Abstract
Research Question:
Do patients with dual diagnosis (DD) with an early initiation of substance use and subsequent early onset substance use disorder (EOS) differ from those with late onset substance use disorder (LOS) regarding characteristics, sex-related risk behaviors, course, and outcome?
Objectives:
The aim is to study EOS and LOS groups of patients with DD attending a treatment center with regard to clinical characteristics, type of psychiatric disorders, risk behaviors, and short-term outcome.
Materials and Methods:
Retrospective chart review of patients diagnosed with DD (n = 307) with regard to the above variables. Diagnoses of both substance use disorders (SUDs) and psychiatric disorders were made by qualified psychiatrists as per the International Classification of Diseases, 10th revision.
Results:
Among 307 participants with DD, 100 were in EOS group (onset of SUD before 18 years of age as assessed clinically) and 207 in LOS group. Cannabis as the primary substance was more prevalent in the EOS (30%) than that of the LOS group (12%). Psychotic disorders were more prevalent in the EOS group (41%) followed by mood disorders (30%), while the reverse was true in the LOS group (27.5% and 56.5%, respectively). When compared to the LOS group, the EOS group had higher number of psychiatric admissions, reported higher prevalence of risky sexual behaviors (unprotected sexual intercourse, multiple sexual partners, and history of sexual intercourse with commercial sex workers), showed poorer treatment adherence, and worse outcome regarding both psychiatric disorder and SUD (all differences significant at P < 0.05).
Conclusions:
DD patients differ significantly based on the age of onset of substance use. These may have therapeutic and management implications.
Keywords: Age of onset, dual diagnosis, outcome
INTRODUCTION
Age of initiation of substance use during childhood/adolescence has been associated with various long-term health and social complications. Early onset of substance use (EOS) occurs generally in the early to late adolescent period (<18 years) of age.[1] Various studies have revealed strong associations between the age of first alcohol/cannabis/cocaine/psychostimulants use and the development of dependence.[2,3,4,5,6,7,8] Earlier studies had defined early age of onset (more particularly to that of alcohol) to be <25 years of age.[9] However, recent literature have highlighted the issue of a more earlier age of onset of substance use, i.e., on or before 17–18 years of age which is mostly the preadolescent and/or adolescent age to be more common and is adversely associated with various psychosocial problems.[1,10,11,12,13,14] Therefore, newer data suggest to limit the cutoff age to define early and late substance use disorder (SUD) with regard to the age of onset to be at 17 or 18 years of age.[1,10,11,12,13,14] Apart from having more severe complications and frequent treatment admissions, the individuals with EOS have an early indicator for the development of the psychiatric disorder.[1,15,16,17] Few studies have demonstrated association between early-onset cannabis use and earlier development of the major depressive disorder, suicidal ideations, and suicidal attempts.[18,19,20,21]
Epidemiological-based and clinical-based studies had revealed that dual diagnosis (DD) or co-occurring disorders exist in about one-third of patients with SUDs.[22,23,24] Early age of initiation of substance use and subsequent development of SUD at an early age have been found to be associated with a longer duration of untreated illness of psychiatric disorder and poorer clinical and functional outcomes.[25,26,27] Poorer treatment-seeking behavior is also linked with EOS group of individuals with DD.[28,29,30] However, there is currently almost no evidence in the available literature regarding any difference in the clinical characteristics, course, and outcome of patients with DD with respect to the age of onset of substance use (i.e., EOS vs. LOS).
With this background, the current study was intended to compare patients with DD with early-onset of substance use (EOS group) with those with DD with late-onset substance use (LOS group) on various parameters (clinical characteristics, risk behavior, and short-term course and outcome).
MATERIALS AND METHODS
The participants of the present study were outpatients visiting the Drug De-addiction and Treatment Centre (DDTC) at the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. DDTC, PGIMER caters to 20 inpatients and yearly average of 2500–3000 new patients. Out of all these patients, detail workup is made for yearly average of 700–1000 patients. In the outpatient services of DDTC, PGIMER, all the participants visiting for the first time are evaluated by a qualified psychiatrist, diagnosis is made as per the International Classification of Diseases, 10th revision (ICD-10)[31] and treatment is initiated. A unique Central Registration Number is assigned to every subject seeking treatment. After an average of 2–3 follow-up visits, the detail workup is done by a trainee psychiatrist in a structured format under the supervision of a qualified psychiatrist and later on is reviewed by the Consultant. During this visit, a DDTC file number is assigned to the subject and if the participant is diagnosed with a comorbid psychiatric disorder, i.e., DD, then an additional DD clinic number is assigned to the same participant. Psychiatric diagnosis was confirmed by two-stage method. The psychiatric diagnosis (both substance use and psychiatric diagnosis) was made clinically by the qualified psychiatrist as per the ICD-10. Later, the diagnosis was confirmed by the consultant. For this study, the DDTC files with DD numbers from 1 to 307 were retrieved and inspected retrospectively. The sociodemographic and clinical details from the detail workup file which included the age of initiation of substance and subsequent development of SUD was recorded. Those with the initiation of substance and onset of clinically diagnosable SUD before the age of 18 years were categorized under the EOS group and others having the initiation of substance use and development of SUD later than 18 years were grouped under the LOS group. The treatment records in these files were analyzed in detail to find out the outcome in terms of no of follow-ups, course of the psychiatric disorder, high-risk behaviors, and consequences in various domains (health, social, marital, family, legal, and occupation). The study protocol was approved by the Institutional Ethical Review Board of the Institute.
Statistical analysis
The analysis was performed using SPSS software version 16 (Statistical Package for the Social Sciences, Chicago, IL, USA). Frequencies and percentages were computed for discontinuous sociodemographic and clinical variables. Mean and standard deviation (SD) for the continuous variables were calculated. Both the groups were compared using t-test, Chi-square test, Fisher's exact test, and Yate's correction wherever applicable. For multiple comparisons, Bonferonni post hoc test correction was carried out. The statistical significance was kept at P < 0.05.
RESULTS
Of the 307 patients with DD, 100 patients had the initiation of substance use and development of SUD before <18 years of age and were categorized into the EOS group and rest 207 patients fell into the LOS group. Both the groups were compared across different variables.
Sociodemographic profile
As evident from Table 1, the difference in age at first presentation to our services in both the groups was statistically significant. There were no females in the EOS group and only four females in the LOS group, but it was not statistically significant. More married and employed individuals were present in the LOS group and the difference was significant too. However, there was no difference in the level of education, locality, religion, and type of family in both the groups.
Table 1.
Comparison of sociodemographic parameters between early onset (EOS; n=100) and late onset (LOS; n=207) substance use group
| Parameters | Mean (SD)/n (%) | t-test/χ2 (P) | |
|---|---|---|---|
| Early onset SUD (n=100) | Late onset SUD (n=207) | ||
| Age at presentation | 29.56 (9.52) (range: 14-67) | 39.35 (11.21) (range: 19-84) | t=−7.516 (<0.001)*** (CI: −12.35-−7.22) |
| Sex | |||
| Male | 100 (100) | 203 (98.1) | χ2=1.95 (0.161) |
| Female | 0 | 4 (1.9) | |
| Education | |||
| Illiterate | 7 (7) | 11 (5.3) | χ2=0.381 (0.943) |
| Under matric | 23 (23) | 48 (23.18) | |
| Matriculate | 25 (25) | 51 (24.6) | |
| Above matric | 45 (45) | 97 (46.8) | |
| Marital status | |||
| Single | 50 (50) | 43 (20.7) | χ2=27.33 (<0.001)*** |
| Married | 48 (48) | 156 (75.4) | |
| Divorced | 2 (2) | 8 (3.86) | |
| Occupation | |||
| Unemployed | 52 (52) | 53 (25.6) | χ2=20.87 (<0.001)*** |
| Employed on paid wages | 48 (48) | 154 (74.3) | |
| Religion | |||
| Hindu | 63 (63) | 130 (62.8) | χ2=0.001 (0.973) |
| Non-Hindu | 37 (37) | 77 (37.1) | |
| Family type | |||
| Nuclear | 58 (58) | 102 (49.3) | χ2=2.05 (0.151) |
| Nonnuclear | 42 (42) | 105 (50.7) | |
| Locality | |||
| Urban | 55 (55) | 118 (57) | χ2=0.11 (0.739) |
| Rural | 45 (45) | 89 (42.9) | |
*P<0.05; **P<0.01; ***P<0.001. SUD – Substance use disorders; SD – Standard deviation; CI – Confidence interval; EOS – Early onset substance use disorder; LOS – Late onset substance use disorder
Clinical profile of the two groups
As depicted in Table 2, the mean age of onset of primary substance use in the EOS and LOS group was 15.65 (SD – 2.33) years of age and 25.51 (SD – 6.74) years, respectively. However, no difference was noted in the mean duration (in months) of the dependence of primary substance in both groups. The age of onset of psychiatric disorder in both the groups was found to be statistically significant (EOS – 23.25 [SD – 8.55] vs. LOS – 32.44 [SD – 10.99]; P < 0.001). In both groups, alcohol was the primary substance abused (EOS – 43% vs. LOS – 59.9%). However, cannabis as the primary substance was more prevalent in the EOS (30%) than the LOS group (12.6%). Overall, the difference in the prevalence of primary substance use in both groups was statistically significant for alcohol (P = 0.005), tobacco (P = 0.001), and cannabis (P < 0.001). While more number of participants in the EOS group had a history of admission to hospital (40%) as compared to the LOS group (28.5%), more number of participants in the LOS group had a poor outcome after admission (EOS – 24% vs. LOS – 54.5%; P = 0.005). With regard to the diagnosis of psychiatric disorder in both groups, psychotic disorders were more prevalent in the EOS group (41%) followed by affective/mood disorders (30%) while the reverse was true in the LOS group (56.5%, 27.5%) [Figure 1]. However, the statistical significant difference after applying correction for multiple comparisons was only for psychotic disorders (P = 0.018) and affective disorders (P < 0.001). Anxiety disorders were the third-most common psychiatric diagnosis in both groups. There was no difference in the presence/absence of externalizing symptoms, history of treatment by faith healers, and family history of SUD in both the groups.
Table 2.
Comparison of clinical profile EOS versus LOS
| Parameters | Mean (SD)/n (%) | t-test/χ2 (P) | |
|---|---|---|---|
| EOS (n=100) | LOS (n=207) | ||
| Age of initiation of primary substance use | 15.65 (2.33) | 25.51 (6.74) | t=−14.206 (<0.001)*** (CI: −11.22-−8.49) |
| Duration in months of dependence of primary substance | 128.38 (96.48) (range: 10-456) | 127.35 (97.70) (range: 2-480) | t=0.086 (0.931) (CI: −22.31-24.36) |
| Number of substance dependence | |||
| 1 | 15 (15) | 48 (23.2) | χ2=4.355 (0.226) |
| 2 | 46 (46) | 97 (46.9) | |
| 3 | 30 (30) | 51 (24.6) | |
| >3 | 9 (9) | 11 (5.3) | |
| Most common primary substance | |||
| Alcohol | 43 (43) | 124 (59.9) | χ2=7.766 (0.005)* |
| Tobacco | 11 (11) | 4 (1.9) | χ2=11.930 (0.001)*** |
| Cannabis | 30 (30) | 26 (12.6) | χ2=13.751 (<0.001)*** |
| Opioids | 15 (15) | 47 (22.7) | χ2=2.484 (0.115) |
| Sedatives/hypnotics | 1 (1) | 5 (2.4) | χ2=0.705 (0.401) |
| Inhalants | 0 | 1 (0.5) | F=0.001 Adjusted post hoc χ2=29.28 (<0.001)*** |
| Age of onset of psychiatric disorder | 23.25 (8.55) (range: 2-55) | 32.44 (10.99) (range: 7-83) | t=−7.354 (<0.001)*** (CI: −11.65-−6.73) |
| Classification of psychiatric disorder | |||
| F00-F09 | 1 (1) | 1 (0.5) | χ2=0.546F |
| F20-F29 | 41 (41) | 57 (27.5) | χ2=5.624 (0.018)* |
| F30-F39 | 30 (30) | 117 (56.5) | χ2=19.005 (<0.001)*** |
| F40-F48 | 20 (20) | 27 (13.0) | χ2=2.517 (0.113) |
| F50-F59 | 0 | 2 (1.0) | F=1.000 |
| F60-F69 | 3 (3) | 2 (1.0) | F=0.334 |
| F70-F79 | 2 (2) | 0 | F=0.105 |
| F90-F98 | 3 (3) | 1 (0.5) | F=0.103 Adjusted post hoc χ2=26.23 (<0.001)*** |
| Past history of admission | |||
| Yes | 40 (40) | 59 (28.5) | χ2=4.080 (0.043)* |
| No | 60 (60) | 148 (71.49) | |
| Outcome of admission | |||
| Improved | 56 (56) | 94 (45.4) | χ2=13.984 (<0.001)*** |
| Not improved | 24 (24) | 113 (54.5) | |
| History of externalizing symptoms | |||
| Yes | 31 (31) | 35 (16.9) | χ2=7.934 (0.005)** |
| No | 69 (69) | 172 (83.1) | |
| History of treatment by faith-healers | |||
| Yes | 13 (13) | 27 (13) | χ2=0.00001 (0.991) |
| No | 87 (87) | 180 (87) | |
| Family history of substance dependence | |||
| Yes | 46 (46) | 87 (42) | χ2=0.433 (0.511) |
| No | 54 (54) | 120 (58) | |
*P<0.05; **P<0.01; ***P<0.001. SD – Standard deviation; CI – Confidence interval; EOS – Early onset substance use disorder; LOS – Late onset substance use disorder
Figure 1.
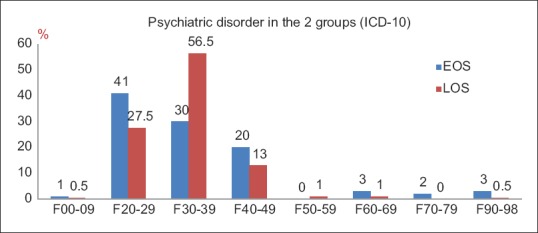
Psychiatric disorders in the early onset substance use disorder (EOS) and late onset substance use disorder (LOS) dual diagnosis patients groups
Comparison of clinical parameters in both the groups
EOS group had both onset of tobacco use and development of dependence at an earlier age as compared to LOS group and the difference was statistically significant in both cases [Table 3]. Both the groups had the almost the same number of participants with intravenous drug use. There was more prevalence of unprotected sexual intercourse, multiple sexual partners, and history of sexual intercourse with commercial sex workers (CSW), history of premarital sexual contact in the EOS group as compared to the LOS group, the difference in all these parameters being significant statistically. With regard to nature of the psychiatric disorder, both the groups did not differ in relation to number of relapse of psychiatric illness due to poor drug compliance, number of relapses, family history of psychiatric disorder, and history of suicide attempt. However, there was more continuous type of psychiatric illness in the EOS group than the episodic type of illness in the LOS group. Clinical insight of psychiatric illness was absent in more subjects in the EOS group, the difference being significant statistically.
Table 3.
Comparison of clinical parameters in both the groups
| Clinical parameters | Mean (SD)/n (%) | t-test/χ2 (P) | |
|---|---|---|---|
| EOS | LOS | ||
| Age of onset of tobacco use | n=82 18.06 (3.80) | n=149 21.75 (5.57) | t=−5.345 (0.003)** (CI: −5.05-−2.33) |
| Age of tobacco dependence | n=82 19.10 (3.84) | n=149 22.97 (5.22) | t=−5.898 (0.024)* (CI: −5.17-−2.58) |
| IDU parameters | n=100 | n=207 | |
| ID dependence | 3 (3) | 7 (3.4) | χ2=0.001 (1.00) |
| History of IDU by IV route | 3 (3) | 6 (2.9) | χ2=0.001 (1.00) |
| Sharing of needles | 3 (3) | 2 (1) | F=1.74 (0.334) |
| Sharing of mixer/vials/cottons | 2 (2) | 4 (1.9) | F=0.002 (1.00) |
| Sharing of syringes | 2 (2) | 2 (1) | F=0.56 (0.599) |
| Reuse of needles/syringes | 2 (2) | 3 (1.4) | F=0.106 (1.00) |
| History of unprotected sexual intercourse | |||
| Present | 14 (14) | 9 (4.3) | χ2=9.064 (0.003)** |
| History of multiple sexual partners | |||
| Present | 14 (14) | 11 (5.3) | χ2=6.801 (0.009)** |
| History of sexual intercourse with CSW | |||
| Present | 16 (16) | 17 (8.2) | χ2=4.262 (0.039)* |
| History of premarital sexual intercourse | |||
| Present | 12 (12) | 9 (4.3) | χ2=6.196 (0.013)* |
| History of surreptitious use of medications | |||
| Present | 33 (33) | 49 (23.7) | χ2=2.997 (0.083) |
| Relapse of psychiatric illness due to poor drug compliance | |||
| Present | 55 (55) | 104 (50.2) | χ2=0.611 (0.434) |
| Number of relapses of psychiatric illness | 1.11 (1.12) | 1.02 (1.14) | χ2=0.652 (0.715) |
| Family history of psychiatric illness | |||
| Present | 34 (34) | 76 (36.7) | χ2=0.216 (0.642) |
| History of involuntary admission due to psychiatric illness | |||
| Present | 15 (15) | 34 (16.4) | χ2=0.102 (0.749) |
| Course of psychiatric illness | |||
| Continuous | 75 (75) | 126 (60.9) | χ2=5.955 (0.015)* |
| Episodic | 25 (25) | 81 (39.1) | |
| History of suicide attempt | |||
| Present | 17 (17) | 33 (15.9) | χ2=0.055 (0.814) |
| Insight of psychiatric illness | |||
| Absent | 33 (33) | 51 (24.6) | χ2=6.09 (0.048)* |
| Partial | 50 (50) | 95 (45.9) | |
| Present | 17 (17) | 61 (29.5) | |
*P<0.05; **P<0.01; ***P<0.001. F – Fischer’s exact. SD – Standard deviation; CI – Confidence interval; EOS – Early onset substance use disorder; LOS – Late onset substance use disorder; IDU – Intravenous drug use; IV – Intravenous; CSW – Commercial sex worker; ID – Intravenous drugs
Comparison of substance use disorder-related consequences in both groups
Although there were several SUD-related complications at the time of initial presentation in both the groups, there was no difference between the two groups statistically [as evident from Table 4].
Table 4.
Comparison of substance use disorders related complications
| Complications | Frequency (%) | χ2 (P) | |
|---|---|---|---|
| EOS (n=100) | LOS (n=207) | ||
| Health related | |||
| Nil | 20 (20) | 50 (24.2) | χ2=1.471 (0.689) |
| Mild | 37 (37) | 81 (39.1) | |
| Moderate | 41 (41) | 71 (34.3) | |
| Severe | 2 (2) | 5 (2.4) | |
| Occupation related | |||
| Nil | 15 (15) | 46 (22.2) | χ2=2.60 (0.457) |
| Mild | 48 (48) | 90 (43.5) | |
| Moderate | 31 (31) | 56 (27.1) | |
| Severe | 6 (6) | 15 (7.2) | |
| Finance related | |||
| Nil | 25 (25) | 59 (28.5) | χ2=2.78 (0.427) |
| Mild | 42 (42) | 91 (44.0) | |
| Moderate | 32 (32) | 51 (24.6) | |
| Severe | 1 (1) | 6 (2.9) | |
| Legal related | |||
| Nil | 71 (71) | 146 (70.5) | χ2=4.010 (0.260) |
| Mild | 27 (27) | 55 (26.6) | |
| Moderate | 2 (2) | 1 (0.5) | |
| Severe | 0 | 5 (2.4) | |
| Family related | |||
| Nil | 26 (26) | 71 (34.3) | χ2=2.158 (0.540) |
| Mild | 52 (52) | 96 (46.4) | |
| Moderate | 21 (21) | 38 (18.4) | |
| Severe | 1 (1) | 2 (1.0) | |
| Marital related | |||
| Nil | 50 (50) | 77 (37.2) | χ2=3.441 (0.064) |
| Mild | 38 (38) | 100 (48.3) | |
| Moderate | 11 (11) | 28 (13.5) | |
| Severe | 1 (1) | 2 (1.0) | |
| Social related | |||
| Nil | 26 (26) | 68 (32.9) | χ2=2.419 (0.548) |
| Mild | 59 (59) | 105 (50.7) | |
| Moderate | 15 (15) | 33 (15.9) | |
| Severe | 0 | 1 (0.5) | |
EOS – Early onset substance use disorder; LOS – Late onset substance use disorder
Comparison of short-term course and outcome
At 1-month follow-up, more subjects in the EOS group worsened than the LOS group in relation to SUD (21% vs. 1%; P < 0.001). At 3-month follow-up, no difference between the groups with regard to either psychiatric disorder or SUD was noted. In addition, when evaluated at 6 months it was seen that the subjects that followed up in the clinic (EOS: 39%; LOS: 34%; P > 0.05), outcome was noted as improved in the EOS group compared to LOS group regarding both psychiatric disorder (87% vs. 62%; P = 0.007) and SUD (82% vs. 62%; P = 0.012), despite a further drop in the follow-ups in both the groups (which was comparable in both the groups (Follow-up: EOS – 39% vs. LOS – 34.29%) [Table 5].
Table 5.
Comparison of follow up status in both groups
| Follow up status | Mean (SD)/n (%) | t-test/χ2 (P) | |
|---|---|---|---|
| EOS (n=100) | LOS (n=207) | ||
| At 1 month | |||
| Number of follow ups | 1.50 (1.106) (range: 0-4) | 1.37 (1.21) (range: 0-5) | t=0.924 (0.356) (CI: −0.15-0.416) |
| Adherence | |||
| Poor | 30 (30) | 77 (37.19) | χ2=1.54 (0.462) |
| >50 | 24 (24) | 45 (21.7) | |
| >75 | 46 (46) | 85 (41.1) | |
| Compliance | |||
| Yes | 67 (67) | 121 (58.5) | χ2=2.075 (0.149) |
| No | 33 (33) | 86 (41.5) | |
| Motivation | |||
| Precontemplation | 43 (43) | 99 (47.8) | χ2=0.836 (0.840) |
| Contemplation | 37 (37) | 71 (34.3) | |
| Preparation | 12 (12) | 20 (9.7) | |
| Action | 8 (8) | 17 (8.2) | |
| Maintenance | 0 | 0 | |
| Insight | |||
| Absent | 28 (28) | 75 (36.23) | χ2=4.707 (0.095) |
| Partial | 46 (46) | 69 (33.3) | |
| Full | 26 (26) | 63 (30.4) | |
| Outcome of psychiatric disorder | |||
| Worsened | 0 | 3 (1.4) | χ2=2.096 (0.350) |
| Unchanged | 35 (35) | 81 (39.13) | |
| Improved | 65 (65) | 123 (59.4) | |
| Outcome of substance dependence | |||
| Worsened | 21 (21) | 2 (1.0) | χ2=48.877 (<0.001) |
| Unchanged | 17 (17) | 87 (42.02) | |
| Improved | 62 (62) | 118 (57.0) | |
| At 3 months | |||
| Number of follow ups |
n=85 1.52 (1.436) (range: 0-6) |
n=175 1.35 (1.52) (range: 0-6) |
t=0.828 (0.409) (CI: −0.225-0.552) |
| Adherence | |||
| Poor | 52 (61.11) | 15 (7.24) | χ2=92.26 (<0.001)*** |
| >50 | 10 (11.76) | 106 (60.57) | |
| >75 | 23 (27.05) | 54 (26.08) | |
| Compliance | |||
| Yes | 45 (45) | 73 (35.3) | χ2=2.909 (0.088) |
| No | 40 (47.05) | 102 (58.28) | |
| Motivation | |||
| Precontemplation | 57 (67.05) | 45 (25.71) | χ2=54.44 (<0.001)*** |
| Contemplation | 22 (25.88) | 80 (45.71) | |
| Preparation | 3 (3.52) | 50 (28.57) | |
| Action | 3 (3.52) | 0 | |
| Maintenance | 0 | 0 | |
| Insight | |||
| Absent | 18 (21.17) | 6 (2.9) | χ2=23.58 (<0.001)*** |
| Partial | 55 (64.70) | 123 (70.28) | |
| Full | 12 (14.11) | 46 (22.2) | |
| Outcome of psychiatric disorder | |||
| Worsened | 2 (2.35) | 3 (1.4) | χ2=2.409 (0.299) |
| Unchanged | 36 (42.35) | 92 (52.5) | |
| Improved | 47 (55.29) | 80 (38.6) | |
| Outcome of substance dependence (%) | |||
| Worsened | 2 (2.35) | 7 (4) | χ2=0.662 (0.718) |
| Unchanged | 42 (49.41) | 90 (51.42) | |
| Improved | 41 (48.23) | 78 (37.7) | |
| Follow ups at 6 months | |||
| Number of follow ups |
n=39 2.31 (1.52) (range: 1-9) |
n=71 2.52 (1.48) (range: 1-9) |
t=−0.715 (0.412) (CI: −0.805-0.378) |
| Adherence | |||
| Poor | 6 (15.4) | 14 (19.7) | χ2=2.284 (0.319) |
| >50 | 8 (20.5) | 22 (31) | |
| >75 | 25 (64.1) | 35 (49.3) | |
| Compliance | |||
| Yes | 32 (82.1) | 45 (63.4) | χ2=4.179 (0.041)* |
| No | 7 (17.9) | 26 (36.6) | |
| Motivation | |||
| Precontemplation | 7 (17.9) | 17 (23.9) | χ2=4.87 (0.301) |
| Contemplation | 15 (38.5) | 24 (33.8) | |
| Preparation | 3 (7.7) | 11 (15.5) | |
| Action | 14 (35.9) | 17 (23.9) | |
| Maintenance | 0 | 2 (2.8) | |
| Insight | |||
| Absent | 3 (7.7) | 4 (5.6) | χ2=0.662 (0.718) |
| Partial | 12 (30.8) | 27 (38.0) | |
| Full | 24 (61.5) | 40 (56.3) | |
| Outcome of psychiatric disorder | |||
| Worsened | 0 | 10 (14.1) | χ2=8.766 (0.007) |
| Unchanged | 5 (12.8) | 17 (23.9) | |
| Improved | 34 (87.17) | 44 (62) | |
| Outcome of substance dependence | |||
| Worsened | 0 | 9 (12.7) | χ2=8.027 (0.012) |
| Unchanged | 7 (17.9) | 18 (25.3) | |
| Improved | 32 (82.1) | 44 (62.0) | |
*P<0.05; **P<0.01; ***P<0.001. SD – Standard deviation; CI – Confidence interval; EOS – Early onset substance use disorder; LOS – Late onset substance use disorder
DISCUSSION
The present study aimed to find out whether there was any relationship between the age of initiation of substance use in patients with DD in the overall course and outcome of DD. To the best of our knowledge, this is the first study in this regard from a tertiary drug de-addiction center in India. Although it was a retrospective study, every possible effort was made to document and analyze all variables related to the diagnosis and management of every subject included in the study.
In the present study, we assessed the treatment details and follow-up data of 307 patients with DD and based on age cutoff of 18 years, the cases were recruited into EOS and LOS group. As evident from the results, participants in the EOS group presented to the healthcare services earlier. It can be because earlier the substance use and development of dependence, earlier is the dysfunction noted in academic, social and work domains by the caregivers and early is the treatment sought by the family. This is in accordance with the report by Substance Abuse and Mental Health Services Administration report[10] which also suggested that 74% of treatment admissions from age 18 to 30 years had the initiation of substance by the age of 17 years or less. Thereby, we can suggest that it is not an uncommon scenario in the adolescent age group to initiate substance earlier.
The mean age of onset of primary substance use in our EOS group was 15.65 (SD – 2.33) years, which is in accordance with the previous studies regarding the age of onset of substance abuse.[3,4,32,33,34,35,36] Although in both the groups, more number of participants were dependent on two substances, yet about 40% of participants in the EOS group were dependent on >3 substances which about 10% was less in the LOS group. Existing literature also supports this view that earlier the age of onset of substance, more is the prevalence of polysubstance dependence.[1,37,38] Alcohol was more common in both groups, but cannabis was the second-most prevalent substance in the EOS group. Similar findings have been reported by various studies which have reported cannabis to be more commonly abused by adolescents worldwide.[39,40,41,42] Higher prevalence of cannabis use has also been regarded as a predictor of subsequent initiation with other illicit and licit drugs or commonly known as the “gateway hypothesis” in the adolescent population.[43,44,45,46] With regard to tobacco use, the EOS group had very early onset of initiation and subsequent dependence and the same had been replicated across several studies. In addition, studies have also reported a strong relationship between early-onset regular smoking to later alcohol use and other risky behaviors in adolescence.[6,47,48,49]
When we introspect about the nature of the psychiatric illness in the two groups, a higher prevalence of psychotic disorders in the EOS group and a higher prevalence of affective disorders in the LOS group were noted. Studies which have evaluated first episode psychosis (mostly in adolescents) have found a high prevalence of comorbid SUD and more particularly cannabis in this age group.[50,51,52,53,54,55] Similarly, studies which have tried to link between substance abuse and affective disorders/Bipolar disorder have found the association of alcohol use/dependence after 18 years of age.[56,57,58,59] Few Indian studies on patients with DD have also reported a higher prevalence of affective disorders and anxiety disorders.[60,61,62,63] However, we were unable to find any previous Indian/Western studies which had tried to compare EOS and LOS patients with DD.
As compared to the LOS group, the EOS group had more high-risk sexual behavior in the form of unprotected sexual encounter, multiple sexual partners, and sexual encounter with CSW. This is also been replicated across several studies that earlier age of onset of SUD has been associated with high-risk sexual behaviors,[64] infrequent condom use and pregnancy,[65,66] sexually-transmitted diseases,[67] violence,[68] depression, and suicide.[69,70,71] With regard to high-risk sexual behavior in those who had early initiation of substance use and subsequent early development of SUD, the role of difficult temperament could not be excluded as it has been well established from number of studies that temperamental characteristics increases one's to various risk-taking behaviors early in the childhood.[72,73,74] Although in this study, we were unable to find any association between temperament and sexual risk behaviors, there is evidence of the high prevalence of sexual risky behaviors in the EOS group suggesting temperamental predisposition.
As far as the SUD-related consequences are concerned, no significant differences were found between the two groups on the various psycho-social-legal domains. It could be because most of the participants with DD had a similar profile of SUD-related complications at the time of presentation. This is in contrast to some studies which have found earlier age of onset of SUD to be associated with more severe psychosocial problems.[11,75]
Another aspect of the present study was to look for any difference in the short-term outcome with regard to follow-up patterns in the two groups. From the study findings, we are able to conclude that (1) At 1 month follow-up, there was not much difference between the two groups in different parameters of adherence, compliance to treatment, insight about psychiatric illness, and outcome of psychiatric illness. Only difference was noted in the worsening in the short-term outcome of SUD in about one-fifth of patients in the EOS-DD group which can be related to the difficulties usually encountered while treating adolescents with SUD[76,77,78,79] and nature of psychiatric illness (mostly psychosis) during initial phases of treatment (2) At 3-month follow-up, despite comparable dropout rates in both the groups, there was a significant difference noted in the adherence rates in the EOS group which was poorer (in those retained in the study after 3 months) than the LOS group. In addition, there was more number of subjects in the EOS-DD group who had the poor motivation to quit substances even at the end of 3 months suggesting that there are several difficulties in ensuring motivation to quit substances in early-onset SUD.[11,76] However, by 3 months, there was not much difference in the short-term outcome of psychiatric illness and substance dependence in both the groups which further suggested that more the contact with treatment services, better is the outcome whether it is EOS or LOS. Retention in the treatment network is the cornerstone of improvement in individuals with DD.[80,81,82,83] (3) At the end of 6 months, despite similar dropout rates in both groups, there was a significant difference noted in the outcome of psychiatric illness and SUD, i.e., EOS group had better outcome in both psychiatric illness and SUD as compared to the LOS group. This can be because that there was more number of subjects with psychotic disorders or cannabis-induced psychotic disorders in the EOS group and keeping them in the treatment net could have possibly led to better outcome in the EOS group with regard to more number of participants with affective disorders in the LOS group which possibly be having an episodic course with periodic relapses leading to more number of unchanged outcome.
We are well aware of our limitations. It was a retrospective study, and there is every possibility that many facts regarding the illness may not have been documented or would have been missed to be documented in the DD case files. The sample was limited to clinic-based treatment-seeking subjects and hence could not be generalized to the community. The study was based on clinical assessment only, without any instrumental or laboratory validation. Moreover, another important limitation of the present study was the short-term outcome was based on those subjects (in both groups) retained in follow-up. Further, we did not use any instrument to measure adherence, compliance, motivation, and insight and these assessments were limited to the assessment clinically by the treating psychiatrists during the follow-ups. All these parameters were rated as per the notes in the available treatment records, and there could be subjective/therapist variation in interpreting the same. Further, it is also a known fact that different SUDs have different clinical courses and have different psychosocial trajectories. However, to demonstrate the impact of age of onset of substance use and subsequent development of SUD of any substance category, we have clubbed all the SUDs into one category. Although it would have been ideal to analyze all the sub-groups, the sample size was too small to go for multiple subgroup analysis. Future studies with a larger sample size should overcome these limitations.
CONCLUSIONS
Despite the above limitations, the present study provided for the first time that there are significant differences in the clinical characteristics, psychiatric diagnosis, and risk behaviors in patients with DD based on the age of onset of SUD suggesting that the short-term course and outcome of patients with DD could be different if taken into account the age of onset of SUD. Of those retained in the follow-up, patients with EOS may actually fare better than the LOS group. This is a new finding that may be due to the type of substances used and type of psychiatric disorders in the EOS group. This study lays the foundation of further prospective studies, which if replicated with appropriate instruments, might have important management implications in DD patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Strashny A. The CBHSQ Report. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. [Last accessed on 2018 Dec 28]. The TEDS Report: Age of Substance Use Initiation among Treatment Admissions Aged 18 to 30. Available from: http://www.ncbi.nlm.nih.gov/books/NBK384841/ [PubMed] [Google Scholar]
- 2.Austic E, McCabe SE, Stoddard SA, Ngo QE, Boyd C. Age and cohort patterns of medical and nonmedical use of controlled medication among adolescents. J Addict Med. 2015;9:376–82. doi: 10.1097/ADM.0000000000000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the national longitudinal alcohol epidemiologic survey. J Subst Abuse. 1997;9:103–10. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- 4.Grant BF. Age at smoking onset and its association with alcohol consumption and DSM-IV alcohol abuse and dependence: Results from the national longitudinal alcohol epidemiologic survey. J Subst Abuse. 1998;10:59–73. doi: 10.1016/s0899-3289(99)80141-2. [DOI] [PubMed] [Google Scholar]
- 5.Liang W, Chikritzhs T. Age at first use of alcohol and risk of heavy alcohol use: A population-based study. Biomed Res Int. 2013;2013:721761. doi: 10.1155/2013/721761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmid B, Hohm E, Blomeyer D, Zimmermann US, Schmidt MH, Esser G, et al. Concurrent alcohol and tobacco use during early adolescence characterizes a group at risk. Alcohol Alcohol. 2007;42:219–25. doi: 10.1093/alcalc/agm024. [DOI] [PubMed] [Google Scholar]
- 7.Varma VK, Basu D, Malhotra A, Sharma A, Mattoo SK. Correlates of early – And late-onset alcohol dependence. Addict Behav. 1994;19:609–19. doi: 10.1016/0306-4603(94)90016-7. [DOI] [PubMed] [Google Scholar]
- 8.Vega WA, Aguilar-Gaxiola S, Andrade L, Bijl R, Borges G, Caraveo-Anduaga JJ, et al. Prevalence and age of onset for drug use in seven international sites: Results from the international consortium of psychiatric epidemiology. Drug Alcohol Depend. 2002;68:285–97. doi: 10.1016/s0376-8716(02)00224-7. [DOI] [PubMed] [Google Scholar]
- 9.Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;236:410–6. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- 10.Windle M, Windle RC. Early onset problem behaviors and alcohol, tobacco, and other substance use disorders in young adulthood. Drug Alcohol Depend. 2012;121:152–8. doi: 10.1016/j.drugalcdep.2011.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poudel A, Gautam S. Age of onset of substance use and psychosocial problems among individuals with substance use disorders. BMC Psychiatry. 2017;17:10. doi: 10.1186/s12888-016-1191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark DB, Kirisci L, Tarter RE. Adolescent versus adult onset and the development of substance use disorders in males. Drug Alcohol Depend. 1998;49:115–21. doi: 10.1016/s0376-8716(97)00154-3. [DOI] [PubMed] [Google Scholar]
- 13.Pope HG, Jr, Gruber AJ, Hudson JI, Cohane G, Huestis MA, Yurgelun-Todd D. Early-onset Cannabis use and cognitive deficits: What is the nature of the association? Drug Alcohol Depend. 2003;69:303–10. doi: 10.1016/s0376-8716(02)00334-4. [DOI] [PubMed] [Google Scholar]
- 14.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2013. [Google Scholar]
- 15.Deas D. Adolescent substance abuse and psychiatric comorbidities. J Clin Psychiatry. 2006;67(Suppl 7):18–23. [PubMed] [Google Scholar]
- 16.Shrier LA, Harris SK, Kurland M, Knight JR. Substance use problems and associated psychiatric symptoms among adolescents in primary care. Pediatrics. 2003;111:e699–705. doi: 10.1542/peds.111.6.e699. [DOI] [PubMed] [Google Scholar]
- 17.Tanaree A, Assanangkornchai S, Kittirattanapaiboon P. Pattern and risk of developing alcohol use disorders, illegal substance use and psychiatric disorders after early onset of alcohol use: Results of the Thai national mental health survey 2013. Drug Alcohol Depend. 2017;170:102–11. doi: 10.1016/j.drugalcdep.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 18.de Graaf R, Radovanovic M, van Laar M, Fairman B, Degenhardt L, Aguilar-Gaxiola S, et al. Early Cannabis use and estimated risk of later onset of depression spells: Epidemiologic evidence from the population-based World Health Organization world mental health survey initiative. Am J Epidemiol. 2010;172:149–59. doi: 10.1093/aje/kwq096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynskey MT, Glowinski AL, Todorov AA, Bucholz KK, Madden PA, Nelson EC, et al. Major depressive disorder, suicidal ideation, and suicide attempt in twins discordant for Cannabis dependence and early-onset Cannabis use. Arch Gen Psychiatry. 2004;61:1026–32. doi: 10.1001/archpsyc.61.10.1026. [DOI] [PubMed] [Google Scholar]
- 20.Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Allebeck P. Cannabis use and depression: A longitudinal study of a national cohort of Swedish conscripts. BMC Psychiatry. 2012;12:112. doi: 10.1186/1471-244X-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shalit N, Shoval G, Shlosberg D, Feingold D, Lev-Ran S. The association between Cannabis use and suicidality among men and women: A population-based longitudinal study. J Affect Disord. 2016;205:216–24. doi: 10.1016/j.jad.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry. 2004;56:730–7. doi: 10.1016/j.biopsych.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borges G, Wang PS, Medina-Mora ME, Lara C, Chiu WT. Delay of first treatment of mental and substance use disorders in Mexico. Am J Public Health. 2007;97:1638–43. doi: 10.2105/AJPH.2006.090985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Girolamo G, Dagani J, Purcell R, Cocchi A, McGorry PD. Age of onset of mental disorders and use of mental health services: Needs, opportunities and obstacles. Epidemiol Psychiatr Sci. 2012;21:47–57. doi: 10.1017/s2045796011000746. [DOI] [PubMed] [Google Scholar]
- 27.McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders: Implications for preventive intervention strategies and models of care. Curr Opin Psychiatry. 2011;24:301–6. doi: 10.1097/YCO.0b013e3283477a09. [DOI] [PubMed] [Google Scholar]
- 28.Carrá G, Bartoli F, Clerici M, El-Guebaly N. Psychopathology of dual diagnosis: New trumpets and old uncertainties. J Psychopathol. 2015;21:390–9. [Google Scholar]
- 29.Daigre C, Grau-López L, Rodríguez-Cintas L, Ros-Cucurull E, Sorribes-Puertas M, Esculies O, et al. The role of dual diagnosis in health-related quality of life among treatment-seeking patients in Spain. Qual Life Res. 2017;26:3201–9. doi: 10.1007/s11136-017-1668-4. [DOI] [PubMed] [Google Scholar]
- 30.Rady A, Salama H, Elkholy O, Shawky A. Dual diagnosis of mental illness and substance abuse: An Egyptian study. Eur Psychiatry. 2013;28:1. [Google Scholar]
- 31.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992. p. 377. [Google Scholar]
- 32.Bansal RK, Banerjee S. Substance use by child labourers. Indian J Psychiatry. 1993;35:159–61. [PMC free article] [PubMed] [Google Scholar]
- 33.Benegal V, Sathyaprakash M, Nagaraja D. Alcohol Misuse in the Andaman and Nicobar Islands. Report on Project Commissioned by the Indian Council of Medical Research and funded by Action Aid, India. Indian Council of Medical Research. 2008 [Google Scholar]
- 34.Dawson DA, Goldstein RB, Chou SP, Ruan WJ, Grant BF. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res. 2008;32:2149–60. doi: 10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tripathi BM, Lal R. Substance abuse in children and adolescents. Indian J Pediatr. 1999;66:569–75. doi: 10.1007/BF02727172. [DOI] [PubMed] [Google Scholar]
- 36.Zernicke KA, Cantrell H, Finn PR, Lucas J. The association between earlier age of first drink, disinhibited personality, and externalizing psychopathology in young adults. Addict Behav. 2010;35:414–8. doi: 10.1016/j.addbeh.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brache K, Stockwell T, Macdonald S. Functions and harms associated with simultaneous polysubstance use involving alcohol and cocaine. J Subst Use. 2012;17:399–416. [Google Scholar]
- 38.Moss HB, Chen CM, Yi HY. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 39.Balhara YP, Mishra A, Sethi H, Singh S, Khandelwal SK. Time trends of Cannabis use among treatment-seeking individuals at government de-addiction centers across India over a period of 7 years. Indian J Psychol Med. 2016;38:331–5. doi: 10.4103/0253-7176.185961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marzell M, Sahker E, Arndt S. Trends of youth marijuana treatment admissions: Increasing admissions contrasted with decreasing drug involvement. Subst Use Misuse. 2017;52:1778–83. doi: 10.1080/10826084.2017.1311349. [DOI] [PubMed] [Google Scholar]
- 41.Marzell M, Sahker E, Pro G, Arndt S. A brief report on Hispanic youth marijuana use: Trends in substance abuse treatment admissions in the United States. J Ethn Subst Abuse. 2017;16:155–64. doi: 10.1080/15332640.2015.1108256. [DOI] [PubMed] [Google Scholar]
- 42.Ray R. The Extent, Pattern and Trends of Drug Abuse in India-National Survey. Ministry of Social Justice and Empowerment, Government of India and United Nations Office on Drugs and Crime. 2004 [Google Scholar]
- 43.Legleye S, Janssen E, Beck F, Chau N, Khlat M. Social gradient in initiation and transition to daily use of tobacco and Cannabis during adolescence: A retrospective cohort study. Addiction. 2011;106:1520–31. doi: 10.1111/j.1360-0443.2011.03447.x. [DOI] [PubMed] [Google Scholar]
- 44.Mayet A, Legleye S, Falissard B, Chau N. Cannabis use stages as predictors of subsequent initiation with other illicit drugs among French adolescents: Use of a multi-state model. Addict Behav. 2012;37:160–6. doi: 10.1016/j.addbeh.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 45.Mayet A, Legleye S, Chau N, Falissard B. Transitions between tobacco and Cannabis use among adolescents: A multi-state modeling of progression from onset to daily use. Addict Behav. 2011;36:1101–5. doi: 10.1016/j.addbeh.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 46.Nkansah-Amankra S, Minelli M. “Gateway hypothesis” and early drug use: Additional findings from tracking a population-based sample of adolescents to adulthood. Prev Med Rep. 2016;4:134–41. doi: 10.1016/j.pmedr.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.John U, Meyer C, Rumpf HJ, Hapke U. Probabilities of alcohol high-risk drinking, abuse or dependence estimated on grounds of tobacco smoking and nicotine dependence. Addiction. 2003;98:805–14. doi: 10.1046/j.1360-0443.2003.00381.x. [DOI] [PubMed] [Google Scholar]
- 48.Myers MG, Kelly JF. Cigarette smoking among adolescents with alcohol and other drug use problems. Alcohol Res Health. 2006;29:221–7. [PMC free article] [PubMed] [Google Scholar]
- 49.White J, Walton D, Walker N. Exploring comorbid use of marijuana, tobacco, and alcohol among 14 to 15-year-olds: Findings from a national survey on adolescent substance use. BMC Public Health. 2015;15:233. doi: 10.1186/s12889-015-1585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barrigón ML, Gurpegui M, Ruiz-Veguilla M, Diaz FJ, Anguita M, Sarramea F, et al. Temporal relationship of first-episode non-affective psychosis with Cannabis use: A clinical verification of an epidemiological hypothesis. J Psychiatr Res. 2010;44:413–20. doi: 10.1016/j.jpsychires.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 51.Galvez-Buccollini JA, Proal AC, Tomaselli V, Trachtenberg M, Coconcea C, Chun J, et al. Association between age at onset of psychosis and age at onset of Cannabis use in non-affective psychosis. Schizophr Res. 2012;139:157–60. doi: 10.1016/j.schres.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.González-Pinto A, Vega P, Ibáñez B, Mosquera F, Barbeito S, Gutiérrez M, et al. Impact of Cannabis and other drugs on age at onset of psychosis. J Clin Psychiatry. 2008;69:1210–6. doi: 10.4088/jcp.v69n0802. [DOI] [PubMed] [Google Scholar]
- 53.Sevy S, Robinson DG, Napolitano B, Patel RC, Gunduz-Bruce H, Miller R, et al. Are Cannabis use disorders associated with an earlier age at onset of psychosis? A study in first episode schizophrenia. Schizophr Res. 2010;120:101–7. doi: 10.1016/j.schres.2010.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wisdom JP, Manuel JI. Prevalence of substance use in people with first-episode psychosis. J Dual Diagn. 2011;7:39–49. doi: 10.1080/15504263.2011.569876. [DOI] [PubMed] [Google Scholar]
- 55.Wisdom JP, Manuel JI, Drake RE. Substance use disorder among people with first-episode psychosis: A systematic review of course and treatment. Psychiatr Serv. 2011;62:1007–12. doi: 10.1176/appi.ps.62.9.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Boschloo L, Vogelzangs N, Smit JH, van den Brink W, Veltman DJ, Beekman AT, et al. Comorbidity and risk indicators for alcohol use disorders among persons with anxiety and/or depressive disorders: Findings from the Netherlands study of depression and anxiety (NESDA) J Affect Disord. 2011;131:233–42. doi: 10.1016/j.jad.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 57.Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3:181–8. [PubMed] [Google Scholar]
- 58.Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009;37:127–37. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Raimo EB, Schuckit MA. Alcohol dependence and mood disorders. Addict Behav. 1998;23:933–46. doi: 10.1016/s0306-4603(98)00068-9. [DOI] [PubMed] [Google Scholar]
- 60.Basu D, Ghosh A. Profile of patients with dual diagnosis: Experience from an integrated dual diagnosis clinic in North India. J Alcohol Drug Depend. 2015;3:1–2. [Google Scholar]
- 61.Kisore P, Lal N, Trivedi JK, Dalal PK, Aga VM. A study of comorbidity in psychoactive substance dependence patients. Indian J Psychiatry. 1994;36:133–7. [PMC free article] [PubMed] [Google Scholar]
- 62.Subodh BN, Hazari N, Elwadhi D, Basu D. Prevalence of dual diagnosis among clinic attending patients in a de-addiction centre of a tertiary care hospital. Asian J Psychiatr. 2017;25:169–74. doi: 10.1016/j.ajp.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 63.Vohra AK, Yadav BS, Khurana H. A study of psychiatric comorbidity in alcohol dependence. Indian J Psychiatry. 2003;45:247–50. [PMC free article] [PubMed] [Google Scholar]
- 64.DuRant RH, Smith JA, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Arch Pediatr Adolesc Med. 1999;153:286–91. doi: 10.1001/archpedi.153.3.286. [DOI] [PubMed] [Google Scholar]
- 65.Di Clemente RJ, editor. Adolescents and AIDS: A Generation in Jeopardy. Newbury Park, CA: Sage; 1992. Psychosocial determinants of condom use among adolescents; pp. 34–51. [Google Scholar]
- 66.Epstein L, Tamir A. Health-related behavior of adolescents: Change over time. J Adolesc Health Care. 1984;5:91–5. doi: 10.1016/s0197-0070(84)80005-4. [DOI] [PubMed] [Google Scholar]
- 67.Shafer MA, Boyer CB. Psychosocial and behavioral factors associated with risk of sexually transmitted diseases, including human immunodeficiency virus infection, among urban high school students. J Pediatr. 1991;119:826–33. doi: 10.1016/s0022-3476(05)80312-9. [DOI] [PubMed] [Google Scholar]
- 68.Choquet M, Menke H, Manfredi R. Interpersonal aggressive behaviour and alcohol consumption among young urban adolescents in France. Alcohol Alcohol. 1991;26:381–90. doi: 10.1093/oxfordjournals.alcalc.a045128. [DOI] [PubMed] [Google Scholar]
- 69.Dawes MA, Mathias CW, Richard DM, Hill-Kapturczak N, Dougherty DM. Adolescent suicidal behavior and substance use: Developmental mechanisms. Subst Abuse. 2008;2:13–28. doi: 10.4137/sart.s1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kaplow JB, Curran PJ, Dodge KA Conduct Problems Prevention Research Group. Child, parent, and peer predictors of early-onset substance use: A multisite longitudinal study. J Abnorm Child Psychol. 2002;30:199–216. doi: 10.1023/a:1015183927979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu P, Bird HR, Liu X, Fan B, Fuller C, Shen S, et al. Childhood depressive symptoms and early onset of alcohol use. Pediatrics. 2006;118:1907–15. doi: 10.1542/peds.2006-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Galéra C, Messiah A, Melchior M, Chastang JF, Encrenaz G, Lagarde E, et al. Disruptive behaviors and early sexual intercourse: The GAZEL youth study. Psychiatry Res. 2010;177:361–3. doi: 10.1016/j.psychres.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 73.Timmermans M, van Lier PA, Koot HM. Which forms of child/adolescent externalizing behaviors account for late adolescent risky sexual behavior and substance use? J Child Psychol Psychiatry. 2008;49:386–94. doi: 10.1111/j.1469-7610.2007.01842.x. [DOI] [PubMed] [Google Scholar]
- 74.Parkes A, Waylen A, Sayal K, Heron J, Henderson M, Wight D, et al. Which behavioral, emotional and school problems in middle-childhood predict early sexual behavior? J Youth Adolesc. 2014;43:507–27. doi: 10.1007/s10964-013-9973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Poudel A, Sharma C, Gautam S, Poudel A. Psychosocial problems among individuals with substance use disorders in drug rehabilitation centers, Nepal. Subst Abuse Treat Prev Policy. 2016;11:28. doi: 10.1186/s13011-016-0072-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bukstein OG, Horner MS. Management of the adolescent with substance use disorders and comorbid psychopathology. Child Adolesc Psychiatr Clin N Am. 2010;19:609–23. doi: 10.1016/j.chc.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 77.Kelly TM, Daley DC. Integrated treatment of substance use and psychiatric disorders. Soc Work Public Health. 2013;28:388–406. doi: 10.1080/19371918.2013.774673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav. 2012;37:11–24. doi: 10.1016/j.addbeh.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Riggs PD. Treating adolescents for substance abuse and comorbid psychiatric disorders. Sci Pract Perspect. 2003;2:18–29. doi: 10.1151/spp032118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Baker KD, Lubman DI, Cosgrave EM, Killackey EJ, Yuen HP, Hides L, et al. Impact of co-occurring substance use on 6 month outcomes for young people seeking mental health treatment. Aust N Z J Psychiatry. 2007;41:896–902. doi: 10.1080/00048670701634986. [DOI] [PubMed] [Google Scholar]
- 81.Judd PH, Thomas N, Schwartz T, Outcalt A, Hough R. A dual diagnosis demonstration project: Treatment outcomes and cost analysis. J Psychoactive Drugs. 2003;35(Suppl 1):181–92. doi: 10.1080/02791072.2003.10400513. [DOI] [PubMed] [Google Scholar]
- 82.Luoto KE, Koivukangas A, Lassila A, Kampman O. Outcome of patients with dual diagnosis in secondary psychiatric care. Nord J Psychiatry. 2016;70:470–6. doi: 10.3109/08039488.2016.1160149. [DOI] [PubMed] [Google Scholar]
- 83.Van Stelle KR, Blumer C, Moberg DP. Treatment retention of dually diagnosed offenders in an institutional therapeutic community. Behav Sci Law. 2004;22:585–97. doi: 10.1002/bsl.602. [DOI] [PubMed] [Google Scholar]


