Abstract
Purpose
To determine the reliability of visual assessment of [123I]FP-CIT SPECT imaging by non-experts in dopamine transporter (DAT) SPECT imaging in patients with early drug-naive Parkinson’s disease (PD). Also, we explored the indications of DAT SPECT imaging in clinical practice by neurologists.
Methods
We collected [123I]FP-CIT SPECT scans of the Levodopa in EArly Parkinson’s disease (LEAP) trial participants that were made prior to recruitment, as part of routine clinical work-up. All scans were reassessed by an expert in DAT imaging. A survey on the use of DAT SPECT imaging was sent to all referring neurologists.
Results
The concordance of the initial local assessment and the expert reassessment was 98.7%. The survey showed that neurologists requested DAT SPECT imaging in only 73.6% of patients to differentiate between a neurodegenerative disease and non-neurodegenerative parkinsonism.
Conclusions
Visual assessment of [123I]FP-CIT SPECT imaging by community nuclear medicine physicians in patients with early PD is reliable. Neurologists who request DAT SPECT scans are not always aware that the high accuracy is limited only to the differentiation between neurodegenerative and non-neurodegenerative parkinsonism. A significant portion of neurologists who request DAT SPECT scans is not always aware that the high accuracy is limited to the differentiation between neurodegenerative and non-neurodegenerative parkinsonism as DAT SPECT cannot reliably distinguish the various Parkinsonian syndromes.
Keywords: DAT SPECT, Visual assessment, Indication, Reliability
Introduction
Parkinsonism is characterized by bradykinesia accompanied by either rigidity and rest tremor, or both. Parkinsonism can be classified into two clinically relevant categories: parkinsonism with nigrostriatal degeneration and parkinsonism or mimics with an intact nigrostriatal system.
First, the most frequent cause of parkinsonism with nigrostriatal cell loss is Parkinson’s disease (PD). Other, less common forms of neurodegenerative parkinsonism, also called atypical Parkinsonian syndromes (APS), include multiple system atrophy, progressive supranuclear palsy, dementia with Lewy bodies, and corticobasal degeneration.
Second, non-neurodegenerative forms of parkinsonism are disorders that are clinically established forms of parkinsonism/parkinsonism mimics but molecular imaging or autopsy shows no signs of nigrostriatal cell loss. Parkinsonism or mimics with an intact nigrostriatal system can be caused by for example medication, functional neurological symptoms, and essential tremor [1].
An accurate clinical diagnosis of PD can be challenging and misdiagnosis is not uncommon, particularly early in the course of parkinsonism since clinical features overlap frequently [2]. Distinguishing neurodegenerative versus non-neurodegenerative forms of parkinsonism is important, considering the differences in prognosis and treatment. Neuroimaging can be a useful tool to distinguish between these two categories. Dopamine transporter single-photon emission computed tomography (DAT SPECT) imaging is an accurate method to differentiate between neurodegenerative and non-neurodegenerative parkinsonism, even at an early stage of the disease [3]. The alterations of the presynaptic dopaminergic neurons can be quite similar between PD and APS. Consequently, a DAT SPECT cannot differentiate between the different forms of neurodegenerative parkinsonism in clinical practice [4].
In clinical practice, DAT SPECT images are assessed by nuclear medicine physicians, radiologists, or neurologists. Previous studies have shown that expertise in DAT SPECT imaging is preferred to visually assess DAT SPECT scans [5]. The focus of DAT SPECT imaging-related research has been on the diagnostic accuracy and the use of DAT SPECT imaging in tertiary referral centers specialized in movement disorders. Little is known about the accuracy of its use in routine clinical practice in general hospitals.
This study evaluates the reliability of visual assessments by community nuclear medicine physicians of 123I-2β-carbomethoxy-3β-(4-iodophenyl)-N-(3-fluoropropyl) nortropane ([123I]FP-CIT) SPECT imaging of patients that took part in the Levodopa in EArly Parkinson’s disease (LEAP) cohort and underwent DAT SPECT imaging prior to recruitment, as part of routine clinical practice. In addition, we present the results of a questionnaire, filled out by general neurologists, on the reasons to request DAT SPECT imaging by general neurologists.
Methods
Design
The current study is a retrospective cross-sectional cohort study of visual assessment of DAT SPECT scans of patients suspected to have PD that underwent [123I]FP-CIT SPECT imaging before they were recruited in the LEAP study. The LEAP study was a multicenter, double-blind, placebo-controlled, randomized delayed-start trial. The aim of the LEAP study was to investigate if early treatment with levodopa has a disease-modifying effect [6].
Study population
For the LEAP study, patients in the Netherlands with recently diagnosed idiopathic PD using the standard clinical criteria were eligible [7]. The other inclusion criteria were a diagnosis made in the past 2 years, age 30 years and older, a life expectancy of more than 2 years, and no limitations in functional health for which the patient needed PD medication.
Study procedures
For all LEAP study participants, we determined whether they underwent [123I]FP-CIT SPECT imaging prior to inclusion as part of routine clinical work-up. We attempted to obtain all [123I]FP-CIT SPECT scans. All institutions acquired and reconstructed the images according to guidelines on DAT SPECT imaging published by the European Association of Nuclear Medicine [8]. Nuclear medicine physicians without extensive expertise in DAT SPECT imaging (non-experts) in the referral hospitals assessed the scans, and [123I]FP-CIT SPECT scans that were evaluated by visual assessment only were included. Subsequently, the [123I]FP-CIT SPECT scans were visually reassessed by an expert DAT SPECT reader (JB). The expert assessor was blinded for the results of the initial assessment by the “non-expert” and clinical details aside from the date of birth and that the patients were participating in the LEAP study. The images were analyzed in a familiar and consistent color scale on a HERMES workstation.
Classification and outcome of [123I]FP-CIT SPECT
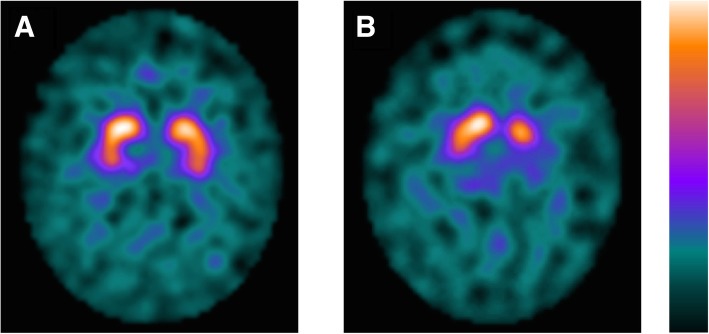
The [123I]FP-CIT SPECT images were classified as either “normal” or “abnormal.” “Normal” DAT SPECT imaging was characterized by clear binding of the radiotracer in the putamen and caudate nuclei both bilaterally, mostly symmetrical. The striata often looks circular or oval-shaped (Fig. 1) [9]. The result of DAT SPECT imaging was considered “abnormal” when low binding was visual in the striatal area, in most cases asymmetrical and lower in the putamen than the caudate nucleus. Reduced binding of the radiotracer is in the early phase of PD usually visible in the dorsal putamen and expands gradually to the ventral putamen and caudate nucleus [9].
Fig. 1.
DAT SPECT imaging. Normal (a) and abnormal (b) [123I]FP-CIT SPECT imaging of patients in the LEAP cohort. Patient A is a 64-year-old male. Patient B is a 63-year-old female. DAT, dopamine transporter; SPECT; single-photon emission computed tomography; LEAP, Levodopa in EArly Parkinson’s disease
Use of DAT SPECT imaging in clinical practice survey
In November 2016, an electronic survey was sent to all neurologists that referred patients for the LEAP study (n = 146). The questionnaire consisted of two multiple-choice questions (Fig. 2). The questions were as follows: (1) “When do you request DAT SPECT imaging?” and (2) “In which percentage of patients with a diagnosis of PD do you use DAT SPECT imaging?” The survey was completed anonymously.
Fig. 2.
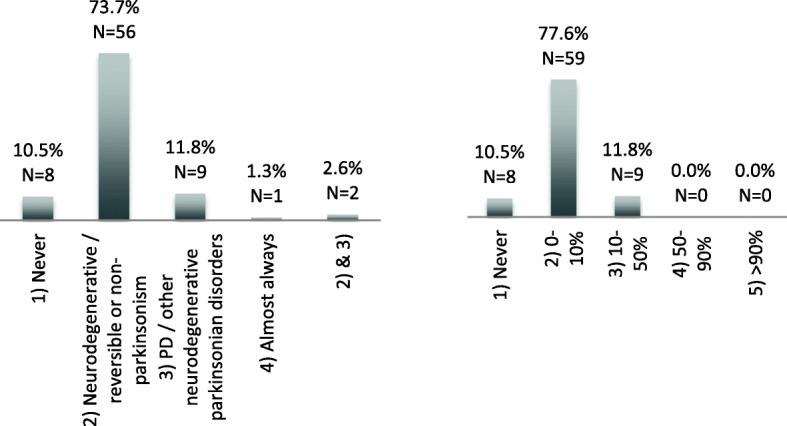
Results of the “Request of DAT SPECT imaging” survey. (1) In which case do you request DAT SPECT imaging? (left panel). (2) How often do you request DAT SPECT imaging? (right panel). DAT, dopamine transporter; SPECT, single-photon emission computed tomography; PD, Parkinson’s disease; N, number of respondents
Results
Demographics
From October 2011 to May 2016, a total of 446 patients were enrolled in the LEAP study. One hundred five of these 446 patients underwent [123I]FP-CIT SPECT imaging prior to inclusion in the LEAP study. Twenty-six scans were excluded. Twenty-one scans were initially assessed by (semi-)quantitative analysis. Four scans were initially assessed by JB. One scan could not be reassessed due to an outdated computer system in one of the referring hospitals. A total of 79 DAT SPECT scans were included in this study (Fig. 3). SPECT was performed 3–4 h after intravenous injection of [123I]FP-CIT (mean amount 185 MBq, range 140–214 MBq). The patient characteristics can be found in Table 1.
Fig. 3.
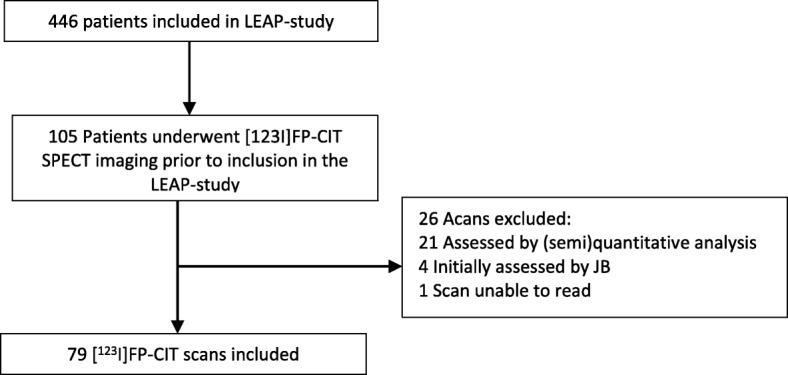
Flowchart of included DAT SPECT scans. LEAP, Levodopa in EArly Parkinson’s disease; DAT, dopamine transporter; SPECT, single-photon emission; computed tomography; JB, J. Booij
Table 1.
Demographic and clinical characteristics
| Patients (n = 79) | |
|---|---|
| Age—years | 63.4 ± 9.9 |
| Male sex—number (%) | 52 (65.8) |
| Symptom duration at imaging (mean ± SD)—years | 1.8 ± 1.5 |
| UPDRS[11] motor score at imaging (0–108) (mean ± SD) | 18.2 ± 9.4 |
SD standard deviation, UPDRS Unified Parkinson’s Disease Rating Scale
Analysis
[123I]FP-CIT SPECT imaging was performed in 30 hospitals (five tertiary referral hospitals and 25 community hospitals). Different dual-headed SPECT cameras and one brain-dedicated SPECT system were used. The initial assessment was “normal” in one patient and “abnormal” in 78 patients. The expert assessment was “normal” in two patients and “abnormal” in 77 patients. The concordance of the non-experts of the referring hospitals and JB on “normal” versus “abnormal” scans in this study was 98.7%.
Use of DAT SPECT imaging survey
Seventy-six neurologists responded to the questionnaire (response rate 52%). 73.6% requested DAT SPECT imaging to differentiate between a neurodegenerative and non-neurodegenerative form of parkinsonism. 11.8% of the neurologists use DAT SPECT imaging to differentiate between PD and APS (Fig. 2).
Discussion
Our findings are in line with the high diagnostic accuracy of visual assessments of DAT SPECT imaging in patients with a clinical diagnosis of early PD. In addition, we showed this is also true in routine clinical practice compared to a highly trained nuclear medicine physician dedicated to DAT imaging.
The strength of this study is that we evaluated the reliability of the visual assessments performed in clinical practice by nuclear physicians with various levels of expertise in neuroimaging in patients with a clinical diagnosis of early-stage PD. It was shown that false-positive (abnormal) outcomes occur more frequently among less experienced observers, while experienced observers classify [123I]FP-CIT SPECT scans correctly using visual assessment only [5]. Our findings suggest that this does not seem to be an issue in clinical practice, considering only one scan was found to be false positive by the expert. A limitation of this study is the selection bias. Our results reveal little about the accuracy of assessments of normal DAT SPECT scans considering the patients were already included in the LEAP study. The LEAP study population is not a typical population in that only patients were included in which the referring neurologist was fairly confident the patient had a diagnosis of PD. Consequently, the rate of abnormal DAT SPECT scans is considerably higher compared to routine clinical practice; therefore, our results may not be applicable to general use.
A possible limitation is that only one expert reassessed the images. Nevertheless, the inter-agreement of visual assessment of DAT SPECT imaging by experts, reported in the literature, is very high (Cohen’s κ 0.87–0.99) [10].
Furthermore, our survey showed that most of the responding neurologists request for [123I]FP-CIT SPECT imaging for an appropriate indication [3]. However, a significant portion (11.8%) of the responding neurologists request [123I]FP-CIT SPECT imaging to differentiate between PD and other APS, although DAT SPECT imaging cannot reliably discriminate between neurodegenerative parkinsonian disorders in routine clinical practice [4]. It is essential for clinicians who apply for [123I]FP-CIT SPECT imaging to have knowledge of the limitations and the information it can provide. With this survey, we gained a unique insight in the use of DAT SPECT imaging by neurologists in clinical practice.
Conclusion
In conclusion, visual assessment of DAT SPECT imaging by non-experts in patients with a clinical diagnosis of early-stage PD is reliable. A significant portion of neurologists who request DAT SPECT scans is not always aware that the high accuracy is limited to the differentiation between neurodegenerative and non-neurodegenerative parkinsonism as DAT SPECT cannot reliably distinguish the various Parkinsonian syndromes.
Acknowledgements
Not applicable
Informed consent
Informed consent was obtained from all individual participants included in the study.
Abbreviations
- [123I]FP-CIT
123I-2β-carbomethoxy-3β-(4-iodophenyl)-N-(3-fluoropropyl) nortropane
- APS
Atypical parkinsonian syndromes
- DAT SPECT
Dopamine transporter single photon emission computed tomography
- JB
Jan Booij
- LEAP study
Levodopa in EArly Parkinson’s disease study
- PD
Parkinson’s disease
Authors’ contributions
SRS contributed to the conception and design of the work, interpretation of the data, and drafting of the manuscript. CV contributed to the conception of the work and substantial revision of the manuscript. MS contributed to the acquisition of the data, interpretation of the data, and substantial revision of the manuscript. JB contributed to the conception and design of the work, interpretation of the data, and substantial revision of the manuscript. RB contributed to the conception and design of the work, interpretation of the data, and substantial revision of the manuscript. All authors approve the submission of this final version of the manuscript.
Authors’ information
Not applicable
Funding
The original LEAP study was supported by unrestricted grants from the Netherlands Organization for Health Research and Development (Dutch governmental fund for health research, project number 0-82310-97-11031), Parkinson Vereniging (Dutch patient organization), Stichting Parkinsonfonds (Dutch funding organization for Parkinson’s disease research), and Stichting Parkinson Nederland (Dutch funding organization for Parkinson’s disease research).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was assessed and approved by the medical ethical committee of the Amsterdam University Medical Centers. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable
Competing interests
Sven R. Suwijn declares that he has no conflict of interest. Constant V. Verschuur declares that he has no conflict of interest. Marleen A. Slim declares that she has no conflict of interest. Jan Booij received grant support from GE Healthcare. Rob MA de Bie received grant support from GE Healthcare and Medtronic.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sven R. Suwijn, Email: s.r.suwijn@amc.uva.nl
Constant V. M. Verschuur, Email: C.V.Verschuur@amc.uva.nl
Marleen A. Slim, Email: M.A.Slim@amc.uva.nl
Jan Booij, Email: J.Booij@amc.uva.nl.
Rob M. A. de Bie, Email: r.m.debie@amc.uva.nl
References
- 1.Poewe W, Wenning G. The differential diagnosis of Parkinson’s disease. Eur J Neurol. 2002;9(Suppl 3):23–30. doi: 10.1046/j.1468-1331.9.s3.3.x. [DOI] [PubMed] [Google Scholar]
- 2.Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson’s disease. Lancet Neurol. 2006;5:75–86. doi: 10.1016/S1474-4422(05)70285-4. [DOI] [PubMed] [Google Scholar]
- 3.Suwijn SR, van Boheemen CJ, de Haan RJ, Tissingh G, Booij J, de Bie RM. The diagnostic accuracy of dopamine transporter SPECT imaging to detect nigrostriatal cell loss in patients with Parkinson's disease or clinically uncertain parkinsonism: a systematic review. EJNMMI Res. 2015;5:12. doi: 10.1186/s13550-015-0087-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kagi G, Bhatia KP, Tolosa E. The role of DAT-SPECT in movement disorders. J Neurol Neurosurg Psychiatry. 2010;81:5–12. doi: 10.1136/jnnp.2008.157370. [DOI] [PubMed] [Google Scholar]
- 5.Meyer PT, Winz OH, Dafotakis M, Werner CJ, Krohn T, Schafer WM. Improved visual [(123) I]FP-CIT SPECT interpretation for evaluation of parkinsonism by visual rating of parametric distribution volume ratio images. Q J Nucl Med Mol Imaging. 2011;55:301–309. [PubMed] [Google Scholar]
- 6.Verschuur CVM, Suwijn SR, Boel JA, Post B, Bloem BR, van Hilten JJ, et al. Randomized delayed-start trial of levodopa in Parkinson’s disease. N Engl J Med. 2019;380:315–324. doi: 10.1056/NEJMoa1809983. [DOI] [PubMed] [Google Scholar]
- 7.Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol. 1999;56:33–39. doi: 10.1001/archneur.56.1.33. [DOI] [PubMed] [Google Scholar]
- 8.Darcourt J, Booij J, Tatsch K, Varrone A, Vander Borght T, Kapucu OL, et al. EANM procedure guidelines for brain neurotransmission SPECT using (123) I-labelled dopamine transporter ligands, version 2. Eur J Nucl Med Mol Imaging. 2010;37:443–450. doi: 10.1007/s00259-009-1267-x. [DOI] [PubMed] [Google Scholar]
- 9.Djang DS, Janssen MJ, Bohnen N, Booij J, Henderson TA, Herholz K, et al. SNM practice guideline for dopamine transporter imaging with 123I-ioflupane SPECT 1.0. J Nucl Med. 2012;53:154–163. doi: 10.2967/jnumed.111.100784. [DOI] [PubMed] [Google Scholar]
- 10.Seibyl JP, Kupsch A, Booij J, Grosset DG, Costa DC, Hauser RA, et al. Individual-reader diagnostic performance and between-reader agreement in assessment of subjects with Parkinsonian syndrome or dementia using 123I-ioflupane injection (DaTscan) imaging. J Nucl Med. 2014;55:1288–1296. doi: 10.2967/jnumed.114.140228. [DOI] [PubMed] [Google Scholar]
- 11.Fahn S, Elton RL, Members of the UPDRS Development Committee . The Unified Parkinson’s Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M, editors. Recent Developments in Parkinson’s Disease, Vol. 2. Florham Park: Macmillan Healthcare Information; 1987. pp. 153–163. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.