Abstract
Importance:
African American individuals face higher atherosclerotic cardiovascular disease (ASCVD) risk than Caucasians; reasons for these differences, including potential differences in patient beliefs regarding preventive care, remain unknown.
Objectives:
Evaluate racial differences in statin utilization and the potential causes for any observed differences.
Design:
Using the 2015 Patient and Provider Assessment of Lipid Management (PALM) Registry data, we compared statin use and dosing between African American and Caucasian outpatient adults potentially eligible for primary or secondary prevention statins.
Setting:
138 United States community practices.
Participants:
5,689 patients (806, 14% African American) eligible for statin therapy in PALM.
Main Outcomes and Measures:
Primary outcomes were use and dosing of statin therapy according to the 2013 ACC/AHA guideline by race. Secondary outcomes included lipid levels and patient-reported beliefs. Poisson regression was used to evaluate the association between race and statin under-treatment (i.e., not on a statin or on a less-than-recommended intensity).
Results:
Among 5,689 patients (806, 14% African American) eligible for statin therapy in PALM, African Americans were less likely than Caucasians to be treated with a statin (71% vs. 75%, p=0.02). Among those treated, African Americans were less likely to receive a statin at the 2013 ACC/AHA guideline-recommended intensity (33% vs. 44%, p<0.001). Median on-treatment low-density lipoprotein cholesterol (LDL-C) levels were higher among African Americans than Caucasians (97 vs. 85 mg/dL, p<0.001). Compared with Caucasians, African Americans were less likely to believe statins were safe (36% vs. 57%, p<0.001) or effective (70% vs. 74%, p=0.008), and were less likely to trust their clinician (87% vs. 95%, p<0.001). The RR for statin under-treatment (i.e., not on a statin or on a less-than-recommended intensity) for African Americans, adjusted for demographics and clinical characteristics was 1.07 (95% CI 1.00–1.15, p=0.05). Racial differences in statin undertreatment were not significant after adjusting for demographic, clinical, socioeconomic status, patient beliefs, and provider factors (final adjusted RR 1.03, 95% CI 0.96–1.11, p=0.35).
Conclusions and Relevance:
African Americans were less likely to receive 2013 ACC/AHA guideline-recommended statin therapy and had higher on-treatment LDL-C levels, though this association was not significant after adjustment for confounders. Differences in demographic, clinical, socioeconomic, patient belief, and provider factors all contributed to observed treatment differences and represent important potential targets for intervention.
Keywords: race, African American, statins, lipids, prevention, risk
The benefits of statin therapy for both primary and secondary prevention are well-established (1–3). African Americans have a higher risk for atherosclerotic cardiovascular disease (ASCVD) than Caucasians (4). Part of the explanation for this increased risk may be due to undertreatment of African Americans for primary prevention. Several studies have shown that African American individuals are less likely to receive statin therapy when indicated relative to Caucasians (5, 6). Nevertheless, the reasons for these racial differences in lipid management remain incompletely understood.
The Patient and Provider Assessment of Lipid Management (PALM) Registry is a large, contemporary, national registry conducted at 138 geographically diverse primary care, cardiology, and endocrinology United States community practices. Beyond collecting detailed clinical, socioeconomic, and core lab lipid data, PALM assessed patient perceptions of personal cardiovascular disease risk, beliefs regarding statin efficacy and safety, and trust in their clinician—all of which have been associated with treatment use and adherence (7). In this study, we: 1) compared overall statin use and use of guideline-recommended statin intensity for African American and Caucasian individuals; 2) examined racial differences in patient perceptions of ASCVD risk, statin efficacy and safety, and trust in their clinicians; and 3) determined whether differences in guideline-recommended statin use persisted after adjustment for demographics, clinical characteristics, socioeconomic status, patient beliefs, and provider characteristics.
Methods
Data Description and Outcomes of Interest: PALM
PALM is a nationwide registry of patients with ASCVD or at high risk for ASCVD at 138 primary care, cardiology, and endocrinology practices (n=7,736) that enrolled patients between May 2015 and November 2015 (7). Patient clinical data (comorbidities, medication use, demographics) and current statin use were abstracted from the medical record by study coordinators at each site (7). Patient surveys were conducted to determine self-reported race, education level, socioeconomic status, and patient beliefs about statins, cholesterol, ASCVD, and clinician trust. Surveys were administered on an iPAD as patients were waiting to be seen in clinic after informed consent was obtained (7). Patient numeracy was assessed using the subjective numeracy score (8, 9). Self-reported income was missing for 1,725 (31%) patients. Missing income data were imputed using 2014 median census household income from the Area Health Resource Files from hrsa.gov based on patient residence zip code or the enrolling site zip code. Core laboratory lipid panels were measured for all patients. Providers in clinics participating in the PALM Registry also completed surveys prior to patient enrollment assessing their self-reported treatment patterns and the primary guideline that they used.
All participants were asked to complete the survey at enrollment (response rate 95.3%); those who did not complete the survey were not eligible for inclusion. In this analysis, we included all patients recommended for statin therapy (n=5,689) based on the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults (1) who were either African American (n=806, 14%) or Caucasian (n=4,883, 86%). Race and ethnicity were both self-reported; 4.6% of African Americans, 12.1% of Caucasians self-identified as Hispanic. Other races were excluded from the analysis, including those who self-identified as Asian (n=112, 1.9%), American Indian/Alaskan Native (n=9, 0.2%), and Native Hawaiian/Pacific Islanders (n=8, 0.1%). Participants were classified as eligible for high-intensity statin therapy per guideline recommendations: 1) clinical ASCVD defined as coronary artery disease (prior myocardial infarction, obstructive coronary artery disease, coronary artery bypass grafting, or percutaneous coronary intervention), cerebrovascular disease (prior transient ischemic attack or stroke), other ASCVD (peripheral arterial disease, abdominal aortic aneurysm, non-coronary arterial revascularization, and carotid stenosis), and aged ≤75 years; 2) low-density lipoprotein cholesterol (LDL-C) ≥190 mg/dL; or 3) diabetes with 10-year ASCVD risk ≥7.5% based on pooled cohort risk equation and aged 40–75 years with LDL-C ≥70 mg/dL (1). We also considered adults aged 40–75 with diabetes and predicted 10-year risk of 7.5% or higher who were on a statin at the time of enrollment eligible for high-intensity statin therapy, regardless of their LDL-C. Participants were eligible for moderate-intensity statin therapy if they did not meet any indication for a high-intensity statin and met one of the following criteria: 1) clinical ASCVD and aged >75 years; 2) diabetes with 10-year ASCVD risk <7.5% and aged 40–75 years with LDL-C ≥70mg/dL or already on a statin; or 3) 10-year risk ≥7.5% and no diabetes, aged 40–75 years with LDL-C ≥70mg/dL or already on a statin. Statin undertreatment was defined as: 1) patients meeting the recommendation for a statin, but not being treated; 2) patients recommended for high-intensity statin, but treated with a moderate/low statin dose; or 3) patients recommended for a moderate-intensity statin, but treated with a low-intensity statin.
Statistical Analysis
Statin treatment patterns (not on statin, on lower than appropriate statin, and on appropriate statin) were evaluated by race within the overall population and by indication (primary and secondary prevention). Differences in the frequency of appropriate statin treatment were assessed by race. Patient demographics, socioeconomic status, clinical and laboratory values, prior statin experience and beliefs about statins, cholesterol, and cardiovascular disease were evaluated by race overall and by indication (primary vs. secondary prevention). Categorical variables were presented as frequencies and differences assessed using the chi-square test when the sample size was sufficient, otherwise an exact test was used. Continuous variables were presented as a median (interquartile range) and compared using the Wilcoxon rank-sum test. A p-value of less than 0.05 indicated that the summary measures (i.e., distribution for continuous variables and proportions for categorical variables) differed by analytic group.
We evaluated the degree to which racial differences in statin utilization among African American and Caucasian populations were due to demographic, clinical, socioeconomic, patient beliefs, and provider factors using sequential multivariable modeling of the association between race and the risk of under-treatment (receiving no statin or less-than-recommended statin intensity) using Poisson regression with generalized estimating equation (GEE) to account for clustering at the site level. First, univariable analysis using race alone (Model 1) was performed to evaluate the unadjusted relative risk between race and undertreatment. Next, the following sequential models were created to evaluate how the relative risk of African American race and statin undertreatment changed when adjusted for possible explanatory factors: Model 2 included age and sex; Model 3 further adjusted for clinical characteristics including prior ASCVD (grouped into coronary heart disease, cerebrovascular disease, and other ASCVD), diabetes, obesity, smoking, and hypertension. Model 4 further adjusted for socioeconomic factors such as yearly income, insurance status, education level, and numeracy score; and Model 5 added in patient beliefs and perceptions including worry about heart disease, clinician trust, beliefs about statin safety and effectiveness, and beliefs about high cholesterol and heart attack risk. Finally, in addition to demographic, clinical, socioeconomic, and patient belief factors, Model 6 included provider factors including provider type (cardiologist vs. non-cardiologist), whether the patient’s provider reported using the 2013 ACC/AHA guideline as their primary resource for lipid management in the provider survey, and clinic setting (urban vs. rural). Nearly all patients had information from the provider survey; however, 35 of 5,689 patients were excluded from the model due to lack of provider information. An additional 40 patients were excluded from the modeling due to lack of information on current statin use. When covariate data were missing for the regression analysis (with the exception of income data as described above) multiple imputation was used, employing the generalized estimating equation method with exchangeable working correlation structure to account for clustering of patients within-site (eTable1). Sensitivity analysis of the multivariable modeling was performed to assess the impact of missing data by re-running the models with multiple imputation, simple imputation and excluding missing data and the results were similar. Finally, in order to determine the relative impact of individual risk factor groups, multivariable modeling of the association between under-treatment and race adjusting for individual confounder groups using Poisson regression was performed for demographic, clinical, socioeconomic, patient belief, and provider factors (eFigure 1).
Results
Among 5,689 patients with a 2013 ACC/AHA guideline indication for statin therapy, 806 (14%) were African American. Table 1 compares the baseline characteristics for African American vs. Caucasian patients with stratification by primary and secondary prevention groups. African American participants were more likely to be younger, female, have diabetes, smoke, and a higher body mass index, were less likely to have had prior ASCVD, but had a higher predicted 10-year ASCVD risk in primary prevention patients. African American individuals more frequently had a history of hypertension and had higher median systolic blood pressures than Caucasians. African American patients also had lower income, educational levels, and subjective numeracy scales, and were more likely to have Medicare than Caucasians. African Americans were less likely to report seeing a cardiologist, but were more likely to report seeing an endocrinologist annually. Providers seen by African American participants were also less likely to report using the 2013 ACC/AHA guideline as their primary guideline. Caucasians who received a statin were more likely than African Americans to stop their statin due to side effects (5.7% vs. 2.9%, p=0.005).
Table 1.
Demographic, Clinical, and Belief Differences in African American vs. Caucasian Adults in PALM
| Overall (n=5689) | Primary Prevention (n=2482) | Secondary Prevention (n=3207) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| African American (n=806) |
Caucasian (n=4883) |
p-value | African American (n=450) |
Caucasian (n=2032) |
p-value | African American (n=356) |
Caucasian (n=2851) |
p-value | |
| Clinical and demographic factors | |||||||||
| Age (years) | 64.0 (57.0–70.0) | 68.0 (62.0–74.0) | <0.001 | 62.0 (55.0–68.0) | 66.0 (60.0–71.0) | <.001 | 67.0 (58.0–73.0) | 71.0 (64.0–78.0) | <0.001 |
| Sex (% female) | 436 (54.1%) | 2,020 (41.4%) | <0.001 | 249 (55.3%) | 1,040 (51.2%) | 0.11 | 187 (52.5%) | 980 (34.4%) | <0.001 |
| ASCVDa | 356 (44.2%) | 2,851 (58.4%) | <0.001 | N/A | N/A | 100 | 100 | ||
| Coronary heart diseaseb | 270 (33.5%) | 2,382 (48.8%) | <0.001 | 270 (75.8%) | 2,382 (83.5%) | <0.001 | |||
| Cerebrovascular diseasec | 71 (8.8%) | 420 (8.6%) | 0.85 | 71 (19.9%) | 420 (14.7%) | 0.01 | |||
| Other ASCVDd | 124 (15.4%) | 937 (19.2%) | 0.01 | 124 (34.8%) | 937 (32.9%) | 0.46 | |||
| Diabetes | 481 (59.7%) | 2,050 (42.0%) | <0.001 | 280 (62.2%) | 986 (48.5%) | <0.001 | 201 (56.5%) | 1,064 (37.3%) | <0.001 |
| HTN | 717 (89.0%) | 3,923 (80.3%) | <0.001 | 384 (85.3%) | 1,521 (74.9%) | <0.001 | 333 (93.5%) | 2,402 (84.3%) | <0.001 |
| Chronic kidney disease | 97 (12.0%) | 492 (10.1%) | 0.09 | 35 (7.8%) | 135 (6.6%) | 0.39 | 62 (17.4%) | 357 (12.5%) | 0.01 |
| BMI | 31.6 (27.3–37.0) | 29.9 (26.3–34.3) | <0.001 | 31.8 (28.1–37.4) | 30.6 (27.1–35.5) | <0.001 | 31.2 (26.5–36.3) | 29.3 (25.8–33.6) | <0.001 |
| Smoking | 134 (17.8%) | 520 (10.8%) | <0.001 | 68 (16.8%) | 235 (11.7%) | <0.001 | 66 (18.9%) | 285 (10.1%) | <0.001 |
| 10-year riske(among those without known ASCVD) | 16.2 (10.4–25.3) | 14.0 (9.2–21.2) | <0.001 | 16.2 (10.4–25.3) | 14.0 (9.2–21.2) | <0.001 | N/A | N/A | |
| Total cholesterol | 179.0 (152.0–212.0) | 167.0 (141.0–198.0) | <0.001 | 184.0 (158.0–212.0) | 180.0 (155.0–212.5) | 0.36 | 171.0 (143.0–209.0) | 156.0 (135.0–186.0) | <0.001 |
| LDL-C | 104.0 (82.0–131.0) | 92.0 (72.0–119.0) | <0.001 | 110.0 (87.0–133.0) | 103.0 (82.5–130.0) | 0.03 | 95.0 (75.0–127.0) | 84.0 (67.0–108.0) | <0.001 |
| HDL-C (core lab) | 55.0 (45.0–66.0) | 50.0 (42.0–61.0) | <0.001 | 55.0 (45.0–67.0) | 52.0 (43.0–64.0) | <0.001 | 54.0 (45.0–65.0) | 49.0 (41.0–59.0) | <0.001 |
| % LDL-C <70 mg/dL | 107 (14.0%) | 1,045 (21.8%) | <0.001 | 49 (10.9%) | 267 (13.1%) | 0.20 | 58 (18.4%) | 778 (28.2%) | <0.001 |
| Systolic BP | 131.0 (122.0–145.0) | 128.0 (119.0–140.0) | <0.001 | 134.0 (124.0–147.0) | 130.0 (120.0–140.0) | <0.001 | 130.0 (120.0–140.0) | 128.0 (118.0–140.0) | <0.001 |
| Socioeconomic factors | |||||||||
| Insurancef | |||||||||
| % private | 356 (48.0%) | 2,933 (60.9%) | <0.001 | 200 (50.5%) | 1,243 (61.9%) | <0.001 | 156 (45.1%) | 1,690 (60.2%) | <0.001 |
| % Medicare | 395 (53.2%) | 3,047 (63.2%) | <0.001 | 184 (46.5%) | 1,118 (55.7%) | <0.001 | 211 (61.0%) | 1,929 (68.6%) | 0.004 |
| % Medicaid | 162 (21.8%) | 455 (9.4%) | <0.001 | 76 (19.2%) | 187 (9.3%) | <0.001 | 86 (24.9%) | 268 (9.5%) | <0.001 |
| % other | 26 (3.5%) | 106 (2.2%) | 0.03 | 15 (3.8%) | 33 (1.6%) | 0.005 | 11 (3.2%) | 73 (2.6%) | 0.53 |
| % no insurance | 20 (2.7%) | 102 (2.1%) | 0.32 | 12 (3.0%) | 63 (3.1%) | 0.91 | 8 (2.3%) | 39 (1.4%) | 0.18 |
| Education (% some college or above)g | 395 (54.0%) | 3,095 (64.2%) | <0.001 | 207 (53.6%) | 1,294 (64.5%) | <0.001 | 188 (54.5%) | 1,801 (64.0%) | <0.001 |
| Subjective numeracy scoreg, h | 12.0 (8.0–18.0) | 17.0 (12.0–21.0) | <0.001 | 13.0 (8.0–18.0) | 17.0 (12.0–21.0) | <0.001 | 12.0 (8.0–18.0) | 17.0 (12.0–22.0) | <0.001 |
| Income | <0.001 | <0.001 | <0.001 | ||||||
| <35000 | 256 (55.3%) | 1,106 (33.9%) | 127 (52.0%) | 466 (32.1%) | 129 (58.9%) | 640 (35.4%) | |||
| 35–75 | 123 (26.6%) | 1,112 (34.1%) | 68 (27.9%) | 512 (35.2%) | 55 (25.1%) | 600 (33.2%) | |||
| 75–100 | 33 (7.1%) | 383 (11.7%) | 20 (8.2%) | 176 (12.1%) | 13 (5.9%) | 207 (11.4%) | |||
| ≥100 | 51 (11.0%) | 661 (20.3%) | 29 (11.9%) | 299 (20.6%) | 22 (10.0%) | 362 (20.0%) | |||
| Provider factors | |||||||||
| Urban provider (%) | 704 (87.3%) | 4,415 (90.8%) | 0.002 | 394 (87.6%) | 1,825 (90.4%) | 0.07 | 310 (87.1%) | 2,590 (91.2%) | 0.01 |
| Cardiologist vs. non-cardiologisti | 212 (27.2%) | 1,840 (38.4%) | <0.001 | 53 (12.1%) | 302 (15.2%) | 0.10 | 159 (46.5%) | 1,538 (55.0%) | 0.003 |
| Cardiologist seen at least once per year | 377 (50.4%) | 2,943 (61.0%) | <0.001 | 114 (28.4%) | 596 (29.7%) | 0.59 | 263 (76.0%) | 2,347 (83.2%) | <0.001 |
| Endocrinologist seen at least once per year | 199 (26.6%) | 849 (17.6%) | <0.001 | 105 (26.2%) | 388 (19.3%) | 0.002 | 94 (27.2%) | 461 (16.3%) | <0.001 |
| 2013 ACC/AHA guideline as primary guideline (%)j | 443 (59.4%) | 2,818 (64.9%) | 0.004 | 194 (46.4%) | 1,061 (59.2%) | <0.001 | 249 (75.9%) | 1,757 (68.8%) | 0.009 |
| Stopped statin due to side effects (%)k | 17 (2.9%) | 248 (5.7%) | 0.005 | 4 (1.4%) | 100 (6.8%) | <0.001 | 13 (4.4%) | 131 (5.1%) | 0.61 |
Abbreviations: ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index; BP, blood pressure; HDL-C, high-density lipoprotein cholesterol; HTN, hypertension; LDL-C, low-density lipoprotein cholesterol; PALM, Patient and Provider Assessment of Lipid Management Registry; Q1-Q3, quarter 1 through quarter 3.
Categorical variables were presented as “n” (percentage); differences by race were assessed using the Chi-Square test when the sample size was sufficient, otherwise an exact test was used. Continuous variables were presented as a median (interquartile range) and compared using the Wilcoxon rank-sum test.
ASCVD = prior MI, coronary artery disease, coronary artery bypass grafting, percutaneous coronary intervention, stroke, abdominal aortic aneurysm, peripheral arterial disease, carotid artery stenosis, or non-coronary arterial revascularization
Coronary heart disease = prior myocardial infarction, coronary artery disease; corMI, CAD, CABG, and PCI
Cerebrovascular disease = prior TIA or stroke
Other ASCVD = AAA, PAD, non-coronary arterial revascularization and carotid stenosis
10-year risk estimated using the pooled cohort equation (1).
Insurance: “other” includes all answers that are not “no”, “private”, “Medicare” or “Medicaid”
Education level and income are by patient report.
Subjective numeracy score as described previously (8, 9).
Cardiologist vs. non-cardiologist denotes whether the patient’s PALM Registry provider was a cardiologist or not.
2013 ACC/AHA Guideline as primary guideline (%) refers to the % of patients whose primary provider listed the 2013 ACC/AHA Cholesterol Guideline as their primary reference guiding cholesterol treatment.
The stopped statin due to side effects (%) refers to the % of all patients who were ever on a statin in that given sub-group
Statin Use and Dosing Intensity
African Americans were modestly less likely than Caucasians to be treated with any statin (71% vs. 75%, p=0.02), or to be treated with a statin at the guideline-recommended intensity (33% vs. 44%, p<0.001); Figure 1. In the overall sample, as well as among those on statin therapy, African Americans had higher LDL-C levels than Caucasians (median 104.0 vs. 92.0, p<0.001 overall, median 97.0 vs. 85.0, p<0.001 among those on statins); Figure 2.
Figure 1. Statin Utilization in African American vs. Caucasian Patients.

Statin treatment and guideline-recommended statin treatment in African Americans vs. Caucasians are presented here, categorized by overall, primary prevention, and secondary prevention sub-groups.
Figure 2. LDL-C Levels Overall and On-treatment in African American vs. Caucasian Patients.
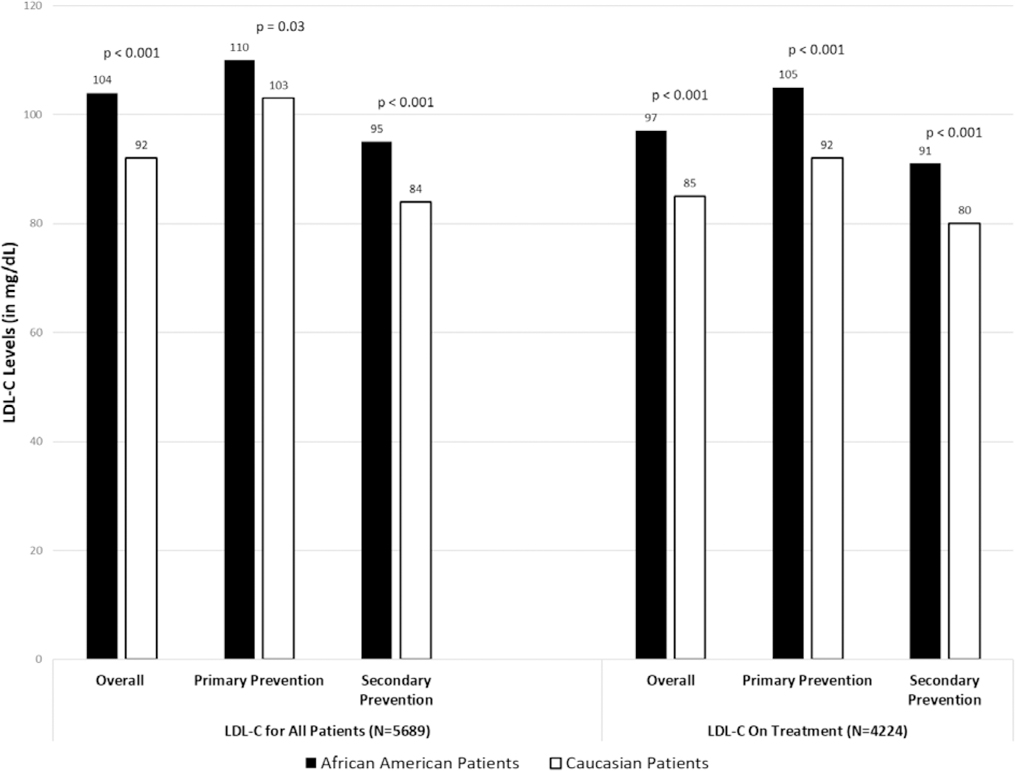
LDL-C levels for all patients and only on-treatment patients are presented here for African Americans vs. Caucasians, categorized by overall, primary prevention and secondary prevention sub-groups.
Abbreviations: LDL-C, low-density lipoprotein cholesterol
Patient Perceptions and Beliefs
African Americans and Caucasians had different perceptions and beliefs about statins, cholesterol, and cardiovascular disease (Table 2). Among those with ASCVD, African Americans were more likely to report worrying about heart disease than Caucasians (13.4% vs. 9.4% worry often about heart attack or stroke, p=0.005). In contrast, African Americans were less likely to report that they perceived their risk of cardiovascular disease to be higher (worse) than their peers (28.6% vs. 36.2, p<0.001). African Americans were less likely to believe statins are effective (70.0% vs. 74.4%, p=0.008) or safe (36.2% vs. 57.3%, p<0.001), and were less likely to trust their clinician than Caucasians (87.0% vs. 94.7%, p<0.001).
Table 2.
Racial Differences in Patient Beliefs about Statins, Cholesterol, and Heart Disease in African American vs. Caucasian Adultsa
| Survey Question | Overall (n=5689) | Primary Prevention (n=2482) | Secondary Prevention (n=3207) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| African American |
Caucasian | p-value | African American |
Caucasian | p-value | African American |
Caucasian | p-value | |
| Worry about disease and cholesterolb | |||||||||
| How often do you think or worry that you may have a heart attack or stroke? (%) | 0.005 | 0.23 | 0.001 | ||||||
| Often | 90 (13.4%) | 433 (9.4%) | 32 (9.0%) | 123 (6.5%) | 58 (18.4%) | 310 (11.5%) | |||
| Occasionally | 195 (29.1%) | 1,341 (29.2%) | 104 (29.3%) | 571 (30.2%) | 91 (28.8%) | 770 (28.6%) | |||
| Rarely or never | 386 (57.5%) | 2,811 (61.3%) | 219 (61.7%) | 1,195 (63.3%) | 167 (52.8%) | 1,616 (59.9%) | |||
| How do you think your risk of heart attack or stroke compares with other men/women your age? (% slightly higher to much worse) | 213 (28.6%) | 1,735 (36.2%) | <0.001 | 99 (25.0%) | 618 (31.0%) | 0.009 | 114 (32.7%) | 1,117 (39.9%) | 0.02 |
| People with high cholesterol are more likely to have a heart attack | 623 (77.3%) | 3,954 (81.0%) | 0.02 | 360 (80.0%) | 1,640 (80.7%) | 0.73 | 263 (73.9%) | 2,314 (81.2%) | 0.001 |
| People don’t need to worry about their cholesterol if they have never had a heart attack or other heart problem. | 71 (8.8%) | 404 (8.3%) | 0.61 | 41 (9.1%) | 154 (7.6%) | 0.27 | 30 (8.4%) | 250 (8.8%) | 0.83 |
| Statin efficacy | |||||||||
| Statin medications are effective in reducing the risk of heart disease and stroke | 564 (70.0%) | 3,635 (74.4%) | 0.008 | 311 (69.1%) | 1,441 (70.9%) | 0.45 | 253 (71.1%) | 2,194 (77.0%) | 0.01 |
| Statin safety | |||||||||
| Statins are safe medications | 292 (36.2%) | 2,800 (57.3%) | <0.001 | 145 (32.2%) | 1,112 (54.7%) | <0.001 | 147 (41.3%) | 1,688 (59.2%) | <0.001 |
| I think statins can cause diabetes | 61 (7.6%) | 299 (6.1%) | 0.12 | 26 (5.8%) | 120 (5.9%) | 0.92 | 35 (9.8%) | 179 (6.3%) | 0.01 |
| I think statins can cause muscle aches or pain | 216 (26.8%) | 1,913 (39.2%) | <0.001 | 96 (21.3%) | 728 (35.8%) | <0.001 | 120 (33.7%) | 1,185 (41.6%) | 0.004 |
| I think statins can cause liver damage | 157 (19.5%) | 1,406 (28.8%) | <0.001 | 67 (14.9%) | 568 (28.0%) | <0.001 | 90 (25.3%) | 838 (29.4%) | 0.11 |
| I think statins can cause memory loss | 101 (12.5%) | 558 (11.4%) | 0.36 | 47 (10.4%) | 206 (10.1%) | 0.85 | 54 (15.2%) | 352 (12.3%) | 0.13 |
| Clinician trust | |||||||||
| How much would you say you trust your doctors’ decisions about your medical care? (% generally trust or completely trust) | 663 (87.0%) | 4,579 (94.7%) | <0.001 | 352 (85.2%) | 1,906 (94.7%) | <0.001 | 311 (89.1%) | 2,673 (94.7%) | <0.001 |
Statin-related beliefs and perceptions are presented here for African Americans vs. Caucasians, categorized by worries about disease, beliefs about efficacy, beliefs about safety, clinician trust and side effect experiences.
Responses presented are collected from patient survey questions asked on a five point Likert scale from strongly disagree to strongly agree, results shown are the % of participants who reported agree to strongly agree
Multivariable and Sequential Modeling of Statin Utilization
Sequential modeling of statin under-treatment among African Americans vs. Caucasians revealed an association between African American race and statin under-treatment (relative risk [RR] 1.14, confidence interval [CI] 1.06–1.22, p<0.001), which persisted after correction for demographics (Figure 3). The association was no longer statistically significant when sequentially adjusted for clinical characteristics (RR for African American vs. Caucasian 1.07, CI 1.00–1.15, p=0.05), socioeconomic status (RR 1.07, CI 0.99–1.15, p=0.07), patient beliefs (RR 1.04, CI 0.97–1.11, p=0.25), and provider characteristics (RR 1.03, CI 0.96–1.11, p=0.35). While the association between race and statin under-treatment lost statistical significance when adjusting for individual sets of confounders in sequential modeling, no individual set of confounders fully accounted for the association between race and statin under-treatment (eFigure 1).
Figure 3. A Sequential Modeling Approach for Racial Differences in Statin Undertreatment of African Americans.
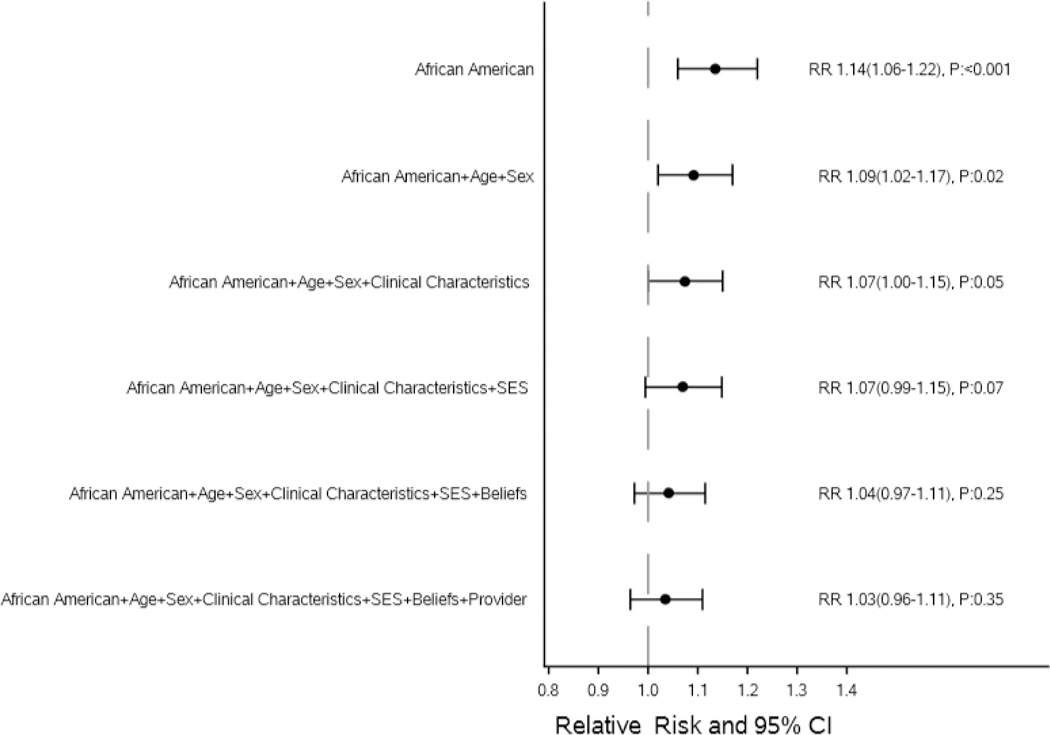
The relative risk of statin undertreatment of African American patients are presented here, both unadjusted and with sequential adjustment for relevant confounders. Statin undertreatment was defined as less than ACC/AHA guideline-recommended statin therapy. The following sequential models were created to evaluate how the relative risk of African American race for statin undertreatment:1) Model 1 adjusted for race alone; 2) Model 2 includes age and sex; 3) Model 3 adds clinical characteristics including prior ASCVD (grouped into coronary heart disease, cerebrovascular disease, and other ASCVD), diabetes, obesity, smoking, and hypertension; 4) Model 4 adds socioeconomic factors such as yearly income, insurance status, education level, and numeracy score; 5) Model 5 adds in patient beliefs and perceptions including worry about heart disease, clinician trust, beliefs about statin safety and effectiveness, and beliefs about high cholesterol and heart attack risk; 6) Model 6 adds provider factors including provider type (cardiologist vs. non-cardiologist), whether the patient’s provider reported using the 2013 ACC/AHA guideline as their primary resource for lipid management in the provider survey, and clinic setting (urban vs. rural).
Abbreviations: ACC, American College of Cardiology; AHA, American Heart Association; CI, confidence interval; OR, odds ratio; SES, socioeconomic status
Discussion
Statins are a cornerstone of therapy for primary and secondary prevention of cardiovascular disease. Among those individuals who meet criteria for statins in PALM, we found that African Americans were slightly less likely than Caucasians to receive statins overall, and much less likely to receive guideline-recommended statin intensity. African Americans and Caucasians had different perceptions and beliefs regarding statin therapy, which along with other factors including demographics, clinical characteristics, socioeconomic status, and lower frequency of care by cardiologists, accounted for the racial differences in treatment observed.
Overall treatment rates with any statin by race were modest, with only an absolute 4% difference overall in the rate of any statin use between African Americans and Caucasians; however, racial differences were more pronounced when statin intensity was considered. In both primary and secondary prevention, African Americans were less likely to receive guideline-appropriate statin intensity than Caucasians. Lower utilization of appropriate intensity statins among African Americans compared with Caucasians contributed to higher LDL-C levels observed among African Americans. Given that the association between even a modest LDL-C reduction and cardiovascular disease risk reduction of major vascular events is well-established (2), differences in appropriate statin therapy utilization and corresponding differences in LDL-C levels may partially explain differences in ASCVD burden between African American and Caucasian adults.
Our finding that African Americans were less likely to receive guideline-appropriate statin therapy is consistent with prior literature. Despite African Americans being at higher risk of ASCVD (4), multiple studies have demonstrated that they have a lower likelihood of treatment and lower adherence to statin therapy (5, 6, 10, 11). Prior literature also suggests that African Americans are less likely to have cholesterol screening (12), have lower long-term adherence post-myocardial infarction despite cardiologist discharge on a statin (10), and worse lipid control (according to the Million Hearts initiative) (13). Why these gaps remain has been poorly understood, and prior studies investigating racial disparities in statin therapy have not included the potential influence of individuals’ beliefs, preferences, and concerns on treatment patterns (5, 14). Our study is one of the first to investigate racial differences in community statin utilization since the publication of the 2013 ACC/AHA cholesterol guideline, and one of the first to evaluate the relative impact of patient beliefs with sociodemographic and clinical information. We confirm that racial differences in statin use persist in the modern treatment era, with lower statin treatment rates among African Americans compared with Caucasians.
The reasons for racial differences are complex, and may be partially explained by differences in several characteristics. African American patients were more frequently female with higher rates of diabetes and tobacco use, were less likely to have prior ASCVD, and had lower socioeconomic and educational levels than Caucasians. African American individuals were more likely to have Medicaid rather than private insurance or Medicare, which may have influenced their access to healthcare services, along with lower socioeconomic status. Financial barriers may be a component of statin underutilization, and some have suggested that interventions such as reduction of insurance copayments for statins may improve adherence in African American communities (15). Nonetheless, adjusting for socioeconomic status did not fully account for the racial differences in statin use found in PALM. Prior work has demonstrated that long-term statin persistence is lower among African Americans, even among those with prescription drug coverage (16). Improving racial disparities in statin utilization will likely require multiple approaches.
The type of provider that a patient sees may also play a role in differential treatment patterns. African Americans were more likely to have seen an endocrinologist and were less likely to be treated by a cardiologist or a provider who reported following the 2013 ACC/AHA cholesterol guideline. These findings may have influenced the observed treatment differences.
While many of the demographic, clinical, and socioeconomic factors that could contribute to treatment differences remain as potential confounders in PALM participants, this study is the first to investigate the potential influence of African Americans’ ASCVD risk perception, clinician trust, and beliefs about statin therapy. Differences in beliefs between African American and Caucasian participants may play a role in differences in treatment patterns. Specifically, African American patients were more likely to believe they were at lower risk than their peers, but were more likely to worry about having a heart attack or stroke. African Americans were less likely to believe that statins are effective and far less likely than Caucasian participants to believe statins are safe. Such perceptions and experiences may influence adherence to statin therapy and willingness to consider therapy; altering that perception can often change patients’ willingness to take a medication (17–20).
Adding complexity to these observations, while the vast majority of both African American and Caucasian individuals reported completely trusting their clinicians, there were differences by race, with fewer African Americans reporting “complete” trust in their clinician than Caucasians. Medical mistrust among African American patients for non–statin-based clinical decisions has been previously documented (21, 22), representing an important challenge for both providers and patients. Trust-building in clinical practice settings is more difficult than ever. Shorter office visits and electronic medical records consume clinicians’ attention, but the process remains critical to the implementation and efficacy of educational efforts. Medical mistrust may also be influenced by poor provider communication. The psychological, cultural, and community aspects that may contribute to these differences in statin beliefs and clinician trust, as well as their potential impact on statin utilization, merit further investigation.
Although this study focused on differences by race, it is worth noting that there was a strikingly high rate of under-treatment among both African American and Caucasian patients overall, with less than half of all patients receiving the guideline-recommended statin therapy level of intensity (23). Therefore, even if African American adults were treated at the same rate as Caucasian adults, significant room for improvement would remain. Despite very low rates of serious adverse effects observed in clinical trials (24–27), we observed ongoing significant safety concerns on the part of patients. We observed a wider racial gap in statin adverse effects in primary vs. secondary prevention, likely reflecting the more standardized treatment approach seen in secondary prevention populations and less consensus on use in primary prevention. Given the track record of statins being relatively safe and well-tolerated medications, the onus is on clinicians and pharmacists to accurately communicate both the safety and risks of these important preventive medications. On the other hand, we were reassured that around eighty percent of both African Americans and Caucasians were aware of the association between high cholesterol and heart attacks, while less than ten percent of both groups felt they didn’t need to worry about their cholesterol if they never had a heart attack or heart problem. This represents a significant triumph in terms of patient education and healthcare awareness. These results highlight the importance of refocusing our emphasis on systemic improvements to better care for our most vulnerable patients by improving the care of the population as a whole. This includes eliciting and addressing patients’ concerns, emphasizing patient education, performance measures and incentives, providing decision support for clinicians, and creating quality improvement initiatives on the local and national levels.
Our study had some limitations. First, we did not directly assess the stated reasoning behind provider decisions to prescribe or not prescribe statin therapy in study participants; therefore, it is possible that contraindications to therapy in both African American and Caucasian participants or patient refusal were present. Second, our study was limited by missing responses for some categories. There was no specific response rate, but African Americans more frequently declined to answer belief questions than Caucasians (eTable1). For missing socioeconomic status data, we used median incomes from household zip codes, which may be inaccurate. Similarly, some patients did not fully report disease and belief perceptions. However, we performed sensitivity analysis of the multivariable modeling to assess the impact of missing data by comparing imputing missing data to excluding missing data and found that the results of the models were analogous. Our results were robust whether we analyzed only responders, simple imputation, or multiple imputation methods. Third, we did not ask about stroke, which is more common in African Americans and may have influenced overall concern among African Americans. Finally, patients’ trust in their clinicians may be over-estimated based on the fact that these surveys were deployed in the clinic setting for study participants who were already being seen by their clinician.
Conclusions
Racial differences persist in statin utilization among adults surveyed in community practice. African American adults were less likely to be treated with any statin or guideline-recommended statin intensity than Caucasians, which may contribute to higher LDL-C levels among African Americans. The reasons underlying racial differences in statin therapy are complex, with African Americans differing from Caucasians in their risk perception, trust in providers, and beliefs about efficacy and safety of statins. Future interventions must consider this complexity while being driven by the patient perceptions, attitudes, and concerns identified here. While improving racial disparities may help reduce the burden of ASCVD in African Americans, the majority of both African American and Caucasian patients were not receiving guideline-appropriate statin therapy. Greater emphasis on following national guidelines when treating both African Americans and Caucasians may improve care and outcomes for all patients.
Supplementary Material
Key Points.
Question:
What are the statin treatment patterns in African American vs. Caucasian adults since the release of the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults?
Findings:
Among 5,689 patients (806, 14% African American) statin-eligible in PALM, African Americans were less likely to receive a statin at the guideline-recommended intensity (33% vs. 44%, p<0.001), though this association was no longer significant after adjusting for demographics, clinical characteristics, socioeconomic status, patient beliefs, and provider factors (RR for statin undertreatment 1.03, CI 0.96–1.11).
Meaning:
African American outpatient adults were less likely to receive guideline-appropriate statin therapy, though this can be explained by a combination of demographics, clinical characteristics, socioeconomic status, patient beliefs, and provider factors.
Acknowledgments
We thank Erin Campbell, MS, for her editorial contributions to this manuscript. Ms. Campbell did not receive compensation for her contributions apart from her employment at the institution where this study was conducted.
Sources of Funding:
The PALM Registry received funding from Sanofi and Regeneron Pharmaceuticals. Dr. Navar is supported by the NHLBI (K01HL133416).
AM Navar: Dr. Navar reports research grants (significant) from Amgen, Sanofi, and Regeneron; consultant/advisory board (modest) for Amgen and Sanofi.
AC Goldberg: Dr. Goldberg reports reports research grants (modest) from Amarin, Amgen, Pfizer, Regeneron; research grants (significant) from Regeneron/Sanofi, IONIS; honoraria (modest) from Merck Manual; consultant/advisory board (modest) from Regeneron/Sanofi, Esperion.
J Robinson: Dr. Robinson reports reports research grants (significant) from Amarin, Amgen, Astra-Zeneca, Eli Lilly, Esai, Glaxo-Smith Kline, Merck, Pfizer, Regeneron/Sanofi, Takeda; consultant/advisory board (modest) for Amgen, Eli Lilly, Merck, Pfizer, Regeneron; consultant/advisory board (significant) for Sanofi, Dr. Reddy Laboratories.
SS Virani: Dr. Virani reports reports research grants (significant) from AHA, ADA, VA; honoraria (significant) from American College of Cardiology, National Lipid Association; other (significant) steering committee for PALM Registry at Duke University (no financial remuneration).
TY Wang: Dr. Wang reports reports research grants (modest) from Pfizer, Bristol Myers Squibb; research grants (significant) from AstraZeneca, Boston Scientific, Daiichi Sankyo, Eli Lilly, Gilead Sciences, Regeneron Pharmaceuticals; honoraria (modest) from Merck, Gilead; honoraria (significant) from Sanofi.
ED Peterson: Dr. Peterson reports reports research grants (significant) from Amgen, Sanofi, Astrazeneca, Merck; consultant/advisory board (modest) from Amgen; consultant/advisory board (significant) from AstraZeneca, Merck, and Sanofi Aventis.
Footnotes
Conflict of Interest Disclosures
MG Nanna: Dr. Nanna reports no relevant disclosures.
P Zakroysky: Ms. Zakroysky reports no relevant disclosures.
Q Xiang: Ms. Xiang reports no relevant disclosures.
VL Roger: Dr. Roger reports no relevant disclosures.
PWF Wilson: Dr. Wilson reports no relevant disclosures.
J Elassal: Dr. Elassal reports being an employee and stockholder in Regeneron Pharmaceuticals, Inc. (significant).
LV Lee: Dr. Lee reports employment (significant) from Sanofi.
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–45. [DOI] [PubMed] [Google Scholar]
- 2.Cholesterol Treatment Trialists (CTT) Collaborators, Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;(1):CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Writing Group Members, Mozaffarian D, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2016 Update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. [DOI] [PubMed] [Google Scholar]
- 5.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42(9):1208–1215. [DOI] [PubMed] [Google Scholar]
- 6.Salami JA, Warraich H, Valero-Elizondo J, et al. National trends in statin use and expenditures in the US adult population from 2002 to 2013: insights from the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2(1):56–65. [DOI] [PubMed] [Google Scholar]
- 7.Navar AM, Wang TY, Goldberg AC, et al. Design and rationale for the Patient and Provider Assessment of Lipid Management (PALM) registry. Am Heart J. 2015;170(5):865–871. [DOI] [PubMed] [Google Scholar]
- 8.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. [DOI] [PubMed] [Google Scholar]
- 9.Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the Subjective Numeracy Scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27(5):663–671. [DOI] [PubMed] [Google Scholar]
- 10.Lauffenburger JC, Robinson JG, Oramasionwu C, Fang G. Racial/ethnic and gender gaps in the use of and adherence to evidence-based preventive therapies among elderly Medicare Part D beneficiaries after acute myocardial infarction. Circulation. 2014;129(7):754–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis AM, Taitel MS, Jiang J, et al. A national assessment of medication adherence to statins by the racial composition of neighborhoods. J Racial Ethn Health Disparities. 2017;4(3):462–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kenik J, Jean-Jacques M, Feinglass J. Explaining racial and ethnic disparities in cholesterol screening. Prev Med. 2014;65:65–69. [DOI] [PubMed] [Google Scholar]
- 13.Eapen ZJ, Liang L, Shubrook JH, et al. Current quality of cardiovascular prevention for Million Hearts: an analysis of 147,038 outpatients from The Guideline Advantage. Am Heart J. 2014;168(3):398–404. [DOI] [PubMed] [Google Scholar]
- 14.Qato DM, Lindau ST, Conti RM, Schumm LP, Alexander GC. Racial and ethnic disparities in cardiovascular medication use among older adults in the United States. Pharmacoepidemiol Drug Saf. 2010;19(8):834–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewey J, Shrank WH, Avorn J, Liu J, Choudhry NK. Medication adherence and healthcare disparities: impact of statin co-payment reduction. Am J Manag Care. 2015;21(10):696–704. [PubMed] [Google Scholar]
- 16.Zhang Y, Baik SH, Chang CC, Kaplan CM, Lave JR. Disability, race/ethnicity, and medication adherence among Medicare myocardial infarction survivors. Am Heart J. 2012;164(3):425–433.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berglund E, Lytsy P, Westerling R. Adherence to and beliefs in lipid-lowering medical treatments: a structural equation modeling approach including the necessity-concern framework. Patient Educ Couns. 2013;91(1):105–112. [DOI] [PubMed] [Google Scholar]
- 18.Kalia NK, Cespedes L, Youssef G, Li D, Budoff MJ. Motivational effects of coronary artery calcium scores on statin adherence and weight loss. Coron Artery Dis. 2015;26(3):225–230. [DOI] [PubMed] [Google Scholar]
- 19.Johnson JE, Gulanick M, Penckofer S, Kouba J. Does knowledge of coronary artery calcium affect cardiovascular risk perception, likelihood of taking action, and health-promoting behavior change? J Cardiovasc Nurs 2015;30(1):15–25. [DOI] [PubMed] [Google Scholar]
- 20.Mamudu HM, Paul TK, Veeranki SP, Budoff M. The effects of coronary artery calcium screening on behavioral modification, risk perception, and medication adherence among asymptomatic adults: a systematic review. Atherosclerosis. 2014;236(2):338–350. [DOI] [PubMed] [Google Scholar]
- 21.Collins TC, Clark JA, Petersen LA, Kressin NR. Racial differences in how patients perceive physician communication regarding cardiac testing. Med Care. 2002;40(1 Suppl):I27–34. [DOI] [PubMed] [Google Scholar]
- 22.Kalichman SC, Eaton L, Kalichman MO, Grebler T, Merely C, Welles B. Race-based medical mistrust, medication beliefs and HIV treatment adherence: test of a mediation model in people living with HIV/AIDS. J Behav Med. 2016;39(6):1056–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Navar AM, Wang TY, Li S, et al. Lipid management in contemporary community practice: results from the Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2017;193:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289:1681–90. [DOI] [PubMed] [Google Scholar]
- 25.Hsia J, MacFadyen JG, Monyak J, Ridker PM. Cardiovascular event reduction and adverse events among subjects attaining low-density lipoprotein cholesterol <50 mg/dl with rosuvastatin. The JUPITER trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin). J Am Coll Cardiol. 2011;57:1666–75. [DOI] [PubMed] [Google Scholar]
- 26.Heart Protection Study Collaborative G. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [DOI] [PubMed] [Google Scholar]
- 27.Yusuf S, Bosch J, Dagenais G, et al. Cholesterol Lowering in Intermediate-Risk Persons without Cardiovascular Disease. N Engl J Med. 2016;374:2021–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


