Abstract
Vision impairment is one of the devastating complications of central nervous system tuberculosis (CNS TB). Optic atrophy is a sequelae of various forms of CNS TB which, ultimately, is responsible for vision impairment. It is usually the secondary optic atrophy which occurs in CNS TB. In this case report, we present the story of an immunocompetent woman presenting as bilateral visual loss. She was found to have primary optic atrophy. Neuroimaging revealed features of chronic meningitis. Polymerase chain reaction test for Mycobacterium tuberculosis was positive in cerebrospinal fluid. Although secondary optic atrophy is common in the CNS TB, as a complication of meningitis, primary optic atrophy per se is infrequently reported.
Introduction
Tuberculosis is one of the most prevalent infectious disease in developing countries. It primarily affects the lungs, but extrapulmonary tuberculosis is on the rising trend in recent years. Central nervous system involvement occurs in about one percent of cases, and often results in significant complications. Haematogenous dissemination of the bacilli that follows primary infection or late reactivation results in the establishment of scattered tuberculous foci in brain. These foci trigger off inflammatory reaction in a susceptible host. Retroviral infection,malnutrition,alcoholism,malignancies,immunosuppressive medications being the important risk factors. Arachnoiditis,vasculitis and obstructive hydrocephalus are the three mechanisms by which tuberculous bacilli cause pathology in CNS tuberculosis. Optic neuropathy in tuberculosis is mostly as a result of chronic papilledema due to meningitis and if not treated, culminates in secondary optic atrophy. Tuberculosis can affect any part of the eye. Ocular tuberculosis can also occur in the absence of neurotuberculosis, diagnosis of which requires high index of clinical suspicion.Primary inflammation of optic nerve head due to retrobulbar optic neuritis is extremely rare in tuberculosis.
Patient and observation
A 22 yr old lady, presented to us with history of sudden onset loss of vision in both the eyes with painful eye movements of one month duration. She could not read recognise objects, and could perceive just rays of light. There was no history of headache, vomiting, altered sensorium. She did not have hearing loss, facial deviation, nasal regurgitation, weakness of limbs or involuntary movements. No history of fever,cough,loss of weight. No history of loose stools,vomiting,dysuria. No past history of hypertension,diabetes mellitus,tuberculosis,cerebrovascular accidents. There were no similar complaints or morbid illness in her family. She was married and had two children. There was no history of abortion. Her menstual history was normal. She did not have any high risk sexual behavior. Her diet was poor in carbohydrates and proteins. She did not have any addictions and did not consume any toxic substance. From the history, we made a provisional diagnosis of optic neuropathy. Infectious etiologies like tuberculosis,retroviral infection, CMV, toxoplasmosis were the primary differential diagnoses. A possibility of intracranial space occupying lesion was also considered.
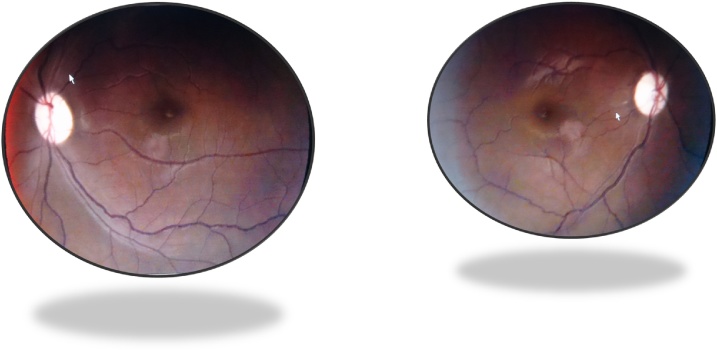
On examination, she was poorly nourished with a BMI of 16 kg/m2. She was pale. Axillary lymphnodes were enlarged bilaterally, 3–4 in number on each side, largest of them measuring 4 x 5 cm-firm, palpable and matted. Examination of eyes showed normal eyelids, conjuctiva, cornea with relative afferent pupillary defect and normal light reflex (Fig. 1). Optic fundii examination showed chalky white disc with well demarcated margins and vessels suggestive of bilateral primary optic atrophy (Fig. 2Figs. 2 and 3 ). Extra ocular movements were normal. Other cranial nerves and sensorimotor system was within normal limits. There were no signs of meningeal irritation. Respiratory, Cardiovascular, Gastrointestinal systems examination revealed no abnormalities.
Fig. 1.

Relative afferent papillary defect.
Figs. 2 and 3.
Chalky white optic disc suggestive of primary optic atrophy.
Haematological investigations revealed anaemia with elevated ESR, as depicted in Table 1 below.
Table 1.
Haematological parameters.
| Hemoglobin | 9.1 grams per dl |
| Total leucocyte count | 9200/cmm |
| Differential count | N56 L36 E7 M1 |
| Platelet count | 4.2 lakhs/cmm |
| MCV | 75 fL |
| ESR | 120 mm in first hour |
| Peripheral smear | Microcytic hypochromic RBC’s |
Renal, liver function tests, serum electrolytes, blood sugar and urine routine examination were within normal limits. Chest x-ray was normal. Mantoux test was done to look for a tuberculous etiology which turned out to be strongly positive (20 x 20 mm). Suspecting tuberculous meningitis lumbar puncture done and cerebrospinal fluid analysis(CSF) showed normal opening pressure −160 mm H20, a normal appearance, elevated protein-256 mg/dl, low sugar 36 mg/dl. CSF contained 200 cells with 100 percent lymphocytes consistent with tuberculous meningitis. CSF Adenosine deaminase was 20 U/L(Positive)(Normal value <10U/L). Polymerase chain reaction for Mycobacterium tuberculosis was positive in CSF. Gram stain,India ink stain,Cryptococcal antigen test,fungal culture were negative in CSF. Fine needle aspiration cytology from axillary lymphnode showed only reactive hyperplasia. Axillary lymphnode biopsy showed caseating granulomatous and lymphadenitis consistent with tuberculosis.Toxoplasma, cytomegalovirus, VDRL and herpes serology were negative.Blood and urine cultures did not show any growth.Rheumatoid factor and antinuclear antibody was negative. Sickling test was negative.Neuroimaging showed pachy and leptomeningitis with no evidence of papilledema, but a thinned out optic nerve (Fig. 4 ).
Fig. 4.
MRI showing pachy, leptomeningitis and thinned out optic nerve.
So we made a final diagnosis of tuberculous meningitis with primary optic atrophy possibly as a complication of retro bulbar optic neuritis.
She was started on antituberculous drug regimen with isoniazid, rifampin, pyrazinamide & ofloxacin (substituted for ethambutol) along with steroids.Though her visual loss persisted, her general condition improved and she is on regular follow up.
Discussion
Optic nerve carries more than a million axonal fibres from the retinal ganglion cells and continues as the optic radiation. Optic neuritis is the most common cause of optic nerve disease in younger adults, whereas ischemia predominates in elderly. Optic neuritis can be due to diverse mechanisms [1]. Pathologically, optic neuritis may be due to demyelination, infection or inflammation secondary to autoimmune disease, sarcoidosis, tumours. Acute viral infections and toxoplasmosis cause inflammation of the optic disc, as an extension of retinitis, so called neuroretinitis should not be confused with optic neuritis [2].
Optic neuropathy in tuberculosis occurs due to tubercular perineuritis(as in our case), papilledema and consecutive optic atrophy due to raised intracranial tension, endarteritis of the optic nerve, toxic neuritis due to drugs(ethambutol and isoniazid), arachnoiditis of the optic chiasma and tuberculoma compressing the optic nerve [3]. The latter occurs in military tuberculosis. In most of the cases of tuberculous perineuritis, optic fundii will be normal(retrobulbar neuritis). In rest of them, there will be visible inflammation of the intraocular part of optic nerve(papillitis) or inflammation of optic disc(discitis) [4].
Clinically, optic neuritis usually presents as mono ocular blindness, and very rarely as bilateral visual loss.Pain, relative afferent papillary defect, dyschromatopsia and central scotoma are other important features. Periocular pain occurs in majority of patients with perineuritis. Visual loss ranges from mild reduction in visual acuity to absent perception of light progressing over a period of one to two weeks [5]. Dyschromatopsia is often out of proportion to loss of visual acuity.In a report by Purvin et al, scotoma occurred in the paracentral and arcuate area in most of the patients [6]. Unfortunately there is no specific diagnostic criteria for tuberculous optic neuropathy. Gupta et al has proposed a criteria for ocular tuberculosis which consists of (1)Clinical signs (2)Positive results in ocular investigations (3)Positive results in systemic investigations (4)Therapeutic response to treatment [7]. Magnetic resonance imaging is the investigation of choice for evaluation of optic nerve disease. All segments of optic nerve(optic nerve head,intraorbital segment,intra canalicular and intracranial segment)can be well visualized in MRI. In the acute stages of perineuritis,MRI shows enhancement within the optic nerve(doughnut sign). Optic nerve may be thinned out in chronic stages.
Whether patients with tuberculous optic neuropathy should be treated with usual four drug regimen (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol) is still a dilemma [8]. Though Isoniazid and ethambutol can cause toxic neuritis, it has not been mentioned anywhere in literature to omit these drugs in a case of tuberculous optic neuropathy. Deterioration in visual acuity and colour vision,after initial improvement following treatment is a definite sign of toxicity [9], [10]. Systemic or intra ocular steroid as an adjunct has a proven role in reducing the inflammation,however studies have yielded diverse results. In a study published by Ang et al, no significant difference in outcome was observed in patients treated concomitantly with antituberculous drugs and steroids versus antituberculous drugs alone [11].
Conclusion
Optic neuropathy in tuberculosis occurs by various pathophysiological processes. Tubercular perineuritis and retrobulbar neuritis though uncommon can lead to primary optic atrophy and permanent visual loss. Prompt diagnosis and initiation of treatment results in good visual outcome.
Authors’ contributions
The authors have read and agreed to the final manuscript.
CREDIT AUTHOR STATEMENT
Conception and design of study: Dr. Santhosh, Dr. Divya
Acquisition of data: Dr.Santhosh
Analysis and/or interpretation of data: Dr.Santhosh,Dr.Divya,Dr.Gomathy
Drafting the manuscript: Dr.Divya,Dr.Gomathy
Revising the manuscript critically for important intellectual content: Dr.Santhosh
Approval of the version of the manuscript to be published
All authors approve the final version of manuscript
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
Acknowledgements
We acknowledge the department of radiodiagnosis for allowing us to use the MRI images.
References
- 1.Davis E.J., Rathinam S.R., Okada A.A., Tow S.L., Petrushkin H., Graham E.M. Clinical spectrum of tuberculous optic neuropathy. J Ophthalmic Inflamm Infect. 2012;2(4):183–189. doi: 10.1007/s12348-012-0079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mansour A.M., Tabbara K.F., Tabbarah Z. Isolated optic disc tuberculosis. Case Rep Ophthalmol. 2015;6(3):317–320. doi: 10.1159/000439376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aupy J., Vital A., Rougier M.B., Gradel A., Meissner W., Marchal C. Presumed tuberculous retrobulbar optic neuritis: a diagnosis challenge. J Neurol. 2015;262(2):481–484. doi: 10.1007/s00415-014-7611-5. [DOI] [PubMed] [Google Scholar]
- 4.Lolly P., Rachita S., Satyasundar M. Ophthalmic manifestations of central nervous system tuberculosis – two case reports. Indian J Tuberc. 2011;58(4):196–198. [PubMed] [Google Scholar]
- 5.Alvarez G.G., Roth V.R., Hodge W. Ocular tuberculosis: diagnostic and treatment challenges. Int J Infect Dis. 2009;13(4):432–435. doi: 10.1016/j.ijid.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Purvin V., Kawasaki A., Jacobson D.M. Optic perineuritis: Clinical and radiographic features. Arch Ophthalmol. 2001;119(3):1299–1306. doi: 10.1001/archopht.119.9.1299. [DOI] [PubMed] [Google Scholar]
- 7.Gupta V., Gupta A., Rao N.A. Intraocular tuberculosis – an update. Surv Ophthalmol. 2007;52(6):561–587. doi: 10.1016/j.survophthal.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal R., Gupta B., Gonzalez-Lopez J.J., Rahman F., Phatak S., Triantafyllopoulou I. The role of anti-tubercular therapy in patients with presumed ocular tuberculosis. Ocul Immunol Inflamm. 2015;23(1):40–46. doi: 10.3109/09273948.2014.986584. [DOI] [PubMed] [Google Scholar]
- 9.Menon V., Jain D., Saxena R., Sood R. Prospective evaluation of visual function for early detection of ethambutol toxicity. Br J Ophthalmol. 2009;93(9):1251–1254. doi: 10.1136/bjo.2008.148502. [DOI] [PubMed] [Google Scholar]
- 10.Ezer N., Benedetti A., Darvish-Zargar M., Menzies D. Incidence of ethambutol-related visual impairment during treatment of active tuberculosis. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2013;17(4):447–455. doi: 10.5588/ijtld.11.0766. [DOI] [PubMed] [Google Scholar]
- 11.Ang M., Htoon H.M. Chee SP. DIagnosis of tuberculous uveitis: clinical application of an interferon-gamma release assay. Ophthalmology. 2009;116(1):1391–1396. doi: 10.1016/j.ophtha.2009.02.005. [DOI] [PubMed] [Google Scholar]