Abstract
Background:
Women with schizophrenia have needs beyond their mental health needs, such as those arising out of their gender, sexual, and reproductive functions. Very little is known about the knowledge, attitude, and practice regarding contraception among women with schizophrenia from India.
Materials and Methods:
Study among women with schizophrenia (in reproductive age group, having at least one living child, and currently staying with husband) from south India explored their knowledge, attitude, and practice of contraception. Adhering to observational design and ethical principles, data were collected using a semi-structured questionnaire. Modified National Family Health Survey-3 questionnaire and Positive and Negative Symptom Scale of Schizophrenia were also used.
Results:
Ninety-six women with schizophrenia participated. The mean age was 33.5 years [standard deviation (SD): 6.8 years], and the mean age of onset of schizophrenia was 29.2 years (SD: 6.2 years). Although nearly 90% had knowledge on at least one method of contraception, the mean total number of methods known was mere two. Out of 65 women who were practising contraception, 86.2% adopted female sterilization. The common reasons for not using contraception were wish for another child/son, lack of awareness, and fear of side effects. Unmet need for family planning was 14%. Informed choice of contraception was below 3%. There was statistically significant association between those who were currently using contraception and variables such as age 31 years and above, undifferentiated subtype of schizophrenia, and greater severity of schizophrenia.
Conclusion:
Although the majority had some knowledge about contraception, decision-making largely rested with others, and informed choice regarding contraception was poor. These could pose an obstetric risk on women with schizophrenia. Sociocultural and illness-related factors influencing contraception need to be explored.
Keywords: Contraception, family planning, reproductive health, schizophrenia, women
Key messages: Women with schizophrenia have low awareness about contraceptive methods, poor informed choices, and decision-making on contraception. There exists a need to empower women with schizophrenia on family planning. We put forward an argument to strengthen reproductive health education in the mental health setting.
Schizophrenia, with its variable prognosis, affects multiple domains of an individual's life. Women with schizophrenia have a better prognosis than men, which is partly attributed to a later age of onset, differences in gender-related roles, and lesser level of expectations on functioning from the family and society.[1,2,3] Women with schizophrenia are also found to have longer sexual relationships, higher rates of marriage, and more number of children than their male counterparts.[3,4] Women with schizophrenia thus experience needs beyond their mental healthcare, and it includes their reproductive health needs. The specific and unique sexual and reproductive needs of women with schizophrenia include those pertaining to a sexual relationship, marriage, pregnancy, delivery, breastfeeding, child rearing, birth control measures, and menstrual difficulties.[5,6] Exposure to psychotropic drugs, exacerbation of schizophrenia, and limited treatment options for schizophrenia in pregnancy and postpartum period complicate the obstetric care and illness outcome of women with schizophrenia.[7,8]
Gender-related roles pose specific challenges for married women. Increased rates of coerced and unprotected sex, unwanted and unplanned pregnancies, induced abortions, and difficulties in utilising antenatal health services are some of them.[6,9] Diagnosis of schizophrenia along with gender-related disadvantages cause significant emotional burden to women with schizophrenia. For example, compared with women without mental illness attending an outpatient department, a higher number of induced abortions and coercion of unwanted sexual contact were reported in women with schizophrenia or mood disorder.[10] These in turn increase the obstetric and perinatal complications among women with schizophrenia.[11] Deficits in parenting and child rearing skills may lead to children born to mothers with mental illness being reared by others.[6,12]
The disparity between fertility preferences of a woman and her fertility behavior is referred to as the unmet need for family planning and also as knowledge, attitude, and practice (KAP) gap. Unmet need for family planning is extensively studied nationally and internationally in community-living women.[13,14,15,16,17] Women, in general, have limited autonomy over their reproductive choices.[18,19] The National Family Health Survey (NFHS) done in 2015 in urban and rural areas of India revealed contraceptive practice in 53.5% of women belonging to the reproductive (15–49 years) age group.[14] The most common method adopted (36%) was female sterilization.[14] Unmet need for family planning and spacing of pregnancies were 10% and 5%, respectively, in the state of Tamil Nadu (NFHS-4), where this study was carried out.[15] Unmet need for family planning has been studied internationally in women with schizophrenia.[6,9] Women with schizophrenia perceive difficulty in planning and obtaining family planning methods and have poor knowledge about contraception.[9] Compared with women without schizophrenia, their capacity for decision-making regarding pregnancy and birth control is diminished.[6,9]
There is lack of Indian research on family planning among women with schizophrenia. To address this paucity of data from India, we studied the KAP of contraception among women with schizophrenia.
MATERIALS AND METHODS
Setting and participants
The study was carried out in the psychiatric department of a medical college in South India. The department is a tertiary care facility catering to the local population as well as those from other states of India. The department provides comprehensive psychiatric care on both outpatient and inpatient bases.
Participants were recruited from the outpatient clinic of the Department of Psychiatry. Tamil-speaking married women of age 18–45 years, with International Classification of Diseases-10 diagnosis of schizophrenia, and accompanied by a caregiver were screened for inclusion in the study. Women with at least one living child and currently living with husband were eligible to participate in the study. Postmenopausal women and women with a history of exacerbation of their illness or inpatient treatment during the preceding 3 months were excluded. Women with intellectual disability or sensory or cognitive impairment were also excluded.
Design and statistical analysis
To assess the objectives, (a) knowledge on contraception, (b) attitude toward contraception, and (c) practice of family planning measures among women with schizophrenia, we adopted an observational study design. The study proposal was approved by the Institutional Review Board of the Medical College (IRB no. 8486 dated 9/10/2013). The study was carried out from October 2013 to May 2015. Based on inclusion and exclusion criteria, consecutive eligible participants were recruited through purposive sampling. The questionnaire was administered among those who provided written informed consent. The first author collected the data using a semi-structured interview schedule.
Descriptive statistics were used to represent sociodemographic factors, illness-related factors, pregnancy, and family details. Variables on KAP were represented as mean (M) with its standard deviation (SD) and/or frequency (N or n) with its percentage (%). Bivariate analysis was done using a comparison of means and Chi-square test; the findings were interpreted at a level of significance P < 0.05. For statistical analysis, SPSS software version 16.0 (SPSS Inc., Chicago, IL, USA) was used.
Assessment tools
Data on knowledge, attitude, and contraceptive practices were collected using a modified version of a questionnaire used in the NFHS-3.[13] To be relevant to the setting, certain questions were modified, such as providing more choices and deleting check questions. The questionnaire on contraception assesses (i) knowledge and its source, (ii) practice of contraception – current use, first use, and past use; complications, including pregnancy, on contraception; and any termination of pregnancy, and (iii) attitude toward using contraceptive methods – reasons for not using or using and reasons for delaying pregnancy. The severity of schizophrenia was rated using the Positive and Negative Syndrome Scale for schizophrenia (PANSS).[20]
RESULTS
Potential participants (124 married women with schizophrenia visiting outpatient clinic) were identified, of which 24 women met exclusion criteria. Of the rest 100 consecutive participants meeting the study criteria, 96 women provided consent. The mean age of participants was 33.5 years (SD: 6.8 years). The mean age of onset of schizophrenia was 29.2 years (SD: 6.2 years). The mean duration of schizophrenia was 4.5 years (SD: 3.9 years). The mean total PANSS score reflecting the severity of the condition was 38.7 (SD: 7.4). Table 1 provides further details on the participants’ sociodemographic and clinical profiles.
Table 1.
Sociodemographic profile and clinical profile of study participants
| Sociodemographic variable | n (%) |
|---|---|
| Age (years) | |
| Upto 30 | 34 (35.4%) |
| 31 and above | 62 (64.6%) |
| Educational status | |
| Illiterate | 7 (7.2%) |
| School education | 71 (73.9%) |
| Graduation | 18 (18.7%) |
| Place of residence | |
| Rural | 66 (68.8%) |
| Urban | 30 (31.2%) |
| Socioeconomic status | |
| Lower | 61 (63.5%) |
| Middle | 35 (36.5%) |
| Upper | 1 (1.0%) |
| Religion | |
| Hindu | 87 (90.6%) |
| Muslim | 6 (6.3%) |
| Christian | 3 (3.1%) |
| Employment status | |
| Unemployed | 90 (93.8%) |
| Employed | 6 (6.2%) |
| Clinical variable | n (%) |
| Schizophrenia subtype | |
| Paranoid schizophrenia | 64 (66.7%) |
| Undifferentiated schizophrenia | 32 (33.3%) |
| Duration of contact with mental health services | |
| <5 years | 77 (80.2%) |
| 5-10 years | 13 (13.5%) |
| More than 10 years | 6 (6.2%) |
| Mode of treatment | |
| Only outpatient treatment | 80 (83.3%) |
| Inpatient treatment at least once | 26 (16.7%) |
| Self-reported treatment compliance | |
| Poor | 18 (18.8%) |
| Misses occasionally | 30 (31.2%) |
| Good | 48 (50.0%) |
Obstetric profile
The participants were married for a mean of 13.8 years (SD: 7.7 years). Eighty-one participants (84.4%) expressed a desire to have two or more children, wherein 70 participants (72.9%) had two or more children. Thirty-one participants (32.3%) had the last childbirth within the last 5 years, 27 participants (28.1%) between the last 5–10 years, and 38 participants (39.6%) more than 10 years ago. Seventeen participants (17.1%) reported that they had their delivery at home.
One out of every five participants (n = 19, 19.8%) had undergone medical termination of pregnancy in the past. Unplanned pregnancy was the leading cause for medical termination of pregnancy (n = 11), followed by medical reasons (n = 3) and reasons such as fear of having a female child, completed family, family wish, and financial reason (n = 1 each). In one patient, it was not possible to elicit any specific reasons.
Knowledge about contraception
Knowledge of any method of contraception was reported by 88.5% of the participants. About a tenth (n = 10, 10.4%) did not know of any method. Half of the participants (n = 49, 51%) had knowledge about more than one contraceptive method. Female sterilization, intrauterine devices, condoms, and oral contraceptive pills were the most commonly known contraceptive methods. The median number of contraceptive methods known per participant was two, ranging from zero to five. The knowledge of individual contraceptive methods among women in this study group is shown in Table 2.
Table 2.
Knowledge of contraception among study participants, n=96
| Contraception methods | Know (%)* |
|---|---|
| Female sterilization | 72 (75.0%) |
| Male sterilization | 2 (2.1%) |
| Oral contraceptive pill | 26 (27.1%) |
| Intrauterine device/loop | 40 (41.7%) |
| Injectable | 5 (5.2%) |
| Implant | 0 (0.0%) |
| Condom | 29 (30.2%) |
| Female condom | 1 (1.0%) |
| Diaphragm | 0 (0.0%) |
| Rhythm method | 6 (6.25%) |
| Withdrawal method | 1 (1.0%) |
*The total percentage is more than 100 because some participants have knowledge about more than one method
Attitude toward the contraceptive practice
A majority of women (n = 65, 67.7%) in the study group were using a contraceptive method at the time of the study. Only three participants (4.6%) cited the presence of schizophrenia as the reason for adopting a contraceptive method. About one-third (n = 31; 32.3%) were not using any contraceptive methods at the time of the study. Many of the subjects had more than one reason for not using contraception. The reasons cited by participants for using and not using contraception are given in Table 3.
Table 3.
Attitude toward contraception among study participants
| Reason for current contraception use (n=65) | n (%)* |
|---|---|
| Small family norm | 38 (58.5%) |
| Completed family | 26 (40%) |
| Economic reasons | 9 (13.8%) |
| Spacing | 3 (4.6%) |
| Exacerbation of illness during pregnancy and postpartum | 3 (4.6%) |
| Social reasons | 3 (4.6%) |
| Motivation to use contraception | 1 (1.5%) |
| Reason for not adopting contraception currently, n=31 | n (%)* |
| Lack of adequate awareness | 11 (35.5%) |
| Fear of side effects | 8 (25.8%) |
| Wants to have a male child/another child | 14 (45.2%) |
| Did not receive information about family planning in mental health services | 10 (32.3%) |
| Social reasons | 3 (9.6% ) |
| Not expecting to have sex | 3 (9.6% ) |
| Difficulty in planning ahead about contraception | 1 (3.2%) |
| Difficulty in accessing family planning services | 1 (3.2%) |
| Felt her view was not considered important by her family | 1 (3.2%) |
| Inconvenient to use | 1 (3.2%) |
*The total percentage is more than 100 because some participants might be citing more than one reason
Nearly 15% of the participants (n = 14, 14.6%) were found to have unmet contraceptive needs, that is, KAP gap or wanting to avoid pregnancy but not using any contraceptive method. Among these subjects who had unmet contraceptive needs, many had reported multiple reasons for not using contraception. The commonly cited reasons were lack of awareness (8 of 14), not receiving any information (7 of 14), fear of side effects (5 of 14), and social reasons/opposition from the family (3 of 14). A majority of the participants (n = 57; 59.4%) felt it to be necessary to discuss with the treating doctor about contraception.
Among those who were current users, only 3.1% were ever told about other methods of contraception. Only 1.5% of current users were told about the side effects of the current contraceptive method being used. None of the current users were told what to do if there are side effects to current methods of contraception.
Out of the 73 women who were the first time users of contraception, 38 (52.1%) had undergone permanent sterilization, whereas the remaining 35 (47.9%) used temporary methods. Among these, 22 (62.9%) had discontinued their use of the temporary method. Reasons for discontinuing contraception were wanting another child (10 of 22, 45.5%), side effects (9 of 22, 40.9%), and other reasons (3 of 22; 13.6%). A majority of the group (49 of 73; 67.1%) had started using contraception for the first time when they had at least two children. In majority of instances, decision-making regarding the use of contraception for the first time was made by others. Decision-makers regarding the use of contraception for the first time are depicted in Figure 1.
Figure 1.
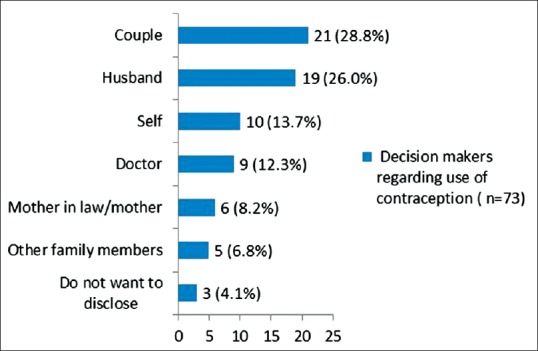
Decision-maker during first use of contraception among study participants, n = 73. X-axis: frequency of responses with percentage; Y-axis: decision-maker of contraception
Contraceptive practice
Women were classified into three mutually exclusive categories with respect to their contraceptive use: those practicing contraception currently – “current users;” those who have used at any time – “ever users;” and those who never practiced contraception – “never users.” Less than a quarter of the study group (n = 22, 22.9%) had never used contraception at any point of time.
Contraceptive use at some point of time (ever use)
Out of 96 women, 74 (77.1%) had used contraception at some point in time. A majority of them (n = 56, 58.3%) underwent sterilization. An intrauterine device was used by 15.6% (n = 15). Among the spouses of the women, 10.4% (n = 10) used condoms, and 3.1% (n = 3) underwent sterilization. Among ever users, rhythm method was practised by 3.1% (n = 3) of the couples and withdrawal method by another 3.1% (n = 3). None of them used female condoms, depot injections, or emergency contraception.
Current use of contraception
A majority of the women (n = 65, 67.7%) were using a contraceptive method at the time of the study. Duration of the practice of any contraceptive method was about 10 years (mean: 9.9 years, SD: 6.6 years). Prevalence of contraception was 26.9% among those with one child, 79.2% among those with two children, 93.3% among those with three children, and 100% among those with four or more children. Out of 65 women who were practicing contraception, the majority (n = 56, 86.2%) had adopted female sterilization. Intrauterine contraceptive device, male sterilisation, use of a male condom, rhythm method, and withdrawal were adopted by only a few (9 of 65; 13.8%) couples. No one was using methods such as oral contraceptive pills, injectable, implants, female condom, or diaphragm.
Association of the current use of contraception with sociodemographic and clinical variables
The mean difference in PANSS total score was statistically significant (P = 0.019) between those who adopted contraception (PANSS score 39.9) and those who did not (PANSS score 36.2). The results of bivariate analysis using Chi-square test are provided in Table 4.
Table 4.
Association of sociodemographic and clinical variables with the current use of contraception using Chi-square test
| Not using contraception | Using contraception | Chi-square value | P | |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age (years) | ||||
| Upto 30 | 17 (54.8%) | 17 (26.2%) | 7.551 | 0.006* |
| 31 and above | 14 (45.2%) | 48 (73.8%) | ||
| Place of residence | ||||
| Urban | 10 (32.3%) | 20 (30.8%) | 0.022 | 0.883 |
| Rural | 21 (67.7%) | 45 (69.2%) | ||
| Education | ||||
| Less than high school | 8 (25.8%) | 15 (23.1%) | 0.086 | 0.770 |
| High school and above | 23 (74.2%) | 50 (76.8%) | ||
| Socioeconomic status | ||||
| Lower | 19 (61.3%) | 42 (64.6%) | 0.100 | 0.752 |
| Middle and upper | 12 (38.7%) | 23 (35.4%) | ||
| Clinical | ||||
| Type of schizophrenia | ||||
| Paranoid | 26 (83.9%) | 38 (58.5%) | 6.098 | 0.014* |
| Undifferentiated | 5 (16.1%) | 27 (41.5%) | ||
| Duration of schizophrenia | ||||
| <5 years | 22 (71.0%) | 41 (63.1%) | 0.579 | 0.447 |
| 5 years and more | 9 (29.0%) | 24 (36.9%) | ||
| Duration of contact with mental health services | ||||
| <5 years | 25 (80.6%) | 52 (80.0%) | 0.006 | 0.941 |
| 5 years and more | 6 (19.4%) | 13 (20.0%) | ||
| Mode of treatment | ||||
| Only outpatient | 28 (90.3%) | 52 (80.0%) | 1.610 | 0.204 |
| At least once inpatient | 3 (9.7%) | 13 (20.0%) |
*P<0.05
DISCUSSION
The study identified low knowledge of contraception among the participants when compared with the state statistics. Knowledge on at least one contraceptive method was 88.5% in our study sample, whereas it was 99.4% in Tamil Nadu (NFHS-4).[15] Also, the mean number of contraceptive methods known to our study participants was only two when the mean number of contraceptive methods known to married women in Tamil Nadu was eight (NFHS-4).[15] This low knowledge in our sample was despite our participants being educated, having at least one child, and having higher contraception prevalence rate than the state average. In our sample, although a majority reported that they knew at least one contraceptive method, 11.5% of participants still reported lack of adequate awareness to decide upon contraception. It further revealed the lacunae in the transition from mere knowledge to adequate awareness and the adoption of contraception among the participants.
Preconception counselling among those with psychosis aids in allaying women's anxieties and thereby preventing disease relapse, in enhancing women's emotional support, in timing pregnancy (i.e., not during a relapse period), in averting unplanned pregnancies and their consequences, in drug rationalization that are safe in pregnancy, in close monitoring of symptoms, in adopting appropriate contraception measures that would not impact the illness, and so on. Education and preconception counselling, which are possible in a mental health setting, will enable the patient to assess the risk–benefit ratio of conceiving a child in the future.[6,9,21] Recognizing these benefits, many existing guidelines have identified imparting knowledge regarding contraception and planning for the family as part of the clinical care.[9,21] However, there is an absence of adequate prepregnancy counselling in Indian psychiatric facilities.[7] Our findings endorse the idea that mental health facilities should give priority in discussing birth control measures, especially when more than half of the study participants expressed their willingness to discuss contraception with their treating psychiatrist. Furthermore, the impact of such an initiative in improving patients’ knowledge can also be evaluated.
Our study revealed that attitude toward contraception among women with schizophrenia in our sample could be mediated by sociocultural factors. Nearly half of those who were not currently using contraceptives cited a desire to have a male child/another child as the reason for not adopting contraception. Family health surveys in India had long before identified the preference for sons in certain Indian states, which include Tamil Nadu. Citing the wish to have a male child or another child as a reason for not using contraception is a culturally sanctioned practice in India.[19,22] However, this reason of wanting to have a male child provided by our sample was different from the reasons for not using contraception in women with schizophrenia from the western world.[9,10,23] More than half of the women in this group were also noted to have discontinued their use of contraceptive practices after the initial use. This should be noted along with the high rates of medical termination of pregnancy in the study population being attributed to unwanted pregnancy. It had to be emphasized that unplanned pregnancy and its consequences carry significant risk in these vulnerable women.[6,11,24]
Only a little above one-third of women reported that they had a role in decision-making about contraception while they adopted contraception for the first time. Decision-making about the use of contraception in Indian women has been recorded to arise from within the family, especially in a joint household.[25] Less than half of the study population also noted that the decision about the first time contraceptive use was taken by the family members. In the extremes of Indian scenario, there were objections to contraceptive use from within the family.[26,27] This is in contrast with the person-centric approach of the West, where the role of the family in reproductive decision making is minimal. Markers of informed choice of family planning – users ever told about other methods, users told about side effects of current method, and users told what to do if there are side effects of the current method – were alarmingly low in our participants. This hard reality existed when NFHS-4 reported informed choice to be three-fouth among Tamil Nadu women.[15] The poor informed choices about methods of contraception and side effects cannot thus be completely attributed to cultural norms such as family-centric decision-making.[25] How does the presence of schizophrenia influence the informed choice of contraception is worth exploring. Our findings on decision-making and informed choices endorse the broader concept of women's mental health in India, wherein biological factors interplay with sociocultural factors.[28,29]
Fourteen percent of the sample reported unmet contraceptive need, whereas unmet contraceptive need in Tamil Nadu as per NFHS-4 was 10%.[15] The common reasons cited by our participants were lack of awareness, lack of information, and fear of side effects. These reasons were similar to those quoted by community-living women in India.[30] One of the consequences of unmet contraceptive need is unplanned pregnancy, which then leads to medical termination of pregnancy. Numbers of unmet contraceptive need, medical termination of pregnancy, and unplanned pregnancy reported in our sample agree with this argument. Sociodemographic factors such as education and socioeconomic status were found to influence decision-making on medical termination of pregnancy among Indian women with psychiatric illness,[31] thereby endorsing the role of social factors. A mental health professional can play a role in surrogate/assisted decision-making with beneficence and non-maleficence regarding the termination of pregnancy in women with major mental illness when the patient's threshold of autonomy and cognitive, evaluative, appreciative understanding of the problem is in question.[32]
The practice of contraception, evident by contraception prevalence rate, in our sample was 67.7%. This was higher than the NFHS-4 Tamil Nadu data for married with at least one child, which was 58.4%.[15] This difference becomes more relevant when we understand that we expect higher rate in NFHS-4 sample than our study sample because NFHS-4 data are from women of a wider age group. Adoption of female sterilization among women (with at least one child) among our participants was comparable to NFHS-4 Tamil Nadu rate, 58.3% and 54.23%, respectively.[15] The trend of higher prevalence of female sterilization with an increasing number of children in this study is similar to the pattern seen in the community. Findings from our hospital-based sample thus matched findings from the community samples. However, sterilization as the major contraceptive practice in our sample was different from the practice reported from the West.[33] Again, sociocultural factors, especially gender-specific roles and family-driven choices in decision-making, might have influenced the practice of contraception among women with schizophrenia.[25] Factors influencing the majority of women with schizophrenia to choose permanent methods over modern reversible methods are yet to be studied in India. Since multiple factors, both personal and social, influence the practice of contraception among women,[34,35] whether such factors would have influenced the specific pattern of contraception practices in our sample need to be studied.
The association between age and contraception was expected: the higher the age, the greater the chance of adopting contraception. Other sociodemographic variables did not have an association with contraception use. The study did not reveal any association between clinical variables studied, except for the severity of schizophrenia and subtype of schizophrenia. These findings need further exploration.
The strengths of the study are we attempted to address a neglected side of healthcare, namely, reproductive health of women with schizophrenia. To our knowledge, this is the first study from India exploring KAP of contraception among women with schizophrenia. The study adopted a nationally valid tool (NFHS) for assessing the primary objective.
The limitations of our study are as follows: comparisons could not be done in view of the absence of controls, results cannot be generalized to community setting in view of hospital-based sampling, and results are not generated for subpopulations due to limited sample size. Further research covering limitations of our study are required to look at various factors influencing contraceptive behavior in women with schizophrenia.
CONCLUSION
Overall, our study brought out the following regarding contraception among women with schizophrenia: deficiencies in their knowledge, limitations in their awareness, possible sociocultural influences on their attitude toward contraception, and a low informed choice in spite of high contraceptive prevalence. Hence, we put forward an argument to strengthen reproductive health education in the mental health setting and study its impact on KAP. Our study results pave way for exploring the notion of sociocultural factors influencing contraceptive practice in women with schizophrenia and schizophrenia further complicating this practice. Such a notion, if proven, emphasizes that contraception is quite complex for Indian women when they suffer from schizophrenia.
Financial support and sponsorship
Fluid research grant, Christian Medical College, Vellore.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors sincerely thank Dr. Reeta Vijayaselvi, Associate Professor, Department of Obstetrics, Christian Medical College, Vellore, for her contributions in conceptualizing contraception among women. They acknowledge the valuable input by Dr. Kishore GSB.
REFERENCES
- 1.Nasser EH, Walders N, Jenkins JH. The experience of schizophrenia: What's gender got to do with it? A critical review of the current status of research on schizophrenia. Schizophr Bull. 2002;28:351–62. doi: 10.1093/oxfordjournals.schbul.a006944. [DOI] [PubMed] [Google Scholar]
- 2.Thara R, Rajkumar S. Gender differences in schizophrenia. Results of a follow up study from India. Schizophr Res. 1992;7:65–70. doi: 10.1016/0920-9964(92)90075-g. [DOI] [PubMed] [Google Scholar]
- 3.Thara R, Kamath S. Women and schizophrenia. Indian J Psychiatry. 2015;57:S246–51. doi: 10.4103/0019-5545.161487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Boer MK, Castelein S, Wiersma D, Schoevers RA, Knegtering H. The facts about sexual (Dys) function in Schizophrenia: An overview of clinically relevant findings. Schizophr Bull. 2015;41:674–86. doi: 10.1093/schbul/sbv001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seeman MV. Schizophrenic men and women require different treatment programs. J Psychiatr Treat Eval. 1983;5:143–8. [Google Scholar]
- 6.Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23:623–35. doi: 10.1093/schbul/23.4.623. [DOI] [PubMed] [Google Scholar]
- 7.Desai G, Babu GN, Chandra PS. Unplanned pregnancies leading to psychotropic exposure in women with mental illness – Findings from a perinatal psychiatry clinic. Indian J Psychiatry. 2012;54:59–63. doi: 10.4103/0019-5545.94649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson GE. Treatment of schizophrenia in pregnancy and postpartum. J Popul Ther Clin Pharmacol. 2012;19:e380–6. [PubMed] [Google Scholar]
- 9.Miller LJ, Finnerty M. Family planning knowledge, attitudes and practices in women with schizophrenic spectrum disorders. J Psychosom Obstet Gynaecol. 1998;19:210–17. doi: 10.3109/01674829809025699. [DOI] [PubMed] [Google Scholar]
- 10.Coverdale JH, Turbott SH, Roberts H. Family planning needs and STD risk behaviors of female psychiatric out-patients. Br J Psychiatry. 1997;171:69–72. doi: 10.1192/bjp.171.1.69. [DOI] [PubMed] [Google Scholar]
- 11.Vigod SN, Kurdyak PA, Dennis CL, Gruneir A, Newman A, Seeman MV. Maternal and newborn outcomes among women with schizophrenia: A retrospective population-based cohort study. BJOG. 2014;121:566–74. doi: 10.1111/1471-0528.12567. [DOI] [PubMed] [Google Scholar]
- 12.Arvaniti A, Spyropoulou A, Zervas I. Parenting capacity of mothers with schizophrenia. Psychiatriki. 2012;23:314–21. [PubMed] [Google Scholar]
- 13.National Family Health Survey (NFHS-3), India, 2005–06. I. Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. [Google Scholar]
- 14.National Family Health Survey (NFHS-4), India, 2015–16. Mumbai: IIPS; 2017. International Institute for Population Sciences (IIPS) and ICF. [Google Scholar]
- 15.National Family Health Survey (NFHS-4), India, 2015–16: Tamil Nadu. Mumbai: IIPS; 2017. International Institute for Population Sciences (IIPS) and ICF. [Google Scholar]
- 16.Darroch JE, Singh S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: An analysis of national surveys. Lancet. 2013;381:1756–62. doi: 10.1016/S0140-6736(13)60597-8. [DOI] [PubMed] [Google Scholar]
- 17.Sedgh G, Hussain R, Bankole A, Singh S. New York, NY: Guttmacher Institute; 2007. Women with an Unmet Need for Contraception in Developing Countries and Their Reasons for not Using a Method, Occasional Report. No. 37. [Google Scholar]
- 18.Moursund A, Kravdal O. Individual and community effects of women's education and autonomy on contraceptive use in India. Popul Stud (Camb) 2003;57:285–301. doi: 10.1080/0032472032000137817. [DOI] [PubMed] [Google Scholar]
- 19.Pachauri S. Priority strategies for India's family planning programme. Indian J Med Res. 2014;140:S137–46. [PMC free article] [PubMed] [Google Scholar]
- 20.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for Schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 21.Seeman MV, Ross R. Prescribing contraceptives for women with Schizophrenia. J Psychiatr Pract. 2011;17:258–69. doi: 10.1097/01.pra.0000400263.52913.dc. [DOI] [PubMed] [Google Scholar]
- 22.Chaudhuri S. The desire for sons and excess fertility: A household-level analysis of parity progression in India. Int Perspect Sex Reprod Health. 2012;38:178–86. doi: 10.1363/3817812. [DOI] [PubMed] [Google Scholar]
- 23.Coverdale JH, Aruffo JA. Family planning needs of female chronic psychiatric outpatients. Am J Psychiatry. 1989;146:1489–91. doi: 10.1176/ajp.146.11.1489. [DOI] [PubMed] [Google Scholar]
- 24.Dudzinski DM. Compounding vulnerability: Pregnancy and schizophrenia. Am J Bioeth. 2006;6:W1–14. doi: 10.1080/15265160500506191. [DOI] [PubMed] [Google Scholar]
- 25.Jejeebhoy SJ. Women's Education, Autonomy, and Reproductive Behaviour: Experience from Developing Countries. OUP Catalogue. 1995 [Google Scholar]
- 26.Dhillon BS, Chandhiok N, Kambo I, Saxena NC. Induced abortion and concurrent adoption of contraception in the rural areas of India (an ICMR task force study) Indian J Med Sci. 2004;58:478–84. [PubMed] [Google Scholar]
- 27.Rai RK, Unisa S. Dynamics of contraceptive use in India: Apprehension versus future intention among non-users and traditional method users. Sex Reprod Health. 2013;4:65–72. doi: 10.1016/j.srhc.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Malhotra S, Shah R. Women and mental health in India. An overview. Indian J Psychiatry. 2015;57:205–11. doi: 10.4103/0019-5545.161479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma I, Pathak A. Women mental health in India. Indian J Psychiatry. 2015;57:201–4. doi: 10.4103/0019-5545.161478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robey B, Ross J, Bhushan I. Meeting unmet need: New strategies. Popul Rep J. 1996:1–35. [PubMed] [Google Scholar]
- 31.Chadda KR, Sood M. Indian research on women and psychiatry. Indian J Psychiatry. 2010;52:229–32. doi: 10.4103/0019-5545.69237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coverdale JH, McCullough LB, Chervenak FA. Assisted and surrogate decision making for pregnant patients who have schizophrenia. Schizophr Bulll. 2004;30:659–64. doi: 10.1093/oxfordjournals.schbul.a007113. [DOI] [PubMed] [Google Scholar]
- 33.Oppelt PG, Baier F, Fahlbusch C, Heusinger K, Hildebrandt T, Breuel C. What do patients want to know about contraception and which method would they prefer? Arch Gynecol Obstet. 2017;295:1483–91. doi: 10.1007/s00404-017-4373-1. [DOI] [PubMed] [Google Scholar]
- 34.Moos MK, Bartholomew NE, Lohr KN. Counseling in the clinical setting to prevent unintended pregnancy: An evidence-based research agenda. Contraception. 2003;67:115–32. doi: 10.1016/s0010-7824(02)00472-9. [DOI] [PubMed] [Google Scholar]
- 35.Pratt R, Stephenson J, Mann S. What influences contraceptive behaviour in women who experience unintended pregnancy? A systematic review of qualitative research. J Obstet Gynaecol. 2014;34:693–9. doi: 10.3109/01443615.2014.920783. [DOI] [PubMed] [Google Scholar]


