Abstract
Objective
The purpose of this study was to generate data for conduction of a power analysis to investigate short-term effects of visceral manipulation associated with conventional physical therapy on pain intensity, lumbar mobility, and functionality of people with chronic low back pain and visceral dysfunctions.
Methods
This was a double-blinded, randomized, controlled, clinical trial preliminary study. A blinded evaluation was conducted involving 20 people with chronic low back pain with visceral dysfunction. Pain perception, lumbar mobility, and functionality were assessed in 3 moments: evaluation 1 (1 week before the intervention), evaluation 2 (immediately after the last intervention), and evaluation 3 (1 week after the last intervention). The protocol consisted of 50-minute session of conventional physical therapy and visceral manipulation. The participants were randomly allocated to 2 groups: 10 for the experimental group (conventional physical therapy and visceral manipulation) and 10 for the control group (conventional physical therapy and placebo visceral manipulation).
Results
Significant reductions were found in the experimental group for lumbar mobility and specific functionality in comparison with the control group (P < .05). There were no significant differences for pain perception and global functionality.
Conclusion
The combination of visceral manipulation and conventional physical therapy program demonstrated significant between-groups differences over time for lumbar spine mobility and specific functionality. These gains occurred after 5 sessions, once a week, and were maintained 1 week after the end of the treatment. This study generated data for conduction of a power analysis to inform the design for future clinical research in this line of inquiry.
Key Indexing Terms: Low Back Pain; Manipulation, Osteopathic; Manipulation, Chiropractic; Rehabilitation; Exercise Therapy; Therapy, Soft Tissue; Physical Therapy Modalities
Introduction
Chronic low back pain (CLBP) has turned into a worldwide challenge that substantially raises health and socioeconomic costs.1., 2. The most common indication for treating this condition is through physical exercise because it improves aerobic capacity and muscular strength, which assist individuals with CLBP to perform their daily activities of living. Even with the great number of pharmacologic and nonpharmacologic resources, there are individuals who still experience low back pain.3., 4.
Some studies have shown a correlation between CLBP and urinary incontinence, respiratory disorders, abdominal scars, and gastrointestinal dysfunctions.5., 6., 7., 8., 9. This correlation could be explained by a mechanical and a neurological mechanism. The abdominal viscera are attached to the lumbar region by the abdominal mesenteries, mesocolon, and Toldt fascia. The mesenteries are connective tissue formed by reflecting layers of the peritoneum that carry arteries, veins, lymphatic vessels, and afferent and efferent autonomic nerve fibers from and to the viscera. In addition, the visceral and somatic innervation have a functional convergence on the spine column.10 Consequently, the state of an organ can influence the state of the somatic tissue.
A dysfunctional organ could be classified as an organ that had surgery, adhesions, or an inflammatory process, which affects the visceral connective tissue mobility, such as fascia. The visceral fascial mobility could affect the somatic tissue mobility close to the organ or the somatic tissue with a corresponding spinal innervation with the dysfunctional viscera.11., 12., 13., 14. Following this line of thought, the state of abdominal and pelvic viscera could interfere with distant body segment mobility because visceral innervation comes from the thoracic and lumbar regions through the sympathetic nervous system.
Visceral manipulation (OVM) is a manual technique that aims to restore mechanical, vascular, and neurologic visceral function.15 Studies performed by Bove and Chapelle,5 McSweeney et al,16 and Tozzi et al17 reported a direct and positive repercussion in the visceral mobility, altering its nociceptive input to the spine. However, only one study investigated the effects of OVM on people with nonspecific low back pain and found significant changes in pain intensity after 52 weeks compared with the control group.18
Therefore, the aim of this study was to investigate short-term effects of OVM associated with conventional physical therapy on pain intensity, lumbar mobility, and functionality of people with chronic low back pain and visceral dysfunctions. Our hypothesis is that by adding OVM to a conventional physical therapy session, the gains would be maximized because this technique would assist in releasing fascial adhesions and reducing nociceptive input to the central nervous system.
Methods
Design
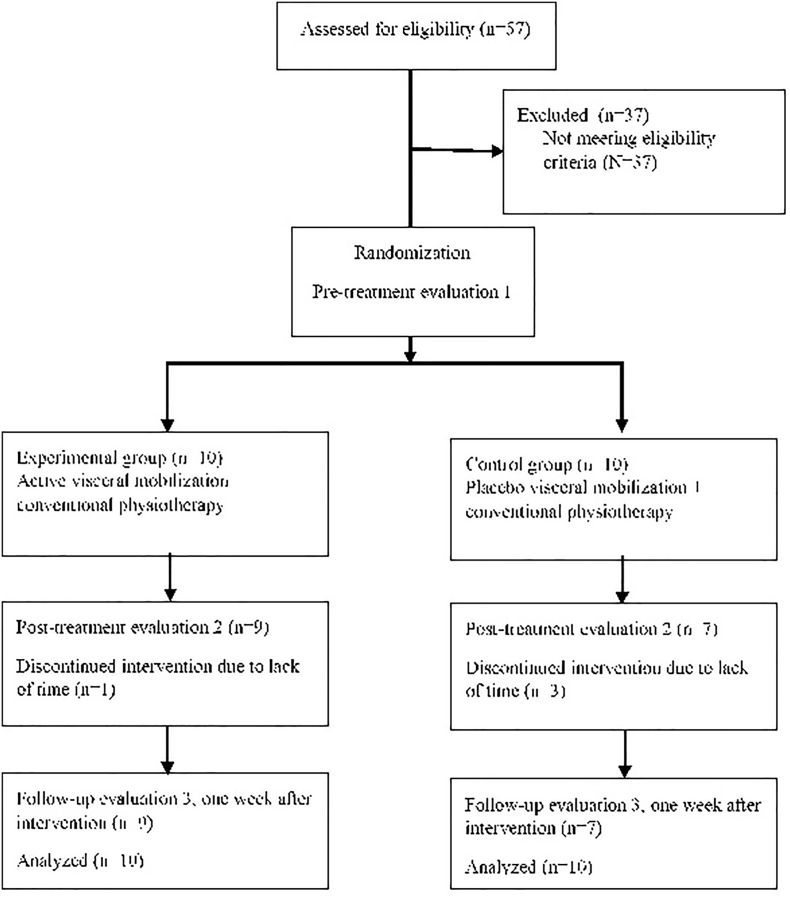
The present double-blinded, randomized, controlled, clinical trial preliminary study was conducted in accordance with the recommendations of the Consolidated Standards Of Reporting Trials 2017 (Fig 1).19 In addition, this study was conducted in compliance with the ethical standards established by the Declaration of Helsinki, and it also received approval from the Human Research Ethics Committee of the University of Sorocaba (São Paulo, Brazil) under process number 1.825.796. This study is registered within ClinicalTrials.gov (NCT03101020). All participants agreed to participate by signing a statement of informed consent.
Fig 1.
Study flow diagram according to Consolidated Standards of Reporting Trials flow diagram 2017.
Participants
A total of 20 participants were recruited from the Health Center of the University of Sorocaba through online forms and third-party referrals. This sample of convenience included 19 women and 1 man, who were allocated in 2 parallel groups: experimental group (10 participants received direct OVM with conservative physical therapy) and control group (10 participants received placebo visceral manipulation with conservative physical therapy).20 The study included 5 intervention sessions over 5 weeks with follow-up at 1 week postintervention.
Eligibility Criteria
Eligible participants were individuals with the following: (1) low back pain for more than 12 weeks, (2) pain ≥2 of 10 on the visual analog pain scale, (3) age from 18 to 80 years old, and (4) history of visceral dysfunction (considered any impaired function of abdominopelvic viscera, reported by the participants during their lifetime, of surgical or nonsurgical origin). For nonsurgical visceral dysfunction, the participants had to present the dysfunction at least 6 months before and until the date of the first evaluation. On the other hand, for visceral surgical dysfunctions, the participants had to have performed the procedure more than 6 months from the date of the first evaluation. To determine whether a participant had visceral dysfunction, we relied only on the patient’s self-report during the anamneses; there was no assessment of clinical examination, imaging exams, or medical reports.
Exclusion criteria were as follows: (1) suspected severe spinal pathology (eg, metastatic, inflammatory, or infectious diseases of the spine; cauda equina syndrome; canal stenosis; fracture of the spine); (2) evidence of neural compression with at least 2 of the following signs: (i) muscle weakness, (ii) diffuse sensory loss or dermatome, and (iii) hyporeflexia or hyperreflexia of the lower limbs; (3) surgery of the spinal column, abdomen, or pelvis in less than 6 months; (4) vascular abnormalities, such as abdominal aortic aneurysm; (5) being under physiotherapeutic, chiropractic, or osteopathic treatment; (6) being pregnant or suspected pregnancy; (7) taking medication that alters visceral motility; (8) taking medication in an acute inflammatory phase of gastrointestinal and urinary disease, such as cholecystitis, renal calculi, peritonitis, and appendicitis; (9) taking medication such as oral corticosteroids, which increase the risk of intestinal perforation; and (10) having gastrointestinal disease associated with the risk of intestinal perforation, for example, Crohn’s disease, diverticular disease, ulcerative peptic disease.
Randomization
A team member who was not involved in the recruitment or research development process performed the block randomization. Using Excel, 20 sequenced numbers were concealed in opaque randomization envelopes, which contained a paper with the letter “E” or “P,” meaning experimental or placebo group, respectively. After the preintervention evaluation, the treating physiotherapist opened the randomization envelope, in another room from the participant, and allocated the participant according to the criteria above.
Interventions
All participants received equal treatment during the assessments and conventional therapy. They were treated 1 time per week for 5 weeks. Each session took 50 minutes, starting with 40 minutes of conventional physical therapy and finishing with 10 minutes of active or placebo visceral manipulation, depending on the participant’s group allocation.
Conventional Physical Therapy
We created a protocol of exercises for individuals with low back pain based on the clinical practice guidelines by Delitto et al (2012). The protocol consisted of general exercises to mobilize, strengthen, and stabilize the spinal column, pelvis, and hip (Fig 2). Once a week for 5 weeks the participant would show up to the clinic and have a private session with the physiotherapist, who taught, supervised, and progressed the exercises. At the end of the first session, the participants received a list with the description and photos of the exercises they performed during that session and that they would need to do every other day at home; however, there was no control if the participants performed the exercises at home. The criteria to progress the exercises were no pain, no fatigue, and no fear on performing them. All participants were oriented to keep an active lifestyle focusing on the activities they could perform.20., 21.
Fig 2.
Conventional physical therapy protocol. (A) Erector spinae stretching: in dorsal decubitus pull the knee toward the abdomen—2 sets of 30 seconds. (B) Knee rolls: roll the knees to one side and the other maintaining both shoulders on the floor—2 sets of 10 seconds per side. (C) Piriformis stretch: in dorsal decubitus cross one ankle over the opposite knee and pull this leg toward the abdomen—2 sets of 30 seconds per side. (D) Pelvic tilts: perform pelvic anteversion and retroversion—10 to 15 repetitions. (E1) Back extensions: in ventral decubitus, extend the back supporting the upper body on flewed elbows—10 to 15 repetitions. (E2) Back extensions progression: the same position but supporting the upper body on the hands with the elbows extended. (F1) Activation of abdominal muscles, in dorsal decubitus perform isometric contraction of the profound abdominal muscles during breathing—3 sets of 10 breathings. (F2) Activation of abdominal muscles progression 1: the same exercise but lifting a flexed knee in the air and maintaining it steady during the set—2 sets of 10 breathings per side. (F3) Activation of abdominal muscles progression 2: the same exercise but lifting an extended knee in the air and maintaining it steady during the set—2 sets of 10 breathings per side. (G1) Activation of back and hip muscles: in side lying, perform isometric contraction of unilateral back and hip muscles during breathing—3 sets of 10 breathings. (G2) Activation of back and hip muscles progression 1: the same exercise but lifting a flexed knee and maintaining the ankle together and the leg steady during the set—2 sets of 10 breathings per side. (G3) Activation of back and hip muscles progression 2: the same exercise but lifting an extended knee and maintaining it steady during the set—2 sets of 10 breathings per side. (H1) Bridge exercise—3 sets of 10 repetitions. (H2) Bridge progression: perform a single leg bridge exercise—3 sets of 10 repetitions per side. (I1,2) Quadruped cat and camel exercise—10 to 15 repetitions. (J1) Single arm or leg raise: in quadruped position raise all limbs (arms and legs) one at a time and maintain the position—1 set of 30 seconds for each limb. (J2) Quadruped opposite arm and leg raise exercise progression—2 sets of 30 seconds per side. (J3) Exercise progression from J2. (K1) Plank: perform the plank exercise supporting the lower body on the knees—2 sets of 30 to 60 seconds. (K2) Plank progression: perform the plank exercise supporting the lower body on the feet—2 sets of 30 to 60 seconds. (L1) Side plank: perform the side plank exercise supporting the lower body on the knees—2 sets of 30 to 60 seconds. (L2) Side plank progression: perform the side plank exercise supporting the lower body on the feet—2 sets of 30 to 60 seconds.
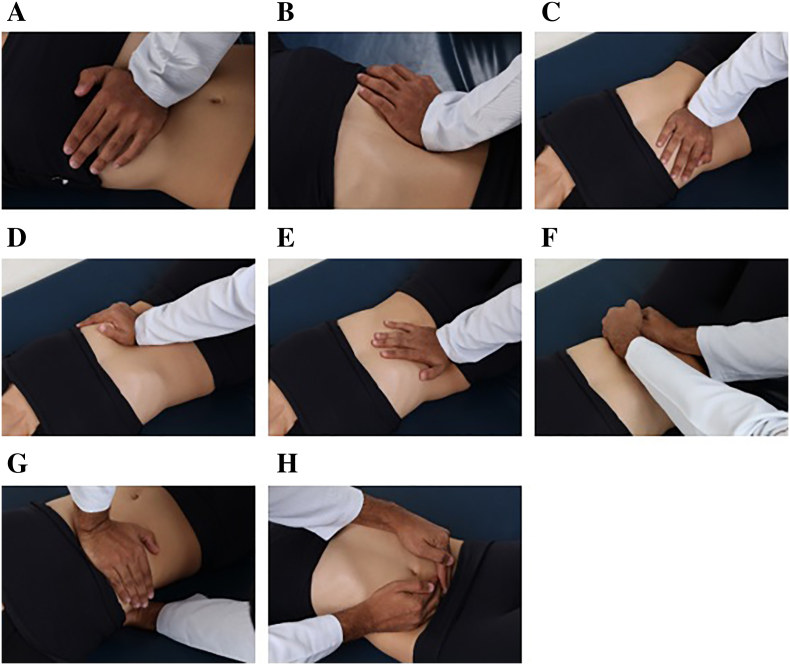
Visceral Manipulation
During all sessions, the participants had to remain in a hook-lying position with the head over a pillow to decrease the tension on the abdominal wall. A physiotherapist with specialization in osteopathy performed the OVM over 8 spots on the abdomen (Fig 3). The techniques applied were cardia manipulation, pylorus manipulation, Oddi sphincter manipulation, duodenojejunal valve manipulation, ileocecal valve manipulation, sigmoid colon manipulation, liver global manipulation, and global hemodynamic manipulation. Each technique took 1 minute, except for the last 2 techniques that were performed 10 times each associated with respiratory inspiration and expiration. These techniques were selected because they manipulate the sphincters of the gastrointestinal system, which have great influence on general organ homeostasis. For the experimental group, the therapist performed a deep pressure with the lower palm over those spots. The placebo visceral manipulation involved a light touch over the same spots, without the intention to treat the patient, with the same amount of time and repetitions as the experimental group.16
Fig 3.
Visceral manipulation protocol. Orientation of the pictures, cranial to the left and caudal to the right. (A) Cardia manipulation (1 minute). (B) Pylorus manipulation (1 minute). (C) Oddi sphincter manipulation (1 minute). (D) Duodenojejunal valve manipulation (1 minute). (E) Ileocecal valve manipulation (1 minute). (F) Sigmoid colon manipulation (1 minute). (G) Liver global manipulation (10 repetitions). (H) Global hemodynamic manipulation (10 repetitions with pressure during expiration and another 10 for inspiration).
Outcomes
All participants were assessed 3 times: pretreatment, post-treatment, and at follow-up. Pretreatment assessment was 1 week before the first session of treatment, post-treatment was right after the last session of treatment, and the follow-up was 1 week after the last session of treatment. A team member who was not involved with the interventions was responsible for collecting all the baseline measures and outcomes.
Primary Outcome
Pain intensity was evaluated through a visual analog pain scale of 11 points, where the participant choose a number from 0 to 10 (0 equal to “no pain at all” and 10 to “unbearable pain”).22
Secondary Outcomes
Lumbar spine mobility was assessed through the original Schober Test. The Roland-Morris Disability Questionnaire was used for general functionality, and the Patient-Specific Functional Scale was used for specific functionality.23., 24., 25., 26., 27.
Adverse Effects
No data related to adverse effects were collected because it was not included in the study methodology.
Blinding
The researchers involved in the evaluation procedures had no access to the allocation of the participants. This information was provided to participants after completion of follow-up evaluations (1 week after the end of the intervention). The investigator responsible for the intervention could not be blinded in relation to the allocation group because he is directly responsible for the application of the visceral manipulation technique.
Statistical Methods
Intention-to-treat analysis was employed when necessary, with the data from the previous evaluation repeated to substitute missing data. The Kolmogorov-Smirnov test demonstrated normal data distribution. Thus, parametric tests were performed and the data were expressed as mean and standard deviation. Two-way analysis of variance was used to compare the effects of stimulation during motor training on the main outcome variables, and the Bonferroni correction for multiple comparisons was employed as the post hoc test. The dependent variables were pain intensity, lumbar mobility, general functionality, and specific functionality. The independent fixed variables were treatment (baseline, post-treatment, and follow-up), group (experimental group and control group), and group–treatment interaction. The Pearson correlation test verified the correlation between the outcomes of the variables. A P value < .05 indicated a statistically significant result. The data were organized and tabulated using the Statistical Package for Social Sciences, version 19.0.
Results
A total of 57 people with chronic low back pain were screened in this study, between June 2017 and July 2017, and 37 did not meet the eligibility criteria. The 20 people who met the eligibility criteria and agreed to participate in the study were randomly assigned to 1 of 2 groups proposed in this study, with a total of 10 people in each group. Clinical characteristics and means and standard deviation of the results obtained in the clinical scales are shown in Table 1 and Table 2, respectively.
Table 1.
Descriptive Statistics (Mean [Standard Deviation] and Frequency Counts) of the Randomly Assigned Clinical Characteristics at Baseline
| Variable | Experimental Group | Control Group |
|---|---|---|
| Age (y) | 41.5 (10.39) | 40.5 (12.12) |
| Height (m) | 1.64 (0.07) | 1.63 (1.09) |
| Body mass (kg) | 66 (16.35) | 73.5 (16.74) |
| Sex | ||
| Male | 0 | 1 |
| Female | 10 | 9 |
| Self-reported visceral dysfunction | ||
| Nonsurgical | ||
| Constipation | 4 | 3 |
| Acid reflux | 4 | 5 |
| Hiatal hernia | 0 | 4 |
| Experienced urinary incontinence | 2 | 0 |
| Subtotal | 10 | 12 |
| Surgical | ||
| Cesarean section | 6 | 7 |
| Abdominoplasty | 0 | 1 |
| Oophorectomy | 0 | 2 |
| Cholecystectomy | 1 | 1 |
| Bariatric surgery | 0 | 1 |
| Subtotal | 7 | 12 |
| Total | 17 | 24 |
Constipation was considered a patient’s self-report of persistent difficulty to defecate. Acid reflux was considered a patient’s self-report of burning pain in the chest area at least twice a week. Hiatal hernia was considered a patient’s self-report of hiatal hernia diagnosed through an abdominal ultrasound performed by a medical doctor. Experienced urinary incontinence was considered a patient’s self-report of uncontrolled leakage of urine. Cesarean section was considered a patient’s self-report of having undergone a surgical procedure to deliver babies. Abdominoplasty was considered a patient’s self-report of having undergone a cosmetic surgery procedure to remove loose skin and excessive fat from the abdomen. Oophorectomy was considered a patient’s self-report of having undergone a surgical procedure to remove 1 or both woman’s ovaries. Cholecystectomy was considered a patient’s self-report of having undergone a surgical procedure to remove the gallbladder. Bariatric surgery was considered a patient’s self-report of having undergone a surgical procedure to reduce the size of the stomach or intestines to achieve weight loss.
Table 2.
Means ± Standard Deviation of the Results Obtained in the Clinical Scales
| Variable | Experimental Group | Control Group |
|---|---|---|
| Visual analog pain scale | ||
| Preintervention | 6.50 (2.33) | 6.00 (0.92) |
| Postintervention | 1.50 (2.42) | 3.50 (2.94) |
| Follow-up | 1.80 (2.93) | 3.30 (3.20) |
| Schober Test | ||
| Preintervention | 14.75 (0.78) | 15.31 (1.00) |
| Postintervention | 15.88 (1.09) | 15.30 (0.63) |
| Follow-up | 15.71 (1.04) | 15.11 (1.04) |
| Roland-Morris Disability Questionnaire | ||
| Preintervention | 12.00 (4.15) | 9.20 (6.16) |
| Postintervention | 6.60 (6.12) | 5.10 (4.48) |
| Follow-up | 5.30 (5.06) | 3.80 (4.53) |
| Patient-Specific Functional Scale | ||
| Preintervention | 5.90 (3.05) | 4.10 (3.08) |
| Postintervention | 3.20 (2.71) | 4.50 (3.29) |
| Follow-up | 3.90 (3.33) | 3.90 (2.77) |
All the effects measured in this study are only over a short-term period of 1 week. Therefore, these results cannot be transposed for long-term effects. In addition, there were no new clinical comorbidities of flare-up of existing co-occurring conditions.
Of the 20 participants, 4 discontinued the intervention because they were unable to attend the proposed sessions owing to lack of time. Three of them were from the control group and 1 was from the experimental group. Thus, it was not possible to perform the postintervention and follow-up evaluation of these participants. These participants were not reassessed in the postintervention or in the follow-up. In addition, a participant from the experimental group fell between the postintervention and follow-up assessment period, which aggravated pain levels. However, we kept and analyzed all the data collected in the follow-up assessment of this patient. All these complications diminished the statistical power of this study.
Primary Outcome
In the analysis of variance, both groups improved in pain (F [2.18] = 30.4, P < .0001). However, there was no significant difference between groups over time (F [2.18] = 0.4, P = .642).
Secondary Outcomes
The lumbar spine mobility and specific functionality improved significantly for the between-group over-time analysis, (F [2.18] = 8.6, P = .002) and (F [2.18] = 6.3, P = .008), respectively. On the other hand, no significant changes were found for the general functionality in the between-group over-time analysis (F [2.18] = 0.2, P = .799).
Correlation
We observed a positive and significant correlation between pain and general functionality (r = 0.717, P = .019) and pain and specific functionality (r = 0.802, P = .005), but not between pain and lumbar spine mobility (r = -0.058, P = .873).
The placebo group also had a significant correlation in the postintervention evaluation between pain and disability (r = 0.859, P = .001) and a discrete correlation between pain and mobility (r = 0.651, P = .041) but not between pain and functionality (r = 0.279, P = .433).
In relation to the conventional physical therapy, all participants from the experimental and control groups reported muscle soreness and fatigue during or after the physical exercises.
Discussion
Our study sought to understand the possible short-term effects of OVM associated with conventional physical therapy on people with chronic low back pain and visceral dysfunctions. In addition, as a preliminary study, we intended to generate data for conducting a power analysis to inform the design for future clinical research in this line of inquiry. We hypothesized that by improving visceral mobility and functionality through OVM, the gains from the conventional physical therapy sessions would be potentialized. This study investigated the short-term effects of 5 sessions consisting of visceral manipulation and conventional physical therapy in patients with chronic low back pain for the outcome measures of pain intensity, lumbar spine mobility, and functionality. There were significant between-group differences over time for lumbar spine mobility and specific functionality.
VM and Pain
Both groups had a significant decrease in pain intensity but not for the between-group analyses. Therefore, there was no effect in adding OVM to conventional physical therapy. This finding diverges from the study of Panagopoulos et al,15 which applied OVM associated with standard physical therapy on 64 patients with low back pain. The experimental group in their study only had a significant between-group difference on pain compared with the control group after 1 year of the intervention. Unfortunately, they did not specify how and which visceral manipulation techniques nor the standard physical therapy intervention they performed. Nonetheless, McSweeney et al16 demonstrated that applying OVM of the sigmoid colon without a co-intervention could decrease pain perception in the somatic tissue that shared the same level of innervation of the viscera manipulated.
VM and Mobility
Because both groups improved on pain perception, the decrease in pain perception could not be responsible for the significant improvement in lumbar mobility. The significant increase in lumbar spine mobility of the experimental group in relation to the control group could be due to the increase in connective tissue motion through visceral manipulation.28 By applying a noninvasive mechanical stimulus (ie, visceral manipulation) to improve connective tissue motion, the lumbar spine mobility improved as well. Under these findings, this study could corroborate the hypothesis that the lack of connective tissue mobility, such as the visceral fascia, is related to the mobility of adjacent joints and muscles. A study conducted by Tozzi et al17 helps to support this hypothesis. They evaluated the mobility of the right kidney through ultrasound screening of people with and without nonspecific low back pain, and they found a significant correlation of people who had a reduced range of right kidney mobility with the presence of nonspecific low back pain.
VM and Functionality
Another finding was that specific functionality had a significant increase for the experimental group compared to the control group, whereas for general functionality both groups had a significant statistical difference. Although the Roland-Morris Disability Questionnaire has a predetermined list of activities and situations limited by low back pain where the participant agrees or disagrees, the Patient-Specific Functional Scale makes the participant write down which specific activities are being jeopardized by their low back pain. Therefore, it could be implied that participants are prone to overestimate their improvements on specific and individualized activities over general activities and situations. Another possibility is that the general scales and questionnaires are not a reliable measure to estimate the patient’s needs and lifestyle compared with specific questionnaires.
Limitations
Unfortunately, our study lacked an assessment to verify visceral mobility owing to a lack of equipment, health professionals trained to assess visceral mobility through imaging exams, and quantitative tests to diagnose visceral dysfunction. However, the focus of this study was not to evaluate the effect of visceral manipulation on visceral dysfunction but to investigate and understand the effects of the visceral manipulation in any individual who had impaired chronic low back pain associated with visceral dysfunction of surgical or nonsurgical origin. According to the hypothesis presented during this study, any kind of visceral function can reverberate in the spinal column owing to mechanical, neurologic, and vascular reasons.
The limited number of men in this study is followed by a trend in other studies where chronic low back pain is more common in women.7., 8., 27. Because this study hypothesizes that visceral function reverberates in somatic tissue function, we could imply that the disproportionate number of men and women with chronic low back pain who volunteered for this study could be due to women being more prone to undergo abdominopelvic surgery during their lifetime, such as cesarean section, than men. However, there are no studies that imply this correlation, and this is not part of the objective of this study. We reinforce the need for epidemiological studies that address this matter.
As this is a preliminary study, the main goal was to provide data for future studies with similar goals and stronger statistical testing. Therefore, this study lacked statistical power to justify a direct and positive relationship between the OVM and the outcomes. First, the high dropout rate for the control group compromised the power of the sample for comparison. Second, both groups were not well matched for all the baseline characteristics, such as the number of visceral dysfunctions, which was higher in the control group. Another limitation was the reliability of the placebo technique, which has no consensus in the literature. Also, no data related to adverse effects were collected, but in the future this information should be collected. The last limitation, as in most intervention treatments in the physical therapy area, was the impossibility of blinding the treating therapist because it is unfeasible in this kind of intervention.
Conclusion
The combination of visceral manipulation and conventional physical therapy program demonstrated significant between-group differences over time for lumbar spine mobility and specific functionality. These gains occurred after 5 sessions, once a week, and were maintained 1 week after the end of the treatment. This study generated data for conduction of a power analysis to inform the design for future clinical research in this line of inquiry.
Funding Sources and Conflicts of Interest
The authors acknowledge financial support from the Brazilian fostering agencies Conselho Nacional de Desenvolvimento Científico e Tecnológico, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, and Fundação de Amparo á Pesquisa. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors declare that they have no conflicts of interest.
Practical Applications
-
•
This study suggests that visceral manipulation associated with an exercise program of physical therapy for patients with chronic low back pain and visceral dysfunction may improve lumbar spine mobility and functionality.
-
•
The participants in this study showed positive effects after 1 week.
-
•
Visceral manipulation associated with an exercise program of physical therapy for patients with chronic low back pain with visceral dysfunction was not superior to an exercise program of physical therapy alone to decrease pain and disability perception in 6 weeks.
Alt-text: Unlabelled Box
Contributorship Information
Concept development (provided idea for the research): L.V.S., H.P.N.
Design (planned the methods to generate the results): L.V.S., H.P.N.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): L.V.S., A.C.B.N.A.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): L.L.C.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): L.L.C., L.A.C.G.
Literature search (performed the literature search): L.V.S., L.L.C.
Writing (responsible for writing a substantive part of the manuscript): L.V.S.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): L.V.S., J.B.P.L., C.S.O.
References
- 1.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Hoy D, Bain C, Williams G. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 3.Saragiotto B, Maher C, Ymato T. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. 2016;1 doi: 10.1002/14651858.CD012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aluko A, DeSouza L, Peacock J. The effect of core stability exercises on variations in acceleration of trunk movement, pain, and disability during an episode of acute nonspecific low back pain: a pilot clinical trial. J Manipulative Physiol Ther. 2013;36(8):497–504.e1-3. doi: 10.1016/j.jmpt.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Bove GM, Chapelle SL. Visceral mobilization can lyse and prevent peritoneal adhesions in a rat model. J Bodyw Mov Ther. 2012;16(1):76–82. doi: 10.1016/j.jbmt.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Brugman R, Fitzgerald K, Fryer G. The effect of osteopathic treatment on chronic constipation–a pilot study. Int J Osteopath Med. 2010;13(1):17–23. [Google Scholar]
- 7.Smith MD, Russell A, Hodges PW. How common is back pain in women with gastrointestinal problems? Clin J Pain. 2008;24(3):199–203. doi: 10.1097/AJP.0b013e31815d3601. [DOI] [PubMed] [Google Scholar]
- 8.Smith MD, Russell A, Hodges PW. Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Aust J Physiotherapy. 2006;52(1):11–16. doi: 10.1016/s0004-9514(06)70057-5. [DOI] [PubMed] [Google Scholar]
- 9.Barwick A, Smith J, Chuter V. The relationship between foot motion and lumbopelvic–hip function: a review of the literature. Foot. 2012;22(3):224–231. doi: 10.1016/j.foot.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. Wolters Kluwer Health/Lippincott Williams & Wilkins; Philadelphia, PA: 2013. [Google Scholar]
- 11.Cervero F. Visceral pain—central sensitisation. Gut. 2000;47(suppl IV):56-57. [DOI] [PMC free article] [PubMed]
- 12.Panagopoulos J, Hancock M, Ferreira P. Does the addition of visceral manipulation improve outcomes for patients with low backpain? Rationale and study protocol. J Bodyw Mov Ther. 2013;17(3):339–343. doi: 10.1016/j.jbmt.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2012;152(suppl 3):1–31. doi: 10.1016/j.pain.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giesecke T, Gracely RH, Grant MAB. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 2004;50(2):613–623. doi: 10.1002/art.20063. [DOI] [PubMed] [Google Scholar]
- 15.Panagopoulos J, Hancock MJ, Ferreira P, Hush J, Petocz P. Does the addition of visceral manipulation alter outcomes for patients with low back pain ? A randomized placebo controlled trial. 2015;19:899-907. [DOI] [PubMed]
- 16.McSweeney TP, Thomson OP, Johnston R. The immediate effects of sigmoid colon manipulation on pressure pain thresholds in the lumbar spine. J Bodyw Mov Ther. 2012;16(4):416–423. doi: 10.1016/j.jbmt.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Tozzi P, Bongiorno D, Vitturini C. Low back pain and kidney mobility: local osteopathic fascial manipulation decreases pain perception and improves renal mobility. J Bodyw Mov Ther. 2012;16(3):381–391. doi: 10.1016/j.jbmt.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P. CONSORT Statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167(1):40–47. doi: 10.7326/M17-0046. [DOI] [PubMed] [Google Scholar]
- 19.Koes BW, van Tulder M, Lin C-WC, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–2094. doi: 10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30(11):1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- 21.Tousignant M, Poulin L, Marchand S, Viau A, Place C. The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: a study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change. Disabil Rehabil. 2005;27(10):553–559. doi: 10.1080/09638280400018411. [DOI] [PubMed] [Google Scholar]
- 22.Nusbaum L, Natour J, Ferraz MB, Goldenberg J. Translation, adaptation and validation of the Roland-Morris questionnaire–Brazil Roland-Morris. Braz J Med Biol Res. 2001;34(2):203–210. doi: 10.1590/s0100-879x2001000200007. [DOI] [PubMed] [Google Scholar]
- 23.Kowalchuk-Horn K, Jennings S, Richardson G, VanVliet D, Hefford C, Abbott JH. The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. J Orthop Sports Phys Ther. 2011;42(1):30–40. doi: 10.2519/jospt.2012.3727. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira L, Costa P, Maher CG. Clinimetric testing of three self-report outcome measures for low back pain patients in Brazil: which one is the best? Spine (Phila Pa 1976) 2008;33(22):2459–2463. doi: 10.1097/BRS.0b013e3181849dbe. [DOI] [PubMed] [Google Scholar]
- 25.Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiother Can. 1995;47:258–263. [Google Scholar]
- 26.Nijs J, Lluch Girbés E, Lundberg M, Malfliet A, Sterling M. Exercise therapy for chronic musculoskeletal pain: innovation by altering pain memories. Man Ther. 2015;20(1):216–220. doi: 10.1016/j.math.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Delitto A, George SZ, Van Dillen L. Low back Pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2012;42(4):1–57. [Google Scholar]
- 28.Langevin HM, Stevens-Tuttle D, Fox JR. Ultrasound evidence of altered lumbar connective tissue structure in human subjects with chronic low back pain. BMC Musculoskelet Disord. 2009;10(1):1–9. doi: 10.1186/1471-2474-10-151. [DOI] [PMC free article] [PubMed] [Google Scholar]