Abstract
Objectives
Recent studies suggest that same-day discharge is safe for the paediatric population after various laparoscopic procedures. Same-day discharge is increasingly common after laparoscopic surgery for uncomplicated appendicitis although it is not standard practice. This prospective study aims to assess parental satisfaction with same-day discharge after laparoscopic appendectomy for uncomplicated appendicitis.
Methods
At our institution, 849 patients with uncomplicated acute appendicitis underwent laparoscopic appendectomy in 2016; of which, 382 were discharged on the same calendar day. Postdischarge surveys assessing parental satisfaction were administered by telephone at the 2-week follow-up.
Results
Approximately 65% of 185 total parental responses reported initial satisfaction with same-day discharge. About 30% were nervous at that time, and 5% did not feel ready to go home yet. Upon reflection, a higher proportion of parents (81.6%) felt same-day discharge was the appropriate course of action, 11.4% were unsure, and 7.0% would not do it again. Some parents cited concerns regarding pain control and incongruous expectations from conversations with staff or surgical experiences of their own.
Conclusions
The majority of parents recalled being happy at discharge, with an increase to 82% retrospectively. Only 7% of parents would not elect to go home on the same day again. Opportunities for improvement include a unified plan from all providers with expectations of same-day discharge if appendicitis is intraoperatively confirmed to be uncomplicated and better analgesic instructions at discharge.
Keywords: Ambulatory, laparoscopic appendectomy, appendicitis, Parental satisfaction, Same-day discharge
The adoption of laparoscopic surgery for many procedures in the 1990s has led to shorter hospital stays, decreased wound infections, and decreased pain (1,2). Since this time, laparoscopic approaches to uncomplicated acute appendicitis in paediatric patients have become standard of care (3). Many laparoscopic procedures have the benefit of being performed on an outpatient basis. It has been demonstrated that it is safe to send paediatric patients home the same day after laparoscopic appendectomy for uncomplicated appendicitis (4,5). Other institutions have evaluated their parental satisfaction with same-day discharge after appendectomy and found high rates of satisfaction among parents (4). Until recently, our institution routinely admitted all patients overnight for postoperative monitoring after an appendectomy, regardless of the time of day the appendectomy was performed.
As part of a prospective study evaluating the safety and feasibility of same-day discharge after laparoscopic appendectomy, we collected survey information from parents to evaluate their satisfaction level with the process. Our goal was to assess parental satisfaction with same-day discharge after laparoscopic appendectomy for uncomplicated appendicitis. We hypothesized that greater than 80% of the parents of patients discharged same day would be satisfied with patient recovery at home.
METHODS
After institutional review board approval (#STU 082015-081), electronic medical records for patients aged 2 to 18 years, who underwent laparoscopic appendectomy in 2016, were reviewed. Data were collected regarding demographics (Table 1) as well as dates and times of admission, surgery, and discharge. Data such as postoperative complications, emergency department (ED) or unscheduled office visits, and readmissions were also collected to separately study safety outcomes of same-day discharge. Inclusion criteria were same-day discharge, defined as discharge on the same calendar day of surgery. Patients undergoing scheduled interval appendectomies were excluded. Patients with complicated appendiceal pathology such as perforation or gangrenous appendicitis were excluded. Patients with additional abdominal pathology, such as malrotation or ovarian torsion, were excluded.
Table 1.
Demographics of patients discharged same day
| Feature | Number (per cent) |
|---|---|
| Sex | |
| Female | 147 (38%) |
| Age | |
| 0–6 | 41 (11%) |
| 7–12 | 216 (57%) |
| 13–18 | 125 (32%) |
| Race | |
| Caucasian or White | 256 (68%) |
| Black or African American | 21 (5%) |
| Asian | 9 (3%) |
| Hispanic | 37 (9%) |
| Other | 38 (10%) |
| Unknown | 21 (5%) |
Of 849 patients that had a laparoscopic surgical approach for acute uncomplicated appendicitis, 382 were discharged on the same calendar day. Decision for same-day discharge was made based on surgeon evaluation and preference along with parental agreement. Same-day discharge was most often initially discussed at time of consultation if deemed appropriate based on clinical appearance and imaging studies. The decision to discharge the same day after surgery was made in conjunction with parental agreement, reassessing appropriateness (based on intraoperative gross pathology and patient’s clinical appearance post-op) and parental consent after the surgery itself. Some patients were discharged after observation from the post anesthesia care unit (PACU) while others were discharged same day after a brief period of observation on the floor depending on whether or not the patient had been admitted prior to surgery. If at any point a parent did not wish to be discharged same day, the request was honoured.
The study population of patients discharged same day was surveyed, most often during the standard 2-week postoperative follow-up phone call from nurses in the Paediatric Surgery Clinic as routinely practiced at our institution for uncomplicated appendicitis. If the clinic nurses were unable to reach a parent after multiple calls and voicemails, a letter was sent to the family’s home requesting the family call the clinic. Finally, author SN attempted to reach the family again by phone. Language interpreters were used when needed.
The survey (Figure 1) questioned parent or guardian feelings about same-day discharge 1) at the time of discharge and 2) in retrospect at the time of follow-up, giving three choices for each question. The final question open-endedly asked parents to provide additional feedback regarding any part of the same-day discharge process.
Figure 1.
Postdischarge survey script.
RESULTS
Recalled satisfaction at time of discharge
One hundred and eighty-five (48.4%) parents of the study population responded to the survey. Of these, 121 (65.4%) reported initial satisfaction with same-day discharge, 55 (29.7%) reported feeling nervous at first, and 9 (4.9%) did not feel ready immediately after surgery Subgroup analysis of patients discharged between 07:00 and 19:00 compared with the patients discharged between 19:00 and 07:00 (‘after hours’) showed no significant difference in satisfaction (satisfied P=0.68; nervous P=0.96; not ready P=0.43) (Table 2). Importantly, when comparing the 48.4% of survey respondents with the 51.6% of survey nonrespondents, there was no difference in the number of complications between the two cohorts (Table 3). Both responders and nonresponders had a similar rate of abscess formation (0 versus 1 patient, P=0.34), in the number of surgical site infections (2 versus 2 patients, P=0.92) and in the number of patients with pain control issues (15 versus 16 patients, P=1.0).
Table 2.
Parental responses to survey
| At discharge (Q1) Number of responses (%) |
In retrospect (Q2) Number of responses (%) |
|||||
|---|---|---|---|---|---|---|
| Between 7a-7p (n=125) | After hours (n=60) | Significance | Between 7a-7p (n=125) | After hours (n=60) | Significance | |
| Positive | 83 (66.4%) | 38 (63.3%) | p=0.68 | 104 (83.2%) | 47 (78.3%) | p=0.42 |
| Uncertain | 37 (29.6%) | 18 (30%) | p=0.96 | 15 (12%) | 6 (10%) | p=0.69 |
| Negative | 5 (4%) | 4 (6.7%) | p=0.43 | 6 (4.8%) | 7 (11.7%) | p=0.08 |
Q1: question 1, Q2: question 2
Table 3.
Comparison of complications between survey responders and nonresponders
| Same-day discharge (n=382) | |||
|---|---|---|---|
| Survey responders (n=185) | Nonresponders (n=197) | Significance (P) | |
| Abscess | 0 (0%) | 1 (0.5%) | 0.34 |
| Nausea/vomiting | 4 (2.2%) | 6 (3%) | 0.62 |
| Pain control | 15 (8.1%) | 16 (8.1%) | 1.0 |
| Surgical site infection | 2 (1.1%) | 2 (1%) | 0.92 |
Satisfaction at 2-week follow-up
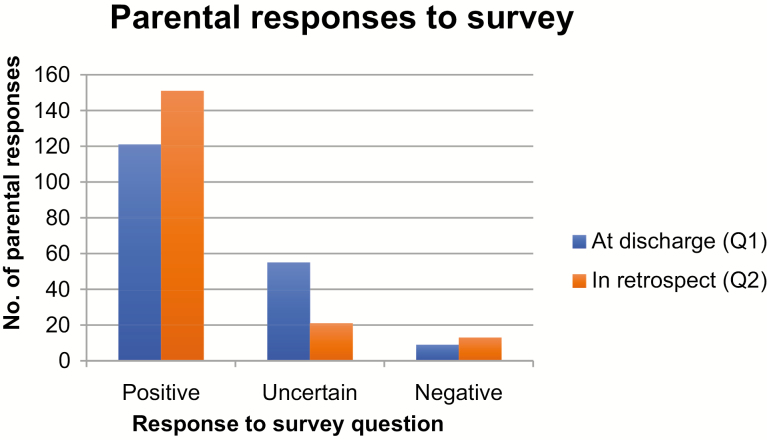
In retrospect, a higher proportion of parents (81.6%) felt that same-day discharge was the correct process for their child. Twenty-one (11.4%) felt unsure that it was best, and 13 (7.0%) would not do it again (Figure 2). Again, there was no statistically significant difference between parental satisfaction in patients discharged same day (i.e., surgery between 07:00 and 19:00) when compared with the patients discharged ‘after hours’ (positive P=0.42; unsure P=0.69; not again P=0.08).
Figure 2.
Parental responses to survey (graph). Q1: question 1, Q2: question 2.
Additional feedback from parental survey
Fifteen parents reported pain as a concern when asked to provide comments. Of these, 13 felt unsure or would not go home the same day again. The other two parents ultimately felt that same-day discharge was appropriate despite their child initially having pain. Four parents reported acetaminophen and ibuprofen were not adequate for pain control. Three parents reported significant pain on the drive home. Five parents reported calling an ambulance or returning to the emergency room due to pain.
Eleven parents mentioned expectations that influenced how they felt about same-day discharge; two reported personal laparoscopic surgeries that required longer recoveries; as a result, one felt unsure about same-day discharge, but the other felt satisfied in this situation. One parent expressed initial nervousness because appendectomies were historically a considerable procedure but was ultimately satisfied with same-day discharge. One parent was unsure because it was the patient’s first surgery. Some parents expected certain milestones (e.g., urinating, eating, overnight observation) to be met prior to discharge.
Other parents had expectations that were set by staff. Four were surprised to be going home on the same day after surgery. Of those, three were initially nervous about it, and two were ultimately satisfied while the third would not do same-day discharge again. Three parents reported the expectation that same-day discharge was set by nurses and staff, and they were satisfied. Additionally, some parents reported they would choose to go home immediately after surgery again, stating that their child recovered better at home.
DISCUSSION
Appendicitis is the most common diagnosis for paediatric patients admitted for abdominal pain (6) that requires surgical intervention in the USA (7). It affects four of every 1,000 children (6), and in a review of 1.9 million discharges from 1997, it was the leading diagnosis in total number of hospital days for a gastrointestinal disorder, amassing $680.4 million in charges that year. At that time, children were routinely monitored postoperatively regardless of presence of perforation, and the mean length of hospital stay was 3.3 days (8).
Since 1997, laparoscopy has become the preferred approach to appendectomy, compared to open appendectomy, A 2004 review article demonstrated evidence of decreased incidence of wound infection, decreased reports of pain on the first postoperative day, shortened hospital stays, and earlier return to normal activity (2) with a 2010 meta-analysis supporting these findings (9). Additionally, a meta-analysis of the paediatric population showed decreased incidence of ileus after laparoscopic appendectomy (1).
Decreased recovery time after laparoscopic appendectomy compared to open appendectomy led to the question: is same-day discharge after laparoscopic appendectomy feasible without compromising patient safety? In studies comparing the time of discharge in relation to surgery, adult patients hospitalized postoperatively were more likely to be readmitted within 30 days than patients that were discharged on the same day (10). In paediatric patients, the readmission rate was not significantly increased for patients discharged the same day after surgery compared with the patients who were hospitalized (11) and was found to be slightly less in the same-day discharge population although not significantly so (1.89% versus 2.33%, P=0.06) (12). This reduction in hospitalization has implications for decreasing costs for patients and hospitals alike (13,14).
Decreased financial burden without risking additional complications is a major benefit of same-day discharge after laparoscopic appendectomy for uncomplicated acute appendicitis. However, it must be balanced by the surgeon’s discretion and patient/guardian preference. At our institution, same-day discharge is a fairly new practice, and some surgeons preferred to have more data prior to changing their practice, contributing to the 40% same-day discharge rate amongst the uncomplicated appendicitis population. Traditionally, patients at Children’s Health were observed overnight postoperatively, often with an uneventful course prior to discharge the following morning, regardless of what time of day their appendectomy had occurred. This led to some patients staying over 24 hours and some less than 12, after the same procedure. Follow-up clinic visits have become replaced by telephone calls 2 weeks postoperatively due to historically high no-show rate for appointments, with the additional benefits of reducing unnecessary travel, costs, and days off of school and work. This likely increased the number of patients who did not respond to the follow-up phone call. However, the rate of response correlates with our general response rate for all appendectomies, of which over 1,000 are performed annually at Children’s Health. Of the 382 patients included in our study, 185 parents (48.4%) were ultimately reached via telephone for follow-up and completion of the satisfaction survey regarding same-day discharge. When compared to the remaining 197 families that were discharged same day but did not respond to the survey, survey responders had similar rates of complications on chart review of telephone encounters, extra clinic appointments, ED visits, and readmissions. It is important to note that the survey was a limitation in our study as it was not composed of a previously validated set of questions to determine satisfaction and also relied entirely on parental recall.
Of the paediatric patients discharged on the same calendar day as their operation, the majority of the parents who responded to the follow-up phone call were satisfied with same-day discharge. The percentage of satisfied parents increased from 65% to 82% when asked how they felt about same-day discharge in retrospect at the 2-week follow-up telephone call. Thirty-two of the initial 55 who were nervous ultimately felt that same-day discharge was the best decision. Of the remaining parents, pain control and discordant expectations were commonly cited reasons for reporting uncertainty or dissatisfaction about same-day discharge.
Eight per cent of the study population reported concern about home pain control. Parents were advised to schedule acetaminophen and alternate with scheduled ibuprofen around the clock at home. However, it is studied that parental recall of instructions upon discharge can be improved (15) and even more so when asked to administer more than one medication (16). Giving standardized instructions via trained staff or students improved parent understanding compared to controls (17). The strategy of dispensing analgesic medications to parents also had good adherence (15,18), especially in a population in which weight-based dosing is utilized. Additionally, as constipation is a common cause of postoperative abdominal pain in children (19) (including 70% of our study population that presented to the ED), providing proper instructions to prevent constipation may further improve overall pain control and parental satisfaction.
Finally, nearly 6% of surveyed parents reported discordant expectations. When developing future protocols for same-day discharge, education should be included about the procedure, its safety, and the probability of uncomplicated intraoperative findings. Improved communication regarding the safety, benefit, and expectation of same-day discharge as well as regarding pain management and prevention may further increase the percentage of parents satisfied with same-day discharge after laparoscopic approach to uncomplicated acute appendicitis.
This study was designed to evaluate the parental satisfaction within the same-day discharge population as it contributes to the feasibility of same-day discharge; however, a future noninferiority study would be beneficial to compare satisfaction between paediatric patients discharged same-day and observed overnight after laparoscopic appendectomy. Furthermore, additional studies should focus on the impact of social factors (e.g., distance from the hospital, access to transportation, and household income) on parental satisfaction with same-day discharge in order to identify patients appropriate for same-day discharge by incorporating both clinical judgment and social factors. A protocol that standardizes patient selection for same-day discharge, early expectation of process, and parental education on postoperative management may impact parental satisfaction with same-day discharge, and thus impact healthcare costs after laparoscopic appendectomy for uncomplicated appendicitis.
CONCLUSIONS
Same-day discharge is well received by parents of patients with uncomplicated appendicitis who underwent laparoscopic appendectomy. The majority of parents recall their initial reactions as positive, and at the 2-week follow-up, an even higher percentage of parents felt satisfied with same-day discharge. Considering high levels of parental satisfaction with studied safety and feasibility of same-day discharge, this process should be considered for this population.
Funding Information: There are no funders to report for this submission.
Potential Conflicts of Interest: All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Work originated and approved by IRB at Children’s Health.
References
- 1. Aziz O, Athanasiou T, Tekkis PP, et al. Laparoscopic versus open appendectomy in children: A meta-analysis. Ann Surg 2006;243(1):17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2004(4):CD001546. [DOI] [PubMed] [Google Scholar]
- 3. Rentea RM, Peter SDS, Snyder CL. Pediatric appendicitis: State of the art review. Pediatr Surg Int 2017;33:269–83. [DOI] [PubMed] [Google Scholar]
- 4. Alkhoury F, Malvezzi L, Knight CG, et al. Routine same-day discharge after acute or interval appendectomy in children: A prospective study. Arch Surg 2012;147(5):443–6. [DOI] [PubMed] [Google Scholar]
- 5. Aguayo P, Alemayehu H, Desai AA, Fraser JD, St Peter SD. Initial experience with same day discharge after laparoscopic appendectomy for nonperforated appendicitis. J Surg Res 2014;190(1):93–7. [DOI] [PubMed] [Google Scholar]
- 6. McCollough M, Sharieff GQ. Abdominal surgical emergencies in infants and young children. Emerg Med Clin North Am 2003;21(4):909–35. [DOI] [PubMed] [Google Scholar]
- 7. Sømme S, Bronsert M, Morrato E, Ziegler M. Frequency and variety of inpatient pediatric surgical procedures in the united states. Pediatrics 2013;132(6):e1466–72. [DOI] [PubMed] [Google Scholar]
- 8. Guthery SL, Hutchings C, Dean JM, Hoff C. National estimates of hospital utilization by children with gastrointestinal disorders: Analysis of the 1997 kids' inpatient database. J Pediatr 2004;144:589–94. [DOI] [PubMed] [Google Scholar]
- 9. Li X, Zhang J, Sang L, et al. Laparoscopic versus conventional appendectomy--a meta-analysis of randomized controlled trials. BMC Gastroenterol 2010;10:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Scott A, Shekherdimian S, Rouch JD, et al. Same-day discharge in laparoscopic acute non-perforated appendectomy. J Am Coll Surg 2017;224(1):43–8. [DOI] [PubMed] [Google Scholar]
- 11. Litz CN, Stone L, Alessi R, et al. Impact of outpatient management following appendectomy for acute appendicitis: An ACS NSQIP-P analysis. J Pediatr Surg 2017;53(4):625–8. doi: 10.1016/j.jpedsurg.2017.06.023 [DOI] [PubMed] [Google Scholar]
- 12. Cairo SB, Raval MV, Browne M, Meyers H, Rothstein DH. Association of same-day discharge with hospital readmission after appendectomy in pediatric patients. JAMA Surg 2017;152(12):1106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dubois L, Vogt KN, Davies W, Schlachta CM. Impact of an outpatient appendectomy protocol on clinical outcomes and cost: A case-control study. J Am Coll Surg 2010;211(6):731–7. [DOI] [PubMed] [Google Scholar]
- 14. Farach SM, Danielson PD, Walford NE, Harmel RP Jr, Chandler NM. Same-day discharge after appendectomy results in cost savings and improved efficiency. Am Surg 2014;80(8):787–91. [PubMed] [Google Scholar]
- 15. Hegarty M, Calder A, Davies K, et al. Does take-home analgesia improve postoperative pain after elective day case surgery? A comparison of hospital vs parent-supplied analgesia. Paediatr Anaesth 2013;23(5):385–9. [DOI] [PubMed] [Google Scholar]
- 16. Grover G, Berkowitz CD, Lewis RJ. Parental recall after a visit to the emergency department. Clin Pediatr (Phila) 1994;33(4):194–201. [DOI] [PubMed] [Google Scholar]
- 17. Isaacman DJ, Purvis K, Gyuro J, Anderson Y, Smith D. Standardized instructions: Do they improve communication of discharge information from the emergency department?Pediatrics 1992;89(6 Pt 2):1204–8. [PubMed] [Google Scholar]
- 18. Walther-Larsen S, Aagaard GB, Friis SM, Petersen T, Møller-Sonnergaard J, Rømsing J. Structured intervention for management of pain following day surgery in children. Paediatr Anaesth 2016;26(2):151–7. [DOI] [PubMed] [Google Scholar]
- 19. Loening-Baucke V, Swidsinski A. Constipation as cause of acute abdominal pain in children. J Pediatr 2007;151(6):666–9. [DOI] [PubMed] [Google Scholar]