DOI] [PubMed] [Google Scholar]
- 17.Klein JR, Litt IF. Epidemiology of adolescent dysmenorrhea. Pediatrics. 1981;68(5):661–4. Epub 1981/11/01. . [PubMed] [Google Scholar]
- 18.Campbell MA, McGrath PJ. Use of medication by adolescents for the management of menstrual discomfort. Arch Pediatr Adolesc Med. 1997;151(9):905–13. Epub 1997/10/06. . [DOI] [PubMed] [Google Scholar]
- 19.Chang SF, Chuang MH. Factors that affect self-care behaviour of female high school students with dysmenorrhoea: a cluster sampling study. Int J Nurs Pract. 2012;18(2):117–24. Epub 2012/03/23. 10.1111/j.1440-172X.2012.02007.x . [DOI] [PubMed] [Google Scholar]
- 20.Wong LP, Khoo EM. Dysmenorrhea in a multiethnic population of adolescent Asian girls. Int J Gynaecol Obstet. 2010;108(2):139–42. Epub 2009/12/01. 10.1016/j.ijgo.2009.09.018 . [DOI] [PubMed] [Google Scholar]
- 21.Ortiz MI, Fernandez-Martinez E, Perez-Hernandez N, Macias A, Rangel-Flores E, Ponce-Monter H. Patterns of prescription and self-medication for treating primary dysmenorrhea in a Mexican population. Proc West Pharmacol Soc. 2007;50:165–7. Epub 2008/07/09. . [PubMed] [Google Scholar]
- 22.Chia CF, Lai JH, Cheung PK, Kwong LT, Lau FP, Leung KH, et al. Dysmenorrhoea among Hong Kong university students: prevalence, impact, and management. Hong Kong Med J. 2013;19(3):222–8. Epub 2013/04/10. 10.12809/hkmj133807 . [DOI] [PubMed] [Google Scholar]
- 23.MacKichan F, Paterson C, Henley WE, Britten N. Self-care in people with long term health problems: a community based survey. BMC Fam Pract. 2011;12:53 Epub 2011/06/22. 10.1186/1471-2296-12-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan A, Wilson S, Taylor A, Greenfield S. Factors associated with self-care activities among adults in the United Kingdom: a systematic review. BMC Public Health. 2009;9:96 Epub 2009/04/07. 10.1186/1471-2458-9-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen CH, Lin YH, Heitkemper MM, Wu KM. The self-care strategies of girls with primary dysmenorrhea: a focus group study in Taiwan. Health Care Women Int. 2006;27(5):418–27. Epub 2006/08/01. 10.1080/07399330600629583 . [DOI] [PubMed] [Google Scholar]
- 26.Schoep ME, Adang EMM, Maas JWM, De Bie B, Aarts JWM, Nieboer TE. Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. BMJ Open. 2019;9(6):e026186 10.1136/bmjopen-2018-026186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015;(7):CD001751 Epub 2015/08/01. 10.1002/14651858.CD001751.pub3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matthewman G, Lee A, Kaur JG, Daley AJ. Physical activity for primary dysmenorrhea: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2018. Epub 2018/04/10. 10.1016/j.ajog.2018.04.001 . [DOI] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12. Epub 2009/07/28. 10.1016/j.jclinepi.2009.06.005 . [DOI] [PubMed] [Google Scholar]
- 30.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414 Epub 2014/12/24. 10.1136/bmjopen-2014-006414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Resurreccion DM, Motrico E, Rigabert A, Rubio-Valera M, Conejo-Ceron S, Pastor L, et al. Barriers for Nonparticipation and Dropout of Women in Cardiac Rehabilitation Programs: A Systematic Review. J Womens Health (Larchmt). 2017;26(8):849–59. Epub 2017/04/08. 10.1089/jwh.2016.6249 . [DOI] [PubMed] [Google Scholar]
- 32.World Bank. World Bank Country and Lending Groups 2018. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 33.Abidoye RO, Agbabiaka BA. Incidence and management of menstrual disorders and foods implicated among Nigerian adolescents. International Journal of Adolescence and Youth. 1994;4(3/4):271–83. ; 23857. [Google Scholar]
- 34.Adinma ED, Adinma JI. Perceptions and practices on menstruation amongst Nigerian secondary school girls. African journal of reproductive health. 2008;12(1):74–83. Epub 2008/04/01. . [PubMed] [Google Scholar]
- 35.Saka J OO-M, Nneka O, Saka A-O, Omolola D-O, Rabiyyah H-A. Primary dysmenorrhea among the adolescents in Kwara state, Nigeria: The prevalence, knowledge and management. Nursing Practice Today. 2018;VOL 5 (4: AUTUMN):395–402. Epub 13 October 2018. [Google Scholar]
- 36.Sule ST, Ukwenya JE. Menstrual Experiences of Adolescents in a Secondary School. J Turk-Ger Gynecol A. 2007;8(1):7–14. WOS:000420580900001. [Google Scholar]
- 37.Abraham S, Fraser I, Gebski V, Knight C, Llewellyn-Jones D, Mira M, et al. Menstruation, menstrual protection and menstrual cycle problems. The knowledge, attitudes and practices of young Australian women. Med J Aust. 1985;142(4):247–51. Epub 1985/02/18. . [PubMed] [Google Scholar]
- 38.Subasinghe AK, Happo L, Jayasinghe YL, Garland SM, Gorelik A, Wark JD. Prevalence and severity of dysmenorrhoea, and management options reported by young Australian women. Aust Fam Physician. 2016;45(11):829–34. Epub 2016/11/03. . [PubMed] [Google Scholar]
- 39.Poureslami M, Osati-Ashtiani F. Attitudes of female adolescents about dysmenorrhea and menstrual hygiene in Tehran suburbs. Archives of Iranian Medicine. 2002;5(4):219–24. [Google Scholar]
- 40.Rostami M. The study of dysmenorrhea in high school girls. Pak J Med Sci. 2007;23(6):928–31. WOS:000254518700023. [Google Scholar]
- 41.Ghaderi F, Asghari Jafarabadi M, Mohseni Bandpei MA. Dysmenorrhea and self-care strategies in Iranian female students: a regression modeling of pain severity and underlying factors. Int J Adolesc Med Health. 2016;29(6). Epub 2016/07/19. 10.1515/ijamh-2016-0017 . [DOI] [PubMed] [Google Scholar]
- 42.Moronkola OA, Uzuegbu VU. Menstruation: symptoms, management and attitude of female nursing students in Ibadan, Nigeria. African journal of reproductive health. 2006;10(3):84–9. Epub 2007/05/24. . [PubMed] [Google Scholar]
- 43.Chiou MH, Wang HH. Predictors of dysmenorrhea and self-care behavior among vocational nursing school female students. The journal of nursing research: JNR. 2008;16(1):17–25. [DOI] [PubMed] [Google Scholar]
- 44.Soderman L, Edlund M, Marions L. Prevalence and impact of dysmenorrhea in Swedish adolescents. Acta Obstet Gynecol Scand. 2019;98(2):215–21. Epub 2018/10/13. 10.1111/aogs.13480 . [DOI] [PubMed] [Google Scholar]
- 45.Wijesiri HS, Suresh TS. Knowledge and attitudes towards dysmenorrhea among adolescent girls in an urban school in Sri Lanka. Nursing & health sciences. 2013;15(1):58–64. Epub 2012/12/01. 10.1111/j.1442-2018.2012.00736.x . [DOI] [PubMed] [Google Scholar]
- 46.Alsaleem MA. Dysmenorrhea, associated symptoms, and management among students at King Khalid University, Saudi Arabia: An exploratory study. J Family Med Prim Care. 2018;7(4):769–74. Epub 2018/09/21. 10.4103/jfmpc.jfmpc_113_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong CL, Ip WY, Choi KC, Lam LW. Examining Self-Care Behaviors and Their Associated Factors Among Adolescent Girls With Dysmenorrhea: An Application of Orem's Self-Care Deficit Nursing Theory. J Nurs Scholarsh. 2015;47(3):219–27. Epub 2015/03/25. 10.1111/jnu.12134 . [DOI] [PubMed] [Google Scholar]
- 48.Devi UT. A Study on Coping Strategies of Menstrual Disturbances among Adolescent Girls at Selected Schools of Coimbatore District. Asian Journal of Nursing Education and Research. 2014;4(2):220–3. . [Google Scholar]
- 49.Ameade EPK, Amalba A, Mohammed BS. Prevalence of dysmenorrhea among University students in Northern Ghana; its impact and management strategies. BMC Womens Health. 2018;18(1):39 Epub 2018/02/13. 10.1186/s12905-018-0532-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yesuf TA, Eshete NA, Sisay EA. Dysmenorrhea among University Health Science Students, Northern Ethiopia: Impact and Associated Factors. Int J Reprod Med. 2018;2018:9730328 Epub 2018/04/04. 10.1155/2018/9730328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pitangui AC, Gomes MR, Lima AS, Schwingel PA, Albuquerque AP, de Araujo RC. Menstruation disturbances: prevalence, characteristics, and effects on the activities of daily living among adolescent girls from Brazil. J Pediatr Adolesc Gynecol. 2013;26(3):148–52. Epub 2013/03/20. 10.1016/j.jpag.2012.12.001 . [DOI] [PubMed] [Google Scholar]
- 52.Marjoribanks J, Proctor M, Farquhar C, Derks RS. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2010;(1):CD001751 Epub 2010/01/22. 10.1002/14651858.CD001751.pub2 . [DOI] [PubMed] [Google Scholar]
- 53.Zhang WY, Li Wan Po A. Efficacy of minor analgesics in primary dysmenorrhoea: a systematic review. Br J Obstet Gynaecol. 1998;105(7):780–9. Epub 1998/08/06. . [DOI] [PubMed] [Google Scholar]
- 54.O'Connell K, Davis AR, Westhoff C. Self-treatment patterns among adolescent girls with dysmenorrhea. J Pediatr Adolesc Gynecol. 2006;19(4):285–9. Epub 2006/07/29. 10.1016/j.jpag.2006.05.004 . [DOI] [PubMed] [Google Scholar]
- 55.Grandi G, Ferrari S, Xholli A, Cannoletta M, Palma F, Romani C, et al. Prevalence of menstrual pain in young women: what is dysmenorrhea? J Pain Res. 2012;5:169–74. Epub 2012/07/14. 10.2147/JPR.S30602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Santer M, Warner P, Wyke S. A Scottish postal survey suggested that the prevailing clinical preoccupation with heavy periods does not reflect the epidemiology of reported symptoms and problems. J Clin Epidemiol. 2005;58(11):1206–10. Epub 2005/10/15. 10.1016/j.jclinepi.2005.02.026 . [DOI] [PubMed] [Google Scholar]
- 57.Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332(7544):749–55. Epub 2006/02/18. 10.1136/bmj.38748.697465.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zahradnik HP, Hanjalic-Beck A, Groth K. Nonsteroidal anti-inflammatory drugs and hormonal contraceptives for pain relief from dysmenorrhea: a review. Contraception. 2010;81(3):185–96. Epub 2010/02/18. 10.1016/j.contraception.2009.09.014 . [DOI] [PubMed] [Google Scholar]
- 59.Metusela C, Ussher J, Perz J, Hawkey A, Morrow M, Narchal R, et al. "In My Culture, We Don't Know Anything About That": Sexual and Reproductive Health of Migrant and Refugee Women. Int J Behav Med. 2017;24(6):836–45. Epub 2017/06/18. 10.1007/s12529-017-9662-3 . [DOI] [PubMed] [Google Scholar]
- 60.Hendrix SL, Alexander NJ. Primary dysmenorrhea treatment with a desogestrel-containing low-dose oral contraceptive. Contraception. 2002;66(6):393–9. Epub 2002/12/25. . [DOI] [PubMed] [Google Scholar]
- 61.O'Connell K, Davis AR, Kerns J. Oral contraceptives: side effects and depression in adolescent girls. Contraception. 2007;75(4):299–304. Epub 2007/03/17. 10.1016/j.contraception.2006.09.008 . [DOI] [PubMed] [Google Scholar]
- 62.Zhu X, Wong F, Bensoussan A, Lo SK, Zhou C, Yu J. Are there any cross-ethnic differences in menstrual profiles? A pilot comparative study on Australian and Chinese women with primary dysmenorrhea. J Obstet Gynaecol Res. 2010;36(5):1093–101. Epub 2010/09/18. 10.1111/j.1447-0756.2010.01250.x . [DOI] [PubMed] [Google Scholar]
- 63.Scambler A, Scambler G. Menstrual symptoms, attitudes and consulting behaviour. Soc Sci Med. 1985;20(10):1065–8. Epub 1985/01/01. . [DOI] [PubMed] [Google Scholar]
- 64.Cronje HS, Kritzinger IE. Menstruation: symptoms, management and attitudes in university students. Int J Gynaecol Obstet. 1991;35(2):147–50. Epub 1991/06/01. . [DOI] [PubMed] [Google Scholar]
- 65.Brantelid IE, Nilver H, Alehagen S. Menstruation during a lifespan: A qualitative study of women's experiences. Health Care Women Int. 2014;35(6):600–16. Epub 2013/12/10. 10.1080/07399332.2013.868465 . [DOI] [PubMed] [Google Scholar]
- 66.Singh A, Kiran D, Singh H, Nel B, Singh P, Tiwari P. Prevalence and severity of dysmenorrhea: a problem related to menstruation, among first and second year female medical students. Indian J Physiol Pharmacol. 2008;52(4):389–97. Epub 2009/07/10. . [PubMed] [Google Scholar]
- 67.Wood JM, Barthalow Koch P, Mansfield PK. Is my period normal? How college-aged women determine the normality or abnormality of their menstrual cycles. Women Health. 2007;46(1):41–56. Epub 2007/11/23. 10.1300/J013v46n01_04 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
PRISMA Checklist.
(DOC)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.


