Case Report
A 72-year-old man with a history of thoracic endovascular aortic repair 8 months before admission presented with a 2-day history of odynophagia without bleeding. With the exception of a heart rate of 130 BPM and a white blood cell count of 17.4 × 109/L, all other vital signs and laboratory test results at this time were within normal limits. Computed tomography revealed a Type B aortic dissection with focal outpouching containing small bubbles of gas arising from the thrombosed lumen of the aorta at the level of T6, suggesting possible aortoesophageal fistula (Figure 1). Esophagogastroduodenoscopy performed the next day showed nonbleeding ulcer in the proximal esophagus (Figure 2). Because aortoesophageal fistula was suspected at the time of esophagogastroduodenoscopy, biopsy and brushings of the aortic ulcer were not obtained.
Figure 1.
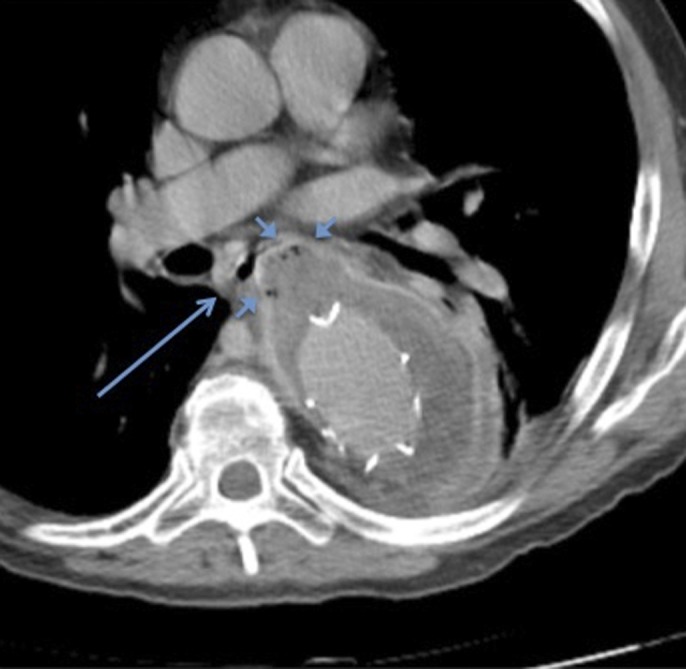
Axial contrast-enhanced computed tomography of the chest showing repair of descending thoracic aortic dissection with aortic stent-graft. The presence of mural thrombus within the false lumen of the aneurysmally dilated descending thoracic aorta is seen along with focal outpouching of the aneurysm sac containing small foci of gas (short arrows) adjacent to the esophagus (long arrow).
Figure 2.

Esophagoduodenoscopy showing nonbleeding ulcer in the proximal esophagus.
Two days after presentation, the patient underwent surgical explant of the thoracic endograft, drainage of a periaortic abscess, and repair of an esophageal fistula between the thrombosed aortic aneurysm sac and the proximal esophagus. Cultures obtained from the periaortic abscess contained Streptococcus viridans species.
The postoperative course was initially complicated by acute renal failure requiring hemodialysis. On postoperative day 10, the patient was noted to have respiratory distress and left-sided thoracic and cervical subcutaneous emphysema, necessitating operative placement esophageal stenting (Figures 3 and 4). He subsequently developed left-sided pleural effusion containing Pseudomonas aeruginosa. After further decompensation and worsening delirium, the patient died on postoperative day 29.
Figure 3.
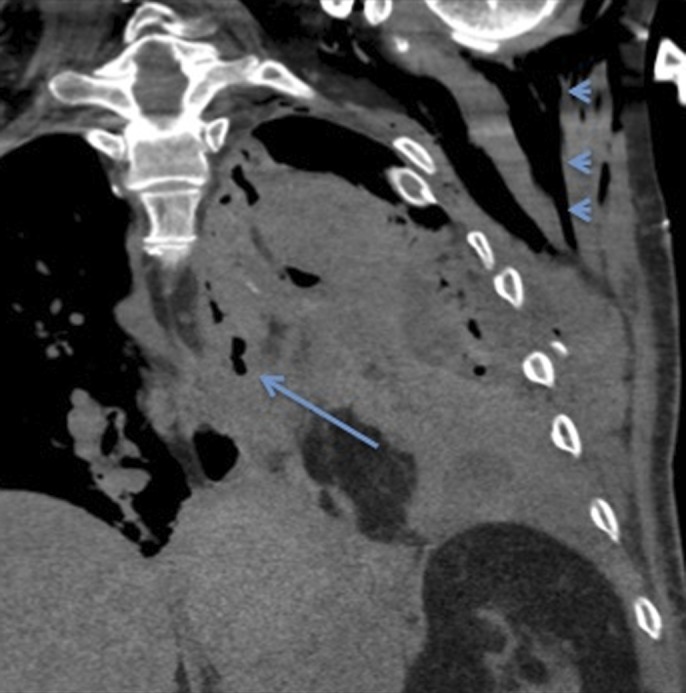
Coronal noncontrast computed tomography of the chest showing foci of gas adjacent to the esophagus (long arrow) following repair, concerning for leak. Extensive subcutaneous emphysema (arrowheads) and left-sided pneumothorax are also observed.
Figure 4.
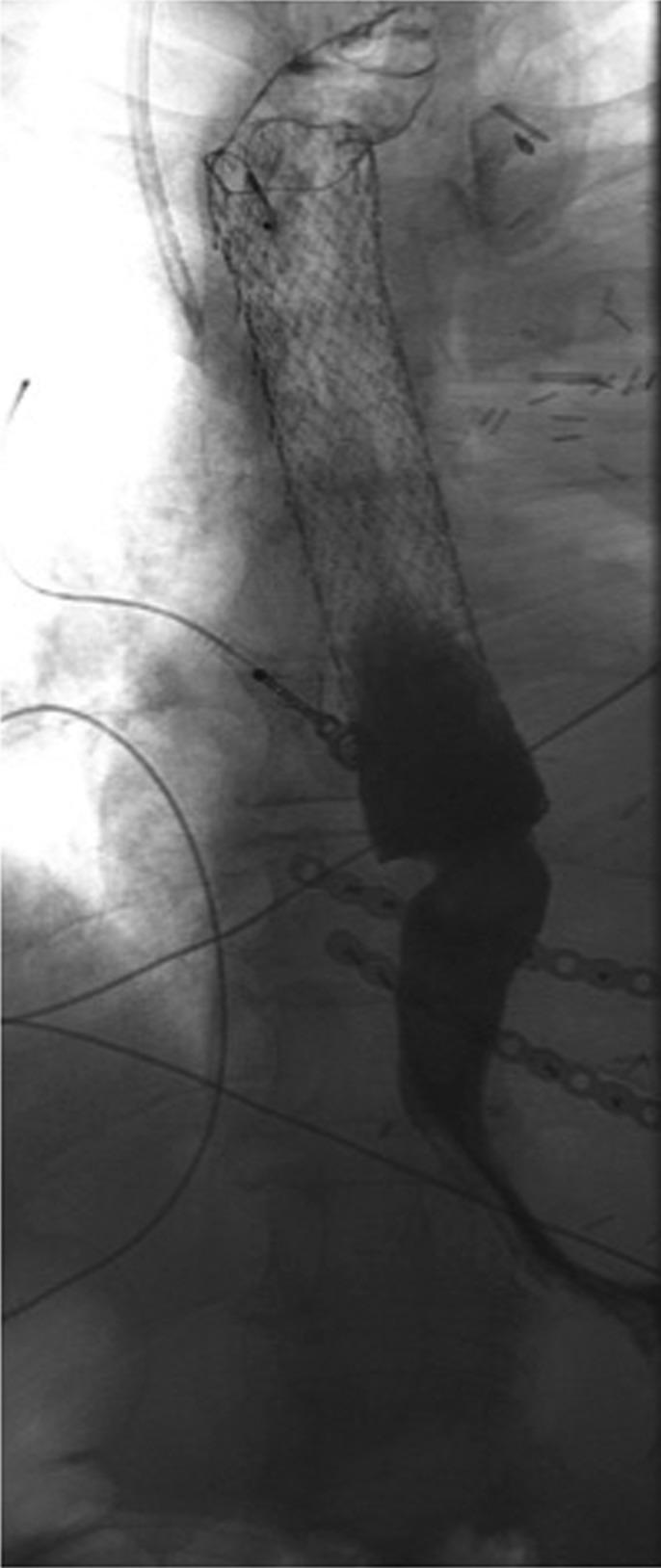
Single-contrast esophagram showing the absence of esophageal leak after repair with metallic stent.
Aortoenteric fistula (AEF) is an abnormal communication between the aorta and an adjacent loop of the bowel. AEF may arise de novo (primary) but is more commonly a complication of aortic reconstructive surgery, occurring in approximately 2% of all patients who undergo thoracic endovascular aortic repair, with most cases presenting within 1 year of surgery.1 These secondary AEFs are believed to be formed most frequently through the combination of chronic low-grade infection of the aortic graft and repetitive pressure on the intestine from aortic pulsations.2 AEFs are most likely to arise in the second part of the duodenum because of the close proximity between the aorta and the intestine and the relative abundance of abdominal aortic aneurysm repairs.3 More rare than aortoduodenal fistulae, aortoesophageal fistulae are associated with both thoracic aortic aneurysm (54% of cases) and esophageal impaction (19% of cases).3
Patients with aortoesophageal fistulae classically present with midthoracic pain, sentinel arterial hemorrhage, and exsanguination after a symptom-free interval (Chiari's Triad).4 Computed tomography is the preferred diagnostic modality because of cost, expediency, and safety.2 Even for those patients who are stable at the time of presentation, postsurgical mortality of aortoesophageal fistula repair historically approaches 100%.1 However, the recent use of covered self-expandable metal stents in a small case series of AEFs has been shown to prolong survival through tamponade of bleeding and avoidance of emergent surgical procedures.5
This nonclassic presentation of aortoesophageal fistula secondary to infected thoracic aortic endograft was notable for proximal aortic erosion without hemorrhage, an extremely rare occurrence. The most likely explanation is that the relatively small aortic fistula was completely insulated from high-pressure aortic blood flow by preexisting aneurysmal thrombus. This case illustrates the principle that aortoesophageal fistula should be suspected in patients with a history of aortic aneurysm who present with esophageal symptoms, even without evidence of hemorrhage.
Disclosures
Author contributions: RCK Wong is the article guarantor. DB Karb wrote the manuscript. E. Mansoor, J. Sullivan, J. Gollamudi, and RCK Wong edited and approved the manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Eggebrecht H, Mehta RH, Dechene A, et al. Aortoesophageal fistula after thoracic aortic stent-graft placement: A rare but catastrophic complication of a novel emerging technique. JACC Cardiovasc Interv. 2009;2(6):570–6. [DOI] [PubMed] [Google Scholar]
- 2.Xiromeritis K, Dalainas I, Stamatakos M, Filis K. Aortoenteric fistulae: Present-day management. Int Surg. 2011;96(3):266–73. [DOI] [PubMed] [Google Scholar]
- 3.Hollander JE, Quick G. Aortoesophageal fistula: A comprehensive review of the literature. Am J Med. 1991;91(3):279–87. [DOI] [PubMed] [Google Scholar]
- 4.Heckstall RL, Hollander JE. Aortoesophageal fistula: Recognition and diagnosis in the emergency department. Ann Emerg Med. 1998;32(4):502–5. [DOI] [PubMed] [Google Scholar]
- 5.Rodrigues-Pinto E, Pereira P, Vilas-Boas F, Peixoto A, Silva M, Macedo G. Esophageal stents in aortoesophageal fistulas—Anecdotal experiences or new armamentarium? Am J Gastroenterol. 2017;112:1343. [DOI] [PubMed] [Google Scholar]


