Abstract
OBJECTIVE
To estimate differences in the length of stay and costs for comparable hospitalizations of patients with spina bifida (SB) with and without pressure injuries.
DESIGN
Retrospective, cross-sectional, observational study.
SETTING
Nationwide Inpatient Sample from years 2010 to 2014.
PARTICIPANTS
Hospitalized patients with SB. Hospitalizations among patients with SB and pressure injuries (n=3888) were matched to hospitalizations among patients with SB but without pressure injuries (n=3888).
INTERVENTIONS
Not applicable.
MAIN OUTCOME MEASURES
Differences in length of stay and total costs between the two groups.
RESULTS
After successful matching, multivariate modelling of costs and length of stay on matched sample showed that hospitalizations with pressure injuries had an increased 1.2 inpatient days and excess average costs of $1,182.
CONCLUSIONS
The estimated average cost of hospitalization increased by 10%, and the estimated average length of stay increased by 24% in the presence of pressure injuries among hospitalized patients with SB, compared with their peers without these injuries. These results highlight the substantial morbidity associated with pressure injuries, which are potentially preventable before or during hospitalizations among persons with SB.
Keywords: spina bifida, pressure injuries, costs and length of stay, propensity score matching
Spina bifida (SB) is a birth defect in which the spinal cord does not develop properly due to incomplete closure of the neural tube during early gestation. It is a multi-system condition that requires lifelong neurosurgical, urologic, musculoskeletal, skin, and habilitation management.1 Depending on the neurologic level of the lesion, patients with SB may have decreased or absent skin sensation, making them vulnerable to skin problems such as pressure injuries. Skin problems (pressure injuries, infections, and other wounds) are also among the top primary diagnoses requiring hospitalization among adults with SB.2 We use the term “pressure injury” throughout this article to be consistent with the National Pressure Ulcer Advisory Panel (NPUAP) who changed the term, “pressure ulcer” to “pressure injury”.3 We keep “pressure ulcer” only when referring to the ICD-9 diagnosis code specifically. Pressure injuries have a negative impact on overall patient well-being, morbidity, and mortality in SB. 4–5 Several studies have provided insight into the risk factors for developing pressure injuries among patients with SB, which include higher lesion level, shunt presence, older age, male sex, prior orthopedic surgery, wheelchair use, obesity, reduced executive functioning, memory deficits, Chiari II malformation, sensory deficits, and urinary incontinence.6–8
Individuals with spinal cord injury have similar vulnerabilities, and the relationship between pressure injuries and healthcare utilization have been relatively well studied in this population. A higher presence of pressure ulcers was found in individuals with spinal cord injury and pneumonia.9 For example, over 1/3 of individuals with acute spinal cord injury develop at least one pressure injury during the time they are hospitalized and receiving inpatient rehabilitation.10 During the chronic phase of spinal cord injury, pressure injuries are among the most common reasons why they are hospitalized or visit emergency rooms.11–12 Pressure injuries are also associated with higher risk for mortality.13 Treatment cost for pressure injuries in individuals with spinal cord injury is estimated to range from $2 to 5 billion annually14 and prevention is estimated to cost less than 1/10 this amount.15 Recurrent pressure injuries may also increase length of stay.16
Little research exists on the cost and length of hospitalizations associated with pressure injuries among SB patients. Such information is important for understanding whether pressure injuries serve as marker for higher cost hospitalizations and to inform economic evaluations of pressure injury prevention strategies. To address this knowledge gap, we aimed at estimating the differences in the length of stay and cost for comparable hospitalizations between patients with SB with any diagnostic code of pressure ulcer (whether present on admission or hospital acquired) and patients with SB without any pressure ulcer diagnostic code.
Methods
Data Sources and Study Population
This is a retrospective study using data over a five-year period (from 2010 through 2014) from the National Inpatient Sample (NIS) database maintained by the Agency for Healthcare Research and Quality’s (AHRQ) Healthcare Cost and Utilization Project (HCUP). The NIS is sampled from the State Inpatient Databases, which include all inpatient data that are currently contributed to HCUP. Starting in 2012, the NIS is a 20 percent stratified systematic sample of all discharges from US community hospitals. Community hospitals (and HCUP data) are short-term, non-Federal and include OB-GYN, ENT, orthopedic, cancer, pediatric, public, and academic medical hospitals. They exclude hospitals whose main focus is long-term care, psychiatric, and alcoholism and chemical dependency treatment. The number of states participating in HCUP increased over the years and in 2015 a total of 48 states were included in HCUP. The NIS contains clinical and nonclinical data elements for each hospital stay, such as primary and secondary diagnoses, demographic characteristics, hospital characteristics, total charges, and length of stay. The NIS has been used to estimate national health care utilization and charges, care quality, and outcomes.17 We obtained data after taking the data use training course and signing the data use agreement. This study was exempt from institutional review board approval.
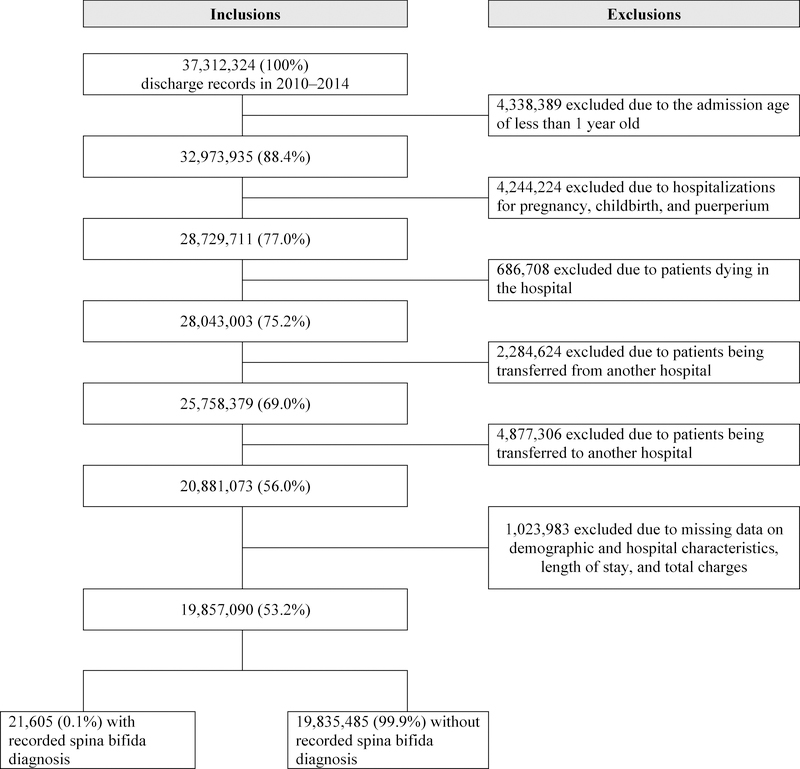
A total of 37,312,324 hospital discharge records from 2010 through 2014 were in the NIS database. We applied several exclusion criteria to these discharge records as depicted in Figure 1. We excluded records of patients with age at admission less than 1 year old and hospitalizations related to pregnancies, childbirth and puerperium, deaths. We excluded hospital transfers in order to capture complete hospital episodes of care. We also excluded end-of-life hospitalizations, because pressure injuries in end-of-life care may follow a different disease course and may incur significantly increased costs.18 Finally, we excluded records with missing information in any of the following variables: length of stay, total charges, age, sex, race, insurance type, region of hospital, bed size of hospital, and location or teaching status of the hospital.
Figure 1.
Flowchart detailing the sample inclusion/exclusion criteria from all the discharge records in the National Inpatient Sample, 2010–2014.
Propensity score matching: Hospitalizations of Patients with SB With and Without Pressure Injuries
We used International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes (http://www.icd9data.com/) to identify hospitalized patients with SB (ICD-9 codes: 741.xx) with and without pressure ulcer (ICD-9 codes: 707.xx). We used the first three digit ICD-9 code because administrative data are for billing purposes and may not be accurate in recording specific 5-digit ICD-9 codes. The ICD-9 code 707 for pressure ulcer include all stages of skin ulcers and we did not distinguish among different stages of pressure ulcers (707.20–707.25). The NIS data included up to 30 discharge diagnoses per hospitalization and we investigated all diagnosis codes listed, including both principal and secondary diagnoses.
We matched the group of hospitalizations of patients with SB with pressure injuries, with a group of hospitalizations of patients with SB without pressure injuries, using propensity scores. Propensity score matching is a statistical technique designed to reduce bias due to confounding variables.19–20 The purpose of propensity score matching is to make two groups comparable by balancing measured covariates. This technique has been applied to assess risk factors associated with hospital acquired pressure injuries and impact on health care use and costs.21 Propensity score matching has also been applied to NIS encounter based data, including cost comparisons.22–23 In our case, a propensity score is the estimated probability that a hospitalization with SB would record pressure ulcer diagnostic codes, either present at admission or developed during hospitalization. We used propensity score matching to construct two groups of hospitalizations that were comparable with regard to the patients’ propensity to have pressure injuries. Before matching, the raw comparisons of hospitalizations, with and without pressure injuries, would overestimate the differences in the length of stay associated with pressure injuries because of the large number of conditions associated with the propensity to develop pressure injuries.
The presence of pressure injuries was modelled through multivariable logistic regression as a function of patient demographic, hospital, and clinical characteristics among all hospitalizations of patients with SB. Patient characteristics included age, sex, insurance type, and race. Hospital characteristics included hospital region, hospital bed size, rural/urban location and teaching status of the hospital. Clinical characteristics were selected based on Clinical Classifications Software (CCS) categories. CCS is a tool developed by the AHRQ for categorizing ICD-9 diagnosis and procedure codes into clinically meaningful categories.24 We used single level CCS diagnosis codes, which grouped more than 14,000 ICD–9 diagnosis codes into over 200 clinical categories. To determine CCS categories to be included in propensity score estimation, we calculated relative risks and their corresponding 95% confidence intervals for each category and selected all categories that has a relative risk significantly higher than one. A total of 47 CCS diagnosis categories were included in propensity score estimation (Supplementary Table 1).
Outcomes
The two main outcomes measured in our study were length of stay in days and total costs in US dollars. We used the hospital-level cost-to-charge ratio files to convert the total charges to costs.25 We also converted annual charges and costs to 2014 dollars, based on the consumer price indices of the Bureau of Labor Statistics.26
Statistical Analysis
The first level of analysis was an overall comparison of hospitalizations with SB between those with and without pressure injury diagnosis. We performed Friedman’s Chi squared tests to evaluate the associations between pressure injuries and demographic and hospital characteristic categorical variables, including year at admission (2010, 2011, 2012, 2013 and 2014), age at admission (1–10, 11–20, 21–30, 31–40, 41–50, 51–60, 61–70, and 71+), insurance type (Medicaid, Medicare, private, uninsured, and other), gender, race/ethnicity (African American, Hispanic, White, and Other), region of hospital (Northeast, Midwest, South, and West), hospital bed size (small, medium, and large), and hospital location/teaching status (rural, urban nonteaching, and urban teaching).
Then we performed propensity score matching using MatchIt package27 in R software (R Foundation for Statistical Computing, version 3.3.3). All the significant variables in Table 1 and Supplementary Table 1 were included in the estimation of propensity score. We constructed one-to-one matched pairs based on nearest neighbor matching method: each hospitalization without a pressure injury was matched to one with a pressure injury that had the closest estimated propensity score on the logit scale.
Table 1.
Demographic characteristics of the patients hospitalized with spina bifida stratified by pressure injuries status before matching on propensity scores. The 2010–2014 Nationwide Inpatient Dataset.
| Pressure Injuries | |||
|---|---|---|---|
| No (n= 17,717) | Yes (n=3,888) | P value | |
| Categorical Variables* | |||
| Year of Admission | |||
| 2010 | 3,617 (20.4%) | 800 (20.6%) | 0.9774 |
| 2011 | 3,600 (20.3%) | 772 (19.9%) | |
| 2012 | 3,533 (19.9%) | 779 (20.0%) | |
| 2013 | 3,455 (19.5%) | 766 (19.7%) | |
| 2014 | 3,512 (19.8%) | 771 (19.8%) | |
| Age at Admission | |||
| 1–10 | 3,397 (19.2%) | 134 (3.5%) | <.0001 |
| 11–20 | 3,319 (18.7%) | 568 (14.6%) | |
| 21–30 | 3,358 (19.0%) | 1,037 (26.7%) | |
| 31–40 | 2,814 (15.9%) | 915 (23.5%) | |
| 41–50 | 2,372 (13.4%) | 670 (17.2%) | |
| 51–60 | 1,372 (7.7%) | 350 (9.0%) | |
| 61–70 | 707 (4.0%) | 170 (4.4%) | |
| 71+ | 378 (2.1%) | 44 (1.1%) | |
| Insurance Type | |||
| Medicaid | 6,420 (36.2%) | 1,469 (37.8%) | <.0001 |
| Medicare | 4,497 (25.4%) | 1,490 (38.3%) | |
| Private | 5,486 (31.0%) | 743 (19.1%) | |
| Uninsured | 482 (2.7%) | 78 (2.0%) | |
| Other | 832 (4.7%) | 108 (2.8%) | |
| Sex | |||
| Male | 7,482 (42.2%) | 2,110 (54.3%) | <.0001 |
| Female | 10,235 (57.8%) | 1,778 (45.7%) | |
| Race | |||
| African American | 1,762 (10.0%) | 403 (10.4%) | <.0001 |
| Hispanic | 2,629 (14.8%) | 492 (12.7%) | |
| White | 10,795 (60.9%) | 2,513 (64.6%) | |
| Other | 2,531 (14.3%) | 480 (12.4%) | |
| Region of Hospital | |||
| Northeast | 2,552 (14.4%) | 592 (15.2%) | 0.0388 |
| Midwest | 4,489 (25.3%) | 944 (24.3%) | |
| South | 7,318 (41.3%) | 1,670 (43.0%) | |
| West | 3,358 (19.0%) | 682 (17.5%) | |
| Bed Size of Hospital | |||
| Small | 2,141 (12.1%) | 455 (11.7%) | 0.4599 |
| Medium | 4,456 (25.2%) | 1,013 (26.1%) | |
| Large | 11,120 (62.8%) | 2,420 (62.2%) | |
| Location/Teaching Status of
Hospital |
|||
| Rural | 1,276 (7.2%) | 392 (10.1%) | <.0001 |
| Urban nonteaching | 3,903 (22.0%) | 1,074 (27.6%) | |
| Urban teaching | 12,538 (70.8%) | 2,422 (62.3%) | |
For categorical variables, we reported frequencies (percentages); P values were from Friedman’s Chi squared tests.
After successful matching, we compared the total costs and length of stay for hospitalizations with SB with and without pressure injuries. We reported both mean and median because length of stay and total costs were skewed due to outliers. The means were compared using the non-parametric Wilcoxon rank sum test because the data were not normally distributed.
We used generalized linear mixed models to estimate total costs and length of stay for hospitalizations among the matched sample. Total costs were modelled to follow a gamma distribution and length of stay was modeled to follow a negative binomial distribution. 22,28 We estimated the least square mean costs in 2014 dollars and the least square mean length of stay in days over the entire sample and over each age group, using pressure injuries as the main predictor in the fitted models. Other covariates included year at admission, age at admission (excluded in the estimation by age group), insurance type, gender, race/ethnicity, region of hospital, hospital bed size and hospital location/teaching status. These statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC). Results were considered statistically significant when a two-tailed test yielded a p value < .05.
Results
After applying our exclusion criteria, 19,857,090 (53.2%) hospitalization records remained and we identified 21,605 (0.1%) hospitalizations associated with SB. Among hospitalizations of patients with SB, we identified 3888 (18.0%) with pressure injuries and 17717 (82.0%) without pressure injuries (Figure 1).
Table 1 presented the characteristics of the hospitalizations of patients with SB, with and without pressure injuries. Compared to hospitalizations without pressure injuries, hospitalizations with pressure injuries were more likely to involve patients who were male, less likely to involve patients who were privately insured, and less likely to be from urban teaching hospitals. Among hospitalizations of patients with SB and pressure injuries, age at admission peaked at 21 to 30 years and the percentage remained higher than that among those without pressure injuries until 70 years of age. In contrast, the percentage of hospitalizations without pressure injuries was much higher among the younger age groups of year 1 through 20 years.
After the one-to-one propensity score matching, the 3,888 hospitalizations of patients with SB with pressure injuries were successfully matched to the same number of hospitalizations of patients with SB without pressure injuries. Both groups of hospitalizations had a similar likelihood of having pressure injuries recorded. The matched groups showed no statistical differences in the percentage distributions of the demographic and hospital characteristics listed in Table 1. We also examined the quality of the matching results by comparing histograms of propensity scores of the matched groups, which suggested no significant differences in the distribution of propensity scores.
Table 2 summarized length of stay and total costs before and after matching on propensity score. The associated length of stay of pressure injuries would have been overestimated if the matching technique was not used to account for the fact that patients with SB who developed pressure injuries were at higher risk for other costly comorbid conditions. After matching by propensity scores, mean/median difference in length of stay associated with pressure injuries was 1.5/1 days (mean: 7.4 vs. 5.9 days, P < .0001; median: 5 vs. 4 days, P < .0001). Mean/median difference in total costs associated with pressure injuries were 1423/1116 dollars (mean: $15,829.9 vs. $14,407.1, P < .0001; median: $9,393.6 vs. $8,277.5, P < .0001).
Table 2.
Total costs and length of stay for patients with spina bifida with and without pressure injuries before and after the 1:1 propensity score matching.
| Pressure Injuries | ||||
|---|---|---|---|---|
| No (n=17,717) Before matching (1) | No (n= 3,888) After matching (2) | Yes (n=3,888) (3) | P value* (2) vs (3) | |
| Length of stay, days | ||||
| Mean (Standard Deviation) | 4.7 (5.6) | 5.9 (7.0) | 7.4 (8.9) | <.0001a |
| Median (Min-Max) | 3.0 (0.0–130.0) | 4.0 (0.0–130.0) | 5.0 (0.0–155.0) | <.0001b |
| Total costs in 2014 dollars | ||||
| Mean (Standard Deviation) | 13,950.6 (19,697.3) | 14,407.1 (22,444.5) | 15,829.9 (24,806.8) | <.0001a |
| Median (Min-Max) | 8,483.4 (45.0–584,423.9) | 8,277.5 (156.2–584,423.9) | 9,393.6 (559.8–526,098.1) | <.0001b |
P values were from Wilcoxon rank sum tests
P values were from Median tests.
Table 3 showed that in multivariate models, compared with matched hospitalizations among patients with SB but without pressure injuries, hospitalizations among patients with SB and pressure injuries had on average, an increased length of stay of 1.2 days and excess costs of $1,182. The estimated average length of stay differences remained significant in each age group from 1 to 70 years. The estimated average total costs differences for patients in the 31 to 60 years of age categories were much higher than the costs differences for patients 30 years of age or younger.
Table 3.
Estimated average costs and length of stay for patients with spina bifida with and without pressure injuries overall matched sample and stratified by age group.
| Age group, years | Number of hospitalizations | Estimated least square mean cost in 2014 dollars | Difference in costs | Estimated least square mean length of stay in days | Difference in length of stay | ||
|---|---|---|---|---|---|---|---|
| Pressure injury | No pressure injury | Pressure injury | No pressure injury | ||||
| 1–10 | 134 | 13,320 | 12,542 | 778 | 5.7 | 4.5 | 1.2* |
| 11–20 | 568 | 9,057 | 8,175 | 882 | 4.6 | 3.7 | 0.9* |
| 21–30 | 1,037 | 11,624 | 10,767 | 857* | 6.0 | 4.9 | 1.1* |
| 31–40 | 915 | 11,571 | 10,145 | 1,426* | 5.7 | 4.7 | 1* |
| 41–50 | 670 | 12,517 | 11,297 | 1,220* | 6.2 | 5.2 | 1* |
| 51–60 | 350 | 12,282 | 10,511 | 1,771* | 4.9 | 4.1 | 0.8* |
| 61–70 | 170 | 10,540 | 9,576 | 964 | 5.1 | 4.0 | 1.1* |
| 71+ | 44 | 11,391 | 16,148 | −4,757 | 5.1 | 5.9 | −0.8 |
| Overall** | 3,888 | 12,911 | 11,729 | 1,182* | 6.2 | 5.0 | 1.2* |
Difference is statistically significant, p value < .05
Overall means generalized linear mixed regression model adjusted for demographic characteristics without stratifying by age group.
Discussion
Patients with SB are prone to pressure injuries and pressure injuries have a significant impact on their morbidity, mortality, and quality of life.6–8 In this study, we build upon previous work and address an information gap by estimating length of stay and costs associated with pressure injuries among hospitalizations of patients with SB.
After successful propensity score matching based on demographic, clinical, and hospital characteristics, we found significant increases in the length of stay and the costs associated with pressure injuries. These results continue to hold in the multivariate modelling on the matched sample. Our study also demonstrated that estimated differences in length of stay and costs associated with pressure injuries differed across age groups, with high costs differences in those 31 to 60 years of age.
Our study found the decade of life that accounts for the highest percentage of hospitalizations with pressure injuries among patients with SB was from age 21 to 30 years. This may indicate transition difficulties for patients with SB as they transition out of coordinated multidisciplinary pediatric care into the disjointed system of adult care for SB.29 Most pressure injuries could potentially be prevented with better outpatient care.
Study Limitations
This study was limited by the inherent limitations of administrative data. We relied on ICD-9 codes (741.xx) to identify SB. It is therefore possible that some hospitalizations of individuals with SB were excluded if these codes were not recorded for the admission. We also did not include hospitalizations of patients with other related congenital spinal cord anomalies (742.5x). In addition, we were unable to distinguish hospitalizations with pressure injuries present upon admission and hospital-acquired pressure injuries because such information was not included in the NIS data. Thus, we can only establish associations of pressure injuries and increased costs and length of stay rather than causality. However, the matching on propensity for pressure injuries tended to equalize the distribution of other comorbid conditions that lengthen hospitalization stay in the groups compared. In an open-cohort study of SB patients, most wounds (260/275) were community acquired.6 We excluded hospitalizations associated with death because end of life care and pressure injuries can be different from hospitalizations not related to death. According to this criterion, we excluded 214 (0.98%) hospitalizations associated with death among all hospitalizations of patients with SB. The fact that 79 (36.9%) of these excluded hospitalizations had pressure injuries suggests that end-of-life care and management of pressure injuries deserve further investigation. Lastly, the NIS data was encounter based and could not distinguish different patients. We were unable to distinguish hospitalizations and readmissions, thus limiting our ability to interpret the results. However, documenting the differences in costs and length of stay is a first step to further our understanding of pressure injuries in the SB population.
Conclusions
After successfully matching hospitalizations with SB on the propensity to have pressure injuries, we found that the estimated average cost of hospitalization increased by 10%, and the estimated average length of stay increased by 24% in the presence of pressure injuries among hospitalized patients with SB, compared with their peers without these injuries. The increased length of stay and costs of hospitalizations could be avoided if pressure injuries were prevented from occurring before or during a hospitalization. These results highlight the substantial morbidity associated with pressure injuries, which are potentially preventable among persons with SB.
Supplementary Material
Supplementary Table 1. Clinical Classifications Software (CCS) diagnosis codes associated with hospitalizations of patients with spina bifida and pressure injuries.
Acknowledgement
We would like to thank William Beierwaltes, PhD, adjunct professor of physiology, Wayne State University Medical School for his helpful comments.
Footnotes
Disclosures: None.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease and Control and Prevention.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dicianno BE, Kurowski BG, Yang JMJ, et al. Rehabilitation and Medical Management of the Adult with Spina Bifida. Am J Phys Med Rehabil. 2008;87(12):1027–1050. [DOI] [PubMed] [Google Scholar]
- 2.Dicianno BE, Wilson R. Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Arch Phys Med Rehabil. 2010;91(4):529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edsberg LE, Black JM, Goldberg M, et al. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wagner R, Linroth R, Gangl C, et al. Perception of secondary conditions in adults with spina bifida and impact on daily life. Disabil Health J. 2015;8(4):492–498. [DOI] [PubMed] [Google Scholar]
- 5.Cai B, McDermott S, Wang Y, et al. Skin ulcers and mortality among adolescents and young adults with spina bifida in South Carolina during 2000–2010. J Child Neurol. 2016;31(3):370–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ottolini K, Harris AB, Amling JK, et al. Wound care challenges in children and adults with spina bifida: an open-cohort study. J Pediatr Rehabil Med. 2013;6(1):1–10. [DOI] [PubMed] [Google Scholar]
- 7.Kim S, Ward E, Dicianno BE, et al. Factors associated with pressure ulcers in individuals with spina bifida. Arch Phys Med Rehabil. 2015;96(8):1435–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plaum PE, Riemer G, Frøslie KF. Risk factors for pressure sores in adult patients with myelomeningocele–a questionnaire-based study. Cerebrospinal Fluid Res. 2006;3(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krishnan S, Karg PE, Boninger ML, et al. Association between presence of pneumonia and pressure ulcer formation following traumatic spinal cord injury. J Spinal Cord Med. 2017; 40(4):415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brienza DM, Krishnan S, Karg PE, et al. Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study. Spinal cord. 2018;56(1):28–34. [DOI] [PubMed] [Google Scholar]
- 11.DeJong G, Tian W, Hsieh CH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil. 2013;94(4):S87–S97. [DOI] [PubMed] [Google Scholar]
- 12.Ditunno JF Jr, Formal CS. Chronic spinal cord injury. N Engl J Med. 1994;330(8):550–556. [DOI] [PubMed] [Google Scholar]
- 13.Krause JS, Carter RE, Pickelsimer EE, et al. A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2008;89(8):1482–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal cord. 1996;34(5):255. [DOI] [PubMed] [Google Scholar]
- 15.Noble PC. The prevention of pressure sores in persons with spinal cord injuries International Exchange of Information in Rehabilitation, World Rehabilitation Fund; 1981. [Google Scholar]
- 16.Guihan M, Garber S, Bombardier C, et al. Predictors of pressure ulcer recurrence in veterans with spinal cord injury. J Spinal Cord Med. 2008;31(5):551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Inpatient Sample (NIS) overview. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality; Rockville, MD: Available at: https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed April 20, 2017. [Google Scholar]
- 18.Carlsson ME, Gunningberg L. Predictors for development of pressure ulcer in end-of-life care: a national quality register study. J Palliat Med. 2017;20(1):53–58. [DOI] [PubMed] [Google Scholar]
- 19.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 20.Ho DE, Imai K, King G, et al. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal. 2007;15(3):199–236. [Google Scholar]
- 21.Dreyfus J, Gayle J, Trueman P, et al. Assessment of risk factors associated with hospital-acquired pressure injuries and impact on health care utilization and cost outcomes in US hospitals. Am J Med Qual. 2017. [DOI] [PubMed] [Google Scholar]
- 22.Goudie A, Dynan L, Brady PW, et al. Costs of venous thromboembolism, catheter-associated urinary tract infection, and pressure ulcer. Pediatrics. 2015;136(3):432–439. [DOI] [PubMed] [Google Scholar]
- 23.Klein EY, Jiang W, Mojica N, et al. National Costs Associated with Methicillin-susceptible and Methicillin-resistant S. aureus Hospitalizations in the United States, 2010–2014. Clin Infect Dis. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality; Rockville, MD: Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed April 28, 2017. [Google Scholar]
- 25.Cost-to-Charge Ratio Files (CCR). Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality; Rockville, MD: Available at: https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed April 20, 2017. [Google Scholar]
- 26.Bureau of Labor Statistics. Consumer price index. Available at: https://www.bls.gov/cpi/. Accessed May 15, 2017.
- 27.Ho DE, Imai K, King G, et al. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28. [Google Scholar]
- 28.Margolis JM, Juneau P, Sadosky A, et al. Health care resource utilization and medical costs of spinal cord injury with neuropathic pain in a commercially insured population in the United States. Arch Phys Med Rehabil. 2014;95(12):2279–87. [DOI] [PubMed] [Google Scholar]
- 29.Dicianno BE. 21st century challenges to the provision of health care to adults with spina bifida: a rehabilitation approach. Arch Phys Med Rehabil. 2014;95(9):1601–1602. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Clinical Classifications Software (CCS) diagnosis codes associated with hospitalizations of patients with spina bifida and pressure injuries.