Abstract
Copper/zinc superoxide dismutase 1 (SOD1) scavenges free radicals that may otherwise damage brain parenchyma. Impaired SOD1 activity drives Alzheimer's disease (AD) neuropathology in animal models and postmortem AD brains. Yet, it is unknown how cerebrospinal fluid (CSF) SOD1 is related in vivo to AD-relevant cognitive, neuroimaging, and CSF neurotoxic factors, and what potential mechanisms underlie these associations. We found that higher CSF SOD1 correlated with better global cognition scores, yet less gray matter (GM) and glucose metabolism in AD-sensitive parietal and frontal regions. Higher CSF SOD1 was also associated with more CSF total tau and phosphorylated tau-181, but not beta-amyloid 1–42. Through mediation analyses, higher total tau largely mitigated higher CSF SOD1 and better global cognition associations, and it fully accounted for less predicted regional GM but not glucose metabolism. Among participants who developed AD over 2 years or had AD at baseline, higher CSF SOD1 was initially related to more regional GM. This association became nonsignificant with full mediation via higher CSF total tau, through which higher CSF SOD1 predicted more total tau and in turn less GM. Our observations lead to the hypothesis that SOD1 antioxidation reflects tau but not amyloid accumulation, which may lead to pro-oxidant-based neurodegeneration and cognitive dysfunction. Antioxid. Redox Signal. 31, 572–578.
Keywords: neurodegeneration, nutrition, biomarkers, free radicals
Introduction
Oxidative stress is thought to play a major role in the pathophysiology of Alzheimer's disease (AD). Particularly, brain proteins and lipids are susceptible to oxidative damage. It is unclear if the oxidative damage seen in AD is a result of the disease process or causes neurological decline. Superoxide dismutase (SOD) is a ubiquitous enzyme that protects against reactive oxygen species (ROS) formed during aerobic respiration (9). Specifically, SOD is an antioxidant enzyme that catalyzes the oxidation/reduction reaction of the superoxide anion into oxygen and hydrogen peroxide. SOD consists of three isoenzymes: copper/zinc SOD, or SOD1, localized predominantly to the cytosol; manganese SOD, or SOD2, within mitochondria; and extracellular SOD, or SOD3. Changes in SOD levels can cause excess ROS in cells, leading to altered intracellular and mitochondrial metabolism, as well as DNA and vascular damage.
SOD1 has been examined in AD for its role in preserving neural integrity and memory performance. Increased SOD1 levels are seen in the pyramidal neurons of AD patients compared with controls (3). For hippocampal cells of AD patients and related transgenic models, SOD1 overexpression downregulates beta-amyloid (Aβ)-induced oxidative stress, using a nonoxidized versus oxidized glutathione ratio as a marker (2). Furthermore, coexpression of SOD1 in amyloid precursor protein transgenic mice blocks endothelial dysfunction that gives rise to hypoperfusion often seen in AD (5). SOD1-deficient Tg2576 mice, meanwhile, show increased Aβ plaque formation, neuroinflammation, tau phosphorylation, and memory decline (6).
Innovation
Despite superoxide dismutase 1's (SOD1) protective role for memory and neuropathology seen in postmortem Alzheimer's disease (AD) brains and AD transgenic models, it is unknown how SOD1 is related in vivo to cognition, brain, and cerebrospinal fluid (CSF) toxic marker outcomes across the AD spectrum. Via mediation, we found that higher CSF total tau and to a lesser extent phosphorylated tau, but not CSF beta-amyloid 1–42, largely mitigated “beneficial” global cognition associations. Total tau fully mediated SOD1 predicted atrophy in AD-sensitive regions. We hypothesize that CSF SOD1 is an in vivo biomarker of tau but not amyloid-related neurodegeneration in AD, where tau's causal role remains unclear.
In this study, cerebrospinal fluid (CSF) SOD1 data collected by the Alzheimer's Disease Neuroimaging Initiative (ADNI) in 287 aged adults were examined with respect to CSF Aβ1–42 and tau pathology markers, brain atrophy and glucose uptake, and cognitive performance.
Results
Data summary
Clinical and demographic data on 287 ADNI participants are presented in Table 1. There were no differences based on years of education, age, or CSF SOD levels at baseline between cognitively unimpaired (CU), mild cognitive impairment (MCI), or AD subjects. As expected for this ADNI subpopulation, the percentage of apolipoprotein E (APOE)4 carriers increased stepwise from CU to AD. There were also significantly fewer women in the MCI and AD relative to CU groups.
Table 1.
Demographic Data for Alzheimer's Disease Neuroimaging Initiative Subjects with Cerebrospinal Fluid Superoxide Dismutase 1
| CU (n = 86) | MCI (n = 135) | AD (n = 66) | |
|---|---|---|---|
| Age (years) | 75.70 ± 5.54 | 74.67 ± 7.32 | 75.04 ± 7.62 |
| Education (years) | 15.64 ± 2.97 | 16.02 ± 2.97 | 15.06 ± 2.93 |
| Sex (% female)* | 48.8% | 32.6% | 43.9% |
| BMI (kg/m2) | 26.54 ± 3.84 | 25.98 ± 3.77 | 26.36 ± 4.28 |
| APOE4 carriage (%)*** | 24.4% | 52.6% | 71.2% |
| CSF SOD (AU) | 21.46 ± 0.34 | 21.49 ± 0.37 | 21.42 ± 0.39 |
| CDR-sob (score)*** | 0.02 ± 0.11 | 1.54 ± 0.86 | 4.37 ± 1.54 |
| ADAS-cog11 (score)*** | 6.05 ± 2.90 | 11.73 ± 4.33 | 18.86 ± 6.73 |
| EF factor (z-score)*** | 0.66 ± 0.62 | −0.08 ± 0.73 | −1.02 ± 0.81 |
| Memory factor (z-score)*** | 0.98 ± 0.50 | −0.15 ± 0.57 | −0.90 ± 0.56 |
| MMSE (score)*** | 29.05 ± 1.02 | 26.92 ± 1.74 | 23.50 ± 1.83 |
Values are mean ± standard deviation unless otherwise stated.
Chi-square p < 0.05, <0.001.
AD, Alzheimer's disease; ADAS-cog, Alzheimer's Disease Assessment Scale-cognitive subscale; APOE, apolipoprotein E; AU, arbitrary units; BMI, body mass index; CDR-sob, Clinical Dementia Rating Scale Sum of Boxes; CSF, cerebrospinal fluid; CU, cognitively unimpaired; EF, executive function; MCI, mild cognitive impairment; MMSE, Mini-Mental State Examination; SOD, superoxide dismutase.
Global cognition and memory
Broadly, we observed that higher CSF SOD1 was related to “better” scores for global cognition but not subdomain tests. Specifically, for Clinical Dementia Rating Scale Sum of Boxes (CDR-sob), higher CSF SOD1 was significantly associated with better scores (β ± standard error [SE] = −0.625 ± 0.285, p < 0.05). Similarly, SOD1 was related to better Alzheimer's Disease Assessment Scale-cognitive subscale (ADAS-cog)11 (β ± SE = −2.768 ± 1.033, p < 0.01) and Mini-Mental State Examination (MMSE) scores (β ± SE = 0.973 ± 0.397, p < 0.05). SOD1 main effects, or interactions with APOE4 status or baseline clinical diagnosis, were nonsignificant for memory and executive function factors, as well as for Rey Auditory Verbal Learning Test (RAVLT) indices.
AD CSF biomarkers
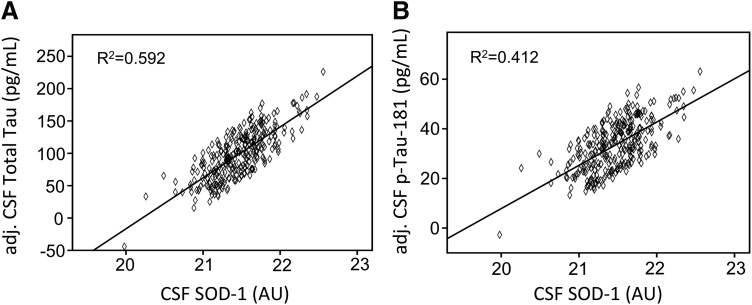
CSF SOD1 was significantly related to higher levels of total tau (β ± SE = 81.666 ± 5.986, p < 0.001) and p-tau-181 (β ± SE = 18.440 ± 2.253, p < 0.001) (Fig. 1). No significant differences were seen with respect to SOD1 and CSF Aβ1–42.
FIG. 1.
Correction between CSF SOD and AU biomarkers. The association between higher CSF SOD1 and higher covariate-adjusted CSF total tau (A) and p-tau-181 (B) values. AU, arbitrary units; CSF, cerebrospinal fluid; SOD1, superoxide dismutase 1.
Regional fluorodeoxyglucose metabolism
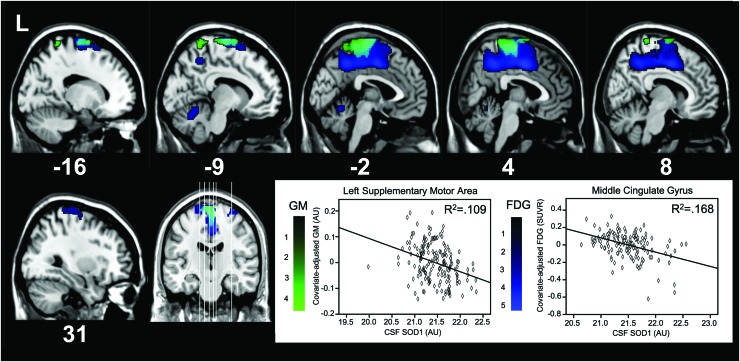
Next, voxel-wise analysis was used to regress CSF SOD1 levels against regional fluorodeoxyglucose (FDG) uptake, an index of glucose metabolism, at baseline. Higher CSF SOD1 was significantly associated with less FDG (p < 0.05, family-wise error [FWE] corrected) in a large cluster with the maximum in left supplementary motor area (Fig. 2, “blue” cluster; Table 2). This cluster bilaterally spanned superior medial frontal gyrus, mid- and posterior cingulate gyri, pre- and postcentral gyri, precuneus, lobulo-limbic transitional gyrus, as well as left angular gyrus. Smaller clusters encompassed anterior cerebellum or pre- and postcentral gyri.
FIG. 2.
Brain areas showing less FDG metabolism (“blue”) and GM (“green”) as a function of more CSF SOD1. Numbers below each brain slice represent the sagittal MNI coordinates of the slice. Overlapping areas showing both less FDG metabolism and GM are teal. The GM graph depicts the relationship at the maximal voxel in the left supplementary motor area (−9, −10.5, 78) and the FDG graph depicts the relationship at the maximal voxel in middle cingulate gyrus (4, −2, 44). FDG, fluorodeoxyglucose; GM, gray matter. Color images are available online.
Table 2.
Negative Main Effects of Superoxide Dismutase on Fluorodeoxyglucose Metabolism
| Location | t value | X, Y, Z | Cluster size (voxels) |
|---|---|---|---|
| Midcingulate gyrus (R) | 5.31 | 4, −2, 44 | 5214 |
| Precuneus (R) | 4.72 | 2, −48, 44 | |
| Midcingulate gyrus (R) | 4.25 | 4, −20, 48 | |
| Cerebellum | 3.28 | −6, −58, −14 | 263 |
| Cerebellum | 3.18 | −8, −64, −22 | |
| Precentral gyrus (R) | 3.00 | 34, −16, 68 | 282 |
| Postcentral gyrus (R) | 2.83 | 38, −36, 70 |
This table depicts regions where all subjects had less predicted FDG metabolism as a function of more CSF SOD1. The highest t value for a given cluster of significant contiguous voxels is shown. For clusters that extended over >15 mm, the highest submaxima t values in those areas are indicated. Coordinates are in MNI atlas space. Brains are oriented in neurological space.
MNI, Montreal Neurological Institute; R, right hemisphere.
Regional gray matter volume
Voxel-wise analysis was also used to examine how CSF SOD1 concentrations were associated with regional gray matter (GM) at baseline. Higher CSF SOD1 was related to less GM (p < 0.05, FWE corrected) in a large cluster (Fig. 2, “green” cluster; Table 3), with the maximally significant voxel in left supplementary motor area. This cluster bilaterally encompassed precuneus and pre- and postcentral gyri, as well as left lobulo-limbic transitional gyrus/paracentral lobule, superior parietal gyrus, and superior frontal gyrus (Fig. 2; Table 3).
Table 3.
Negative Main Effects of Superoxide Dismutase on Regional Gray Matter Volume
| Location | t value | X, Y, Z | Cluster size (voxels) |
|---|---|---|---|
| Supplementary motor area (L) | 4.57 | −9, −10, 78 | 3855 |
| Precuneus (L) | 4.33 | −10, −50, 72 | |
| Paracentral lobule (R) | 4.23 | 2, −28, 69 |
This table depicts regions where all subjects had less predicted gray matter as a function of more CSF SOD1. The highest t value for a given cluster of significant, contiguous voxels is shown. For clusters that extended over >15 mm, the highest submaxima t values in those areas are indicated. Coordinates are in MNI atlas space. Brains are oriented in neurological space.
L, left hemisphere.
Preacher–Hayes mediation of SOD1 for memory, GM, and FDG-positron emission tomography outcomes
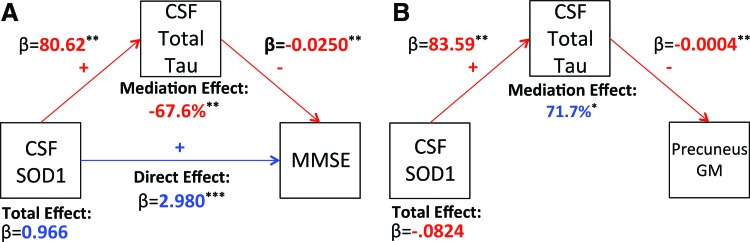
Finally, Preacher–Hayes mediation analyses were used to separately determine if CSF total tau, p-tau-181, or Aβ1–42 acted as a mediator for the associations between SOD1 and global cognition, GM, and FDG outcomes. In summary, CSF total tau or to a lesser extent p-tau-181, but not CSF Aβ1–42, partially or fully mediated SOD1 associations.
For the higher SOD1 and better MMSE score association (direct effect β ± SE = 2.980 ± 0.441, p < 0.001), higher total tau acted as a partial mediator, decreasing the statistical effect of SOD1 on MMSE by 67.6% (indirect effect β ± SE = −2.014 ± 0.358, p < 0.01) (Fig. 3A). In a separate model, p-tau-181 also showed a significant although weaker partial mediation of the SOD1 and MMSE association, decreasing the statistical effect by 51.5% (direct effect β ± SE = 2.002 ± 0.407, p < 0.001; indirect effect β ± SE = −1.028 ± 0.237, p < 0.01). Similar associations were seen for CDR-sob and ADAS-cog11.
FIG. 3.
Mediation on effects of SOD1 on MMSE and Precuneus GM by tau. Preacher–Hayes mediation of CSF SOD1, total tau, and MMSE scores at baseline (A). Preacher–Hayes mediation of CSF SOD1, CSF total tau, and regional GM volume in left precuneus in a submaximum voxel (−10.5, −49.5, 72) (B). **p < 0.01, ***p < 0.001. MMSE, Mini-Mental State Examination. Color images are available online.
For the higher CSF SOD1 and less regional GM association, we focused on precuneus because hypometabolism and atrophy there are imaging markers of progression from preclinical AD to AD. As shown in Figure 1, SOD1 originally predicted less precuneus GM to a moderate degree (β ± SE = −0.064 ± 0.0142, p < 0.001). CSF total tau fully mediated this relationship (indirect effect: β ± SE = −0.035 ± 0.015, p < 0.05) (Fig. 3B), where the SOD1-GM direct effect was nonsignificant (β ± SE = −0.047 ± 0.024, p > 0.05). In a separate model, p-tau-181 partially mediated SOD1 and precuneus GM associations, increasing the degree of association by 35% (direct effect: β ± SE = −0.049 ± 0.016, p < 0.05; indirect effect: β ± SE = −0.017 ± 0.008, p < 0.05). Total tau and p-tau-181 did not mediate associations between higher CSF SOD1 and less baseline regional FDG uptake.
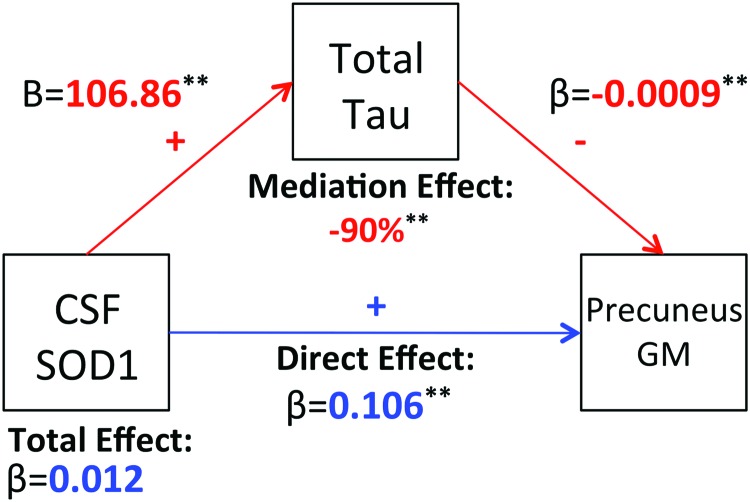
To explore if AD onset and progression drove these GM mediation results, we reran models only with MCI participants who converted to AD within 24 months and participants classified as AD at baseline. As shown in Figure 4, higher CSF SOD1 was related to more regional GM in the precuneus (direct effect: β ± SE = 0.106 ± 0.034, p < 0.01). Higher total tau levels fully mediated this association via suppression, decreasing the statistical effect on GM by 90% (indirect effect: β ± SE = −0.094 ± 0.027, p < 0.01) and rendering the total effect association between CSF SOD1 and more regional GM nonsignificant. Recall that for voxel-wise analyses including all participants (Fig. 3B), higher SOD1 predicted less GM that was also fully mediated by higher CSF total tau.
FIG. 4.
Mediation on effects of SOD1 on Precuneus GM by tau in AD and MCI participants who convert to AD. Preacher–Hayes mediation of CSF SOD1, total tau, and regional GM volume in left precuneus in a submaximum voxel (−10.5, −49.5, 72) among participants with MCI who converted to AD within 24 months and AD participants diagnosed at baseline. AD, Alzheimer's disease; MCI, mild cognitive impairment. Color images are available online.
Discussion
Progressive pro-oxidant damage has been associated with AD hallmarks such as tau and amyloid neuropathology, memory decline, and less neural integrity in AD-sensitive regions. In this study, we observed across the AD spectrum that more CSF SOD1 was related to more CSF tau species but not Aβ1–42. CSF total tau via mediation suppressed “beneficial” SOD1 associations with cognition and fully accounted for less predicted GM, but not glucose uptake, in AD-sensitive parietal and frontal regions. Even so, this leads to the further question of whether total tau induces pro-oxidation or reflects a specific pro-oxidative process separate from Aβ1–42.
In AD rodent models, higher SOD1 expression generally appears to induce protection in brain (1, 5, 6) and preserve cognition (4). We observed that higher CSF SOD1 corresponded to better global cognitive function based on CDR-sob, ADAS-cog11, and MMSE in all participants. This is consistent with a study among aged mice that overexpressed extracellular SOD (i.e., SOD1), which showed improved motor learning and decreased age-related decline in spatial memory compared with controls (4). The authors also illustrated an improvement in long-term potentiation, a molecular process underlying learning and memory, in the mice overexpressing extracellular SOD. While our observations are correlational and mediation with these data cannot be used to make causal interpretations, it was nonetheless interesting that higher total tau, but not CSF Aβ1–42, reflected drastic mitigation but not erasure of CSF SOD1 associations with global cognition.
Here, regardless of clinical diagnosis, higher SOD1 levels across all participants were strongly correlated with more CSF total tau and p-tau-181 levels, but not Aβ1–42. This led to our hypothesis that progressive neurodegeneration reflecting more tau deposition might induce more SOD1 to minimize free radical damage. These findings parallel those of Winer et al. (8), who showed a significant positive correlation between CSF SOD1 levels and both tau and phosphorylated tau in aged adults with AD. They also observed weak CSF SOD1 associations with CSF Aβ1–42 across all diagnostic groups and no associations among any of the subgroups (8), which is in line with our observing no such relationships in this study. We hypothesize that SOD1 activity may reduce tau-related neurodegeneration in areas affected later in the disease, where other antioxidant factors may regulate pro-oxidant damage reflecting amyloidosis. Alternatively, since tau is indicative of neuronal injury, and oxidative stress can cause cell death, tau and SOD1 may track neurodegeneration during AD onset and progression better than Aβ1–42.
Indeed, for regional GM and FDG metabolism, CSF SOD1 was related to less GM and glucose metabolism in the precuneus, posterior cingulate gyrus, paracentral lobule, and frontal gyri. Our mediation analyses suggest that tau accumulation reflecting progressive pro-oxidant damage may affect atrophy in these areas, in part distinguishing AD onset and progression. Indeed, CSF SOD1 no longer significantly predicted more GM in participants with AD onset or AD at baseline after total tau mediation. It is our hypothesis that SOD production may thus be futile in controlling free radical levels once a participant is on a trajectory for AD onset and progression. This phenomenon may extend beyond neural parenchyma. For example, erythrocyte SOD activity was significantly higher in a group of 27 AD participants compared with controls; the SOD levels in the AD and control participants were also positively correlated with serum malondialdehyde levels, which is a marker of oxidative stress, suggesting that the body is producing SOD in an attempt to reduce oxidative stress levels (8).
We should note several limitations with this study. First, all analyses were correlational, and while mediation analyses suggested more total tau largely drove SOD1 associations, it remains unclear if tau accumulation induces redox imbalance or serves an antioxidant function to reduce pro-oxidative damage. Therefore, experimental paradigms are needed to test if AD human tau neurons transplanted in AD or control rodent parietal and frontal regions induce pro- or antioxidation, and how CSF SOD1 application affects neurite integrity with or without tau present. Dietary recall was also not collected in ADNI participants, which would have been helpful to assess the link between diets that induce oxidative stress and SOD1 expression in the brain. Participant CSF samples were only assayed at baseline, so we were unable to longitudinally examine CSF SOD1 and variation over time in AD outcomes. Finally, plasma SOD1 that was assayed in ADNI1 did not pass quality control measures, which did not allow us to see if similar associations occurred in the periphery.
In summary, we observed that CSF SOD1 has strong associations with total tau and p-tau-181 in CSF, global cognition, and regional GM and glucose metabolism, all of which have been linked with AD etiopathogenesis. We observed that CSF SOD1 is associated with better global cognition, yet less GM and glucose uptake in parietal and frontal areas that are sensitive to AD-related changes. We noted that higher total tau appears to partially or fully mediate these associations, nearly mitigating the statistical effect of more SOD1 on better MMSE scores and less regional GM volume. Because of these novel findings, we hypothesize that CSF SOD1 may simultaneously be related to the degree of AD-related neurodegeneration seen in the brain specific to tau accumulation, and also reflect the degree of free radical scavenging as a compensatory mechanism. Future work should examine if CSF SOD1 levels are related to regional tau deposition and track progressive accumulation across **p < 0.01. the AD spectrum; in addition, forthcoming research should determine the utility of peripheral SOD1 as a biomarker for AD outcomes.
Notes
Participants
Data from middle-aged to aged adults were obtained from the ADNI database. The ADNI was launched in 2003 as a public–private partnership, led by Principal Investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of MCI and early AD. For up-to-date information see Alzheimer's Disease Neuroimaging Initiative website. Written informed consent was obtained from all ADNI participants at their respective ADNI sites. The ADNI protocol was approved by site-specific institutional review boards. Baseline CSF data for SOD1 were available for 287 subjects: 86 CU individuals, 135 MCI individuals, and 66 individuals with AD.
Participants with MCI met the following diagnostic criteria: (1) memory complaint identified by the participant or their study partner; (2) abnormal memory as assessed by the Logical Memory II subscale from the Wechsler Memory Scale-Revised; (3) MMSE score between 24 and 30; (4) CDR of 0.5; and (5) deficits not severe enough for the participant to be diagnosed with AD by the site physician at screening. Participants with AD met similar criteria, however, were required to have an MMSE score between 20 and 26, a CDR of 0.5 or 1.0, and National Institute of Neurological and Communicative Disorders and Stroke/Alzheimer's Disease and Related Disorders Association criteria for probable AD.
Mass spectrometry and SOD1
Data were downloaded from the Biomarkers Consortium CSF Proteomics multiple reaction monitoring (MRM) data set. The ADNI Biomarkers Consortium Project investigated the extent to which selected peptides, measured with mass spectrometry (MS), could discriminate among disease states. Briefly, MRM-MS was used for targeted quantitation of 567 peptides representing 221 proteins in a single run (Caprion Proteome, Inc., Montreal, Canada). Analyses for this report focused on cytosolic SOD1 levels, which were assayed in the CSF multiplex panel as reflected by the peptide GDGPVQGIINFEQK.
APOE genotype
The ADNI Biomarker Core at the University of Pennsylvania conducted APOE ɛ4 genotyping. We characterized participants as having zero APOE ɛ4 alleles, one APOE4 allele, or two APOE ɛ4 alleles. Analyses did not differ when discriminating APOE4 carriage versus noncarriage.
Amyloid and tau CSF biomarkers
CSF sample collection, processing, and quality control of p-tau-181, total tau, and Aβ1–42 are described in the ADNI1 protocol manual. Briefly, CSF samples were analyzed using INNO-BIA Alz Bio3 immunoassay reagents with the Luminex platform. Statistical modeling was completed to confirm reliability of results across seven laboratories before implementation with ADNI.
Neuropsychological assessment
ADNI utilizes an extensive battery of assessments to examine cognitive functioning with particular emphasis on domains relevant to AD. A full description is available at (www.adni-info.org/Scientists/CognitiveTesting.aspx). All subjects underwent clinical and neuropsychological assessment at the time of scan acquisition. Neuropsychological assessments included the following: the CDR-sob, MMSE, RAVLT, and ADAS-cog. A composite memory score encompassing the RAVLT, ADAS-cog, MMSE, and Logical Memory assessments was also utilized. This composite memory score was used in formal analyses to represent global memory among subjects.
MRI acquisition and preprocessing
T1-weighted MRI scans were acquired within 10–14 days of the screening visit following a back-to-back three-dimensional magnetization-prepared rapid gradient echo scanning protocol described in the ADNI MRI Technical Procedures Manual. The SPM12 “New Segmentation” tool was used to extract modulated GM volume maps. Maps were smoothed with an 8 mm Gaussian kernel and then used for all voxel-wise analyses.
Fluorodeoxyglucose-PET
Briefly, 185 MBq of [18-153-F]-FDG was injected intravenously. After 30 min, six 5-min frames were acquired. Frames of each baseline image series were coregistered to the first frame and combined into dynamic image sets. Each set was averaged, reoriented to a standard 160 × 160 × 96 voxel spatial matrix of resliced 1.5 mm3 voxels, normalized for intensity, and smoothed with an 8 mm full width at half maximum kernel. To derive the standardized uptake value ratio, pixel intensity was normalized according to the pons since it demonstrates preserved glucose metabolism in AD. Normalization to the pons removed interindividual tracer metabolism variability. The Montreal Neurological Institute template space was used to spatially normalize images using SPM12.
Statistical analysis
All analyses were conducted using SPSS 25 (IBM Corp., Armonk, NY) or SPM12. For non-MRI or FDG analyses, linear mixed regression models tested the main effects of CSF SOD1 on outcomes, including neuropsychological performance and AD CSF biomarkers, including Aβ1–42, total tau, and p-tau-181. Main effects and interactions with APOE4 allele load were separately tested in a single model. Covariates included age at baseline, body mass index (BMI), sex, and baseline clinical diagnosis. Participant's years of education were also included as a covariate for models with cognitive tests as an outcome of interest. Baseline diagnosis was not used as a covariate for models with cognitive tests as an outcome of interest to avoid multicollinearity. Preacher–Hayes mediation analyses were conducted in SPSS 25 using PROCESS v3.3. Nonsignificant covariates were removed from final models for model parsimony.
For voxel-wise analysis, second-level mixed models tested the main effects of SOD1 on regional GM volume and FDG, controlling for age, sex, BMI, APOE4 status, and baseline clinical diagnosis. Voxel and cluster statistical thresholds were set at p < 0.005 (uncorrected) and p < 0.05 (FWE corrected), respectively. Results were considered significant at the cluster level. As described previously (7), to further reduce type 1 error, we utilized a GM threshold of 0.2 to ensure that voxels with <20% likelihood of being GM were not analyzed. For GM, Monte Carlo simulations in ClusterSim were used to estimate that 462 contiguous voxels were needed for such a cluster to occur at FWE p < 0.05. For FDG voxel-wise analyses, Monte Carlo simulations were used to estimate that 224 contiguous voxels were needed for such a cluster to occur at FWE p < 0.05.
Acknowledgments
This study was funded by the Iowa State University, NIH R00 AG047282, and AARGD-17-529552. Neither funding source had any involvement in the report. Data used in preparation of this article were obtained from the Alzheimer's Disease Neuroimaging Initiative (ADNI) database (http://adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data, but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at (http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf). Data collection and sharing for this project were funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI; National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer's Association; Alzheimer's Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai, Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research and Development, LLC.; Johnson and Johnson Pharmaceutical Research and Development LLC.; Lumosity; Lundbeck; Merck and Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health. The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer's Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Abbreviations Used
- Aβ
beta-amyloid
- AD
Alzheimer's disease
- ADAS-cog
Alzheimer's Disease Assessment Scale-cognitive subscale
- ADNI
Alzheimer's Disease Neuroimaging Initiative
- APOE
apolipoprotein E
- BMI
body mass index
- CDR-sob
Clinical Dementia Rating Scale Sum of Boxes
- CSF
cerebrospinal fluid
- CU
cognitively unimpaired
- EF
executive function
- FDG
fluorodeoxyglucose
- FWE
family-wise error
- GM
gray matter
- MCI
mild cognitive impairment
- MMSE
Mini-Mental State Examination
- MNI
Montreal Neurological Institute
- MRI
magnetic resonance imaging
- MRM
multiple reaction monitoring
- MS
mass spectrometry
- PET
positron emission tomography
- RAVLT
Rey Auditory Verbal Learning Test
- ROS
reactive oxygen species
- SE
standard error
- SOD1
superoxide dismutase 1
Contributor Information
Collaborators: for the Alzheimer's Disease Neuroimaging Initiative
References
- 1. Borg J. and Chereul E. Differential MRI patterns of brain atrophy in double or single transgenic mice for APP and/or SOD. J Neurosci Res 86: 3275–3284, 2008 [DOI] [PubMed] [Google Scholar]
- 2. Celsi F, Svedberg M, Unger C, Cotman CW, Carrì MT, Ottersen OP, Nordberg A, and Torp R. Beta-amyloid causes downregulation of calcineurin in neurons through induction of oxidative stress. Neurobiol Dis 26: 342–352, 2007 [DOI] [PubMed] [Google Scholar]
- 3. Delacourte A, Defossez A, Ceballos I, Nicole A, and Sinet PM. Preferential localization of copper zinc superoxide dismutase in the vulnerable cortical neurons in Alzheimer's disease. Neurosci Lett 92: 247–253, 1988 [DOI] [PubMed] [Google Scholar]
- 4. Hu D, Serrano F, Oury TD, and Klann E. Aging-dependent alterations in synaptic plasticity and memory in mice that overexpress extracellular superoxide dismutase. J Neurosci 26: 3933–3941, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Iadecola C, Zhang F, Niwa K, Eckman C, Turner SK, Fischer E, Younkin S, Borchelt DR, Hsiao KK, and Carlson GA. SOD1 rescues cerebral endothelial dysfunction in mice overexpressing amyloid precursor protein. Nat Neurosci 2: 157–161, 1999 [DOI] [PubMed] [Google Scholar]
- 6. Murakami K, Murata N, Noda Y, Tahara S, Kaneko T, Kinoshita N, Hatsuta H, Murayama S, Barnham KJ, Irie K, Shirasawa T, and Shimizu T. SOD1 (copper/zinc superoxide dismutase) deficiency drives amyloid beta protein oligomerization and memory loss in mouse model of Alzheimer disease. J Biol Chem 286: 44557–44568, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Willette AA, Bendlin BB, Starks EJ, Birdsill AC, Johnson SC, Christian BT, Okonkwo OC, La Rue A, Hermann BP, Koscik RL, Jonaitis EM, Sager MA, and Asthana S. Association of insulin resistance with cerebral glucose uptake in late middle-aged adults at risk for Alzheimer disease. JAMA Neurol 72: 1013–1020, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Winer L, Srinivasan D, Chun S, et al. SOD1 in cerebral spinal fluid as a pharmacodynamic marker for antisense oligonucleotide therapy. JAMA Neurol 70: 201–207, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zuo L, Zhou T, Pannell BK, Ziegler AC, and Best TM. Biological and physiological role of reactive oxygen species—the good, the bad and the ugly. Acta Physiol 214: 329–348, 2015 [DOI] [PubMed] [Google Scholar]