Abstract
Objective:
This study examines the prevalence and risk factors associated with risky sexual behaviors in community college students.
Participants:
A diverse sample of 18–19-year-old community college students (N = 264).
Methods:
Baseline data from an online prevention program administered in 2015.
Results:
Community college students in this sample disproportionately experienced sexual assault and were unlikely to test for STIs. Higher intentions to engage in risky sexual behaviors were associated with gender and sexual experience, but also with having lower intentions to communicate with a sexual partner about pregnancy and STIs, and having higher gender norm endorsement.
Conclusions:
Older adolescents attending community colleges may be at high risk for poor sexual health outcomes, and appropriate theory-based education should be tailored to meet the needs of these underserved students.
Keywords: community college, risky sexual behavior, health education, sexual health knowledge, older adolescents
Risky Sexual Behaviors Among Older Adolescents
Adolescence, typically defined as the period from 10–19 years of age, is a critical time for social, emotional, and cognitive development, as well as self-exploration. When adolescents transition from high school to college, they enter a unique phase of growth as they pursue different academic challenges, join new social groups, and often explore romantic attachments. Although many adolescents have already become sexually active by the time they graduate high school,1 sexual exploration oft6en continues and becomes more likely during older adolescence. Older adolescence, defined as the period from 18–19 years of age for the purposes of this paper, is therefore a critical period of development to study.
While many older adolescents practice safe sex, a substantial portion of young people take sexual risks. According to self-reports from sexually active high school seniors, about 16% did not use any method of pregnancy prevention, and as many as 21% used drugs or consumed alcohol before or during the last time they engaged in sexual intercourse.2 Among sexually active 18–19-year-olds who are not trying to conceive, only about 40% report consistent and correct use of contraception.
Risky sexual behaviors, such as unprotected sex, intoxicated sex, or incorrect use of contraception, are alarmingly pervasive in older adolescents3,4 and put individuals at increased risk for poor health outcomes, such as sexually transmitted infections (STIs), sexual assault, and unintended pregnancy. Of all teen pregnancies, two-thirds occur among 18- to 19-year-olds.5 Adolescents and young adults (15–24) also account for a substantial proportion of all new HIV/AIDS infections in the U.S.6 HPV infection is also widespread among sexually active male and female undergraduates,7,8 which can lead to cancer in both men and women.
Community College Populations
Community colleges are two-year, public institutions that offer more affordable higher education compared to four-year colleges. Community colleges also typically enroll a diverse population of students;9 nearly half of community college students in the U.S. are from racial minority groups, and over a third are first-generation college students.9 While community college students make up nearly half of all undergraduates in the U.S.,9,10 they are often overlooked in sexual health research. For example, the American College Health Association’s National College Health Assessment (ACHA-NCHA), the pre-eminent annual college health survey, only surveyed three, two-year institutions out of 51 colleges and universities total.9 That means community colleges make up less than 6% of the ACHA-NCHA sample, despite enrolling about half of all undergraduates in the U.S.9
The limited data on the sexual behaviors of community college students suggest they may be at an increased risk for poorer sexual health outcomes. Some studies indicate that, in comparison to students enrolled in four-year institutions, these students are less likely to consistently or correctly use contraception, and are more likely to be sexually active and have casual sex.11–13 There are also insufficient preventive services and sexual health resources at community colleges,10,14,15 and only 20% of students at two-year institutions, compared to 33% of students at four-year institutions, report receiving pregnancy prevention information.3 With such limited resources, it is no surprise that community college students in some areas of the country are twice as likely to become unintentionally pregnant after enrolling in college compared to the average four-year college student.11,16
Gender Differences
Sexual risk behaviors often differ by gender.17 For example, 18–24-year-old male college students at both traditional four-year and two-year institutions tend to have had more lifetime sexual experience and a higher number of casual partners than their female counterparts.13 Men are also generally more likely to engage in risky sexual behaviors,18 including intoxicated sex.19,20 While some gender differences may be attributable to biological factors, the social environment plays an influential role as well. Gender norms, the standards or expectations that a dominant culture assigns to men and to women respectively, also influence behavior. An example of a gender norm is the expectation for young men to act brave, strong, or aggressive, while young women are expected to be polite, demure, or nurturing. Some adolescents may follow gender norms in order to be accepted by their peers, but gender norm adherence can also lead to lower self-esteem and perceived pressure to engage in stereotypical gendered behaviors21, including risky or unsatisfying sexual behaviors.22 While gender differences in risk-taking have been well-studied among four-year college populations, it is unclear if these findings are generalizable to community college students.
Theory of Reasoned Action
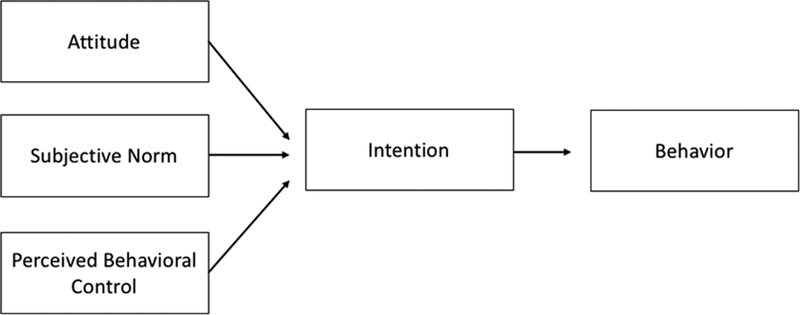
In addition to considering gender differences, health behavior theory must also guide the study of sexual risk behaviors. The Theory of Planned Behavior, proposed by Ajzen (1985) as an elaboration on Fishbein’s (1980) Theory of Reasoned Action, is a relevant tool for measuring the constructs and factors that influence risky behavior. The combined Theory of Reasoned Action and Planned Behavior (TRA/TPB) posits that attitudes, perceived norms, and perceived behavioral control (self-efficacy) contribute to intentions to perform a behavior (see Figure 1).23,24 There have been other adjustments and evolutions to TRA/TPB; while knowledge was not originally included in TRA/TPB, it was later added in the early 2000s to create the Integrated Behavioral Model.23 TRA/TPB and the Integrated Behavior Model have both been successfully applied to predict behavior change related to sexual risk-taking.23,25,26 Social Norms Theory has also grown out of TRA/TPB, and suggests that higher perceived rates of sexual activity in peers increases the likelihood an individual will engage in sexual risk behaviors themselves.27
Figure 1.
Theory of Reasoned Action and Planned Behavior (TRA/TPB)
According to TRA/TPB, intention is a strong predictor of actual behavior, and can be used as a proxy for predicting future behavior when true behavioral measures are unavailable.23,28 Models for behavioral intention are based on an assumption of rational choice, otherwise known as “value-expectancy theories.” However, these theories do not fully explain decision-making for arousal-associated behaviors—when there is momentary temptation or arousal, adolescents may be guided more by whim or impulse than by reason.29 Despite these limitations, there is still great value in applying these theories to measure risk. Numerous recent meta-analyses have found that TRA/TPB is still a relevant, efficacious theory that can help to predict and explain sexual risk behaviors.25,26
The Current Study
Older adolescents enrolled in community colleges are at high risk for poor sexual health outcomes. This population is underserved and underrepresented in research, a gap which this paper attempts to address. While Trieu, Bratton, & Marshak11 conducted a preliminary examination of risky sexual behaviors in community college students, their sample included only heterosexual students who were already sexually active. The present study includes students who identify as sexual minorities as well as students who are not yet sexually active. It also focuses exclusively on older adolescents aged 18–19-years old, a time of rapid romantic and sexual development.30
This article presents an exploratory study of community college students designed to (1) assess the prevalence of sexual history and current behaviors (e.g. experience of sexual assault and abusive relationships, history of STI testing), and (2) identify factors that are associated with intentions to engage in risky sexual behaviors in the future. The results of this study can inform future educational policy and health promotion endeavors by helping to prioritize intervention targets and identify subgroups of community college students at high risk for negative health outcomes.
METHODS
Procedures
The authors performed an analysis of secondary, cross-sectional pretest data collected in an IRB-approved randomized controlled trial, which was conducted to examine the effectiveness of an online sexual health program for community college students. The original efficacy study used a convenience sample from eight community college campuses representing four urban and four rural counties in one state in the Southeastern U.S. Inclusion criteria were defined as: being 18 or 19 years old and being enrolled as a community college student (as documented by possession of a current student identification card or college email address) at one of the participating campuses. Exclusion criteria included not being fluent in English or not having access to a smartphone or tablet.31
Participants
A total of 264 students completed the pretest questionnaire from April-December, 2015. Between 12 and 52 students were recruited from each of the eight participating campuses.
Table 1 presents the demographic characteristics of the students in the sample. This sample was 56% female, with a mean age of 18.5 (SD = 0.5). The sample was racially and economically diverse, with over a third of participants reporting that they qualified for a Pell grant and the majority of respondents identifying with racial or ethnic minority group. Regarding racial self-identification, just over half of students identified as white, and a quarter of students identified as Black. For ethnicity, one in five students identified as Hispanic or Latino. Both the racial composition and proportion of students who identified as heterosexual in the sample were similar to national estimates for community colleges.9,32 Half of the students identified as Christian, while only 10% of students identified as a member of another religion, including Muslim, Jewish, Hindu, Buddhist, Mormon, or Jehovah’s Witness. Over a third of the students identified as agnostic, atheist, or unsure about their religious affiliation. Despite the requirement for participants to be fluent English speakers, no one who was approached or who contacted the research team to participate in the study was excluded due to lack of English fluency. A number of participants, however, did speak English as a second language and/or were foreign born.
Table 1.
Demographic Characteristics (N = 264)
| Characteristic | N | % |
|---|---|---|
| Age | M = 18.5, SD = 0.5 | Range = 18–19 |
| Gender | ||
| Female | 147 | 56% |
| Male | 109 | 41% |
| Trans gender queer, or gender questioning | 7 | 3% |
| Race / Ethnicity* | ||
| White | 145 | 55% |
| Black | 68 | 26% |
| Hispanic / Latino | 54 | 20% |
| Asian | 10 | 4% |
| American Indian / Alaska Native | 6 | 2% |
| Native Hawaiian/Pacific Islander | 3 | 1% |
| More than one race | 59 | 22% |
| Sexual orientation | ||
| Heterosexual | 217 | 84% |
| Gay/Lesbian | 3 | 1% |
| Bisexual | 21 | 8% |
| Asexual | 5 | 2% |
| Queer | 8 | 3% |
| Unsure | 4 | 2% |
| Religion | ||
| Protestant | 87 | 38% |
| Catholic | 38 | 17% |
| Other religion (Muslim, Jewish, Hindu, Buddhist, Jehovah’s Witness, Mormon) | 23 | 10% |
| Other (agnostic, atheist, unsure) | 80 | 35% |
| Socioeconomic Status | ||
| Low income (Pell grant eligible) | 107 | 41% |
| Highest level of parental education | ||
| Some high school | 15 | 6% |
| Finished high school | 29 | 11% |
| Some beyond | 62 | 24% |
| Finished college | 109 | 42% |
| School beyond college | 45 | 17% |
Respondents may check more than 1 response; percentages add to over 100%
Lifestyle characteristics for students in the sample can be found in Table 2. Most respondents were fulltime students, lived with a parent or guardian, and were not international students. Most students were also on their parent’s health insurance plan. Two students reported that they were experiencing homelessness. The sample was split between students who reported they were single and students being in a committed dating relationship. A small number of students reported having children.
Table 2.
Lifestyle Characteristics (N = 264)
| Characteristic | n | % |
|---|---|---|
| Student status | ||
| Full-time | 218 | 83% |
| International student | ||
| Yes | 10 | 4% |
| Insurance | ||
| Parent’s plan | 194 | 79% |
| Own plan | 19 | 8% |
| Other plan | 13 | 5% |
| No health insurance | 20 | 8% |
| Housing* | ||
| With parent or guardian | 217 | 82% |
| With spouse/romantic partner | 16 | 6% |
| With another roommate | 18 | 7% |
| Alone | 3 | 1% |
| Experiencing homelessness | 2 | 1% |
| Has children | ||
| Yes | 5 | 2% |
| Not sure | 5 | 2% |
| Relationship Status | ||
| Single | 142 | 55% |
| Committed relationship | 110 | 43% |
| Married | 2 | 1% |
| Separated or divorced | 2 | 1% |
Respondents may check more than 1 response; percentages add to over 100%
Measures
Background characteristics
Demographic characteristics - Participants responded to questions about how they identify according to their race, ethnicity, gender, sexual orientation, and religious affiliation. Pell Grant eligibility was used as a reliable measure of socioeconomic status.33,34 In the analyses, the variable on Pell Grant eligibility was dichotomized as 0 = students who were not eligible or did not know their eligibility, and 1 = students who reported that they were eligible. Information was also collected on relationship status, asking students to report if they were in a committed dating relationship, single, married, separated, or divorced. Students were also asked to report their sexual orientation. For the variable on sexual orientation, all results are reported in Table 1. For the analysis, sexual orientation was dichotomized to 0 = heterosexual, 1 = students who identified as gay, lesbian, bisexual, asexual, queer, or unsure. Students also reported the highest level of education achieved by their parents. For the analysis, the variable for parent education was dichotomized to 0 = neither parent obtained a college degree, and 1 = one or both parents had a college degree or more.
Sexual history - Students were asked about their previous sexual experience (anal, vaginal, or oral sex; 0 = no, 1 = yes), and whether they had used a condom during their last sexual encounter. Self-reported data were also collected on whether participants had ever contracted an STI, had ever been formally tested for an STI, or had ever received the HPV vaccine.
Sexual assault and abusive relationships - Students reported whether they had experienced unwanted sexual touching (attempted or completed), or if they had experienced unwanted penetration (attempted or completed) within the last 12 months. Participants also self-reported past 12-month involvement in a physically or emotionally abusive relationship.
Outcome of interest
Intentions to engage in risky sexual behavior - An additive risk index was used to assess the self-reported likelihood for a participant to engage in a range of risk behaviors in the next six months. The questions were adapted from existing measures.35,36 The risk behaviors examined included: having sex with a casual partner; having sex with someone of unknown STI status; going out with the intent of having sex; leaving a party or social event with someone they had just met; using alcohol or drugs before or during a sexual encounter; having sex with someone who had multiple sexual partners in the past; having sex with someone who was engaging in sex with others during the same time period; and having sex themselves with multiple sexual partners during the same time period. Each of the eight questions had a 4-item, Likert response scale (1 = Not at all likely, 2 = Unlikely, 3 = Likely, 4 = Extremely likely).
Cognitions related to sexual health
Intentions to communicate with a partner – Intentions to communicate with a sexual partner about STIs and pregnancy (α = .87) was assessed using fiveitems35, 36. The question stem was, “If you were to decide to engage in sexual activity with a new partner in the next six months, how likely would you be to…” Examples of items include, “talk with a partner about HIV/AIDS or other STIs?”, “talk with a partner about a pregnancy plan?”, or “talk with a partner about past sexual partners?” Each of the questions was rated on a 4-point Likert response scale (1 = Very unlikely, 4 = Extremely likely).
Intentions to get tested for STIs – One item captured students’ intentions to get tested for STIs: “If you were to decide to engage in sexual activity with a new partner in the next six months, how likely would you be to get tested for STIs?” The question had a 4-point Likert response scale (1 = Very unlikely, 4 = Extremely likely), and for the analyses it was dichotomized such that 0 = Very unlikely/Unlikely, and 1 = Likely/Extremely likely.
Self-Efficacy to use a condom – One adapted self-efficacy question35 assessed participants’ confidence in their ability to use a condom. Students responded to the statement, “I can use a condom correctly or explain to my partner how to use a condom correctly.” The question had a 4-point Likert response scale (1 = Strongly disagree, 4 = Strongly agree). For the analysis, this was dichotomized to 0 = Strongly disagree/Disagree, and 1 = Strongly agree/Agree.
Perceived Gender Norms – Five items36 assessed normative beliefs about gender roles (α=.59). Example items include “Raising children is primarily a woman’s responsibility”, and “A man who cries in front of a woman is making a fool of himself.” Participants were asked to indicate how much they agreed with each statement on a 4-point Likert response scale (1 = Strongly disagree, 4 = Strongly agree).
Descriptive norms around sexual behavior - Four items (α=.80) assessed perceived peer behaviors around sexual activity.37 Students estimated what percentage of people their age were having sex; had unprotected sex at last intercourse; had sex with a casual partner; and had sex while high on drugs or while intoxicated.
Knowledge - Participant knowledge of sexual risks and protections was assessed using the Knowledge of Sexual Risk and Protection questionnaire38, consisting of 23 fact-based multiple choice questions. Items included “How can someone get an STI?” and “True or false: You can tell if someone has an STI by looking at them.” Correct responses were summed to derive a total knowledge score.
Overview of Statistical Analyses
Basic descriptive statistics were calculated to assess sexual history and current behaviors. An ANOVA was performed to confirm that the outcome of interest, intentions to engage in risky sexual behavior, did not differ significantly across the eight campuses where data were collected (F = 0.85, p = 0.55). Because there was no significant difference across campuses, a multi-level model was not required in the main analyses., Both bivariate and multivariate linear regression models were used to assess which factors were associated with intentions to engage in risky sexual behaviors. The outcome of interest was considered approximately normally distributed (mean = 12.5, median = 10, mode = 8, skew = 1.1, kurtosis = 0.3). Due to the exploratory nature of this study, the authors developed different multivariate models and presented the most satisfactory model here. First, bivariate linear regression (i.e., an unadjusted model) was conducted between each predictor and the outcome of interest. Based on the results from these analyses, a multivariate model (i.e., an adjusted model) was built. Predictors that were non-significant in the bivariate model, or that had very low adjusted R2 values, were not added to the multivariate model, unless they were deemed to be theoretically relevant and important to the outcome variable. Model parameterization was determined using the contrast statement in SAS, which quantified if a particular variable, or set of variables, improved model fit. For example, adding the race variables as a block did not significantly improve model fit; therefore, they were excluded from the adjusted model.
For the regression models, the race variable was dummy coded so that students who identified as White were compared to all others in the sample. Those who identified as multiracial were separated into their own group to create mutually exclusive categories, while students who identified only as Asian, American Indian, or Pacific Islander were not examined separately due to small numbers. The gender variable was binary, including those who self-identified as male compared to those who self-identified as female. The number of students who self-reported as trans gender queer, or gender questioning (n = 7) was too small to be examined in separate analyses and those students were therefore excluded from the bivariate and multivariate models. Due to missing values in the outcome variable and the binary gender variable, the final analysis dataset consisted of 240 participants.
RESULTS
Descriptive statistics explored the sexual history and sexual health practices of this sample of community college students (see Table 3). Over two-thirds of the participants reported previous sexual experience (i.e., oral, vaginal, or anal sex). Of those who had ever had sex, the majority had engaged in vaginal sex and oral sex. About a third of sexually active students reported that they had ever had anal sex. For those engaging in vaginal or anal sex, about two-thirds of students reported using a condom during their last sexual encounter. The lowest rates of condom use were reported by female students during their last experience of anal sex, where only a quarter said that the penetrative partner had used a condom.
Table 3.
Sexual History, Pregnancy and STI Protection, and STI Medical History
| Experience | Male students | Female students | ||||
|---|---|---|---|---|---|---|
| n | % (n = 109) |
% sexually active (n = 76) |
n | % (n = 147) |
% sexually active (n = 104) |
|
| Sexual history (ever) | ||||||
| Never had sex | 33 | 30% | - | 43 | 29% | - |
| Oral sex | 72 | 66% | 96% | 96 | 65% | 92% |
| Vaginal sex | 60 | 55% | 80% | 96 | 65% | 91% |
| Anal sex | 22 | 20% | 29% | 40 | 27% | 38% |
| Condom use (last time) | ||||||
| Vaginal sex | 34 | - | 64% of N = 60 | 58 | - | 66% of N = 96 |
| Anal sex | 12 | - | 55% of N = 11 | 11 | - | 28% of N = 40 |
| Medical history (ever) | ||||||
| Had an STI | 2 | 2% | 2% | 7 | 3% | 4% |
| Tested for an STI | 30 | 28% | 33% | 55 | 37% | 52% |
| Vaccinated for HPV | 37 | 34% | 39% | 65 | 44% | 51% |
| Talked with doctor about sexual health | 40 | 37% | 37% | 80 | 54% | 66% |
A small fraction (4%) of students reported having ever had an STI, although only a third of sexually active male students reported they had ever been formally tested. For both males and females, a slightly higher proportion of students had received the HPV vaccine than had ever been tested for STIs. Less than half of females and only a third of males in this sample had received the HPV vaccine. Most students said that they had never talked with a medical professional about sex, contraception, or romantic relationships.
Table 4 shows the reported experience with sexual assault and abusive relationships within the last 12 months. Notably, one out of every ten men and one out of every four women reported having been touched sexually without consent or having experienced an attempt at sexual touching without consent. Three percent of men and 10% of women reported having experienced rape or attempted penetration without consent in the last year. Experience with being in a physically abusive relationship was reported by 4% of men and 8% of women, while emotional abuse within the last year was reported by 8% of men and 20% of women.
Table 4.
Sexual Assault (Attempted and Completed) and Abusive Relationships
| Experience (last 12 months) | Male students | Female students | ||
|---|---|---|---|---|
| n | % | n | % | |
| Sexually touched without consent | 13 | 12% | 36 | 25% |
| Raped and attempted penetration | 3 | 3% | 15 | 10% |
| Emotionally abusive relationship | 9 | 8% | 29 | 20% |
| Physically abusive relationship | 4 | 4% | 11 | 8% |
Bivariate and multivariate linear regression models examined predictors of community college students’ intentions to engage in risky sexual behavior (see Table 5). Gender was significantly related to intentions to engage in risky sexual behaviors in the unadjusted model, such that male students had higher intentions to engage in risky sexual behaviors than female students (p < .0001). After controlling for other covariates, gender was still significantly associated with intentions to engage risky sexual behavior (p < .05). No other demographic variable, including parental educational attainment, Pell Grant eligibility (i.e., socioeconomic status), sexual orientation, or race, were significantly associated with the outcome. The (i.e., vaginal, anal, or oral sex) was associated with greater intentions to engage in risky sexual behaviors in the future. This association remained strong even after controlling for covariates in the adjusted model (p < .0001).
Table 5.
Bivariate and Multivariate Linear Regression Models for the Intentions to Engage in Risky Sexual Behavior in the Next Six Months (N = 240)
| Unadjusted model | Adjusted model 1 adjusted R2 = 0.21 |
Adjusted model 2 adjusted R2 = 0.21 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | Beta-weight | SE | P value | Adjusted R2 | b | Beta-weight | SE | P value | b | Beta-weight | SE | P value | |
| Demographic variables | |||||||||||||
| Gender 0 = Male 1 = Female |
−2.8 | −0.28 | 0.62 | <.0001 | 0.08 | −2.31 | −0.23 | 0.64 | <0.001 | −8.42 | −0.84 | 4.21 | <0.05 |
| Highest parental education 0 = No college degree 1 = College degree or more |
−0.12 | −0.01 | 0.65 | 0.87 | −0.004 | - | - | - | - | - | - | - | - |
| Pell grant eligibility 0 = Not eligible or don’t know 1 = Eligible |
0.40 | 0.04 | 0.66 | 0.54 | −0.003 | 0.63 | 0.06 | 0.60 | 0.3 | 0.68 | 0.07 | 0.60 | 0.26 |
| Sexual orientation 0 = Heterosexual 1 = Not heterosexual |
−0.70 | -0.05 | 0.90 | 0.44 | −0.002 | - | - | - | - | - | - | - | - |
| Race/Ethnicity | |||||||||||||
| White 0 = Everyone else 1 = White |
−0.13 | −0.01 | 0.65 | 0.84 | −0.004 | - | - | - | - | - | - | - | - |
| Black 0 = Everyone else 1 = Black |
0.93 | 0.08 | 0.74 | 0.21 | 0.002 | - | - | - | - | - | - | - | - |
| Hispanic 0 = Everyone else 1 = Hispanic |
0.64 | 0.05 | 0.82 | 0.44 | −0.002 | - | - | - | - | - | - | - | - |
| Mixed 0 = Everyone else 1 = Mixed race |
−0.4 | −0.03 | 0.86 | 0.64 | −0.003 | - | - | - | - | - | - | - | - |
| Behavioral | |||||||||||||
| Had sex previously 0 = No 1 = Has had vaginal, anal, and/or oral sex |
3.14 | 0.29 | 0.67 | <.0001 | 0.08 | 3.23 | 0.30 | 0.6 | <.0001 | 3.07 | 0.28 | 0.67 | <.0001 |
| Cognitions | |||||||||||||
| Self-efficacy to use a condom 0 = Strongly disagree/Disagree 1 = Strongly agree/Agree |
2.28 | 0.14 | 1.03 | <.0001 | 0.01 | 0.66 | 0.04 | 1.01 | 0.52 | 0.65 | 0.04 | 1.02 | 0.52 |
| Intentions to communicate with a partner about pregnancy and STI prevention | −0.35 | −0.23 | 0.10 | <.001 | 0.05 | −0.21 | −0.14 | 0.10 | <.05 | −0.23 | −0.15 | 0.10 | <.05 |
| Intentions to get tested for STIs 0 = Very unlikely/Unlikely 1 = Likely /Extremely likely |
−1.3 | −0.13 | 0.66 | <.05 | 0.01 | −0.60 | −0.06 | 1.02 | 0.52 | −0.60 | −0.06 | 0.66 | 0.37 |
| Perceived peer norms | 0.02 | 0.07 | 0.02 | 0.25 | 0.001 | 0.04 | 0.11 | 0.02 | 0.06 | 0.04 | 0.11 | 0.02 | 0.06 |
| Gender norm acceptance | 2.26 | 0.22 | 0.65 | <.001 | 0.04 | 1.3 | 0.13 | 0.62 | <.05 | 1.33 | 0.13 | 0.62 | <.05 |
| Sexual health knowledge | −0.23 | −0.12 | 0.23 | 0.07 | 0.01 | −0.10 | −0.05 | 0.12 | 0.44 | −0.3 | −0.15 | 0.18 | 0.11 |
| Interaction terms | |||||||||||||
| Sexual health knowledge* Gender | - | - | - | - | - | - | - | - | 0.37 | 0.66 | 0.25 | 0.14 | |
In both the adjusted and the unadjusted model, less intention to communicate with a sexual partner about STIs and pregnancy prevention was associated with higher intentions to engage in risky sexual behaviors (p < .05). Furthermore, greater endorsement of traditional gender role norms was associated with higher intentions to engage in risky sexual behavior (p < .05). According to the models, sexual health knowledge, intentions to get tested for STIs, and self-efficacy to use a condom were not associated with intentions to engage in risky sexual behaviors. Perceived peer norms around sexual activity and risk-taking, however, were close to the significance threshold for an association with intentions to engage in risky sexual behaviors (p < .06).
For both adjusted models, the adjusted R2 value was 0.21– the models account for approximately 21% of the variability seen in intentions for risky sexual behavior. In both adjusted models, gender and having had sex previously had the highest beta weights, and therefore are likely the most influential independent variables in the model.
The second adjusted model (Adjusted Model 2) determined that the effect of sexual health knowledge on intentions does not differ significantly for male students compared to female students. By adding this interaction term, the coefficient for gender increased from −2.31 to −8.59. The second adjusted model suggests that, on average, female students in the sample scored lower on the additive risk index for intentions to engage in risky sexual behavior by 8.59 points compared to males, while holding all other variables constant including the interaction term.
COMMENT
This paper examined the sexual health status and related risk-taking behaviors of a diverse sample of older adolescents enrolled in community college. The results make a significant contribution to our understanding of the behaviors and cognitions associated with risky sexual behavior among community college students by building upon a relatively sparse body of literature. Findings reveal community college students may be at a high risk for experiencing poor sexual health outcomes, and that there may be important risk pathways and intervention points to curb risky sexual behaviors in this underserved population.
The sexual health of community college students
Alarming differences in sexual assault victimization and intimate partner abuse exist between the students in this sample and students attending traditional four-year colleges. Past 12-month experience of rape or attempted penetration without consent was two to three times as high for both male and female students in the present sample compared to average college rates reported by American College Health Association-National College Health Assessment (ACHA-NCHA).32 Experience with being in a physically abusive relationship was also twice as high for both male and female students in the present sample.32 These differences may be attributable in part to the substantial differences in participants’ average age, socioeconomic status, or geographic location. The ACHA-NCHA survey samples students primarily enrolled in four-year institutions across the U.S., representing a range of backgrounds, whereas students in the present study were only recruited from community colleges in the Southeast United States, and many came from low income homes (41%) and identified as racial or ethnic minority students. These demographic differences highlight the fact that community college students constitute a particularly high-risk group of late adolescents for a range of negative sexual health experiences and outcomes.
In the present study, both male and female community college students experienced unwanted sexual advances, attempted penetration, and even rape at disturbingly high rates. In addition to the serious emotional and physical repercussions associated with sexual assault, victims may also be more likely to struggle academically and may eventually drop out of school after an incident.39,40 Thus, the high prevalence of unwanted sexual experiences, including rape, may contribute to the high dropout rates reported by many community colleges.41 Extrapolating from the findings in the present sample, it may be important to directly address risky sexual behaviors and exposure to traumatic sexual experiences on community college campuses to improve both health and educational outcomes. Resources should be dedicated to preventing assault and abusive relationships among community college students and to providing survivors with adequate recovery supports.
While previous research has focused primarily on heterosexual female victims at residential, four-year institutions, information is lacking in the community college setting about victimization, especially among male students. Given the high proportion of male students who reported unwanted sexual experiences, including rape, in the present sample, additional research is urgent and essential to better understand the patterns of perpetration and victimization in the community college setting.
The majority of students in this sample were living with a parent, guardian or other family member, which suggests that campus dormitories may not be the only place where assault and abusive relationships are a problem. It is possible that older adolescents attending community colleges are at equal or elevated risk for assault and/or abuse compared to those who are attending four-year colleges or universities.42 Differences may also be attributable to the lack of education about healthy relationships and a lack of supportive resources on campus for students attending community college, although additional research is required in this area and no definitive conclusions can be made at the present time.
This study found that many students reported engaging in risky sexual behaviors, such as anal sex. About one-fourth of female students in the sample reported having engaged in anal sex. While these estimates are comparable to national estimates,43,44 and anal sex among college populations seems to be on the rise,44,45 many female students reported that their penetrative partner had not used protection. This is a particular health concern given that anal sex increases the risk for acquiring certain STIs including syphilis and chlamydia. Anal sex is also the single riskiest sexual behavior for transmitting HIV, especially for the receptive partner.46 Future research should examine these emerging patterns in sexual activity among college students more closely. Education around safe anal sex is important for students of all sexual identities, with particular emphasis on the benefits of condom use. Some research suggests there could be a link between unprotected anal sex and coercion, such that experiences of anal sex may often be unwanted among at-risk heterosexual female adolescents.47 Future research should consider assessing how coercion, sexual pressure, or lack of communication shape the prevalence of anal sex and the use of protection during anal sex in this population.
The findings in this study related to STIs also revealed a potentially urgent need for screening and preventative education among community college students. Very few participants reported they had received the HPV vaccine or had ever been tested for an STI. According to 2013 data from the National College Health Assessment-II, nearly 75% of females and 50% of male students aged 18- to21-years-old have received the HPV vaccine,48 compared to less than half of females and only a third of males in this sample. The American Academy of Pediatrics estimate that nearly 1 in 4 adolescent females aged 14- to 19-years-old have had an STI.49 While only about 4% of students in this sample reported ever having an STI, they also reported low rates of STI testing. It is possible that the findings on STI rates in this study are underestimated, given that many students are unaware of their STI status. Among sexually active males in the current sample, only a third reported ever being tested for an STI in their lifetime compared to 38% of male community college students in California, who reported being tested for HIV in the past year.11 The California study only included sexually active, heterosexual community college students, and these higher rates of recent testing may be due in part to variations in student demographics and geographic location. For example, California implemented the Health Services Association – California Community Colleges (HSACCC), which works specifically to improve the health of community college students statewide, and could have bolstered recent testing rates.
Factors associated with future risky sexual behaviors
As expected, gender differences were found in intentions to engage in risky sexual behaviors. Male students in the sample were more likely to report higher intentions for sexual acts which may include multiple partners, casual sex, or intoxicated sex. Similarly, endorsement of traditional gender role norms was associated with future risky sexual behaviors. Researchers have argued that internalized gender norms may lead men to pursue the masculine ideal of sexual adventurer, while women may feel pressure pursue the stereotyped notion of feminine passivity.22 This could contribute to pressure for men to have more casual relationships, while women may feel more pressure to acquiesce on important sexual decisions.22 Gender norms reinforce imbalanced power dynamics between heterosexual partners, but they also may discourage healthy communication between sexual partners. One of the stereotypes of masculinity is to be unemotional and terse;50 men are acculturated even as children to avoid uncomfortable or emotional conversations,51 and aspiring to the stereotype of taciturn masculinity may leave male students more hesitant and/or less equipped to talk to their partners about STIs, pregnancy prevention, and even the emotional consequences of engaging in sexual intercourse. Some research indicates that endorsing traditional gender norms among men may be highly correlated with aggression, antisocial behavior, and low emotional awareness, but also with earlier sexual initiation and less condom use.52
Based on these preliminary findings, interventions could be developed to help older adolescents deconstruct the social messages about gender expectations they receive through media and other cultural avenues. Popular media are inundated with images that convey gender norm expectations,53 and providing youth with media literacy education is one promising approach to disrupt acceptance and adherence to rigid gender role norms.54
Another factor that was significantly associated with higher intentions for engaging in risky sexual behaviors was past sexual experience. Past behavior tends to be a strong predictor of future behavior, and results suggest this may hold true for the present sample. According to other research, adolescents who become sexually active at earlier ages often have a greater number of sexual partners and more frequent intercourse compared to their peers,55 thus increasing their risk for poor sexual health outcomes. Sexual education and support for adolescents should begin early (i.e., before first intercourse) in order to delay initiation of sexual activity. Additional education and resources may still be relevant to equip students who are already sexually active with the skills they need to engage in sex while minimizing risk, or to consider refraining from additional sexual encounters.
Not surprisingly, lower intention to communicate with a sexual partner about important sexual health topics was significantly associated with higher intentions to engage in future risky sexual behaviors. During risky sexual encounters (e.g., sex with person of unknown STI status, sex while intoxicated, sex with a casual partner), the need for communication about sexual health is of paramount importance. However, in the current study, community college students who were engaging in more risky sexual behaviors were less likely to communicate with their partner about contraception, STI history, sexual history, or pregnancy prevention. Educators should be positioned to teach and model communication skills by, for example, providing students with scripts that they could use for practicing sexual health communication. The development and mastery of these skills through role play and group discussion could ultimately build stronger intentions to discuss sexual health. Open dialogue between potential sexual partners may also have the added benefit of reducing sexual assaults as the negotiation of consent is made more intentional and explicit, although additional study in this area is needed.
Several factors in these analyses were not associated with intentions for future risky sexual behaviors. The findings revealed that students in the sample who were more likely to engage in risky sexual behaviors were similarly knowledgeable compared to their peers about sexual health risks and/or medical outcomes. As other research has suggested, simply teaching fact-based information about the consequences of risky sexual behavior may not be enough to deter future risk behaviors.56–58 Similarly, plans for STI testing and self-efficacy for condom use were not associated with students’ reported likelihood of future risky sexual behaviors. Rather than discount these arguably important factors related to sexual health, future research could continue to examine how a combination of knowledge and skills-based education, which is inclusive and targeted to meet the needs of higher-risk groups, can prevent sexual risk behaviors.
While other studies have suggested sexual behavior may differ by race, ethnicity,59,60 or sexual orientation,61 this study did not find that demographic characteristics were significantly associated with intentions to engage in risky sexual behavior. Additionally, measures of SES, such as Pell Grant eligibility or parental educational attainment, were not significantly related to intentions around sexual risk behaviors. For racial or sexual minority students and students from low SES backgrounds that do engage in risky sexual behavior, they may have fewer resources or supports to manage negative social-emotional outcomes, or to mitigate health problems resulting from these risky behaviors (fewer resources due to financial barriers and/or discrimination). Examining how demographic characteristics differ for observed sexual behavior and sexual health outcomes in this population is a direction for future research, as most research has been conducted with majority heterosexual white samples attending four-year institutions.62,63 It is possible disparities in sexual health outcomes exist for this group, even if demographic factors are not significantly associated with intentions to engage in risky sexual behavior.
This study adds to the literature supporting that the Theory of Reasoned Action updated by the Theory of Planned Behavior (TRA/TPB) provides a useful but imperfect framework for understanding the cognitions related to risky sexual behaviors. This theory connects attitudes, norms, and self-efficacy to intentions across sexual behaviors, but does not address the role of affect in decision making. This study found some of the TRA/TPB-informed variables to be significantly associated with sexual risk behaviors, but not all. Future research should also explore the role of affect and arousal in sexual decision making, in order to test theory that does not assume purely rational choice.
Limitations
This study had several limitations. Data were only collected from community college students who owned a cell phone or tablet with internet access, criteria met by approximately two-thirds of all American community college students.64 The students without smartphone access may differ from students included in the study on important behaviors and outcomes. Students were approached and voluntarily chose to participate, and therefore those who elected to participate may have been more informed about sexual health or more open-minded to sexual health education efforts. Despite these limitations, the sample was racially and economically diverse, and was drawn from a group of community college students, which constitutes an understudied, underserved, and high-risk population. While students were sampled from multiple schools in both urban and rural areas, this study only surveyed participants from a single state.
In addition, the outcome measure (i.e., intentions) may underestimate the true proportion of students actually engaging in risky sexual behavior. The outcome measure, was captured using an additive risk index that asked participants how much they felt it was likely they would engage in a number of risky sexual behaviors (e.g., having sex with someone of unknown STI status, having sex with someone they had just met) within the next six months. According to some studies, people may be more willing to engage in these behaviors or act irrationally in the moment (due to arousal, when visually primed, or peer-pressured), but have lower explicit intentions to engage in these behaviors in the abstract.65 Future research might examine willingness to engage in risky sexual behaviors, under a range of interpersonal and contextual conditions, in addition to assessing behavioral intentions. Furthermore, this study uses intentions as a proxy for actual behavior. The data were also self-reported and therefore, may represent a social desirability bias for sensitive topics such as sexual activity, intentions to engage in risky behaviors, and STI disclosure.
Methodologically, the study utilized a cross-sectional design, and a causal relationship between the independent and dependent variables could not be evaluated. Other cognitive predictors of intentions could not be included in the adjusted model because they were very highly correlated with each other. For example, the investigators were interested in understanding the relationship between rape myth acceptance and intentions to engage in risky sexual behavior. Rape myth acceptance, however, was both highly correlated with gender and with gender norm acceptance, so this variable could not be included in the adjusted regression models. Furthermore, the small size of the sample prevented the inclusion of mediators and moderators in the analysis. Gender likely operates on sexual intentions through a number of cognitions, but it was not possible to parse out these relationships in the present study. Future research should use larger sample sizes when possible to better understand the mediation and moderation pathways in sexual risk-taking behaviors.
Conclusions
While research and resources around sexual health are typically focused on students attending four-year colleges, we cannot continue to ignore the other half of undergraduates in the United States who attend two-year community colleges. Even when older adolescents are not living in a residential dormitory at a four-year institution, they are still at risk—perhaps even at higher risk—for experiencing poor sexual health outcomes. Notably, these community college students may be not only engaging in risky sex equally if not more than other college students, but they also have access to fewer sexual health resources. Furthermore, the national dialogue on sexual assault has largely excluded mention of community college students,63 yet there is growing evidence that they are in great need of education and support regarding their sexual health.
This study has identified a number of topics that could be addressed in educational programming for students. First, community college students may benefit from help finding appropriate and practical ways to have conversations with a sexual partner around STIs and pregnancy prevention. Educational programs could also focus on reducing the negative impact of gender role stereotypes and promoting more equitable relationships.66 Sharing knowledge about heathy relationships, building skills around soliciting consent to engage in sexual behaviors, and helping students stand up to prevent abusive or coercive relationships should be central tenets of any sexual health programming. This is especially important given the alarmingly high prevalence of recent experiences with sexual assault, rape, and abusive relationships in this study sample. At the policy level, it may be important to partner with local health departments to provide sexual health resources on community college campuses such as STI testing, HPV vaccinations, condoms, and referrals to health services. Such efforts are poised to substantially improve the health status of community college students.
Acknowledgments:
Research reported in this paper was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number R21DA035665 to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Tracy M. Scull, innovation Research & Training, Durham, NC.
Elyse M. Keefe, innovation Research & Training, Durham, NC.
Julie M. Kafka, University of North Carolina, Chapel Hill, NC.
Christina V. Malik, innovation Research & Training, Durham, NC.
Janis B. Kupersmidt, innovation Research & Training, Durham, NC.
Sources
- 1.McNeely C, Blanchard J. The Teen Years Explained: A Guide to Healthy Adolescent Development. In: Health CfAHaJHBSoP, ed2009
- 2.Kann L, McManus T, Harris WA, et al. Youth Risk Behavior Surveillance - United States, 2015. Centers for Disease Control;2016. [DOI] [PubMed] [Google Scholar]
- 3.Kaye K, Suellentrop K, Sloup C. The Fog Zone: How Misperceptions, Magical Thinking, and Ambivalence Put Young Adults at Risk for Unplanned. Washington DC: National Campaign to Prevent Teen and Unplanned Pregnancy;2009. [Google Scholar]
- 4.Caldeira KM, Arria AM, O’Grady KE, Zarate EM, Vincent KB, Wish ED. Prospective associations between alcohol and drug consumption and risky sex among female college students. Journal of Alcohol and Drug Eduation. 2009;53(2). [PMC free article] [PubMed] [Google Scholar]
- 5.Kost K, Henshaw S, Carlin L. U.S. Teenage Pregnancies, Births and Abortions: National and State Trends and Trends by Race and Ethnicity. Guttmacher Institute;2010. [Google Scholar]
- 6.Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187–193. [DOI] [PubMed] [Google Scholar]
- 7.Winer RL. Genital human papillomavirus infection: Incidence and risk factors in a cohort of female university students. American Journal of Epidemiology. 2003;157(3):218–226. [DOI] [PubMed] [Google Scholar]
- 8.Saslow D, Castle PE, Cox JT, et al. American Cancer Society Guideline for Human Papillomavirus (HPV) Vaccine Use to Prevent Cervical Cancer and Its Precursors. CA: a cancer journal for clinicians. 2007;57(1):7–28. [DOI] [PubMed] [Google Scholar]
- 9.American Association of Community Colleges: 2016 Fact Sheet. 2016.
- 10.Habel MA, Becasen JS, Kachur R, Eastman-Mueller H, Dittus PJ. Community colleges: Rethinking STD prevention for the nontraditional college campus. Community College Journal of Research and Practice. 2016:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trieu SL, Bratton S, Marshak HH. Sexual and Reproductive Health Behaviors of California Community College Students. Journal of American College Health. 2011;59(8). [DOI] [PubMed] [Google Scholar]
- 12.Attin OM. Comparing Two-Year Community College and Four-Year University Student Social and Behavioral Sexually Transmitted Infection Risk Factors: College of Health Sciences, Walden University; 2013. [Google Scholar]
- 13.Lyons H, Manning W, Giordano P, Longmore M. Predictors of heterosexual casual sex among young adults. Arch Sex Behav. 2013;42(4):585–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eisenberg ME, Lechner KE, Frerich EA, Lust KA, Garcia CM. Characterizing sexual health resources on college campuses. J Community Health. 2012;37(5):940–948. [DOI] [PubMed] [Google Scholar]
- 15.Kershner S, Flynn S, Prince M, Potter SC, Craft L, Alton F. Using data to improve fidelity when implementing evidence-based programs. J Adolesc Health. 2014;54(3 Suppl):S29–36. [DOI] [PubMed] [Google Scholar]
- 16.Association TACH. American College Health Association - National College Health Assessment Spring 2007 Reference Group Data Report (Abridged). Journal of American College Health. 2008;56(5). [DOI] [PubMed] [Google Scholar]
- 17.Petersen JL, Hyde JS. A meta-analytic review of research on gender differences in sexuality, 1993–2007. Psychological Bulletin. 2010;136(1):21–38. [DOI] [PubMed] [Google Scholar]
- 18.Dir AL, Coskunpinar A, Cyders MA. A meta-analytic review of the relationship between adolescent risky sexual behavior and impulsivity across gender, age, and race. Clin Psychol Rev. 2014;34(7):551–562. [DOI] [PubMed] [Google Scholar]
- 19.Mair C, Ponicki WR, Gruenewald PJ. Reducing risky sex among college students: Prospects for context-specific interventions. AIDS Behav. 2016;20 Suppl 1:S109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. 2009;10(4):376–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Egan SK, Perry DG. Gender identity: A multidimensional analysis with implications for psychosocial adjustment. Developmental Psychology. 2001;37(4):451–463. [DOI] [PubMed] [Google Scholar]
- 22.Shearer CL, Hosterman SJ, Gillen MM, Lefkowitz ES. Are Traditional Gender Role Attitudes Associated With Risky Sexual Behavior and Condom-related Beliefs? Sex Roles. 2005;52(5–6):311–324. [Google Scholar]
- 23.Glantz K Health Behavior and Health Education: Theory, Research, and Practice. 4 ed. San Fransisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 24.Manstead AS, van eekelen SAM. Distinguishing between perceived behavioral control and self-efficacy in the domain of academic achievement intentions and behaviors. Journal of Applied Social Psychology. 1998;28(15):1375–1392. [Google Scholar]
- 25.Tyson M, Covey J, Rosenthal HES. Theory of planned behavior interventions for reducing heterosexual risk behaviors: A meta-analysis. Health Psychology. 2014;33(12):1454–1467. [DOI] [PubMed] [Google Scholar]
- 26.Sheeran P, Maki A, Montanaro E, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychology. 2016;35(11):1178–1188. [DOI] [PubMed] [Google Scholar]
- 27.Scholly K, Katz AG, Jan, Holck PS. Using social norms theory to explain perceptions and sexual health behaviors of undergraduate college students: An exploratory study. Journal of American College Health. 2005;53(4):159–166. [DOI] [PubMed] [Google Scholar]
- 28.Predicting Sutton S. and explaining intentions and behavior: How well are we doing? Journal of Applied Social Psychology. 1998;28(15):1317–1338. [Google Scholar]
- 29.Ariely D Predictably Irrational: The Hidden Forces that Shape Our Decisions. New York: Harper Perennial; 2010. [Google Scholar]
- 30.Fromme K, Corbin WR, Kruse MI. Behavioral risks during the transition from high school to college. Dev Psychol. 2008;44(5):1497–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Authors. 2018.
- 32.American College Health Association. National College Health Assessment II: Fall 2016 Reference Group Data Report. Hanover, MD: American College Health Association;2016. [Google Scholar]
- 33.Wei CC, Horn L. Federal Student Loan Debt Burden of Noncompleters. National Center for Education Statistics;2013. [Google Scholar]
- 34.Douglass JA, Thomson G. The poor and the rich: A look at economic stratification and academic performance among undergraduate students in the United States. Berkeley, CA: Center for Studies in Higher Education at University of California, Berkley;2008. [Google Scholar]
- 35.Soet JE, Dudley WN, Dilorio C. The effects of ethnicity and perceived power on women’s sexual behavior. Psychology of Women Quarterly. 1999;23:707–723. [DOI] [PubMed] [Google Scholar]
- 36.Brown MJ, Gladstone N Development of a Short Version of the Gender Role Beliefs Scale. International Journal of Psychology and Behavioral Sciences. 2012;2(5):154–158. [Google Scholar]
- 37.Turchik JA, Garske JP. Measurement of Sexual Risk Taking Among College Students. Archives of sexual behavior. 2007;38(6):936–948. [DOI] [PubMed] [Google Scholar]
- 38.Scull TM, Kupersmidt JB, Malik CV, Keefe EM. Examining the efficacy of an mHealth media literacy education program for sexual health promotion in older adolescents attending community college. Journal of Community Psychology. 2018;66(3):165–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jordan CE, Combs JL, Smith GT. An Exploration of Sexual Victimization and Academic Performance Among College Women. Trauma Violence Abuse. 2014;15(3):191–200. [DOI] [PubMed] [Google Scholar]
- 40.Amar AF, Gennaro S. Dating Violence in College Women. Nursing Research. 2005;54(4):235–242. [DOI] [PubMed] [Google Scholar]
- 41.Schneider M, Yin L. The Hidden Costs of Community Colleges. Washington, D.C.: American Institutes for Research;2011. [Google Scholar]
- 42.Zweig JM, Barber BL, Eccles JS. Sexual Coercion and Wellbeing in Young Adulthood: Comparisons by Gender and College Status. Journal of Interpersonal Violence. 1997;12(2). [Google Scholar]
- 43.Chandra A, Copen CE, Mosher WD. Sexual behavior, sexual attraction, and sexual identity in the United States: Data from the 2006–2010 National Survey of Family Growth. International Handbook on the Demography of Sexuality. Dordrecht: Springer; 2013. [Google Scholar]
- 44.Benson LS, Martins SL, Whitaker AK. Correlates of Heterosexual Anal Intercourse among Women in the 2006–2010 National Survey of Family Growth. J Sex Med. 2015;12(8):1746–1752. [DOI] [PubMed] [Google Scholar]
- 45.Chandra A, Mosher WD, Copen C, Sionean C. Sexual Behavior, Sexual Attraction, and Sexual Identity in the United States: Data From the 2006–2008 National Survey of Family Growth. Centers for Disease Control and Prevention;2011. [PubMed] [Google Scholar]
- 46.Center for Disease Control and Prevention. Anal Sex and HIV Risk. 2016; https://www.cdc.gov/hiv/risk/analsex.html.
- 47.Silverman JG, McCauley HL, Decker MR, Miller E, Reed E, Raj A. Coercive forms of sexual risk and associated violence perpetrated by male partners of female adolescents. Perspect Sex Reprod Health. 2011;43(1):60–65. [DOI] [PubMed] [Google Scholar]
- 48.Thompson EL, Vamos CA, Vazquez-Otero C, Logan R, Griner S, Daley EM. Trends and predictors of HPV vaccination among U.S. College women and men. Prev Med. 2016;86:92–98. [DOI] [PubMed] [Google Scholar]
- 49.Forhan SE, Gottlieb SL, Sternberg MR, et al. Prevalence of sexually transmitted infections among female adolescents aged 14 to 19 in the United States. Pediatrics. 2009;124(6):1505–1512. [DOI] [PubMed] [Google Scholar]
- 50.Antony M The Masculine Century: A Heretical History of Our Time. Bloomington, IN: iUniverse, Inc.; 2008. [Google Scholar]
- 51.Wood JT. Gendered Interaction: Masculine and Feminine Styles of Verbal Communication. In: Verderber K, ed. Voices: A Selection of Multicultural Readings. Belmont, CA: Wadsworth Publishing Company; 1995. [Google Scholar]
- 52.Lee YM, Florez E, Holm K, Horwitz J, Waters R. Latino adolescent perspectives toward sexually transmitted infection educational programs. International Journal of Nursing Knowledge. 2016;27(1):17–23. [DOI] [PubMed] [Google Scholar]
- 53.Media Sharda A. and gender stereotyping: The need for media literacy. International Research Journal of Social Sciences. 2014;3(8):43–49. [Google Scholar]
- 54.Jeong SH, Cho H, Hwang Y. Media Literacy Interventions: A Meta-Analytic Review. J Commun. 2012;62(3):454–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O’Donnell L, O’Donnell CR, Stueve A. Early sexual initiation and subsequent sex-related risks among urban minority youth. Family Planning Perspectives. 2001;33(6):268–275. [PubMed] [Google Scholar]
- 56.Klanger B, Tydén T, Ruusuvaara L. Sexual behavior among adolescents in Uppsala, Sweden. Journal of Adolescent Health. 1993;14(6):468–474. [DOI] [PubMed] [Google Scholar]
- 57.Walcott CM, Chenneville T, Tarquini S. Relationship between recall of sex education and college students’ sexual attitudes and behavior. Psychology in the Schools. 2011;48(8):828–842. [Google Scholar]
- 58.Register-Mihalik JK, Guskiewicz KM, McLeod TCV, Linnan LA, Mueller FO, Marshall SW. Knowledge, attitude, and concussion-reporting behaviors among high school athletes: A preliminary study. Journal of Athletic Training. 2013;48(5):645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ahrold TK, Meston CM. Ethnic differences in sexual attitudes of U.S. college students: gender, acculturation, and religiosity factors. Arch Sex Behav. 2010;39(1):190–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Buhi ER, Marhefka SL, Hoban MT. The State of the Union: Sexual Health Disparities in a National Sample of US College Students. Journal of American College Health. 2010;58(4):337–346. [DOI] [PubMed] [Google Scholar]
- 61.Oswalt SB, Wyatt TJ. Sexual health behaviors and sexual orientation in a U.S. national sample of college students. Arch Sex Behav. 2013;42(8):1561–1572. [DOI] [PubMed] [Google Scholar]
- 62.Luquis RR, Brelsford GM, Rojas-Guyler L. Religiosity, spirituality, sexual attitudes, and sexual behaviors among college students. J Relig Health. 2012;51(3):601–614. [DOI] [PubMed] [Google Scholar]
- 63.Bennett L, Perkins L, Baligad B. Community Colleges and Sexual Misconduct: Unique Challenges and Opportunities. Association for Student Conduct Administration;2015. [Google Scholar]
- 64.Smith A, Rainie L, Zickuhr K. College students and technology. 2011; http://www.pewinternet.org/2011/07/19/college-students-and-technology/
- 65.Roberts ME, Gibbons FX, Kingsbury JH, Gerrard M. Not intending but somewhat willing: the influence of visual primes on risky sex decisions. Br J Health Psychol. 2014;19(3):553–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Barker G, Ricardo C, Nascimento M, Olukoya A, Santos C. Questioning gender norms with men to improve health outcomes: evidence of impact. Glob Public Health. 2010;5(5):539–553. [DOI] [PubMed] [Google Scholar]