ABSTRACT
Esophageal squamous cell carcinoma (ESCC) is the predominant type of esophageal carcinoma worldwide. It occurs mostly in the upper and middle thirds of the esophagus. We present the case of a young African American woman with Goltz syndrome who presented with dysphagia and weight loss and was found to have distal esophageal papillomatosis and squamous cell carcinoma. This occurrence of ESCC in an atypical location in a young woman without traditional risk factors is suggestive of malignant transformation of underlying papillomatosis. Goltz syndrome is a rare disorder, occasionally associated with esophageal papillomatosis. Although esophageal papillomatosis is considered to be benign, our case shows that it could have malignant potential and hence is likely worthy of surveillance.
INTRODUCTION
Esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC) together constitute most of the histological subtypes of esophageal cancers. ESCC is the predominant histological pattern worldwide and occurs primarily in the upper and middle one-third of the esophagus.1 Although its incidence in the United States has been declining compared with EAC, ESCC remains more common in older African American men who consume tobacco and alcohol.2 Other risk factors of ESCC include drinking hot beverages, preexisting structural diseases (such as achalasia and caustic strictures), and human papillomavirus infection.3 Some case reports have also highlighted the possibility of development of malignancy in association with squamous papillomas of the esophagus,4–9 with the latter by itself being a rare occurrence.10,11 Goltz syndrome is a rare genetic disorder that causes mucocutaneous papillomatosis, occasionally involving the esophagus.12 To date, there are no reports of malignancy in Goltz syndrome.
CASE REPORT
A 37-year-old African American woman with a medical history of Goltz syndrome presented to the hospital with progressive dysphagia, poor appetite, weight loss, and shortness of breath. Two months before this admission, the patient was in her usual state of health when she started experiencing dysphagia that progressed to the extent that she began regurgitating her meals. Severe dysphagia and reduced appetite led to poor oral intake and loss of 15 lbs of weight over 2 months. She denied odynophagia, heartburn, melena, or similar episodes in the past. She was not on any daily medications. Her surgical history was remarkable for resection of multiple benign facial and labial papillomas as a teenager. The patient worked as a care partner in a medical facility until her new-onset illness and lived with her family. She had never consumed tobacco or alcohol and did not use illicit drugs. There was no family history of gastrointestinal cancers.
On physical examination, the patient appeared cachectic with stable vital signs. Her heart, lung, and abdominal examination was benign. Musculoskeletal examination revealed oligodactyly and lobster-claw deformities in her hands and feet (Figure 1). Her skin was notable for patches of hypopigmentation and hyperpigmentation on the arms and chest (Figure 2).
Figure 1.
Musculoskeletal examination revealed oligodactyly and lobster claw deformities in her hands (A) and feet (B).
Figure 2.

Skin examination revealed patches of hypopigmentation and hyperpigmentation on the arms and chest.
Laboratory evaluation was remarkable for hemoglobin of 6.5 g/dL.
A chest x-ray was obtained in the emergency department and showed no acute pulmonary abnormality, but a mass in the region of the gastric cardia. A computed tomography scan of the abdomen with contrast revealed a large, 5.7-cm gastric mass, distal esophageal thickening, and upper abdominal lymphadenopathy (Figure 3). Esophagogastroduodenoscopy showed subtle distal esophageal papillomas and a large, pedunculated mass arising from the gastroesophageal (GE) junction and extending into the gastric fundus (Figure 4). Endoscopic ultrasound (EUS) showed a large pedunculated mass beginning at the GE junction and prolapsing into the gastric fundus (Figure 5). The mass involved all the esophageal layers including the adventitia and appeared to encase the aorta and abut the pleura indicating an invasive tumor. Two enlarged nodes were noted in the distal esophagus and one in the celiac region. EUS staging was noted to be at least T3N2. Pathologic evaluation of biopsy specimens from the mass revealed moderately differentiated invasive squamous cell carcinoma, and a polyp, also at the GE junction and close to the mass, showed features of a benign squamous papillary lesion (Figure 6). On the basis of the EUS-visualized aortic and pleural involvement, the tumor was initially considered to be surgically unresectable until a positron emission tomography scan ruled out metastatic disease. The patient was started on a concurrent platinum-based chemoradiation therapy. Re-staging positron emission tomography scan performed after 4 cycles showed excellent disease response and the patient underwent transhiatal esophagectomy with cervical esophagogastrostomy. Surgical pathology showed complete response to therapy and no residual viable tumor was identified. Pathologic staging was ypT0tpN0. The patient is 12 months post-procedure now and continues to do well.
Figure 3.
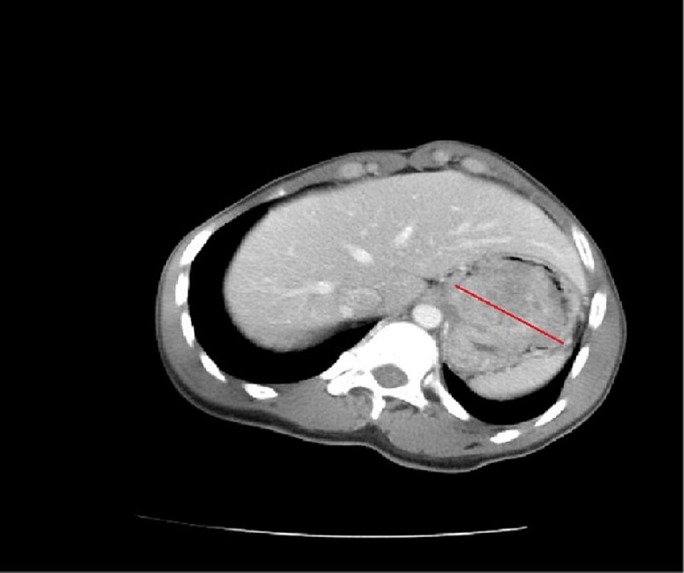
Computed tomography of the abdomen with contrast showing the gastric mass.
Figure 4.

Esophagogastroduodenoscopy showing subtle distal esophageal papillomas and a large, pedunculated mass arising from the gastroesophageal junction and extending into the gastric fundus.
Figure 5.

Endoscopic ultrasound showing a large pedunculated mass beginning at the gastroesophageal junction and prolapsing into the gastric fundus.
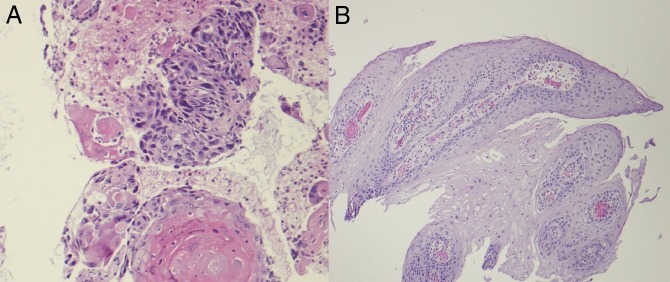
Figure 6.
Pathologic evaluation of biopsy specimens from (A) abdominal mass revealing moderately differentiated invasive squamous cell carcinoma and (B) polyp at the gastroesophageal junction showing characteristics of a benign squamous papillary lesion.
DISCUSSION
Focal dermal hypoplasia, also known as Goltz syndrome, is a rare X-linked dominant disorder caused by a mutation in the PORCN gene located on the X chromosome (p11.23).13,14 PORCN encodes the human homolog of Drosophila melanogaster porcupine, an endoplasmic reticulum protein involved in the processing of proteins of the Wingless-related integration site or Wnt signaling pathway. This pathway is critical in the embryonic development of mesoectodermal structures including skin, craniofacial and long bones, eyes, and teeth. Hence, the dysregulation of this pathway results in a wide array of multisystemic manifestations involving the skin (reticular hyperpigmentation or hypopigmentation, atrophy, telangiectasias, and papillomas), skeleton (syndactyly, ectrodactyly, hypoplasia or aplasia of truncal skeleton), eyes (coloboma, microphthalmia), mucous membranes (raspberry papillomas), and teeth (small, malformed, or absent teeth).15–18 There are approximately 300 cases of Goltz syndrome reported to date worldwide, and the majority are women (90%) because the disease carries a high rate of in utero lethality in males.19
Although mucocutaneous papillomas involving the mouth, nose, larynx, vagina, and rectum were observed in 45%–65% of the cases, esophageal papillomas seem to be particularly infrequent.20,21 Per literature review, there are only 5 cases of esophageal papillomas associated with Goltz syndrome.12,22–25 Similar to our patient, all previously reported cases had a degree of dysphagia requiring endoscopic therapy. However, all cases had squamous papillomas without dysplasia, in contrast to our patient who was found to have ESCC. Hence, papillomatosis associated with Goltz syndrome has been considered nonmalignant, and there are no recommendations for surveillance. Given the fact that ESCC occurs mostly in the upper and middle one-third of esophagus vs EAC in the distal one-third and the GE junction, this occurrence of ESCC in an atypical location in a young woman without traditional risk factors is suggestive of malignant transformation of underlying papillomatosis. Our case shows that papillomas associated with Goltz syndrome could have malignant potential and therefore are worthy of surveillance. To our knowledge, this is the first reported case of esophageal cancer associated with Goltz syndrome.
DISCLOSURES
Author contributions: M. Hafiz wrote the manuscript, and is the article guarantor. S. Sundaram, AR Naqash, and P. Walker wrote the manuscript. J. Speicher and N. Talaat edited the article. A. Sutton conducted histopathological analysis and contributed pathology images.
Financial disclosure: None to report.
Previous presentation: The case report was presented at World Congress of Gastroenterology at ACG2017; October 13–18, 2017; Orlando, FL.
Informed consent was obtained for this case report.
REFERENCES
- 1.Napier KJ, Scheerer M, Misra S. Esophageal cancer: A review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol. 2014;6(5):112–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prabhu A, Obi K, Lieberman D, Rubenstein JH. The race-specific incidence of esophageal squamous cell carcinoma in individuals with exposure to tobacco and alcohol. Am J Gastroenterol. 2016;111(12):1718–25. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19(34):5598–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Attila T, Fu A, Gopinath N, Streutker CJ, Marcon NE. Esophageal papillomatosis complicated by squamous cell carcinoma. Can J Gastroenterol. 2009;23(6):415–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reed PA, Limauro DL, Brodmerkel GJ, Jr, Agrawal RM. Esophageal squamous papilloma associated with adenocarcinoma. Gastrointest Endosc. 1995;41(3):249–51. [DOI] [PubMed] [Google Scholar]
- 6.Waluga M, Hartleb M, Sliwinski ZK, Romanczyk T, Wodolazski A. Esophageal squamous-cell papillomatosis complicated by carcinoma. Am J Gastroenterol. 2000;95(6):1592–3. [DOI] [PubMed] [Google Scholar]
- 7.Narayani RI, Young GS. Recurrent proximal esophageal stricture associated with dysplasia in squamous cell papillomatosis. Gastrointest Endosc. 2002;56(4):591–4. [DOI] [PubMed] [Google Scholar]
- 8.Reynoso J, Davis RE, Daniels WW, Awad ZT, Gatalica Z, Filipi CJ. Esophageal papillomatosis complicated by squamous cell carcinoma in situ. Dis Esophagus. 2004;17(4):345–7. [DOI] [PubMed] [Google Scholar]
- 9.Wolfsen HC, Hemminger LL, Geiger XJ, Krishna M, Woodward TA. Photodynamic therapy and endoscopic metal stent placement for esophageal papillomatosis associated with squamous cell carcinoma. Dis Esophagus. 2004;17(2):187–90. [DOI] [PubMed] [Google Scholar]
- 10.Mosca S, Manes G, Monaco R, Bellomo PF, Bottino V, Balzano A. Squamous papilloma of the esophagus: Long-term follow up. J Gastroenterol Hepatol. 2001;16(8):857–61. [DOI] [PubMed] [Google Scholar]
- 11.Orlowska J, Jarosz D, Gugulski A, Pachlewski J, Butruk E. Squamous cell papillomas of the esophagus: Report of 20 cases and literature review. Am J Gastroenterol. 1994;89(3):434–7. [PubMed] [Google Scholar]
- 12.Kashyap P, Sweetser S, Farrugia G. Esophageal papillomas and skin abnormalities: Focal dermal hypoplasia (Goltz syndrome) manifesting with esophageal papillomatosis. Gastroenterology. 2011;140(3):784, 1111. [DOI] [PubMed] [Google Scholar]
- 13.Wang X, Reid Sutton V, Omar Peraza-Llanes J, et al. Mutations in X-linked PORCN, a putative regulator of Wnt signaling, cause focal dermal hypoplasia. Nat Genet. 2007;39(7):836–8. [DOI] [PubMed] [Google Scholar]
- 14.Grzeschik KH, Bornholdt D, Oeffner F, et al. Deficiency of PORCN, a regulator of Wnt signaling, is associated with focal dermal hypoplasia. Nat Genet. 2007;39(7):833–5. [DOI] [PubMed] [Google Scholar]
- 15.Wright JT, Puranik CP, Farrington F. Oral phenotype and variation in focal dermal hypoplasia. Am J Med Genet C Semin Med Genet. 2016;172C(1):52–8. [DOI] [PubMed] [Google Scholar]
- 16.Bree AF, Grange DK, Hicks MJ, Goltz RW. Dermatologic findings of focal dermal hypoplasia (Goltz syndrome). Am J Med Genet C Semin Med Genet. 2016;172C(1):44–51. [DOI] [PubMed] [Google Scholar]
- 17.Goltz RW. Focal dermal hypoplasia syndrome: An update. Arch Dermatol. 1992;128(8):1108–11. [PubMed] [Google Scholar]
- 18.Goltz RW, Henderson RR, Hitch JM, Ott JE. Focal dermal hypoplasia syndrome: A review of the literature and report of two cases. Arch Dermatol. 1970;101(1):1–11. [DOI] [PubMed] [Google Scholar]
- 19.Bostwick B, Van den Veyver IB, Sutton VR. Focal dermal hypoplasia. In: Adam MP, Ardinger HH, Pagon RA, et al. (eds). GeneReviews®. Washington, Seattle (WA): University of Washington, Seattle; May 15, 2008; updated July 21, 2016. https://www.ncbi.nlm.nih.gov/books/NBK1543. Accessed on February 14, 2019. [Google Scholar]
- 20.Rhee KY, Baek RM, Ahn KJ. Airway management in a patient with focal dermal hypoplasia. Anesth Analg. 2006;103(5):1342. [DOI] [PubMed] [Google Scholar]
- 21.Gordjani N, Herdeg S, Ross UH, Grimme H, Kleinschmidt M, Brandis M. Focal dermal hypoplasia (Goltz-Gorlin syndrome) associated with obstructive papillomatosis of the larynx and hypopharynx. Eur J Dermatol. 1999;9(8):618–20. [PubMed] [Google Scholar]
- 22.Brinson RR, Schuman BM, Mills LR, Thigpen S, Freedman S. Multiple squamous papillomas of the esophagus associated with Goltz syndrome. Am J Gastroenterol. 1987;82(11):1177–9. [PubMed] [Google Scholar]
- 23.Pasman EA, Heifert TA, Nylund CM. Esophageal squamous papillomas with focal dermal hypoplasia and eosinophilic esophagitis. World J Gastroenterol. 2017;23(12):2246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zala L, Ettlin C, Krebs A. [Focal dermal hypoplasia with keratoconus, papillomatosis of esophagus and hidrocystomas (author's transl)]. Dermatologica. 1975;150(3):176–85. German. [PubMed] [Google Scholar]
- 25.Bertani H, Mirante VG, Caruso A, Manno M, Brancaccio ML, Conigliaro R. Successful treatment of diffuse esophageal papillomatosis with balloon-assisted radiofrequency ablation in a patient with Goltz syndrome. Endoscopy. 2014;46(Suppl 1):E404–5. [DOI] [PubMed] [Google Scholar]