Abstract
Tuberculosis (TB) is a secular disease caused by a bacillus, highly prevalent in Brazil. The genito-urinary tract involvement is rare, with the epididymis the most affected location. Treatment usually involves the combination of 3–4 drugs for TB for 6 months and surgery can be useful in complications.
Keywords: Extra-pulmonary tuberculosis, Genitourinary tuberculosis, Isolated testicular tuberculosis, Tuberculosis
Introduction
Pulmonary tuberculosis is the most common form of TB disease. It is caused by a bacillus, whose knowledge and treatment are extremely old, however, it is still a serious global health problem.1
The infection usually occurs by inhaling the micobacterium tuberculosis that may remain in latent form or evolve into pulmonary TB. In cases of non-cure in the first infection, the bacilli can also gain entry via the hematogeneous and lymphatic spread to other regions of the body, resulting in the extra pulmonary disease.2
Genitourinary TB is consider the second most common form among the extra pulmonary TB, being only behind the lymph nodes that is the most common site.3
It is difficult to diagnosis, and often late, especially due to the poor symptoms and the latency between the first infection and the clinical manifestations that can occur up to 30 years after exposed to the bacterium. In most cases, it clinically mimics other testicular lesions. The genital tract is less affected than the urinary tract, and epididimis is the most common site of genital TB in men.2,4
Diagnostic imaging such as ultrasound (USG) and magnetic resonance (RM) of testes, USG-guided fine needle aspiration cytology and in specific cases surgical approach usually use to confirm the diagnosis.2
Clinical treatment comprising rifampicin, isoniazid, pyrazinamide, and ethambutol is the mainstay of treatment.5
This article report one case of adult patients treated at the Urology Department of the Hospital Universitário Cassiano Antônio de Moraes, with a postoperative diagnosis of epididymis TB, followed by a review of the literature on the best diagnosis conduct, treatment and follow-up of these case.
Case report
A 30-year-old patient, with no comorbidities, presented with pain in the right testicular for approximately 6 months, which was previously treated as an orchiepididymitis in another service. In addition, he was reported sporadic fever. On physical examination revealed palpable nodule in a right testicle upper pole in an epididymis topography, but not distinguishable at physical examination. Laboratory tests, included PPD, were all negative.
USG of testis demonstrated an consistent diagnosis with right epididymitis (Fig. 1A). Magnetic resonance (MRI) of testis showed an oval expansive formation located in the right epididymis measuring 2 cm in largest diameter, causing a slight compression on the adjacent ipsilateral testis, without invade it (Fig. 1B and C). Differential diagnoses in this clinical context should be, according to the radiological report, include neoplasia of epididymis.
Fig. 1.
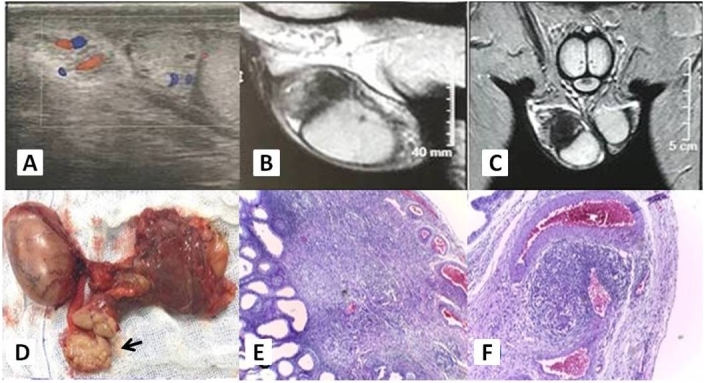
Radiological findings in patients with epididymis tuberculosis. A) Doppler ultrasonography of the right testis. B) Magnetic resonance imaging in a sagittal section of the right testis. C) Magnetic resonance imaging in a coronal section of the right testis. D) Macroscopy with epididymis open longitudinally. E) Microscopy with smaller increase showing chronic inflammation granulomatous tuberculoid. F) Microscopy with greater increase showing chronic inflammation granulomatous tuberculoid. Arrow: Nodule in the epididymis.
After magnetic resonance imaging, we opted for a surgical intervention, right orchi-epididymectomy through the inguinal canal, due to the possibility of malignant neoplasm of the epididymis (Fig. 1D).
The histopathological showed a chronic necrotizing tuberculosis and granulomatous in the epididymis with negative fungi and BAAR. The lesion was located at the head of the right epididymis (Fig. 1E and F).
The patient returned with treatment initiated before the surgery and recived another 2 months of rifampicin, isoniazid, pyrazinamide and ethambutol, followed by 4 months of rifampicin and isoniazid.
Complete resolution of left epididymis nodule was documented at the end of 6 months of treatment.
Discussion
Genitourinary TB is an uncommon presentation of TB and comprises 8–15% of extra-pulmonary TB. Isolated genital involvement is seen about in 28% patients of genitourinary TB. Diagnosis of epididymis TB is uncommon, therefore can be challenging.2
The clinical manifestations may be poor and especially occur many years after the primary infection. Initial presentation may include testicular pain, palpable mass, swelling without any discharging sinus, scrotal involvement and in more advanced cases fistulas and infertility.2,4 In our case, clinical findings were painful nodule and fever.
The definitive diagnosis of epididymis tuberculosis is determinate by isolating the bacillus from the epididymis. Finding of the epithelioid granulomas and acid-fast bacilli (AFB) on Ziehl-Neelsen staining in the materials obtained from the epididymis confirm the diagnosis of TB. Another possibility is the Polymerase Chain Reaction (PCR), which is a fast molecular test with high sensitivity and specificity rates.5 In our case, the base of the diagnosis was the histology of the postoperative findings.
The treatment of urogenital TB, as well as pulmonary tuberculosis and other extra pulmonary forms involves a combination of drugs aimed at avoiding bacillary resistance and should be initiated immediately after histological or microbiological diagnosis or even empirically in case of clinical, radiological and laboratory suspect disease.2
Unless there are complications such as abscesses and cutaneous fistulas or extensive involvement of the epididymis and testis, pharmacological treatment is the first line for cases of epididymis TB, and surgery is the second option when pharmacological treatment fails. Epididymectomy is the surgery of choice, associated orchiectomy maybe or may not be use, depending on each case, which the surgery happens after 4–6 weeks of pharmacotherapy.2
In the case, the treatment for urogenital TB began as recommended by the literature in preoperative. However, due to the risk of epididymis neoplasia, surgery therapy ended up in the course of pharmacotherapy and not after 6 weeks as recommended by the studies.
Thus, it is observed that the conduct adopted in our case, although not the first line treatment for epididymis TB, surgical management was based on the clinical and intraoperative suspicion of epididymis neoplasia, supported by the absence of a previous suggestive pulmonary TB history or immunosuppression and supported by an imaging examination that did not rule out the possibility of a neoplastic process.
Conclusion
Despite being a rare disease and it difficult diagnosis, isolated epididymis TB should be considered as a differential diagnosis in cases presenting with testicular mass.
Pharmacological treatment is the first line for cases of epididymis TB, and surgery is the second option when pharmacological treatment fails. A surgical approach should be considered only in cases where the diagnosis is not clearly established or when there is a strong clinical indication such as abscesses, cutaneous fistulas or extensive involvement of the epididymis and testis.
The aim of this article was to elucidate and bring more insights to this rare diagnosis and to conduct it adequately as recommended by the literature.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Saúde SdVeSMd. 2019. Manual de recomendações de controle da tuberculose no Brasil. [Google Scholar]
- 2.Madeb R., Marshall J., Nativ O., Ertuk E. Epididimal tuberculosis: case report and review of literature. Urology. 2005 Apr;65(4):798. doi: 10.1016/j.urology.2004.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Figueiredo A.A., Lucon A.M., Srougi M. Urogenital tuberculosis. Microbiol Spectr. 2017 Jan;5(1) doi: 10.1128/microbiolspec.tnmi7-0015-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen S.M. Isolated tuberculous epididymitis. Formos J Surg. 2017 Apr;50(2):74–76. [Google Scholar]
- 5.Figueiredo A.A., Lucon A.M., Arvellos N.A. A better understanding of urogenital tuberculosis pathophysiology based on radiological findings. Eur J Radiol. 2010 Nov;76(2):246–257. doi: 10.1016/j.ejrad.2009.05.049. [DOI] [PubMed] [Google Scholar]


