Abstract
This study addresses three research questions critical to understanding if and how skin color shapes health among African Americans: Does skin color predict body-mass index (BMI) among African American adults aged 32–55? To what extent is this relationship contingent on gender or age? Do sociodemographic, psychosocial, and behavioral factors explain the skin color-BMI relationship? Using data from the Coronary Artery Risk Development in Young Adults Study and growth curve models, results indicate that dark-skinned women have the highest levels of BMI across adulthood compared to all other skin color-gender groups. BMI gaps between dark- and lighter-skinned women remain stable from ages 32–55. Among men, a BMI disadvantage emerges and widens between light- and dark-skinned men and their medium-skinned counterparts. Observed sociodemographic characteristics, stressors, and health behaviors do not explain these associations. Overall, findings suggest that skin color- and gender-specific experiences likely play an important role in generating BMI inequality.
Keywords: skin color inequality, intersectionality, life course, African Americans
Overweight and obesity are significant health concerns in the United States (US). These statuses are linked to cardiovascular disease, which remains the leading cause of death in the US, as well as several psychiatric disorders, poor health conditions, and premature mortality (Hruby et al. 2016; Petry et al. 2010). Research also documents stark racial disparities in overweight/obesity and body-mass index (BMI), with African Americans experiencing higher BMIs at almost every stage of life compared to their white counterparts (Ailshire and House 2011; Hargrove 2018). Studies have generally been unable to completely explain these disparities in BMI, even when accounting for social factors such as socioeconomic status (SES) or stressors.
The persistent BMI disadvantages of African Americans may be a result, in part, of the tendency of prior research to rely on self-identification variables as the sole measure of race (Cobb et al. 2016). This stands in contrast to a long tradition of scholarship indicating that race is a multifaceted, evolving social concept comprised of different indicators (Roth 2016). An important status characteristic that may intersect with other indicators of race to shape health is skin color. It is well-documented that African Americans with lighter skin experience social and economic advantages compared to their darker-skinned counterparts given their closer physical resemblance to Europeans and Eurocentric standards of beauty, intelligence, and morality (Dixon and Telles 2017; Monk 2014). Research on this topic also suggests that the consequences of skin color are gendered, with skin tone being more salient in the lives of black women compared to black men (Hunter 2007).
While the body of research on skin tone and health is growing, several limitations characterize the current literature. First, this research is comprised of older studies that focused on a specific health outcome (e.g., blood pressure) and a handful of more recent studies that produce mixed findings (e.g., Borrell et al. 2006; Monk 2015). Second, the extent to which the physical health consequences of skin color vary by gender is unclear. Prior research has generally treated the consequences of social statuses as additive in nature, precluding opportunities to examine the health consequences of unique positions in the social hierarchy (e.g., occupying dominant positions in the gender hierarchy, yet subordinate positions in the racial hierarchy). Intersectionality perspectives posit that dimensions of inequality such as race, color, and gender are experienced simultaneously and are interdependent—that is, they mutually construct the meanings and experience of one another (Collins 2015; López and Gadsden 2016). Social statuses may therefore combine in ways that differentiate the social realities and health-relevant contexts of individuals belonging to broadly-defined social groups.
Third, whether and how the health consequences of skin color and gender unfold with age is unknown. No studies have examined how skin color and gender combine to shape age-trajectories of BMI across adulthood. Relatedly, the potential mechanisms underlying skin color-gender differences in BMI across adulthood remain unclear. Our understanding of the dynamic and complex nature of BMI inequality among African Americans therefore remains limited.
The present study seeks to fill gaps of prior research by investigating the extent to which skin color shapes BMI trajectories between early adulthood and mid-life. Three central research questions frame this study. First, does skin color predict age-trajectories of BMI among African American adults? Second, is the relationship between skin color and BMI contingent on gender? Third, do sociodemographic, psychosocial, and behavioral factors explain the skin color-BMI relationship? To address these questions, I examine skin color differences in BMI among African Americans across ages 32–55 using panel data from the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
BACKGROUND
Skin Color and Health: An Overview
Skin tone is a significant determinant of life chances and lived experiences among African Americans. Colorism, or the systematic privileging of light skin, represents a structural and ideological system of inequality that affords minorities with lighter skin complexions advantages over their darker-skinned counterparts (Dixon and Telles 2017). Historically, the phenotypic resemblance and assumed similarity to Eurocentric standards of beauty, morality, and intellect granted light-skinned blacks greater access to resources and opportunities including education, property, and jobs (Keith and Herring 1991; Monk 2014). Intergenerational transfers of these social and economic privileges situated light-skinned African Americans in privileged positions in the social hierarchy relative to their darker-skinned counterparts (Adams, Kurtz-Costes, and Hoffman 2016; Hill 2002a).
While skin color stratification in several aspects of life is well-documented, particularly SES (Monk 2014), considerably less is known about the extent to which skin color shapes physical health among African Americans. Older studies on this topic focused on blood pressure and found that dark-skinned African Americans had increased risks for high blood pressure/hypertension compared to their lighter-skinned counterparts (Boyle 1970; Harburg et al. 1978; Klag et al. 1991). Recent studies of skin color have given more attention to its broader health consequences, relying on stress process perspectives to explicate how positions in the social structure influence health. Stress process models posit that risk (e.g., stress exposure) and protective factors (e.g., the availability of socioeconomic and coping resources) arise out of one’s social context (Pearlin et al. 1981). Studies utilizing a stress process framework would predict that dark-skinned African Americans have the worst health because, given their placement in the social hierarchy, they are more likely than their lighter-skinned counterparts to be exposed to stressors/discrimination and experience barriers to socioeconomic achievement. Yet, while studies generally find that African Americans of darker-skin experience worse physical health, findings are mixed, and disparities are not explained by measures of SES or stressors.
For example, of two studies using data from the CARDIA Study, one finds no significant association between skin tone and self-ratings of health (Borrell et al. 2006) while the other documents significantly higher blood pressure among dark-skinned African Americans, even when accounting for sociodemographic characteristics, health behaviors, and medication use (Sweet et al. 2007). A more recent study using the National Survey of American Life finds that African Americans who self-report having darker skin have higher odds of hypertension than their light-skinned counterparts (Monk 2015). This relationship is not explained by sociodemographic factors or experiences of racial and skin color discrimination. Similarly, Cobb and colleagues (2016) report a skin color gradient in allostatic load, a measure of physiological functioning, that is not accounted for by SES among African American adults living in Nashville, Tennessee.
While these studies provide critical insights into the association between skin color and health, several limitations remain. First, the relationship between skin color and BMI is less clear. That is, no studies have investigated how the intersections of skin color, gender, and age may uniquely shape trends in BMI. Documenting the nature of BMI inequality is critical for tracing future disease and health risks. Indeed, BMI is an indicator of poor or worsening health even before disease is manifest in young and middle-aged adults, for whom clinical diagnoses may be premature (Hruby et al. 2016). Second, use of stress process models to explain associations between skin color and health has been limited. These models, for example, do not explicitly account for the possibility that the relationship between skin color and health may be contingent on other social characteristics (e.g., gender). Additionally, they give insufficient attention to the life course-patterning of health inequalities. Both issues are discussed in more detail below.
Skin Color and Gender: An Intersectionality Approach
The extent to which skin color and gender combine to shape BMI among African Americans is unclear. Prior research has tended to overlook how the nature of health inequalities may be conditional on specific social statuses. To address this limitation, scholars have increasingly used an intersectionality framework to understand health disparities (Ailshire and House 2011; Brown et al. 2016; Hargrove 2018). Intersectionality posits that systems of inequality are interlocking, with social statuses mutually constructing the meanings and consequences of each other (Collins 2015). The simultaneity and interdependence of social statuses may produce unique social contexts in which both power and disadvantage are experienced (Lòpez and Gadsden 2016). Thus, an individual’s location in the racial, color, and gender hierarchies may produce unique forms of gendered racism or colorism that shape opportunities for healthy living (Gilbert et al. 2016; Hall 2017).
Indeed, scholars posit that given its intersection with sexism, forms and consequences of colorism vary by gender (Hill 2002a; Hall 2017). Skin color is argued to be more consequential in the lives of African American women compared to men because the significance and consequences of beauty are gendered. Physical appearance and attractiveness play a role in determining socioeconomic success and other life chances for women living in patriarchal societies in ways they do not for men (Anderson et al. 2010; Hamermesh 2011). Beauty, defined by fairer skin and other European features, can therefore act as a form of capital women use to accumulate socioeconomic resources and lessen exposure to risks (Dixon and Telles 2017; Keith and Herring 1991; Hunter 2007). Darker-skinned African American women, and to some degree men, may lack access to this type of capital. Few studies, however, have explicitly considered whether and how health varies by the joint statuses of skin color and gender. It is possible that the intersections of skin color and gender unequally distribute health risk and protective factors relevant for weight gain among African Americans.
Incorporating Age: A Life Course Perspective
Insufficient attention has also been given to how the relationships among skin color, gender, and BMI might vary with age. Life course theory posits that social factors collectively and cumulatively combine throughout one’s life span to shape health. The salience of social factors or statuses (e.g., skin color) depends on an individual’s experiences, roles, and stage in life (Ferraro 2016). It is therefore likely that risks and resources relevant for health accumulate or dissipate over the life course, affecting the nature of health inequality across age (Ferraro, Schafer, and Wilkinson 2016).
Three hypotheses describe patterns of intracohort inequality over time. First, aging-as-leveler posits that the negative consequences of aging disproportionately affect the socially advantaged because these individuals have been able to delay the onset of poor health to later ages. Furthermore, the socially disadvantaged who survive to older ages may represent a selective, robust group (House et al. 2005). This hypothesis therefore predicts that BMI gaps will diminish with age. Second, persistent inequality asserts that health (dis)advantages hold over time, with age doing little to either ameliorate or exacerbate the inequality (Ferraro and Farmer 1996). Consequently, persistent inequality predicts that disparities in BMI are stable with age.
Third, cumulative disadvantage posits that individuals with advantages early in life accumulate more resources and opportunities over time that can be used to avoid or allay health risks (Ferraro 2016; Shuey and Willson 2008). Conversely, those who are initially disadvantaged acquire more disadvantages and risks as they age, resulting in a widening of health inequalities with age. While there is no available empirical research to infer whether and how disparities in BMI by skin color change with age, prior research indicates that racial inequalities in health tend to widen throughout early and midlife given cumulative and differential exposure to risks and resources (Hargrove 2018; Shuey and Willson 2008). Similar processes may operate for skin color inequalities in health with age.
Mechanisms Linking Skin Color to Health
A final limitation of prior research is the insufficient attention given to a diverse set of mechanisms that may link skin color to health (see Monk 2015 for an exception). Sociodemographic characteristics are one likely mechanism. Research has documented a robust relationship among education, income, marital status, and health (Adler and Stewart 2010; Robards et al. 2012). These factors embody intrinsic and tangible resources that grant access to health promoting resources, behaviors, and knowledge, as well as limit exposure to health risks (Phelan and Link 2015). Additionally, the distribution of sociodemographic characteristics varies by skin color among African Americans, as lighter-skinned individuals tend to have higher levels of education, income, and marriage compared to their darker-skinned counterparts (Hamilton, Goldsmith, and Darity 2009; Monk 2014). These advantages stem from increased access to prestigious educational environments and rewarding labor markets for those of lighter skin, as well as their greater desirability in marriage pools (Dixon and Telles 2017; Goldsmith, Hamilton, and Darity 2007; Hamilton et al. 2009; Wade, Romano, and Blue 2004).
Chronic and discrimination-related stressors are another potential mechanism underlying relationships between skin color and BMI. Social stressors affect health through several pathways, including the structuring of opportunities and resources, residence in impoverished neighborhoods, unhealthy coping behaviors, and advanced bodily deterioration (Gee and Ford 2011; Williams and Mohammed 2013). It is likely that exposure to stressors among African Americans varies by skin color for several reasons. First, as a marker of status, skin color significantly influences the allocation of social, economic, and political resources. Darker-skinned individuals, particularly women, tend to have fewer of these resources, creating more obstacles to successfully navigate life relative to their light-skinned counterparts (Keith and Herring 1991; Monk 2014).
Second, within racialized societies such as the US, skin tone is a phenotypic feature that signals other presumed personal characteristics, including race, attractiveness, and competency (Adams et al. 2016; Bonilla-Silva 2017). Given that individuals rely on such characteristics to navigate social interactions (Fishbein and Ajzen 2011), it is likely that darker-skinned African Americans experience greater exposure to discrimination than their light-skinned counterparts. However, modest evidence provides support for this hypothesis (Keith et al. 2017; Monk 2015). One possible explanation is that the meanings and consequences of skin color are not static—they are dependent on social contexts (Celious and Oyserman 2001; Uzogara and Jackson 2016). For example, while individuals with light skin may experience more favorable treatment from whites compared to their darker-skinned counterparts, they may also experience considerable unfair treatment from other African Americans because they are less readily perceived as members of the black community (Hall 2017; Monk 2015; Uzogara and Jackson 2016). In turn, social cues and treatments by in-group members that do not confirm personal identities and act to exclude individuals from the groups with which they identify can induce stress and unhealthy behaviors (Campbell and Troyer 2007; Hall 2017).
Moreover, African Americans with medium skin tones may be less stigmatized in majority black contexts or in interactions with other African Americans, as these individuals represent the “prototypic” black phenotype (Maddox 2004; Uzogara and Jackson 2016). Medium brown skin tones have not generally been associated with the negative characteristics assigned to light and dark brown skin within the African American community (Adams et al. 2016; Celious and Oyserman 2001). This argument would predict that those with medium brown skin complexions enjoy more favorable interactions in intra-racial settings compared to their light- and dark-skinned counterparts, reducing exposure to adverse, unhealthy experiences. While there are competing hypotheses for which skin tones may be disadvantaged in terms of health, there is broad agreement that skin color is used by society to evaluate and position others in the social hierarchy (Dixon and Telles 2017; Monk 2014). Such judgments influence the nature of social interactions with in- and out-group members, and subsequently, exposures to chronic and discrimination-related stressors.
Lastly, health behaviors may undergird the relationship between skin color and BMI. Expectations and roles stemming from hegemonic notions of masculinity and femininity has led to the unequal distribution of unhealthy behaviors by gender. For example, men are more likely than women to engage in behaviors linked to both unhealthy weight (e.g., alcohol use, cigarette smoking, limited attention to diet) and healthy weight (e.g., physical activity) because fulfilling expectations of hegemonic masculinity requires displays of risky behaviors and physical strength (Courtenay 2000; Gilbert et al. 2016). Women, conversely, tend to engage in healthier behaviors because social constructions of beauty place harsher social and economic penalties on women who do not fit ideal body types or beauty standards (Fikkan and Rothblum 2011; Hamermesh 2011). One exception is physical activity, of which women are less likely to engage because constraints surrounding work and family roles disproportionately restrict women’s leisure time (Bird and Rieker 2008). Prior scholarship supports the possibility that perceptions of masculinity/femininity and, therefore expected roles and behaviors, vary by skin color. Men and women of darker brown skin, for example, are coded as more masculine compared to their light-skinned counterparts. Conversely, those with lighter brown skin are considered more feminine (Dixon and Telles 2017; Hall 1995). The intersections of skin color and gender may therefore create different social contexts within which healthy behaviors vary.
Present Study
The extent to which skin color intersects with gender to shape age-trajectories of BMI among African American adults remains unknown. Also unclear is whether sociodemographic, psychosocial, and behavioral factors account for these relationships. The present study aims to fill these crucial gaps by investigating skin color-gender variations in the age-patterning of BMI among African Americans aged 32–55. Informed by health disparities research and colorism, intersectionality, and life course perspectives, the following hypotheses are proposed:
Hypothesis #1: skin color will significantly predict BMI among African Americans such that those with darker skin will exhibit higher BMIs than their light-skinned counterparts.
- Hypothesis #2: the skin color-BMI relationship will be contingent on gender and age.
- Hypothesis #2a: Dark-skinned women will experience the highest BMIs compared to all other skin color-gender groups and the magnitude of skin color disparities in BMI will be larger among women.
- Hypothesis #2b: BMI disparities by skin color will widen with age, consistent with the cumulative disadvantage hypothesis.
Hypothesis 3: sociodemographic characteristics, stressors, and health behaviors will account for skin color-gender differences in BMI.
DATA AND METHODS
Data
This study used four waves of panel data from the Coronary Artery Risk Development in Young Adults (CARDIA) Study, a representative sample of black and white young adults living in four US cities: Birmingham, AL; Minneapolis, MN; Chicago, IL; and Oakland, CA. In Birmingham, Chicago, and Minneapolis, participants were recruited by random-digit dialing from total communities or specific census tracts. In Oakland, participants were randomly selected from a membership roster of a health-care plan. Participants were selected from each site so there would be approximately equal amounts of individuals in each gender (men/women), age (<25 and >=25), race (white/black), and education (<=high school education and > high school education) subgroup. Baseline interviews were conducted in 1985/86 when respondents were 18–30 years old (N=5,115). Follow-up interviews were conducted at seven additional timepoints across a 25-year span. Response rates ranged from 72–90% across the eight waves of data. For further information about the design of the CARDIA Study, see Friedman et al. (1988).
Given the variables of interest, all analyses were restricted to information from Years 15 (2000–2001), 20 (2005–2006), and 25 (2010–2011) except skin color, which was measured in Year 7 of the study (1992–1993). The analytic sample consisted of participants who self-identified as African American or black and were not missing on the skin color measure (N=1,592). While response rates for African Americans in Year 15 were lower compared to prior years (about 65%), supplemental analyses (available upon request) indicated that African American respondents who left the study prior to Year 15 did not differ significantly from those who remained in terms of objective measures of health and physician diagnosed chronic conditions. Those who attrited, however, were less likely than those who remained in the study to have a college degree and had slightly lower average incomes. Overall, the sociodemographic and health profile of the analytic sample was similar to that of the original CARDIA sample. It is also important to note that nativity status was unknown, as there was no available information on respondents’ birthplace. While studies have documented lower levels of obesity among black immigrants compared to their US-born counterparts (Goel et al. 2004), foreign-born blacks made up less than 5% of the US black population from 1980–1990 (Anderson 2015), reducing potential biases attributable to immigration processes.
Dependent Variable
The outcome of interest was BMI. Respondent height and weight were measured at each wave of the study. BMI was computed by the standard equation:
To minimize bias, women who were pregnant at a particular observation were treated as missing for that observation only.
Independent Variables
Main predictors.
Three binary variables measured skin tone among African Americans: light (yes=1), medium (yes=1), and dark (yes=1). Skin tone was assessed in Year 7 with a Photovolt 577 reflectance meter. Values of these meter readings indicated the percentage of reflected light from the upper arm. Lower values (low reflectance) indicated darker skin and higher values (high reflectance) indicated lighter skin. Skin tone categories were based on the 25th and 75th percentiles of the observed reflectance distribution among the African American sample (range=7.1–51.2). Respondents with values above the 75th percentile were considered “light” (ref. group), respondents with values between the 25th and 75th percentiles were considered “medium”, and respondents with values below the 25th percentile were considered “dark”. These cut points were used to discern distinctive skin tone groups, particularly at the extreme ends of the skin color spectrum, and accurately capture how individuals may be viewed in the social world. Findings, however, were robust to alternative constructions of skin color categories (see online Appendix A). Age was measured in years and centered at age 32, and gender was assessed with a dummy variable (0=men; 1=women). Men were the reference group.
Mechanisms.
Three sociodemographic characteristics were considered. Education was measured with self-reports of: 1) the highest degree earned; and 2) the highest grade of school completed in years (0–20+). This information was used to create three dummy variables: high school education or less (ref. group; yes=1), more than high school/some college (yes=1), and college or more (yes=1). Respondents’ combined family income was assessed with an ordinal variable that was treated as continuous (Sweet et al. 2007): 1=$24,999 or less; 2=$25,000–49,999; 3=$50,000–74,999; 4=$75,000–99,999; 5=$100,000 or more. Marital status was measured by a dummy variable in which individuals who were married/living in a marriage-like relationship (1=yes) were compared to those who were not married.
Beginning in Year 15, participants were asked about chronic strains (lasting for more than 6 months) in four domains of life: health of close others, work, finances, and relationships. Response categories were recoded to 0 “no;” 1 “yes, but not very stressful;” 2 “yes, moderately stressful;” and 3 “yes, very stressful”, and averaged across the four domains (range=0–3). CARDIA collected information on discrimination in Years 15 and 25. Participants were asked whether they had experienced discrimination, been prevented from doing something, or been hassled or made to feel inferior in any of the following situations because of their race or color: at school, getting a job, getting housing, at work, at home, getting medical care, or on the street or in a public setting. Responses categories included: 0 “never;” 1 “rarely;” 2 “sometimes;” or 3 “often.” Racial or color discrimination was measured as the average of these seven experiences (α=.79 and .81 in Years 15 and 25, respectively), resulting in a range of 0–3. Measures of discrimination in Year 20 were imputed by averaging discrimination values from Years 15 and 25, specific to each skin color-gender group. Supplemental analyses indicated that results were robust to alternative imputation approaches (see online Appendix B).
Four health behaviors were also considered. Heavy alcohol use was defined as having more than 14 drinks in a week for men and more than 7 drinks for women. Smoking status was measured with three dummy variables in which current regular cigarette smokers (1=yes) and former regular smokers (1=yes) were compared to those who never smoked cigarettes regularly (1=yes). Fast food consumption was assessed as the number of times a week the respondent consumed fast food (range=0–21). Lastly, physical activity was measured by 8 intense and 5 moderate self-reported physical activities within the past year. For each activity, a score was computed using the following equation:
Intensity was defined as the number of kilocalories expended in one minute of a specific activity (Jacobs et al. 1989) and frequency of each activity was predefined in the questionnaire. Scores for each activity were then summed, resulting in a total physical activity score expressed in exercise units (see online Appendix C for more details on the physical activity measure). Given the large values of this measure, the final variable was divided by 100. All proposed mechanisms were time-varying.
Controls.
All models controlled for two measures of attrition: the number of waves a respondent was not interviewed across Years 15–25 due to dropout and whether the respondent died (1=yes) at any point across the three waves.
Analytic Strategy
Growth curve models estimated within a mixed model framework were used to examine inequalities in individual BMI trajectories from ages 32–55. Growth curve models estimated person-specific intercepts (BMI at age 32) and slopes (rates of change with age) that described intra-individual patterns of change in health as a function of age (Raudenbush and Bryk 2002). Both fixed effects of covariates and random effects for the intercept and age slope were included in each model. Estimating random effects for the intercept and slope accounted for person-specific errors (or subject-specific deviations), which represented unobserved differences between individuals that were stable over time and not accounted for by the covariates. Among the random effects, repeated observations (Level 1) were nested within respondents (Level 2). Comparisons of likelihood ratio tests indicated a linear growth curve with random intercepts and linear slopes provided the best fit to the data. All models were stratified by gender, and coefficients for skin tone and each explanatory variable were regressed on the intercepts and linear age slopes.
Maximum likelihood estimation was used to handle missing data on the outcome (Raudenbush and Bryk 2002). This approach allowed respondents who had at least one valid BMI measure between Years 15–25 to be incorporated in the analysis. Listwise deletion was used to handle missing data on the predictors.
Testing of hypotheses.
Growth curve models were used to test Hypothesis 1. Significant coefficients for skin color on the intercept and/or age slopes suggested that skin color helps shape BMI trajectories. Chow tests, which evaluated whether the coefficients for skin color were statistically different for men and women, were used to formally test Hypothesis 2a. Significant Chow tests for the skin color coefficients provided evidence that the association between skin color and BMI varied by gender. Non-significant Chow tests suggested that the skin color disparity in BMI was similar across genders.
The life course hypotheses were tested by regressing skin tone on the linear age slopes. Given the age slopes were positive or non-significant, the cumulative disadvantage hypothesis (#2b above) was supported if results indicated BMI inequalities widened with age (significant positive coefficient for skin color on the age slopes). Conversely, the aging-as-leveler hypothesis was supported if results indicated BMI inequalities narrowed with age (significant negative skin color × age interaction) while the persistent inequality hypothesis was supported if age slopes were similar across groups (non-significant skin color × age interaction). Lastly, a stepwise modeling approach was used to evaluate the extent to which the proposed explanatory factors accounted for skin color disparities in BMI (Hypothesis 3). A smaller skin color coefficient in subsequent models compared to the skin color coefficient in the base model, in tandem with statistically significant coefficients for the proposed mechanism, provided evidence that the mechanism under consideration helped explain BMI disparities.
RESULTS
Table 1 presents means and proportions of the study variables at Year 15, stratified by skin color and gender. Compared to men, women tend to have higher levels of BMI and lower levels of income and marriage. Women also report more chronic burdens than men and are less likely to heavily consume alcohol, smoke cigarettes, engage in physical activity, or eat fast food. Moreover, several differences by skin color within gender are evident. Compared to light-skinned women, women with dark skin have a higher BMI, and women with medium and dark brown skin have lower levels of education and income. Additionally, medium-skinned women report fewer chronic burdens than their light- and dark-skinned counterparts. Among men, those of medium and dark brown skin have lower levels of education and report fewer experiences of discrimination than light-skinned men. Dark-skinned men are more likely to have lower levels of income and be current cigarette smokers compared to light-skinned men.
Table 1.
Means and Proportions of Study Variables at Year 15 of the CARDIA Study (2000–2001), by Gender and Skin Color
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Light | Medium | Dark | Total | Light | Medium | Dark | Total | |
| BMI | 30.534* | 30.952*† | 34.809*† | 31.558 | 28.884 | 28.868† | 29.402† | 29.052* |
| Sociodemographic Characteristics | ||||||||
| High School or Less | .241* | .265*† | .304*† | .266 | .279 | .360† | .429† | .369* |
| Some College | .412* | .460*† | .494*† | .452 | .365 | .409† | .364† | .386* |
| College or More | .347* | .275*† | .202†* | .282 | .356 | .231† | .207† | .245* |
| Income | 2.624* | 2.353*† | 2.266†* | 2.416 | 2.962 | 2.733† | 2.414† | 2.666* |
| Married | .473* | .467*† | .437*† | .463 | .567 | .601† | .485† | .556* |
| Stressors | ||||||||
| Chronic Burdens | .956* | .843†* | .994*† | .905 | .817 | .784† | .809† | .799* |
| Racial/Color Discrimination | .608* | .595*† | .652*† | .609 | .762 | .640† | .611† | .652* |
| Health Behaviors | ||||||||
| Heavy Alcohol Use | .065* | .079*† | .076*† | .074 | .106 | .142† | .141† | .136* |
| Never Smoked | .633* | .594*† | .620*† | .610 | .606 | .598† | .515† | .571* |
| Former Smoker | .147* | .139*† | .101*† | .134 | .115 | .100† | .101† | .103* |
| Current Smoker | .216* | .254*† | .278*† | .248 | .269 | .299† | .374† | .319* |
| Physical Activity | 2.431* | 2.246*† | 2.285*† | 2.308 | 4.251 | 4.215† | 4.167† | 4.205* |
| Fast Food Consumption | 3.076* | 3.214*† | 2.678*† | 3.068 | 3.340 | 3.259† | 3.726† | 3.434* |
| Controls | ||||||||
| Age | 40.073* | 39.769*† | 39.462*† | 39.800 | 40.163 | 39.388† | 39.566† | 39.587* |
| Number of Waves Missing | .306* | .309*† | .323*† | .311 | .462 | .498† | .439† | .472* |
| Died During Study Period | .016* | .021*† | .019*† | .019 | .038 | .043† | .056† | .046* |
| N | 245* | 433*† | 158*† | 836 | 104 | 281† | 198† | 583* |
p<.05 significant difference between men and women of same skin tone
p<.05 significant difference among skin tones within gender (ref=light skin tone)
Table 2 presents results from growth curve models of BMI between ages 32 and 55. Model 1 estimates skin color disparities in BMI trajectories. The significant positive coefficient for dark skin on the BMI intercept among women (3.850) indicates that dark-skinned women have an almost 4-point higher BMI at age 32 than light-skinned women (intercept=29.388), providing support for Hypothesis 1. Given that the BMI threshold for obesity is 30, results suggest that on average, light-and medium-skinned women tend to be overweight (BMI of 29) while dark-skinned women tend to be obese (BMI of 33) at age 32. Additionally, the small (approximately 1 BMI point), non-significant coefficients for medium and dark skin on the intercept among men in tandem with the significant Chow tests for the intercept and dark skin coefficient suggests that all women, regardless of skin color, have higher BMIs than men. Furthermore, the magnitude of the dark-light disparity in BMI at age 32 is greater among women than men, supporting Hypothesis 2a.
Table 2.
Growth Curve Models of Skin Color, Gender, Sociodemographic Characteristics, Stressors, and Health Behaviors on BMI Trajectories; CARDIA Study; Years 15–25
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed Effects | Women | Men | m≠wa | Women | Men | m≠w | Women | Men | m≠w | Women | Men | m≠w | Women | Men | m≠w |
| Intercept | 29.388*** (.571) | 27.279*** (.619) | † | 29.180*** (.786) | 26.441*** (.761) | † | 29.419*** (.574) | 27.243*** (.627) | † | 29.730*** (.637) | 28.308*** (.675) | 29.770*** (.844) | 27.869*** (.824) | ||
| Skin Color (ref. Light) | |||||||||||||||
| Medium | .139 (.696) | 1.038 (.697) | .109 (.696) | .891 (.693) | .160 (.697) | 1.059 (.699) | .277 (.692) | 1.094 (.686) | .243 (.691) | .921 (.684) | |||||
| Dark | 3.850*** (.880) | 1.091 (.733) | † | 3.799*** (.881) | 1.119 (.732) | † | 3.892*** (.881) | 1.121 (.737) | † | 4.088*** (.874) | 1.280 (.723) | † | 4.040*** (.875) | 1.259 (.722) | † |
| Sociodemographic Characteristics | |||||||||||||||
| Some College (ref.<=HS) | −.177 (.481) | .035 (.400) | −.372 (.476) | .111 (.403) | |||||||||||
| College or More (ref.<=HS) | −1.028** (.654) | −1.064* (.517) | −1.366* (.666) | −1.275* (.525) | |||||||||||
| Income | .094 (.194) | .220 (.148) | .088 (.192) | .128 (.150) | |||||||||||
| Married | .863* (.423) | .992** (.357) | .914* (.414) | .969** (.356) | |||||||||||
| Stressors | |||||||||||||||
| Chronic Burdens | −.119 (.285) | −.162 (.251) | −.112 (.282) | −.042 (.250) | |||||||||||
| Race/color Discrimination | .468 (.408) | .053 (.339) | .556 (.410) | .116 (.333) | |||||||||||
| Health Behaviors | |||||||||||||||
| Heavy Alcohol Use | −.331 (.804) | −.485 (.486) | −.308 (.804) | −.558 (.485) | |||||||||||
| Current Smoker (ref. Never) | −.273 (.579) | −.925* (.419) | −.287 (.592) | −1.081* (.438) | |||||||||||
| Former Smoker (ref. Never) | 1.344* (.628) | −.644 (.570) | † | 1.349* (.628) | .966 (.573) | † | |||||||||
| Physical Activity | −.162 (.085) | −.155** (.049) | −.162 (.085) | −.154** (.049) | |||||||||||
| Fast Food Consumption | −.035 (.047) | .003 (.037) | −.038 (.047) | −.001 (.037) | |||||||||||
| Attrition: | |||||||||||||||
| Non–response | −.273 (.687) | −.282 (.459) | −.356 (.685) | −.237 (.458) | −.296 (.688) | −.281 (.460) | −.245 (.680) | −.212 (.453) | −.370 (.679) | −.267 (.451) | |||||
| Death | −.377 (2.973) | −.487 (1.639) | −.118 (2.965) | −.228 (1.630) | −.415 (2.975) | −.479 (1.640) | .085 (2.937) | −.568 (1.616) | .299 (2.930) | −.354 (1.607) | |||||
| Linear Slope (Age) | .166*** (.028) | .199*** (.030) | .155*** (.045) | .192*** (.043) | .163*** (.028) | .201*** (.030) | .183*** (.034) | .159*** (.036) | .155*** (.049) | .136*** (.049) | |||||
| Skin Color (ref. Light) | |||||||||||||||
| Medium | .014 (.035) | −.104** (.034) | † | .016 (.035) | −.089* (.035) | † | .012 (.035) | −.105** (.035) | † | −.001 (.034) | −.107** (.034) | † | .000 (.034) | −.091** (.034) | |
| Dark | −.033 (.044) | −.052 (.036) | −.029 (.044) | −.044 (.037) | −.035 (.044) | −.053 (.036) | −.050 (.043) | −.061 (.036) | −.045 (.043) | −.052 (.036) | |||||
| Sociodemographic Characteristics | |||||||||||||||
| Some College (ref.<=HS) | .030 (.034) | .037 (.028) | .043 (.034) | .004 (.028) | |||||||||||
| College or More (ref.<=HS) | .045 (.042) | .083* (.035) | .066 (.042) | .089 (.034) | |||||||||||
| Income | .002 (.013) | −.003 (.010) | .002 (.013) | .002 (.010) | |||||||||||
| Married | −.048 (.031) | −.046 (.026) | −.055 (.030) | −.046 (.026) | |||||||||||
| Stressors | |||||||||||||||
| Chronic Burdens | .005 (.022) | .012 (.020) | .003 (.022) | .008 (.019) | |||||||||||
| Race/color Discrimination | −.054* (.027) | .000 (.022) | −.059* (.027) | −.009 (.022) | |||||||||||
| Health Behaviors | |||||||||||||||
| Heavy Alcohol Use | .002 (.055) | −.023 (.036) | .003 (.055) | −.015 (.035) | |||||||||||
| Current Smoker (ref. Never) | −.087* (.037) | .002 (.029) | −.087* (.038) | .020 (.030) | |||||||||||
| Former Smoker (ref. Never) | −.041 (.039) | .038 (.035) | −.039 (.039) | .059 (.036) | |||||||||||
| Physical Activity | −.006 (.006) | .005 (.004) | −.006 (.006) | .005 (.004) | |||||||||||
| Fast Food Consumption | .009* (.004) | .003 (.003) | .009* (.004) | .003 (.003) | |||||||||||
| Attrition: | |||||||||||||||
| Non–response | .060 (.045) | .020 (.031) | .065 (.045) | .021 (.031) | .061 (.045) | .020 (.031) | .060 (.044) | .020 (.031) | .067 (.044) | .025 (.031) | |||||
| Death | .190 (.289) | −.164 (.132) | .179 (.288) | −.152 (.131) | .192 (.289) | −.164 (.132) | .137 (.283) | −.139 (.130) | .130 (.282) | −.134 (.130) | |||||
| Random Effects | |||||||||||||||
| Level 1 Residual | 2.009*** (.066) | 1.370*** (.052) | 2.015*** (.067) | 1.358*** (.052) | 2.007*** (.066) | 1.369*** (.053) | 1.968*** (.066) | 1.356*** (.052) | 1.969*** (.067) | 1.346*** (.052) | |||||
| Level 2 Age | .275*** (.019) | .176*** (.015) | .270*** (.020) | .175*** (.015) | .274*** (.019) | .175*** (.016) | .266*** (.019) | .173*** (.015) | .259*** (.020) | .170*** (.015) | |||||
| Level 2 Intercept | 7.709*** (.252) | 5.389*** (.199) | 7.649*** (.255) | 5.322*** (.198) | 7.719*** (.253) | 5.396*** (.200) | 7.677*** (.255) | 5.278*** (.198) | 7.628*** (.255) | 5.212*** (.197) | |||||
| −2 Log Likelihood | 12509 | 7462 | 12496 | 7435 | 12504 | 7461 | 12419 | 7417 | 12398 | 7391 | |||||
| N | 936 | 656 | 936 | 656 | 936 | 656 | 936 | 656 | 936 | 656 | |||||
’m≠w’ indicates Chow tests for differences between men and women
p<.05,
p<.01,
p<.001
p<.05 significant difference in coefficients for men and women
The significant positive coefficients for age among women and men (.166 and .199, respectively) and non-significant Chow test suggest that BMI increases similarly with age regardless of gender. The magnitude of the age coefficients indicates about a four-point increase in BMI across ages 32–55, placing the average BMI for all skin color-gender groups, except medium-skinned men, in the obese category by the mid- to late–40s. The non-significant coefficient for dark skin on the age slope among women suggests that the dark-light BMI disparity remains stable between ages 32–55, consistent with the persistent inequality hypothesis and in contrast with Hypothesis 2b. Among men, while there are no significant skin color differences in BMI at age 32, there is a significant interaction between medium skin and age. The small negative coefficient for medium skin on the age slope (–.104) suggests that medium-skinned men gain weight less quickly with age compared to their light- and dark-skinned counterparts. Consequently, a BMI gap between medium- and light/dark-skinned men emerges and slightly widens between ages 32 and 55, providing support for Hypothesis #2b (cumulative disadvantage). There is ultimately a two-point BMI difference among men by age 55. These findings also provide partial support for Hypothesis 1 given that skin color influences the age slopes among men, but in an unexpected direction.
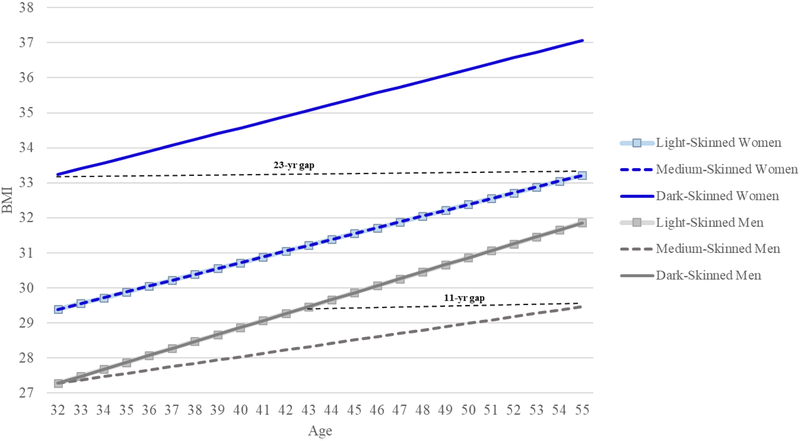
Figure 1 plots the results from Model 1 and compares the average ages when skin color-gender subgroups experience comparable levels of BMI. As Figure 1 illustrates, dark-skinned women have the BMI of lighter-skinned women 23 years later. Said differently, a 32–year old dark-skinned woman has the BMI profile of a 55–year old light- or medium-skinned woman. Additionally, a 43–year old light- or dark-skinned man has the BMI of a medium-skinned man who is more than 10 years older. Moreover, dark-skinned women have, on average, a 4–point higher BMI than their female counterparts, and a 5– or 8–point higher BMI than men.
Figure 1.
Trajectories of BMI by Skin Color and Gender across Ages 32–55, CARDIA Study (N=1,592)
Note: Figure 1 is based on results from Model 1 of Table 2.
Model 2 adds education, income, and marital status to Model 1. Among women, none of the sociodemographic factors explain the initial and stable disadvantages of dark-skinned women compared to their lighter-skinned counterparts. Among men, the significant coefficient for college education or more on the age slope reduces the medium skin × age interaction to –.089, accounting for approximately 14% of the diverging BMI trajectories between medium- and non-medium skinned men. Model 3 regresses chronic and discrimination-related stressors on the intercept and age slopes, showing that neither chronic burdens nor racial/color discrimination are associated with BMI for women and men across ages 32–55. Results from Model 4, which add health behaviors to the base model, indicate that while some behaviors directly affect weight gain, none help explain the stable skin color differences in BMI among women, nor the small, emerging BMI gap between medium- and light/dark-skinned men.
Results from Model 5 (the full model) indicate that the stable BMI disadvantages of dark-skinned women relative to lighter-skinned women, as well as the diverging BMI trajectories between medium- and light/dark-skinned men, are not explained by the proposed mechanisms. The coefficients for dark skin on the intercept among women (4.040) and for medium skin on the age slope among men (–.091) remain statistically significant. Comparing these coefficients to results from Model 1, the dark-light BMI disparity among women increases by approximately 5% when accounting for sociodemographic characteristics, stressors, and health behaviors. Furthermore, about 13% of the diverging BMI trajectory between medium- and light-/dark-skinned men is accounted for by education. Overall, these findings are in contrast to the expectation provided by Hypothesis 3.
DISCUSSION
This study is among first to document the extent to which skin color intersects with gender to shape age-trajectories of BMI across adulthood. Prior studies have used cross-sectional data to examine the independent effects of skin color and other social statuses on specific health outcomes, none of which included BMI. Much of this older research produced mixed findings and did not consider how simultaneously-experienced social statuses might jointly combine to affect the age-patterning of health. Results from this study therefore advance our understanding of the complex and dynamic nature of health inequality across the life course in several ways.
Summary of Findings
First, findings indicated that skin color significantly shaped BMI trajectories across adulthood and that the skin color-BMI relationship was gendered. Skin color differences in BMI were larger among women than men across ages 32–55. Dark-skinned women, furthermore, had the highest BMI between early adulthood and mid-life compared to all other skin color-gender groups. These stark health disadvantages of dark-skinned women are likely a result of the consequences stemming from intersections between skin color and gender. While prior work has proposed several explanations for the gendered consequences of skin color (e.g., mate selection), why/how dark skin exerts a particularly harsh penalty for African American women may be best understood within the context of interlocking systems of inequality.
For example, perceived attractiveness is a critical component of socioeconomic success for women of all races living in a patriarchal society (Anderson et al. 2010). Beauty is an attribute of women that is evaluated and linked to life chances in a similar manner to which other characteristics (intelligence, political influence) are evaluated and related to life chances among men (Hamermesh 2011; Lakoff and Scherr 1984). As a result, beauty—of which fair skin is one indicator—acts as a form of capital that women, who tend to be socioeconomically and politically disadvantaged relative to men, can use to acquire socioeconomic resources beneficial for health (Hunter 2007). In the context of skin color stratification, the gendered experiences of colorism likely make access to and opportunities for good health particularly difficult for dark-skinned women compared to other skin color-gender groups. That is, the location of dark-skinned women in the social structure (occupying subordinate positions in both the color and gender hierarchies) may be linked to stronger barriers to socioeconomic achievement and increased exposure to stressors relative to lighter-skinned women (who occupy subordinate positions in the gender hierarchy yet dominant positions in the color hierarchy) and African American men (who occupy dominant and varied positions in gender and color hierarchies, respectively).
Results also indicated that the dark-light disparity in BMI among women remained stable with age, providing support for the persistent inequality hypothesis. The medium-light/dark disparity among men, however, widened with age, consistent with the cumulative disadvantage hypothesis. The widening BMI gap resulted from medium-skinned men gaining weight at a slightly slower rate than light- and dark-skinned men, suggesting potential advantages associated with medium brown skin among men that translate into reduced risks for weight gain. One possibility is that having a medium brown complexion affords men a type of protection against negative experiences relevant for BMI. The intersections of skin color and gender, for example, create notions of danger and criminality among dark-skinned men (Gilbert et al. 2016), and inauthenticity and femininity among light-skinned men (Hall 1995). Having a skin tone that is not at the extremes, but rather represents the “prototypic” black phenotype, may exempt medium skin men from the disadvantages and stigmas associated light- or dark-skin, particularly when interacting with other African Americans (Celious and Oyserman 2001). This, in turn, may protect medium-skinned men from stressors and experiences of discrimination—several of which may not be measured here—that are linked to weight gain. While the data used here preclude examining these possibilities, future research should explore how the racial composition of neighborhoods and schools as well as social interactions with in-group versus out-group members may differentiate the health consequences of skin color.
It is important to note that the age-patterning of BMI may reflect, in part, the effects of birth cohort or sociohistorical period. CARDIA respondents were born between 1955 and 1968. Older cohorts were exposed to de facto and de jure segregation for longer periods of time and, conversely, had fewer opportunities to benefit from several transformative historical events (e.g., the Civil Rights Act in 1964). These varying social contexts may have conferred differential cumulative exposure to risk and protective factors across the life course. Similarly, CARDIA respondents were entering different stages of adulthood when the “obesity epidemic” began, further differentiating risks for weight gain. While sensitivity analyses (not shown) indicated results were robust to controlling for cohort, year of measurement, and interactions between age and cohort/period, future research should continue to explore the interrelated consequences of age, period, and cohort in the context of the obesity epidemic.
This study also extends previous literature by examining the extent to which sociodemographic, psychosocial, and behavioral factors explain skin color differences in BMI trajectories. Findings indicated that these factors did not account for skin color disparities in BMI among women or men. Several sociodemographic factors have similarly been shown to have limited relationships with health among African Americans (Cobb et al. 2016; Hargrove 2018; Monk 2015). Scholars have cited the measurement of some socioeconomic resources and differences in the meaning of SES as reasons for these modest associations (Kaufman, Cooper, and McGee 1997; Williams and Mohammed 2013). For example, measures of income do not adjust for differences in purchasing power, stability of funds, and consequently, the availability of funds for health-related resources. Commonly-measured socioeconomic characteristics also do not account for a host of deleterious conditions that accompany and likely differentiate the health benefits of resources (Krieger et al. 1993). Future research should consider alternative indicators of socioeconomic position that may better capture individuals’ health relevant contexts, such as wealth, perceptions of social deprivation, and neighborhood-level socioeconomic (dis)advantage.
Other studies have also found that perceived racial discrimination is not directly related to physiological markers of health among African Americans (Chae et al. 2010; Fuller-Rowell, Doan, and Eccles 2012). Scholars have proposed various explanations for these non-significant relationships, including differential reporting of stressors/discrimination by health status; internalized racism as a moderator of the discrimination-health relationship; and the acknowledgment of discrimination serving as a protective mechanism. Another possibility is, given that systems of inequality are not experienced equally by African Americans, chronic and discrimination-related stressors specific to skin color and age statuses play a larger role in shaping health during young and middle adulthood. For example, a recent indicated that discrimination based on skin color is disproportionately experienced by dark- and light-skinned African Americans when such behaviors are enacted by other African Americans (Monk 2015). While the gendered and colored nature of racial discrimination has been documented (Collins 2015; Keith et al. 2017; Wingfield 2007), most commonly-used survey measures of discrimination do not reflect such intersectional experiences (Harnois and Ifatunji 2011). Moreover, additional factors such as racial identity, sense of belonging, and internalized racism may be more salient in shaping health inequalities along skin color lines (Cobb et al. 2016; Monk 2015). Future work should consider not only the unique lived experiences among racial groups, but also explicitly examine the role of a more comprehensive set of theoretically-important structural and psychosocial factors. Relatedly, other aspects of physical appearance, including body shape, further intersect with presumed race and gender to shape individuals’ appraisals and responses to others. While beyond the scope of the present study, future research should explore how multiple aspects of physical appearance are differentially consequential for health.
In addition to the social pathways described above, unmeasured biological mechanisms may play a role in generating BMI disparities (Björntorp 2001; Yau and Potenza 2014). For example, when stressors are experienced, the brain outputs stress mediators that affect multiple bodily systems (McEwen 2009). Glucocorticoids are a major stress hormone the body releases and are responsible for fat deposition, adipose tissue accumulation, and inflammation. Prolonged exposure to stressors and the subsequent chronic activation of these stress responses can lead to metabolic dysregulations that influence weight gain, including the promotion of fat storage and increased appetite via leptin resistance (Lee et al. 2014; McEwen 2009). To the extent that chronic stressors are unequally distributed by skin color, it is possible that biological mechanisms contribute to health differences among African Americans. Future research on this topic is needed.
Limitations
This study is not without limitations. First, the data used are not nationally representative and findings cannot be unequivocally generalized to the overall African American population. However, not only were CARDIA participants sampled from geographically diverse areas, but the health statuses of CARDIA respondents at baseline were similar to those of African American participants in national datasets collected around the same time (Friedman et al. 1988). Thus, findings from this study likely reflect, at least in part, relationships between skin color and BMI among the broader African American population.
Second, because BMI calculations do not account for muscle and bone mass, overweight/obese statuses may be overestimated. Evidence also suggests that those measured as overweight by BMI standards experience similar or increased rates of survival and cardiovascular health compared to those measured as normal weight (McGee et al. 2005; Romero-Corrak et al. 2006). While the present study is less concerned with categorizing individuals into weight classes, other measures of adiposity may be useful for delineating weight groups and assessing the health implications of overweight/obesity statuses.
Third, the present study cannot evaluate whether skin color disparities in BMI vary by nativity and ethnicity because such information was not collected in the CARDIA Study. Prior research has shown that US-born African Americans have poorer health, including higher BMIs, than their US- and foreign-born counterparts from African or Caribbean countries (Goel et al. 2004; Hamilton and Hummer 2011). Given variations in racial and color hierarchies in the US and African diasporic nations, it is possible that perceptions of discrimination and the discrimination-health relationship may differ based on place of origin and ethnic identification (Ryan, Gee, and Laflamme 2006; Viruell-Fuentes, Miranda, and Abdulrahim 2012). When possible, future studies should consider how ethnicity and nativity combine with skin color to shape pathways to health.
A fourth limitation is the measurement of skin color, which lacks the subjective and arbitrary nature of social appraisals and judgments made by others in society (Maddox 2004). Information on self-perceptions of skin shade is also not available, precluding the possibility of examining the effects of self-identification on BMI trajectories. It is likely that subjective and objective indicators of skin shade are differentially consequential for health, as they reflect unique aspects of skin color stratification. For example, self-ratings of skin tone are argued to be shaped by relational processes and dynamics of power (Monk 2015). They may therefore be more useful for evaluating the health consequences of an individual’s personal or social identity that stems from their placement in the social structure. Conversely, interviewer-rated skin color may be better suited to assess how individuals are understood and treated by others. Objective measures of skin shade, however, are important, and at times preferable, indicators of color. These measurements allow for comparability across studies and populations, and reduce biases and use of non-relevant information inherent in interviewer ratings of skin color (Hill 2002b).
Conclusion
Despite these limitations, findings suggest skin color plays an important role in shaping BMI trajectories among African Americans between young adulthood and middle age. The age-patterning of BMI likely reflects broader social forces that afford unique dis(advantages) to African Americans on the basis of both skin color and gender—social forces that are not completely captured by traditional measures of sociodemographic characteristics, stressors, and health behaviors. Indeed, commonly-measured health relevant factors do not account for the heterogeneity of lived experiences and opportunities for healthy living among the African American population. Treating African Americans as a monolith runs the risk of mis-specifying structural and stress processes that undergird and shape the nature of health inequalities across the life course. Scholars interested in explaining health inequalities may need to rethink the applicability of existing measurements of SES and stressors for characterizing and influencing the lives of individuals located at different intersections of racial, color, and gender hierarchies.
Supplementary Material
ACKNOWLEDGMENTS
I would like to thank Tyson Brown, Bob Hummer, and Erika Leslie for their helpful comments on several drafts of this article.
Biography
Taylor W. Hargrove is an assistant professor in the Department of Sociology at the University of North Carolina at Chapel Hill. She is also a faculty fellow at the Carolina Population Center. Her research seeks to uncover and explain the development of health disparities across the life course, focusing on the consequences of race/ethnicity, skin color, gender, and social class. She is currently engaged in research that explores how neighborhood contexts shape linkages among individual-level characteristics and biological measures of health in early adulthood.
REFERENCES
- Adams Elizabeth A., Kurtz-Costes Beth E., and Hoffman Adam J.. 2016. “Skin Tone Bias among African Americans: Antecedents and Consequences across the Life Span.” Developmental Review 40:93–116. [Google Scholar]
- Ailshire Jennifer A., and House James S.. 2011. “The Unequal Burden of Weight Gain: An Intersectional Approach to Understanding Social Disparities in BMI Trajectories from 1986 to 2001/2002.” Social Forces 90(2):397–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson Tammy L., Grunert Catherine, Katz Arielle, and Lovascio Samantha. 2010. “Aesthetic Capital: A Research Review on Beauty Perks and Penalties.” Sociology Compass 4(8):564–575. [Google Scholar]
- Bird Chloe, and Rieker Patricia. 2008. Gender and Health: The Effects of Constrained Choices and Social Policies. New York: Cambridge University Press. [Google Scholar]
- Björntorp P 2001. “Do Stress Reactions Cause Abdominal Obesity and Comorbidities?“ Obesity rReviews 2(2):73–86. [DOI] [PubMed] [Google Scholar]
- Bonilla-Silva Eduardo. 2017. Racism without Racists: Color-blind Racism and the Persistence of Racial Inequality in America. Lanham, MD: Rowman & Littlefield. [Google Scholar]
- Borrell Luisa N., Kiefe Catarina I., Willaims David R., Diez-Roux Ana V., and Larsen Penny Gordon. 2006. “Self-Reported Health, Perceived Racial Discrimination, and Skin Color in African Americans in the CARDIA Study.” Social Science & Medicine 63:1415–1427. [DOI] [PubMed] [Google Scholar]
- Edwin Boyle Jr.. 1970. “Biological Pattern in Hypertension by Race, Sex, Body Weight, and Skin Color.” JAMA 213(10):1637–1643. [PubMed] [Google Scholar]
- Brown Tyson H., Richardson Liana J., Hargrove Taylor W., and Thomas Courtney S.. 2016. “Using Multiple-hierarchy Stratification and Life Course Approaches to Understand Health Inequalities: The Intersecting Consequences of Race, Gender, SES, and Age.” Journal of Health and Social Behavior 57(2) 200–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell Mary E., and Troyer Lisa. 2007. “The Implications of Racial Misclassification by Observers.” American Sociological Review 72(5):750–765. [Google Scholar]
- Celious Aaron, and Oyserman Daphna. 2001. Race from the Inside: An Emerging Heterogeneous Race Model. Journal of Social Issues 57(1):149–165. [Google Scholar]
- Chae David H., Lincoln Karen D., Adler Nancy E., and Syme S. Leonard. 2010. “Do Experiences of Racial Discrimination Predict Cardiovascular Disease Among African American Men? The Moderating Role of Internalized Negative Racial Group Attitudes.” Social Science & Medicine 71(6):1182–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb Ryon J., Thomas Courtney S., Laster Pirtle Whitney N., and Darity William A. Jr. 2016. “Self-Identified Race, Socially Assigned Skin Tone, and Adult Physiological Dysregulation: Assessing Multiple Dimensions of “Race” in Health Disparities Research.” Social Science & Medicine 2:595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins Patricia Hill. 2015. “Intersectionality’s Definitional Dilemmas.” Annual Review of Sociology 41:1–20. [Google Scholar]
- Dixon Angela R., and Telles Edward E.. 2017. “Skin Color and Colorism: Global Research, Concepts, and Measurement.” Annual Review of Sociology 43:405–424. [Google Scholar]
- Ferraro Kenneth F. 2016. “Life Course Lens on Aging and Health” Pp. 386–406 in Handbook of the Life Course, edited by Shanahan MJ, Mortimer JT, and Johnson MK. Switzerland: Springer International Publishing. [Google Scholar]
- Ferraro Kenneth F. and Farmer Melissa M.. 1996. “Double Jeopardy to Health Hypothesis for African Americans: Analysis and Critique.” Journal of Health and Social Behavior 37(1):27–43. [PubMed] [Google Scholar]
- Ferraro Kenneth F., Schafer Markus H., and Wilkinson Lindsay R.. 2016. “Childhood Disadvantage and Health Problems in Middle and Later Life: Early Imprints on Physical Health?” American Sociological Review 81(1):107–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fikkan Janna L., and Rothblum Esther D.. 2012. “Is Fat a Feminist Issue? Exploring the Gendered Nature of Weight Bias.” Sex Roles 66(9–10):575–592. [Google Scholar]
- Fuller-Rowell Thomas E., Doan Stacey N., and Eccles Jacquelynne S.. 2012. “Differential Effects of Perceived Discrimination on the Diurnal Cortisol Rhythm of African Americans and Whites.” Psychoneuroendocrinology 37(1):107–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman Gary D., Cutter Gary R., Donahue Richard P., Hughes Glenn H., Hulley Stephen B., Jacobs David R., Liu Kiang, and Savage Peter J.. 1988. “CARDIA: Study Design, Recruitment, and Some Characteristics of the Examined Subjects.” Journal of Clinical Epidemiology 41(11):1105–1116. [DOI] [PubMed] [Google Scholar]
- Gee Gilbert C, and Ford Chandra L.. 2011. “Structural Racism and Health Inequities: Old Issues, New Directions.” DuBois Review: Social Science Research on Race 8(1):115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert Keon L., Ray Rashawn, Siddiqi Arjumand, Shetty Shivan, Baker Elizabeth A., Elder Keith, and Griffith Derek M.. 2016. “Visible and Invisible Trends in Black Men’s Health: Pitfalls and Promises for Addressing Racial, Ethnic, and Gender Inequities in Health.” Annual Review of Public Health 37:295–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel Mita Sanghavi, McCarthy Ellen P., Phillips Russell S., and Wee Christina C.. 2004. “Obesity among US Immigrant Subgroups by Duration of Residence.” JAMA 292(23): 2860–2867. [DOI] [PubMed] [Google Scholar]
- Goldsmith Arthur H., Hamilton Darrick, and Darity William. 2007. “From Dark to Light: Skin Color and Wages among African-Americans.” Journal of Human Resources 42(4):701–738. [Google Scholar]
- Camille Hall J.. 2017. “No Longer Invisible: Understanding the Psychosocial Impact of Skin Color Stratification in the Lives of African American Women.” Health & Social Work 42(2):71–78. [DOI] [PubMed] [Google Scholar]
- Hall Ronald E. 1995. “Dark Skin and the Cultural Ideal of Masculinity.” Journal of African American Men 1(3):37–62. [Google Scholar]
- Hamermesh Daniel S. 2011. Beauty Pays: Why Attractive People Are More Successful. Princeton University Press, 2011. [Google Scholar]
- Hamilton Darrick, Goldsmith Arthur H., and Darity William. 2009. “Shedding “Light” on Marriage: The Influence of Skin Shade on Marriage for Black Females.” Journal of Economic Behavior & Organization 72(1):30–50. [Google Scholar]
- Hamilton Tod G., and Hummer Robert A.. 2011. “Immigration and the Health of US Black Adults: Does Country of Origin Matter?” Social Science & Medicine 73(10): 1551–1560. [DOI] [PubMed] [Google Scholar]
- Harburg Ernest, Gleibermann Lillian, Roeper Peter, Schork M. Anthony, and Schull William J.. 1978. “Skin Color, Ethnicity, and Blood Pressure I: Detroit Blacks.” American Journal of Public Health 68(12):1177–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hargrove Taylor W. 2018. “Intersecting Social Inequalities and Body Mass Index Trajectories from Adolescence to Early Adulthood.” Journal of Health and Social Behavior 59(1):56–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnois Catherine E., and Ifatunji Mosi. 2011. “Gendered Measures, Gendered Models: Toward an Intersectional Analysis of Interpersonal Racial Discrimination.” Ethnic and Racial Studies 34(6):1006–1028. [Google Scholar]
- Hill Mark E. 2002a. “Skin Color and the Perception of Attractiveness among African Americans: Does Gender Make a Difference?” Social Psychology Quarterly 65(1):77–91. [Google Scholar]
- Hill Mark E. 2002b. “Race of the Interviewer and Perception of Skin Color: Evidence from the Multi-City Study of Urban Inequality.” American Sociological Review 67(1):99–108. [Google Scholar]
- Hruby Adela, Manson JoAnn E., Qi Lu, Malik Vasanti S., Rimm Eric B., Sun Qi, Willett Walter C., and Hu Frank B.. 2016. “Determinants and Consequences of Obesity.” American Journal of Public Health 106(9):1656–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter Margaret. 2007. “The Persistent Problem of Colorism: Skin Tone, Status, and Inequality.” Sociology Compass 1(1): 237–254. [Google Scholar]
- Jacobs David R. Jr, Hahn Lorraine P., Haskell William L., Pirie Phyllis, and Sidney Stephen. 1989. “Validity and Reliability of Short Physical Activity History: CARDIA and the Minnesota Heart Health Program.” Journal of Cardiopulmonary Rehabilitation 9(11): 448–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman Jay S., Cooper Richard S., and McGee Daniel L.. 1997. “Socioeconomic Status and Health in Blacks and Whites: The Problem of Residual Confounding and the Resiliency of Race.” Epidemiology 8(6):621–628. [PubMed] [Google Scholar]
- Keith Verna M., and Herring Cedric. 1991. “Skin Tone and Stratification in the Black Community.” American Journal of Sociology 97(3): 760–768. [Google Scholar]
- Keith Verna M., Nguyen Ann W., Robert Joseph Taylor Dawne M. Mouzon, and Chatters Linda M.. 2017. “Microaggressions, Discrimination, and Phenotype among African Americans: A Latent Class Analysis of the Impact of Skin Tone and BMI.” Sociological Inquiry 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klag Michael J., Whelton Paul K., Coresh Josef, Grim Clarence E., and Kuller Lewis H.. 1991. “The Association of Skin Color with Blood Pressure in US Blacks With Low Socioeconomic Status.” Journal of American Medical Association 265(5):599–602. [PubMed] [Google Scholar]
- Krieger Nancy, Rowley Diane L., Herman Allen A., and Avery Byllye. 1993. “Racism, Sexism, and Social Class: Implications for Studies of Health, Disease, and Well-Being.” American Journal of Preventive Medicine 9(6):82–122. [PubMed] [Google Scholar]
- Lee Mi-Jeong, Pramyothin Pornpoj, Karastergiou Kalypso, and Fried Susan K.. 2014. “Deconstructing the Roles of Glucocorticoids in Adipose Tissue Biology and the Development of Central Obesity.” (BBA)-Molecular Basis of Disease 1842(3):473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López N, and Gadsden VL. 2016. Health Inequities, Social Determinants, and Intersectionality. Discussion Paper, National Academy of Medicine, Washington, DC: Retrieved July 25, 2018 (https://nam.edu/wp-content/uploads/2016/12/Health-Inequities-Social-Determinants-and-Intersectionality.pdf.) [Google Scholar]
- Maddox Keith B. 2004. “Perspectives on Racial Phenotypicality Bias.” Personality and Social Psychology Review 8(4):383–401. [DOI] [PubMed] [Google Scholar]
- McEwen Bruce S. 2008. “Central Effects of Stress Hormones in Health and Disease: Understanding the Protective and Damaging Effects of Stress and Stress Mediators.” European Journal of Pharmacology 583(2–3):174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee Daniel L., and Diverse Populations Collaboration. 2005. “Body Mass Index and Mortality: A Meta-analysis Based on Person-Level Data from Twenty-Six Observational Studies.”Annals of Epidemiology 15(2):87–97. [DOI] [PubMed] [Google Scholar]
- Monk Ellis P. 2014. “Skin Tone Stratification among Black Americans, 2001–2003.” Social Forces 92(4):1313–1337. [Google Scholar]
- Monk Ellis P. 2015. “The Cost of Color: Skin Color, Discrimination, and Health among African Americans.” American Journal of Sociology 121(2):396–444. [DOI] [PubMed] [Google Scholar]
- Pearlin Leonard I., Menaghan Elizabeth G., Lieberman Morton A., and Mullan Joseph T. 1981. “The Stress Process.” Journal of Health and Social Behavior 22(4):337–356. [PubMed] [Google Scholar]
- Phelan Jo C., and Link Bruce G.. 2015. “Is Racism a Fundamental Cause of Inequalities inHealth?” Annual Review of Sociology 41:311–330. [Google Scholar]
- Raudenbush Stephen W. and Bryk Anthony S.. 2002. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Ryan Andrew M., Gee Gilbert C., and Laflamme David F.. 2006. “The Association between Self-Reported Discrimination, Physical Health and Blood Pressure: Findings from African Americans, Black Immigrants, and Latino Immigrants in New Hampshire.” Journal of Health Care for the Poor and Underserved 17(2): 116–132. [DOI] [PubMed] [Google Scholar]
- Shuey Kim M, and Willson Andrea E.. 2008. “Cumulative Disadvantage and Black-White Disparities in Life-Course Health Trajectories.” Research on Aging 30(2):200–225. [Google Scholar]
- Sweet Elizabeth, McDade Thomas W., Kiefe Catarina I., and Liu Kiang. 2007. “Relationships between Skin Color, Income, and Blood Pressure among African Americans in the CARDIA Study.” American Journal of Public Health 97(12):2253–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzogara Ekeoma E., and Jackson James S.. 2016. “Perceived Skin Tone Discrimination across Contexts: African American Women’s Reports.” Race and Social Problems 8(2):147–159. [Google Scholar]
- Viruell-Fuentes Edna A., Miranda Patricia Y., and Abdulrahim Sawsan. 2012. “More than Culture: Structural Racism, Intersectionality Theory, and Immigrant Health.” Social Science & Medicine 75(12):2099–2106. [DOI] [PubMed] [Google Scholar]
- Wade Joel T., Romano Melanie, and Blue Leslie. 2004. “The Effect of African American Skin Color on Hiring Preferences.” Journal of Applied Social Psychology 34(12):2550–2558. [Google Scholar]
- Williams David R., and Mohammed Selina A.. 2013. “Racism and Health I: Pathways and Scientific Evidence.” American Behavioral Scientist 57(8):1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingfield Adia H. 2007. “The Modern Mammy and the Angry Black Man: African American Professionals’ Experiences with Gendered Racism in the Workplace.” Race, Gender, & Class 14(2): 196–212. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.