Abstract
Licorice has been used as a medicinal plant from 2.500 years. It shows a wide range of biological and pharmacological activities, including anti-inflammatory and immune regulatory actions. One of its most known effects is the induction of hypertension, and it can induce what appears to be pseudohyperaldosteronism, due to glycyrrhetinic acid, the main active component of the root. Glycyrrhetinic acid and metabolites block the 11 beta-hydroxysteroid dehydrogenase type 2 and also bind mineralocorticoid receptors directly, acting as agonists. However, other interesting therapeutic uses of licorice are linked to its anti-androgen and estrogen-like activity, especially in the treatment of polycystic ovary syndrome (PCOS) in conjunction with spironolactone therapy. In this brief review, we report the main features and possible therapeutic uses of this ancient plant.
Keywords: licorice, aldosterone, polycystic ovary syndrome (PCOS), pseudohyperaldosteronism, glycyrrhetinic acid (GA), hypertension, inflammation
Introduction
Licorice is a perennial plant, native to Mediterranean area and Asia Minor, studied for a long time as for its several biological and endocrine properties. The main constituents are triterpene saponins, whose main component is glycyrrhizic acid (GI) that is hydrolyzed into glycyrrhetinic acid (GA) in the stomach and duodenum. Other important constituents are flavonoids, such as glabridin, accounting about 1–24% of the root weight dependent on the species.
Licorice has been used as a medicinal plant for 2,500 years and its ancient applications were confirmed by recent scientific studies (1). In the fourth century B.C., Teophrastus reported that the Scythians were able to survive in the desert eating licorice roots as a thirst quencher and this effect was due to sodium and water retention, subsequently ascribed to the mineralocorticoid effect of licorice (2). Its most frequent side effect is pseudohyperaldosteronism, a clinical condition characterized by hypertension, hypokalemia and suppression of plasma renin and aldosterone levels (3). These effects were first reported by Revers in 1946 (4), and until 1970, licorice intoxication was a frequent cause of factitious hypertension and hypokalemia. Pseudohyperaldosteronism can be due to prolonged intake not only of licorice roots, but also of products flavored with licorice to ameliorate the taste, such as herbal products, candies, breath fresheners, tobacco, teas, and even laxatives (5). However, many other endogenous or exogenous conditions can lead to pseudohyperaldosteronism, such as Liddle's Syndrome, Cushing's syndrome, apparent mineralocorticoid excess (AME) syndrome, prolonged use of grapefruit (6), intake of fludrocortisone, and some enzyme deficiencies, such as deficiencies of 11 hydroxylase, 17 alpha-hydroxylase, or 5 alpha-reductase (7). The knowledge of the effects of overconsumption of mineralocorticoid-like substances has reduced the prevalence of this pathological condition.
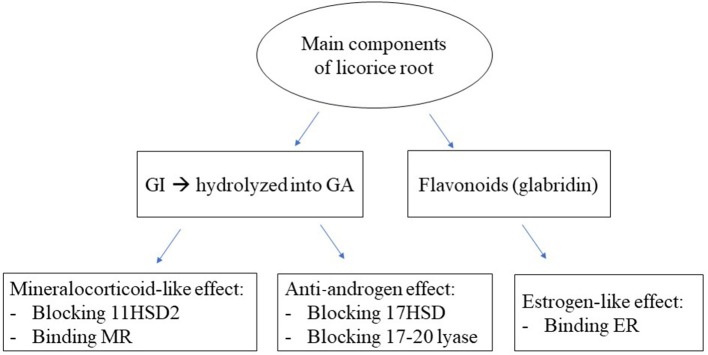
Moreover, licorice has several other clinical applications, due to its anti-androgen and estrogen-like activity (Figure 1), that are especially used in the treatment of polycystic ovary syndrome (PCOS) in association with spironolactone, a mineralocorticoid receptor (MR) blocker.
Figure 1.
Endocrine effects of the main components of licorice. GI, glycyrrhizic acid; GA, glycyrrhetinic acid; 11HSD2, 11 beta-hydroxysteroid dehydrogenase 2; MR, mineralocorticoid receptor; 17HSD, 17 hydroxysteroid dehydrogenase; ER, estrogen receptor.
In this brief review, we report the features, mechanisms of endocrine actions and the possible therapeutic uses of licorice and its derivatives, focusing mainly on in vitro and in vivo studies in humans.
The Mineralocorticoid Effect and the Mechanism of Pseudohyperaldosteronism
Aldosterone is the main mineralocorticoid, produced by the zona glomerulosa of the adrenal cortex, and it is mainly regulated by angiotensin II and potassium. It regulates electrolyte and water balance, and consequently blood pressure, by stimulating gene expression of serum-glucocorticoid-inducible kinase 1 (SGK1) and epithelial sodium channel (ENaC), involved in sodium and potassium regulation and reabsorption in renal tissues (8). Aldosterone exerts its effects via the MR, which belongs to the nuclear receptor superfamily and acts as a ligand-dependent transcription factor (9).
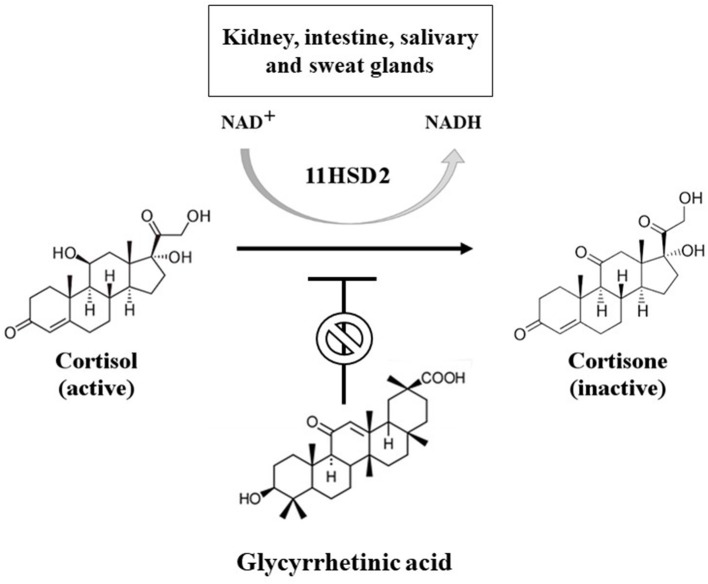
Cortisol, the main glucocorticoid, and aldosterone bind the MR with similar affinity, but cortisol levels are 100–1,000 times higher than that of aldosterone. For this reason, in the classical target tissues of aldosterone, such as kidney, intestine and salivary and sweat glands, the MR activation is regulated by the presence of the enzyme 11 beta-hydroxysteroid dehydrogenase type 2 (11HSD2), which inactivates cortisol to cortisone (Figure 2). Cortisone has no affinity for MR and glucocorticoid receptor, ensuring the activation of the MR only by aldosterone. However, if the enzyme is saturated (by significantly increased cortisol levels, such as in Cushing's syndrome) or mutated (as in AME syndrome) or blocked (as during prolonged intake of licorice), cortisol is able to bind and activate MR, leading to a pseudohyperaldosteronism (7).
Figure 2.
Mechanism of conversion of cortisol into cortisone through 11 beta-hydroxysteroid dehydrogenase 2 (11HSD2). This enzyme is a NAD-dependent dehydrogenase enzyme, mainly expressed in the kidney, intestine, salivary and sweat glands. It can be inhibited by glycyrrhetinic acid, leading to functional mineralocorticoid excess due to unmetabolized cortisol at the level of classical target tissues of aldosterone.
Licorice-induced pseudohyperaldosteronism is mainly due to GA, which acts through two different mechanisms (Figure 1): it can block 11HSD2 (Figure 2) and directly bind to the MR as an agonist, with an affinity of about 5,000 times lower than aldosterone, evaluated in kidney cytosol or kidney slices from adrenalectomized rats (10). However, during chronic overconsumption of licorice, plasma concentrations of GA support a direct effect of GA at the MR level, notwithstanding the low affinity (11). Moreover, it has been demonstrated in human mononuclear leukocytes (MNL) by radioreceptor assay that the mineralocorticoid effector mechanism of GA can be reversed by coincubation with canrenone, a MR blocker, derivative of spironolactone (11). The effect on the 11HSD2 occurs even with relatively low serum concentrations of GA, while the binding to MR starts later when the substance has accumulated in the blood (12).
The accurate personal history, including a detailed dietary and drug history, and the measurement of renin, aldosterone and serum and urinary electrolytes are necessary for an accurate diagnosis of these forms of hypertension (13). The more accurate parameter to diagnose the reduced function of 11HSD2 is the measurement of the urinary cortisol metabolites, represented by the increased urinary cortisol/cortisone or urinary tetrahydrocortisol+allo-tetrahydrocortisol (TFH+alloTHF)/tetrahydrocortisone (THE) ratios (14). Increased urinary cortisol/cortisone ratio is an important tool, also for the differential diagnosis with Cushing's syndrome, since cortisol levels can be very high during chronic licorice intake (15).
The features of pseudohyperaldosteronism are linked to individual factors, such as the age, the gender, a previous history of hypertension, the time of transit and hydrolysis of GI to GA in the stomach and duodenum (10). Cessation of licorice intake and, in some cases, treatment with MR blockers can recover the abnormalities, but sometimes hypertension can persist due to other causes, as reported in some cases of primary aldosteronism after adrenalectomy.
Mineralocorticoids, Licorice and Inflammation
In the last few decades, many studies have evaluated the role of aldosterone not only in the sodium balance and hypertension, but also in the pathogenesis of inflammation (16). This effect was hypothesized by Selye immediately after the discovery of the first mineralocorticoid, deoxycorticosterone (DOC). He reported an inflammatory activity of DOC in contrast to the anti-inflammatory action of glucocorticoids (17). The inflammatory effect of aldosterone is mediated through MR and non-genomic pathways not yet deeply clarified (16). Therefore, all the substances with a mineralocorticoid-like action may induce not only alterations of electrolytes and hypertension, but also inflammatory reactions in several tissues.
Since 1980, aldosterone excess has been reportedly involved in the inflammatory reaction, heart fibrosis, cardiovascular and cerebrovascular risk and atrial fibrillation. The protective effect of MR blockers, like spironolactone, canrenone, potassium canrenoate and eplerenone, to prevent the inflammatory effect of aldosterone in non-epithelial cells, was evidenced in the studies of Pitt and collaborators in patients with severe heart failure. The authors reported a significant reduction of the prevalence of heart failure relapse and cardio-cerebrovascular accidents when the MR blockers were added to the conventional treatments of these pathological conditions (18–20). The protective effect of MR blockers is opposite to the effect of other diuretics that increase aldosterone secretion and inflammatory reaction (21, 22). Recent researches are exploring the protective effect of spironolactone as an anti-inflammatory and immunomodulatory agent even in the treatment of other pathological conditions, such as rheumatoid arthritis and central serous chorioretinopathy (23, 24).
We investigated the inflammatory effect of aldosterone using MNL, which are the cells mainly involved in inflammation. In 1985, we characterized MR in MNL (25), and subsequently, we showed that in vitro aldosterone and GA were able to regulate the intracellular concentration of electrolytes (26) and the cellular volume (27), through both genomic and non-genomic pathways (28). In 2004 we investigated a possible involvement of aldosterone in the MNL model (29). Incubation of mononuclear cells with aldosterone enhanced the protein expression of PAI-1 and p22phox, two markers of inflammation. The effect of aldosterone was reversed by coincubation with canrenone. In the same study, we also evaluated the effect of GA, which was similar to aldosterone at concentrations consistent with its affinity for MR.
Licorice as Anti-Inflammatory: the Erythrocyte Model
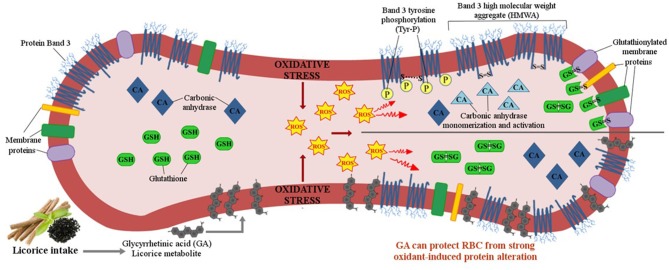
In erythrocytes, the proinflammatory effect has been evaluated by the increased sensitivity to diamide, a mild oxidant able to trigger the tyrosine phosphorylation (Tyr-P) of erythrocyte membrane proteins, mainly band 3 (30). The increased band 3 Tyr-P levels correlate with chronic deficiency of cellular anti-oxidative defenses. A previous study demonstrated that GA prevents the erythrocyte alterations induced by diamide in a dose-dependent manner, preserving membrane integrity against oxidative and proteolytic damage (31) (Figure 3). These effects mediated by GA are opposite from those of aldosterone, that exacerbates the alterations induced by diamide. The prooxidative effect of aldosterone was confirmed in both in vitro studies, incubating erythrocytes from healthy volunteers with increasing aldosterone concentrations, and in vivo experiments, evaluating erythrocytes from patients with primary aldosteronism (30). The erythrocyte membrane alterations were mediated by aldosterone in a dose- and time-dependent manner and were almost completely prevented by canrenone or cortisol, suggesting a non-genomic effect mediated by MR (32). Moreover, aldosterone-related alterations led to increased autologous IgG binding, which could induce premature erythrocyte removal from circulation (30).
Figure 3.
Red blood cell (RBC) membrane alterations induced by oxidative stress and the possible anti-inflammatory effect of licorice. Glycyrrhetinic acid (GA), which has been shown to directly interact with membrane sphingolipids and cholesterol, can induce a protective shield against membrane protein oxidation, mainly avoiding protein band 3, the main constituents of RBC membranes, from being oxidized by ROS to form high molecular weight aggregate (HMWA), recognized by circulating IgG as premature aged cells. GA also prevents protein glutathionylation, which would avoid cytosolic GSH store depletion and support the correct functioning of cytosolic enzymes such as Carbonic Anhydrase (CA2).
The discrepancy between the effects of GA in MNL and erythrocytes demands an explanation. The protective effect could be related to a direct interaction of GA at the level of plasma membrane (30), not mediated by MR, preventing membrane protein oxidation (Figure 3) and/or to the glucocorticoid activity of GA (10). These data suggest that licorice can induce pseudohyperaldosteronism and an inflammatory reaction related to the binding to MR and to the blocking of 11HSD2, but it can also show anti-inflammatory and antiatherosclerotic (33) effects modulating cellular membrane fluidity and oxidative stress, and showing an estrogen-like (34) and glucocorticoid-like activity (10).
Therapeutic Use of Licorice
Licorice root has been widely used for several therapeutic properties. In particular, GA has antiviral and antimicrobial activities, stimulating T-helper 1 immune response and the interferon gamma secretion (35). Licorice has also been used in the treatment of the chronic fatigue syndrome (36) and of Addison's disease, especially before the discovery of fludrocortisone (37): these effects are due to the reduced inactivation of cortisol in cortisone through the block of 11HSD2, even when cortisol production is reduced, and to the binding to the MR. These properties have been applied even in the treatment of postural hypotension in some diabetic patients with secondary hypoaldosteronism (38).
In recent years, the most fascinating use of licorice has been in the treatment of PCOS. We previously demonstrated that licorice can decrease the secretion of testosterone both in men and in women (39, 40). In healthy men this effect is not usually relevant, as the serum concentrations of testosterone are relatively high, while in women affected by hyperandrogenism, as in PCOS, the anti-androgen effect of licorice can be important, especially when associated with spironolactone. Spironolactone acts not only as MR blocker, but also as androgen receptor antagonist, affecting both gonadal and adrenal steroidogenesis and causing sex steroid-related clinical manifestations, such as impotence and gynecomastia in men, and menstrual irregularities and breast tenderness in women. Therefore, it is widely used in the treatment of PCOS, being effective for hirsutism, acne, effluvium capillorum and other clinical signs of hyperandrogenism (41). However, during treatment, patients may complain about side effects due to its anti-mineralocorticoid effect, causing hypotension and hyperkalemia. The addition of licorice can blunt the diuretic activity of spironolactone and enhance the anti-androgen effect (Figure 1), reducing androgen secretion by blocking the 17 hydroxysteroid dehydrogenase and 17–20 lyase in the ovaries and adrenals (42). It is worth noting that licorice can also reduce the prevalence on intermenstrual bleeding occurring in about 20–50% of women taking spironolactone (43). This effect could be related to the stimulation of aromatase activity and/or to the estrogen-like effect of glabridin, a flavonoid present in some commercial preparations of licorice (44). Recent studies support the estrogen-like effect of glabridin even at the level of bones in rats with ovariectomized-induced osteoporosis (45). All these properties of licorice can explain the use of the root even in the past as a remedy for sterility of women, reducing biochemical hyperandrogenism and improving ovulation rate (40), and probably as a sort of natural alternative to hormonal replacement therapy, improving symptoms of estrogen depletion (34). The effectiveness of herbal medicine containing licorice has been recently proven even in overweight PCOS patients (46). PCOS patients frequently have insulin-resistance, obesity and an increased risk of developing metabolic syndrome and cardiovascular disease, partially related to a proinflammatory systemic status (47) and a relative hyperaldosteronism (48) associated to this condition. These findings support the use of spironolactone in this syndrome and the cotreatment with licorice may improve even the metabolic alterations (49), blocking 11HSD1, and thus, reducing the availability of cortisol at the level of adipocytes. Indeed, in a previous study, we reported that the use of a cream containing 2.5% GA for 1 month significantly reduced the thickness of the superficial fat layer in comparison to a placebo cream, without changes in blood pressure, plasma renin, aldosterone and cortisol values (50).
In conclusion, licorice extracts have been used for more than 2,000 years as a medicinal plant and its consumption should not be limited by the possible onset of pseudohyperaldosteronism, since it can offer many other interesting therapeutic applications.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Armanini D, Fiore C, Mattarello MJ, Bielenberg J, Palermo M. History of the endocrine effects of licorice. Exp Clin Endocrinol Diabetes. (2002) 110:1–5. 10.1055/s-2002-34587 [DOI] [PubMed] [Google Scholar]
- 2.Fiore C, Eisenhut M, Ragazzi E, Zanchin G, Armanini D. A history of the therapeutic use of liquorice in Europe. J Ethnopharmacol. (2005) 99:317–24. 10.1016/j.jep.2005.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conn JW, Rovner DR, Cohen EL. Licorice-induced pseudoaldosteronism. Hypertension, hypokalemia, aldosteronism, and suppressed plasma renin activity. JAMA. (1968) 205:492–6. 10.1001/jama.205.7.492 [DOI] [PubMed] [Google Scholar]
- 4.Revers FE. Heedt succus liquiritiae een gegenzde werking of de maagweer? Nedl Tijdschr Geneesk. (1946) 90:135–7. [PubMed] [Google Scholar]
- 5.Scali M, Pratesi C, Zennaro MC, Zampollo V, Armanini D. Pseudohyperaldosteronism from liquorice-containing laxative. J Endocrinol Invest. (1990) 13:847–8. 10.1007/BF03349639 [DOI] [PubMed] [Google Scholar]
- 6.Palermo M, Armanini D, Delitala G. Grapefruit juice inhibits 11beta-hydroxysteroid dehydrogenase in vivo, in man. Clin Endocrinol. (2003) 59:143–4. 10.1046/j.1365-2265.2003.01806.x [DOI] [PubMed] [Google Scholar]
- 7.Sabbadin C, Armanini D. Syndromes that mimic an excess of mineralocorticoids. High Blood Press Cardiovasc Prev. (2016) 23:231–5. 10.1007/s40292-016-0160-5 [DOI] [PubMed] [Google Scholar]
- 8.Booth RE, Johnson JP, Stockand JD. Aldosterone. Adv Physiol Educ. (2002) 26:8–20. 10.1152/advan.00051.2001 [DOI] [PubMed] [Google Scholar]
- 9.Fuller PJ, Yao Y, Yang J, Young MJ. Mechanisms of ligand specificity of the mineralocorticoid receptor. J Endocrinol. (2012) 213:15–24. 10.1530/JOE-11-0372 [DOI] [PubMed] [Google Scholar]
- 10.Armanini D, Karbowiak I, Funder JW. Affinity of licorice derivatives for mineralocorticoid and glucocorticoid receptors. Clin Endocrinol. (1983) 19:606–12. 10.1111/j.1365-2265.1983.tb00038.x [DOI] [PubMed] [Google Scholar]
- 11.Armanini D, Wehling M, Weber PC. Mineralocorticoid effector mechanism of licorice derivates in human mononuclear leukocytes. J Endocrinol Invest. (1989) 12:303–6. 10.1007/BF03349993 [DOI] [PubMed] [Google Scholar]
- 12.Armanini D, Lewicka S, Pratesi C, Scali M, Zennaro MC, Zovato S, et al. Further studies on the mechanism of the mineralocorticoid action of licorice in humans. J Endocrinol Invest. (1996) 19:624–9. 10.1007/BF03349029 [DOI] [PubMed] [Google Scholar]
- 13.Sontia B, Mooney J, Gaudet L, Touyz RM. Pseudohyperaldosteronism, liquorice, and hypertension. J Clin Hypertens. (2008) 10:153–7. 10.1111/j.1751-7176.2008.07470.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White PC, Mune T, Agarwal AK. 11 beta-Hydroxysteroid dehydrogenase and the syndrome of apparent mineralocorticoid excess. Endocr Rev. (1997) 18:135–56. 10.1210/edrv.18.1.0288 [DOI] [PubMed] [Google Scholar]
- 15.Ceccato F, Trementino L, Barbot M, Antonelli G, Plebani M, Denaro L, et al. Diagnostic accuracy of increased urinary cortisol/cortisone ratio to differentiate ACTH-dependent Cushing's syndrome. Clin Endocrinol. (2017) 87:500–7. 10.1111/cen.13391 [DOI] [PubMed] [Google Scholar]
- 16.Sabbadin C, Calò LA, Armanini D. The story of spironolactones from 1957 to now: from sodium balance to inflammation. G Ital Nefrol. (2016) 33.S66.12. [PubMed] [Google Scholar]
- 17.Selye H. Stress and inflammation. Am J Proctol. (1953) 4:229–30. [PubMed] [Google Scholar]
- 18.Pitt B, Zannad F, Remme W, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. (1999) 341:709–17. 10.1056/NEJM199909023411001 [DOI] [PubMed] [Google Scholar]
- 19.Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. (2003) 348:1309–21. 10.1056/NEJMoa030207 [DOI] [PubMed] [Google Scholar]
- 20.Armanini D, Sabbadin C, Donà G, Bordin L, Clari G. Aldosterone receptor blockers spironolactone and canrenone: two multivalent drugs. Expert Opin Pharmacother. (2014) 15:909–12. 10.1517/14656566.2014.896901 [DOI] [PubMed] [Google Scholar]
- 21.Ma J, Albornoz F, Yu C, Byrne DW, Vaughan DE, Brown NJ. Differing effects of mineralocorticoid receptor-dependent and -independent potassium-sparing diuretics on fibrinolytic balance. Hypertension. (2005) 46:313–20. 10.1161/01.HYP.0000174327.53863.86 [DOI] [PubMed] [Google Scholar]
- 22.Armanini D, Bordin L, Clari G. Serum potassium, thiazides, aldosterone, and mineralocorticoid receptors. Hypertension. (2012) 60:e9. 10.1161/HYPERTENSIONAHA.112.197889 [DOI] [PubMed] [Google Scholar]
- 23.Singh H, Bala S, Jain D, Jagota R, Mathur R. Spironolactone (an adjuvant therapy) in rheumatoid arthritis: a case control study. Reumatologia. (2018) 56:87–91. 10.5114/reum.2018.75519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang SK, Sun P, Tandias RM, Seto BK, Arroyo JG. Mineralocorticoid receptor antagonists in central serous chorioretinopathy: a meta-analysis of randomized controlled trials. Ophthalmol Retina. (2019) 3:154–60. 10.1016/j.oret.2018.09.003 [DOI] [PubMed] [Google Scholar]
- 25.Armanini D, Strasser T, Weber PC. Characterization of aldosterone binding sites in circulating human mononuclear leukocytes. Am J Physiol. (1985) 248(3 Pt1):E388–90. 10.1152/ajpendo.1985.248.3.E388 [DOI] [PubMed] [Google Scholar]
- 26.Wehling M, Armanini D, Strasser T, Weber PC. Effect of aldosterone on sodium and potassium concentrations in human mononuclear leukocytes. Am J Physiol. (1987) 252(4 Pt 1):E505–8. 10.1152/ajpendo.1987.252.4.E505 [DOI] [PubMed] [Google Scholar]
- 27.Wehling M, Kuhls S, Armanini D. Volume regulation of human lymphocytes by aldosterone in isotonic media. Am J Physiol. (1989) 257(2 Pt 1):E170–4. 10.1152/ajpendo.1989.257.2.E170 [DOI] [PubMed] [Google Scholar]
- 28.Wehling M. Specific, nongenomic actions of steroid hormones. Annu Rev Physiol. (1997) 59:365–93. 10.1146/annurev.physiol.59.1.365 [DOI] [PubMed] [Google Scholar]
- 29.Calò LA, Zaghetto F, Pagnin E, Davis PA, De Mozzi P, Sartorato P, et al. Effect of aldosterone and glycyrrhetinic acid on the protein expression of PAI-1 and p22(phox) in human mononuclear leukocytes. J Clin Endocrinol Metab. (2004) 89:1973–6. 10.1210/jc.2003-031545 [DOI] [PubMed] [Google Scholar]
- 30.Bordin L, Donà G, Sabbadin C, Ragazzi E, Andrisani A, Ambrosini G, et al. Human red blood cells alterations in primary aldosteronism. J Clin Endocrinol Metab. (2013) 98:249–501. 10.1210/jc.2012-3571 [DOI] [PubMed] [Google Scholar]
- 31.Fiore C, Bordin L, Pellati D, Armanini D, Clari G. Effect of glycyrrhetinic acid on membrane band 3 in human erythrocytes. Arch Biochem Biophys. (2008) 479:46–51. 10.1016/j.abb.2008.08.011 [DOI] [PubMed] [Google Scholar]
- 32.Bordin L, Saccardi C, Donà G, Sabbadin C, Andrisani A, Ambrosini G, et al. Mineralocorticoid receptor is involved in the aldosterone pathway in human red blood cells. Am J Transl Res. (2016) 8:314–28. [PMC free article] [PubMed] [Google Scholar]
- 33.Fogelman Y, Gaitini D, Carmeli E. Antiatherosclerotic effects of licorice extract supplementation on hypercholesterolemic patients: decreased CIMT, reduced plasma lipid levels, and decreased blood pressure. Food Nutr Res. (2016) 60:30830. 10.3402/fnr.v60.30830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boonmuen N, Gong P, Ali Z, Chittiboyina AG, Khan I, Doerge DR, et al. Licorice root components in dietary supplements are selective estrogen receptor modulators with a spectrum of estrogenic and anti-estrogenic activities. Steroids. (2016) 105:42–9. 10.1016/j.steroids.2015.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fiore C, Eisenhut M, Krausse R, Ragazzi E, Pellati D, Armanini D, et al. Antiviral effects of Glycyrrhiza species. Phytother Res. (2008) 22:141–8. 10.1002/ptr.2295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baschetti R. Chronic fatigue syndrome and liquorice. N Z Med J. (1995) 108:156–7. [PubMed] [Google Scholar]
- 37.Borst JG, Ten Holt SP, De Vries LA, Molhuysen JA. Synergistic action of liquorice and cortisone in Addison's and Simmonds's disease. Lancet. (1953) 1:657–63. 10.1016/S0140-6736(53)91800-5 [DOI] [PubMed] [Google Scholar]
- 38.Basso A, Dalla Paola L, Erle G, Boscaro M, Armanini D. Licorice ameliorates postural hypotension caused by diabetic autonomic neuropathy. Diabetes Care. (1994) 17:1356. 10.2337/diacare.17.11.1356 [DOI] [PubMed] [Google Scholar]
- 39.Armanini D, Bonanni G, Palermo M. Reduction of serum testosterone in men by licorice. N Engl J Med. (1999) 341:1158 10.1056/NEJM199910073411515 [DOI] [PubMed] [Google Scholar]
- 40.Armanini D, Mattarello MJ, Fiore C, Bonanni G, Scaroni C, Sartorato P, Palermo M. Licorice reduces serum testosterone in healthy women. Steroids. (2004) 69:763–6. 10.1016/j.steroids.2004.09.005 [DOI] [PubMed] [Google Scholar]
- 41.Armanini D, Andrisani A, Bordin L, Sabbadin C. Spironolactone in the treatment of polycystic ovary syndrome. Expert Opin Pharmacother. (2016) 17:1713–5. 10.1080/14656566.2016.1215430 [DOI] [PubMed] [Google Scholar]
- 42.Armanini D, Castello R, Scaroni C, Bonanni G, Faccini G, Pellati D, et al. Treatment of polycystic ovary syndrome with spironolactone and licorice. Eur J Obstet Gynecol Reprod. (2007) 131:61–7. 10.1016/j.ejogrb.2006.10.013 [DOI] [PubMed] [Google Scholar]
- 43.Sabbadin C, Andrisani A, Zermiani M, Donà G, Bordin L, Ragazzi E, et al. Spironolactone and intermenstrual bleeding in polycystic ovary syndrome with normal BMI. J Endocrinol Invest. (2016) 39:1015–21. 10.1007/s40618-016-0466-0 [DOI] [PubMed] [Google Scholar]
- 44.Sakamoto K, Wakabayashi K. Inhibitory effect of glycyrrhetinic acid on testosterone production in rat gonads. Endocrinol Jpn. (1988) 35:333–42. 10.1507/endocrj1954.35.333 [DOI] [PubMed] [Google Scholar]
- 45.Klasik-Ciszewska S, Kaczmarczyk-Sedlak I, Wojnar W. Effect of glabridin and glycyrrhizic acid on histomorphometric parameters of bones in ovariectomized rats. Acta Pol Pharm. (2016) 73:517–27. [PubMed] [Google Scholar]
- 46.Arentz S, Smith CA, Abbott J, Fahey P, Cheema BS, Bensoussan A. Combined lifestyle and herbal medicine in overweight women with Polycystic Ovary Syndrome (PCOS): a randomized controlled trial. Phytother Res. (2017) 31:1330–40. 10.1002/ptr.5858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Donà G, Sabbadin C, Fiore C, Bragadin M, Giorgino FL, Ragazzi E, et al. Inositol administration reduced oxidative stress in erythrocytes of patients with polycystic ovary syndrome. Eur J Endocrinol. (2012) 166:703–10. 10.1530/EJE-11-0840 [DOI] [PubMed] [Google Scholar]
- 48.Armanini D, Bordin L, Donà G, Sabbadin C, Bakdounes L, Ragazzi E, et al. Polycystic ovary syndrome: implications of measurement of plasma aldosterone, renin activity and progesterone. Steroids. (2012) 77:655–8. 10.1016/j.steroids.2012.02.010 [DOI] [PubMed] [Google Scholar]
- 49.Sil R, Ray D, Chakraborti AS. Glycyrrhizin ameliorates insulin resistance, hyperglycemia, dyslipidemia and oxidative stress in fructose-induced metabolic syndrome-X in rat model. Indian J Exp Biol. (2013) 51:129–38. [PubMed] [Google Scholar]
- 50.Armanini D, Nacamulli D, Francini-Pesenti F, Battagin G, Ragazzi E, Fiore C. Glycyrrhetinic acid, the active principle of licorice, can reduce the thickness of subcutaneous thigh fat through topical application. Steroids. (2005) 70:538–42. 10.1016/j.steroids.2005.01.007 [DOI] [PubMed] [Google Scholar]