Abstract
Optimal care of the patient with hepatocellular carcinoma (HCC) necessitates the involvement of multiple providers. Because the patient with HCC often carries 2 conditions with competing mortality risks (cancer and underlying cirrhosis), no single provider is equipped to deal with all of these patients’ needs adequately. Multidisciplinary teams (MDTs) have evolved to facilitate care coordination, reassessments of clinical course, and nimble changes in treatment plans required for this complex group of patients. Providers or sites that elect to manage patients with HCC thus are increasingly aware of the need to build their own MDT or communicate with an established one. The availability of new communication technologies, such as teleconferencing or teleconsultation, offers the possibility of MDT expansion into underserved or rural areas, as well as areas such as correctional facilities. Although the availability of resources for HCC patient care varies from site to site, construction of an MDT is possible in a wide spectrum of clinical practices, and this article suggests a blueprint for assembly of such collaboration. Research strategies are needed to explain how MDTs improve clinical outcomes so that MDTs themselves can be improved.
Keywords: HCC, Hepatocellular Carcinoma, Liver Cancer, Multidisciplinary Team
Advances in diagnostics, surgery, technology, and pharmaceuticals have altered the way cancer is managed. The number and sophistication of treatments has grown such that no single specialty offers the complete spectrum of care. Quality cancer management increasingly depends on patient access to multimodality therapy and timely evaluation and treatment from an array of specialized professionals. A limitation of this specialized approach is that it requires effective and simultaneous communication between providers to ensure coordinated treatment. One organizational structure that has evolved to provide the coordination and communication necessary for contemporary cancer management is the multidisciplinary team (MDT).1
Multidisciplinary Team Definitions
MDTs provide health services through at least 2 health providers working collaboratively with patients and their caregivers to achieve coordinated care.2 This definition, however, needs further clarification if it is to be useful for measuring outcomes as well as for making policy decisions. We suggest a more specific definition. A liver MDT should consist of at least one representative from each specialty of providers who care for patients with liver tumors at a particular institution, and meets regularly as a group to make consensus diagnostic and management recommendations for this group of patients. It is important for this meeting to be regular (once a week for larger institutions, perhaps every 2 to 4 weeks for smaller institutions, depending on case volume), and to include all provider types. In this way input from multiple, independent providers may be obtained. Such regular meetings may occur in the context of a specific clinic day when the patient is seen by multiple providers, or at a regular conference in which providers meet in absence of patients. Although widely regarded to have beneficial effects on patient care, data to support this claim for liver MDTs are lacking. A more rigorous definition will allow centers to bring uniformity to liver MDTs and subsequently track outcomes related to the entity. This is important because MDTs already are becoming the standard of care worldwide for treatment of multiple cancers, driven in part by the publication of national guidelines recommending their use and composition.3
Benefits of a Multidisciplinary Team for Management of Hepatocellular Carcinoma
MDTs are particularly relevant for the management of hepatocellular carcinoma (HCC), the most common primary liver cancer and a multifaceted disease with a poor prognosis. The treatment of HCC is multimodal, with options that vary by center and include surgical resection, orthotopic liver transplantation (OLT), in situ ablation, transarterial therapies (chemoembolization or radiotherapy), and targeted molecular therapies. Because most HCCs develop in the setting of chronic liver disease,4 risk of death involves tumor- and nontumor-related factors,5 emphasizing the importance of OLT as the most comprehensive and likely curative therapy. As such, a roadmap to OLT needs to be outlined for eligible patients. Advances in screening awareness and diagnostics also have allowed HCC to be diagnosed at earlier stages when more effective non-OLT treatments are available. This necessitates the involvement of multiple specialists (eg, hepatobiliary surgeon, hepatologist, oncologist, radiologist, and transplant physician/surgeon) to provide individualized treatment strategies. These providers must find ways to coordinate treatment recommendations and to collaborate on how to best manage patients within the confines of local resources.5,6 The use of an MDT is one way to accomplish this task. By coordinating resources and minimizing communication failures, MDTs can route patients quickly and efficiently to appropriate therapeutic regimens and thereby optimize outcomes. As mentioned earlier, regular meetings are key to the success of the liver MDT. Regular meetings provide many benefits, such as: (1) input from all types of available providers for each case—key input frequently is elicited from providers who may not have otherwise been consulted; (2) development of a comprehensive treatment plan involving 2 or more providers—a difficult and time-consuming proposition in the absence of regular real-time meetings; (3) minimization of communication errors between providers and delays in treatment as a result of such miscommunications; (4) uniformity in treatment approach over time; (5) forum to address difficult questions in which a group consensus recommendation can strengthen patient and provider confidence in the management plan; and (6) significantly increase provider awareness about new research in related fields—for example, the hepatologist keeps the group current on hepatology issues relevant to HCC, while the interventional radiologist keeps the group current on specific treatment technologies, and the oncologist updates the group on available clinical trials with new medications. The earlier-described benefits of a liver MDT would not be expected to materialize from usual provider-to-provider communication regarding care of a specific patient. Because management is so complex, we favor initial presentation of every patient with HCC at the liver MDT, to outline a comprehensive management plan. However, liver MDT providers will be able to expedite some straightforward cases without formal presentation to the group precisely because they are regular attendees and familiar with the group practice and current research. Such expediency is necessary in light of the ballooning numbers of patients with HCC.
The window of time for HCC treatment is short, with end-organ liver dysfunction contributing significantly to complications and mortality. Therefore, the role of MDTs in enabling efficient and rapid connection of patients with treatment is essential.5
The increasing incidence of HCC7–9 is expected to continue,10 and MDTs consequently are expected to become even more important. Reasons behind the increase in HCC incidence include effects of the hepatitis C virus epidemic11,12 as well as the increasing incidence of nonalcoholic steatohepatitis–associated HCC.13–15
Given that the health care burden of HCC continues to increase, developing more effective management is paramount. In December 2012, we and other HCC experts gathered for a round-table discussion to identify best practices for developing an HCC-specific MDT. This article discusses the advantages of using MDTs for HCC treatment. The collaborators reviewed several MDTs and compiled a series of recommendations for creating and maintaining MDTs for treating HCC.
Current Hepatocellular Carcinoma Guidelines
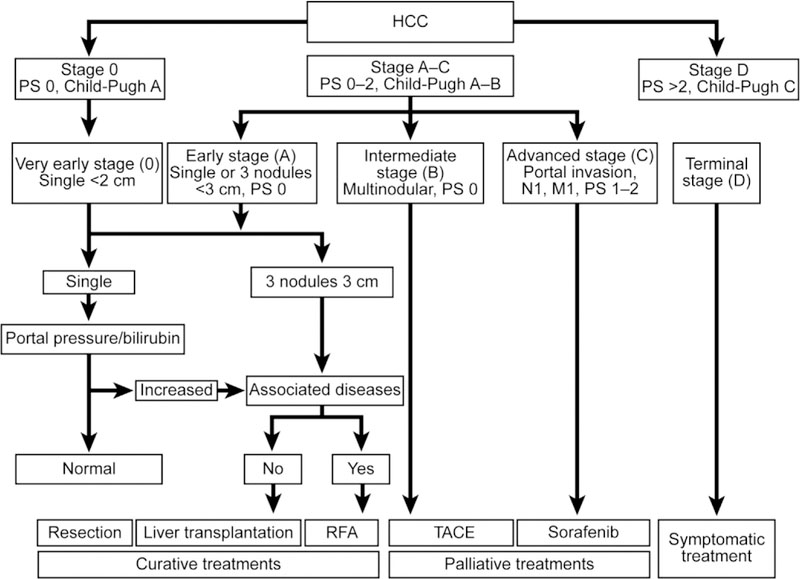
A liver MDT program should be able to provide the standard of care for HCC as encompassed by guidelines provided by authoritative national and international bodies. The American Association for the Study of Liver Diseases offers recommendations on the screening, treatment, and management of HCC.16 In addition, the Barcelona Clinic Liver Cancer (BCLC) staging system recommends treatments based on tumor stage, liver function, performance status, and the impact of treatment17 (Figure 1). Guidelines, although useful, must be adapted to fit areas of expertise at the local level. Many centers formalize an HCC treatment algorithm based on national guidelines but tailored to local expertise. Because liver transplant is one treatment option, contact with a center that performs liver transplantation strengthens the management strategy.
Figure 1.
BCLC staging system for HCC.16 M1, metastatic disease; N1, node positive; PS, performance score; RFA, radiofrequency ablation; TACE, transarterial chemoembolization. Reproduced with permission of John Wiley & Sons, Inc. Hepatology 2011;53:1020–1022.
Hepatocellular Carcinoma Management
According to the American Association for the Study of Liver Diseases Practice Guidelines for the management of HCC, the complexity of HCC disease indicates that it should be managed in multidisciplinary settings.16 However, multidisciplinary management is not being used to its full potential. A recent survey of physicians in the United States found that only 44% of physicians routinely adopted a multidisciplinary approach to treating HCC.18 A study of the Surveillance Epidemiology and End Results (SEER) database for patients with HCC used the number of specialists as a surrogate for multidisciplinary care, finding that 40% of patients with HCC saw only 1 provider and 37% saw 2 providers.19 Such estimates, however, have not been replicated in rigorous fashion, and moreover are complicated by a lack of a uniform definition of the liver MDT. Multicenter collaborations and comprehensive epidemiologic data are needed to understand the real proportion of patients with HCC receiving true MDT care, which as defined earlier is likely less than half. Multidisciplinary management is important because there are currently therapies available for several different stages of HCC, but judgments must be made by several different specialists before determining which therapies to use.10,16,20 Because HCC treatment is multimodal, an MDT likely will be the most effective approach. According to current treatment guidelines, an MDT should include hepatologists, pathologists, cross-sectional and interventional radiologists, surgeons, and medical and surgical oncologists.5,10,16 We sought to create a guideline that will help providers set up and fully use a liver MDT for the management of patients with HCC.
Clinical Evidence of the Advantages of Liver Multidisciplinary Teams for Hepatocellular Carcinoma Management
Research focused on liver MDT experiences has found that MDTs improve HCC screening, treatment, and
management. Through establishing a community-wide approach to treatment, an MDT allows for standardized screening procedures and can result in an earlier diagnosis of HCC.5,21,22 Chang et al20 noted that using an MDT significantly increased the number of patients who were evaluated for American Joint Committee on Cancer stages 1 and 2 HCCs that were amenable to curative or palliative treatment. The investigators conjectured that this was owing to improved screening, more awareness of atrisk individuals among clinicians, and better communication across specialties.
An MDT is also more likely to provide the most appropriate treatment to the individual patient. Lack of access to multidisciplinary care has been found to be a major contributor to lack of treatment in patients with HCC.18 A population-based cohort study that used data from the Surveillance Epidemiology and End Results Medicare-linked database showed that fewer than 30% of patients aged 65 years and older who were diagnosed with HCC received any therapy.23 A similar study found that palliative treatments such as transarterial chemoembolization and systemic chemotherapy were given to 13% to 23% and 11% to 14% of patients, respectively, who were not receiving curative treatment.24
Within a liver MDT, patients with HCC also will be more likely to receive appropriate treatments according to the current standard of care. The team also will be able to reach an agreement about treatment protocols and avoid unnecessary or inappropriate treatment, streamline diagnosis and prescriptions, as well as improve access to appropriate specialists and long-term follow-up evaluation.
Data also show that MDTs promote the rapid transfer of clinical information among the members of the treatment team, strengthening working relationships.21 In an evaluation of the early results of implementing a multidisciplinary management team for HCC at a Veterans Affairs Medical Center in San Francisco, data showed that the MDT improved patient outcome in several ways20: (1) the number of HCC referrals was doubled; (2) there was a significant increase in the number of patients evaluated for early stage HCC (from 14 to 75); (3) more patients received curative treatment (6% before vs 19% after) or palliative treatment (31% before vs 45% after); and (4) implementation of the MDT improved overall patient survival (from 21% to 65%). Overall, the investigators found that multidisciplinary collaboration and multimodal treatment led to improved outcomes when treating patients with HCC.20 Favorable outcomes were observed further in a study that assessed treatment allocation in a multidisciplinary subspecialty liver cancer clinic in San Francisco, in which 86% of patients that were evaluated received treatment for their disease.25
Setting up a Multidisciplinary Team
The appropriate strategy for a given center will depend on several factors, including local expertise and resources, proximity to an OLT center, the Organ Procurement and Transplantation Network region, and the demographics of the population being served. The strategies described here may serve as a guide; however, each center likely will tailor the exact characteristics to their particular needs and available resources.
Create Fertile Ground
It is important to convince the administration that the necessary resources are made available to the team. To do this, representatives from specialties that will support the MDT, preferably well-respected specialists who are in a position to inform changes and decisions, should be included in the meetings with hospital or clinic administration. This may include the medical director of the proposed group, liver treatment directors, a Chief Medical Officer, Board Members, and transplant administrators.
A strategic plan should be devised that includes an introduction with a background on HCC, the vision for the group, and the components that would make up the group, as well as enumerating the benefits and strengths of the MDT. Furthermore, the existing deficiencies that justify establishing the MDT, such as disorganized care and follow-up evaluation for patients with HCC, poor communication with referral sources, inadequate collaboration, and inability to adequately track outcomes, should be included in the strategic plan.
Establish Core Providers
Depending on the center, different providers will be available and willing to participate in an MDT. A commitment from these providers must be secured to meet on a regular basis. The meeting interval may be determined based on the number of patients that will be served, but should be no less often than monthly to allow timely review of cases. Providers in a liver MDT may include the following: a transplant hepatologist (ideal), hepatologist, or gastroenterologist; a transplant surgeon; a hepatobiliary surgeon; an interventional radiologist; a diagnostic body radiologist; a radiation oncologist; a medical oncologist; a pathologist; a palliative care specialist; and a nurse coordinator who is also an HCC specialist.
Administrative support is key to the success of an MDT program, and the program must include a nurse specialist in HCC or a hepatobiliary oncology specialist who will administer and coordinate the program. Recent data from an HCC MDT showed that a nurse coordinator position was critical for bringing patients into the MDT system, maintaining patient data, and ensuring that assessments, interventions, and follow-up visits were scheduled and completed efficiently.22 The authors also noted that additional support services may be provided by psychologists, social workers, and nutritionists.
Establish Relationships With Providers Outside the Multidisciplinary Team to Cover Local Deficiencies
OLT determines the treatment roadmap for a significant number of patients with HCC; therefore, a relationship with an OLT program is essential for any liver MDT. Any center that lacks an OLT facility will need to form an outside relationship with such a facility. Because transplantation for liver cancer depends on time accrued on the transplant list (US Department of Health and Human Services, Organ Procurement and Transplant Network Policy 3.6), it is beneficial for patients who are transplant candidates to be referred early in their cancer care to begin accrual of wait time.
Establish a Director or Co-directors of the Multidisciplinary Team
An MDT is a group of providers with different levels of experience arising from different specialties and departments. Such groups are most successful when decisions are reached through consensus, with a space for minority opinions to be expressed and considered.21 However, an acknowledged leader of the group is important to address matters of triage, control the agenda, and to make adjustments if patient presentations are not receiving adequate consideration. This leader also will guide the group in matters of local quality control and coordination with research and clinical trials, as well as provide direct outreach to the community that the group serves. Ideally, the leader or co-leaders will view themselves as facilitators and remain open to critical input from group members. Patients should be kept informed about the MDT approach throughout their treatment.22
Integrate the Multidisciplinary Team With Clinical Flow
Patients may enter the MDT through direct referrals to any of the specific MDT providers. After seeing an MDT provider, the patient’s case should be placed on the MDT agenda and presented at the next opportunity. At this time, recommendations for patient care may be made. Alternatively, patients may be referred to the MDT group with no specific MDT provider in mind. In this case, a triage system must be in place so that patients can be directed to the correct personnel. Triage can be performed primarily by any of the MDT providers, but ideally should be uniform and prompt, and the system should be specific to the needs of the institution.
Triage can be managed by a nurse coordinator or other equivalent medical assistant. This person will be responsible for examining referrals. If appropriate for the situation, the relevant data then can be recorded on a single standardized form, which will allow the busy provider to quickly make triage decisions about patients referred to the MDT conference/clinic. Too much information will slow down the provider as well as the personnel performing the record review, while too little information will lead to ineffective triage. The end point of triage should be recommendations of the MDT provider(s) during the initial patient visit, clarity on the urgency of the case, and any further studies or tests the patient should receive in the interim or at the time of being seen by the MDT provider.
Staging System
It is important that the MDT providers agree on a particular staging system for HCC. Dedicated use of one system will help guide treatment decisions over time and create common ground for discussing treatment options and prognostic information. It is highly recommended that the group use an HCC staging system that includes characteristics of the tumor and the state of any concurrent liver disease. Current validated systems that include both tumor and liver characteristics include the BCLC, Cancer of the Liver Italian Program, Okuda, Groupe d’Etude et de Traitement du Carcinome Hepatocellulaire, and the Chinese University Prognostic Index.10 Although the most widely used staging system is the BCLC staging system, each MDT should determine the best system for their particular situation.
Multidisciplinary Team Treatment Algorithm
Once the MDT has agreed upon a particular staging system, group members should become familiar with current standards of care relevant to their specialty with regards to the various stages of HCC, and together produce a brief outline of how the team will handle patients at all stages of the disease. This local algorithm should take into account the particular expertise of the MDT and make allowances for eventualities in which help outside the MDT may be warranted, including referral to a transplant center. The goal of the algorithm should be to create a pathway for patients at all stages of HCC, to streamline the MDT process and, over time, standardize treatments. It is necessary to update the algorithm periodically as new treatments and paradigms emerge, or when expertise within the MDT group changes.
Operating a Multidisciplinary Team in Real Time
The MDT must be efficient, or participation from members of the MDT team will diminish. An agenda should be created for each MDT meeting. This agenda should provide details about each patient and the relevant clinical data. It can be made in advance by the nurse coordinator or other medical assistant.
There are a few basic principles that may help to maintain efficiency. These include the following. First, it is necessary to identify the first case: The general flow may begin with the designated leader or chair of the MDT identifying the first case, followed by a brief clinical vignette presented by one of the providers who has seen the patient, followed by a radiology review, a discussion, and, lastly, a consensus decision. Second, a standardized, 1-page form should be used. This form may be useful for recording the relevant facts, including the clinical/laboratory characteristics that determine liver function, tumor characteristics for staging, and the tumor stage, as well as a very brief summary and the group’s consensus recommendations. This form should be readily accessible in the event the patient is re-presented in the MDT. Third, a summary must be generated. After the MDT conference, the coordinator may create a brief summary statement based on the completed form and enter this into the patient’s electronic medical record. The primary provider for the patient or the MDT nurse coordinator then should contact the patient to relay the recommendations of the MDT, and the coordinator and the patient can discuss how to best proceed, based on patient preference. Fourth, final recommendations must be made. A letter to the referring physician should briefly describe the recommendations of the MDT and make note of the communication with the patient and the agreed-upon plan.
Finally, the question of how and whether to document the proceedings and recommendations of the MDT has plagued such groups. Traditional clinical documentation platforms are not well suited to the MDT. Concerns have been voiced about opening up providers or institutions to liability if MDT proceedings are recorded in the patient’s medical record. However, there may be equal concerns about liability if an MDT made recommendations that were not documented. It seems clear that the best thing for patient care is clear documentation, and our own MDTs document recommendations. To the best of our knowledge there have been no successful lawsuits regarding this issue. Methods of documentation vary widely, and this is an important part of the MDT field in evolution. Standardization of MDT documentation is necessary, both for patient care and outcomes research, and this certainly will evolve in the next several years.
Future Challenges for Liver Multidisciplinary Teams
Virtual Multidisciplinary Teams
The lack of access to specialty care to underserved patients and areas26,27 is a barrier to the implementation of the concept that all patients with cancer, no matter where they live and to whom they are referred, should have equal access to high and uniform standardized care. Many cancer MDTs have incorporated the use of telemedicine or teleconferencing to close the gap of access, and virtual participation of other providers in the presentation and discussion of cancer cases has allowed for the extension and expansion of MDTs. All relevant sites are linked through telemedicine technology so that the team can meet using real-time videoconferencing to share knowledge. Ideally, each site would have up-to-date videoconferencing equipment so that high-quality video and audio can be projected, as well as detailed images, such as pathology slides or radiologic scans. The use of telehealth technology is especially relevant for centers that lack full resources because this would allow communication with the necessary specialists that are not available at the local site. The next step to possibly reduce some of the logistical problems with starting and maintaining participation in the face-to-face MDT meetings is to move forward to a fully virtual MDT (vMDT). The definition and characteristics of such an entity have been described in a recent report from Munro and Swartzman,28 which defined the concept of truly vMDT as the following: (1) non–co-location (MDT members are not present in the same room); (2) asynchronous participation (attendees dropping in and out of a continuing discussion); (3) variable composition (core members may co-opt additional temporary members as indicated by the specific problem); (4) unbounded geography; and (5) diversified platform (with the availability of increasing bandwidth it will be possible to include videoclips, notes, images, and virtual microscopy). We conclude that the complete replacement of the traditional face-to-face MDT with vMDT in cancer management is unlikely at this time owing to challenges in setting up vMDTs, which may include finding quality equipment, connecting the correct personnel, and setting up a structure for reimbursement.
Bioinformatics
One of the difficulties facing providers working within a liver MDT is the large amount of information that must be processed. Many patients are referred to MDTs from outside providers, therefore data-gathering represents a significant time investment. There is also a lack of standardized documentation of MDT proceedings. Notes from MDTs typically are scant in data and only briefly mention recommendations. Later care of the patient may be more difficult because of a lack of documentation. As the bioinformatics field advances, MDT providers need to be involved in such efforts so that a more comprehensive MDT note can be generated with a minimum of extra work.
Reimbursement
Most MDTs receive little or no funding from the clinical operation, and what they do receive is vulnerable. As an example, the University of California at Los Angeles Medical Center eliminated funding for the salary of a nurse practitioner in an MDT29 even though the program showed successful outcomes.30–32
Providers must donate the extra time and effort to make the MDT a reality. As cost and time restraints increase, hospitals will need to find a way to reimburse providers and support staff of the MDT for this service. Justifying the resources to sponsoring institutions will depend on showing the magnitude of downstream revenue and/or showing improved patient outcomes as the result of MDT use. This is a challenging task given the complexity of patient care. Although it makes sense that MDT care of patients with HCC results in better patient care, better provider communication and thus streamlining of work, and more targeted (and expensive) therapy thus bringing more revenue to hospitals, data supporting these claims are scant. Ideally, a before and after MDT implementation financial analysis would be performed, or even a comparison of different medical systems (with and without MDTs for HCC), to better understand if it makes sense to support MDTs from the institutional point of view.
Some data can be gathered easily, however, and points to the magnitude of medical resources associated with patients involved with liver MDTs. Figure 2 shows the number of cases seen in a weekly MDT conference (Oregon Health and Science University) over the past 3 years, averaging approximately 550 case presentations per year. Approximately one quarter are new HCC cases, while 40% are repeat presentations, (presentation for ongoing HCC management after an initial plan has been enacted). The remainder of the cases are non-HCC malignancies and difficult hepatobiliary problems. That a multidisciplinary group of providers (10–15 in this instance) meets weekly for 1 to 2 hours with little or no support (salary or otherwise) from the institution attests to the perceived benefit of involved providers. A similar pattern has been noted for all of our institutions, and is likely common around the country.
Figure 2.
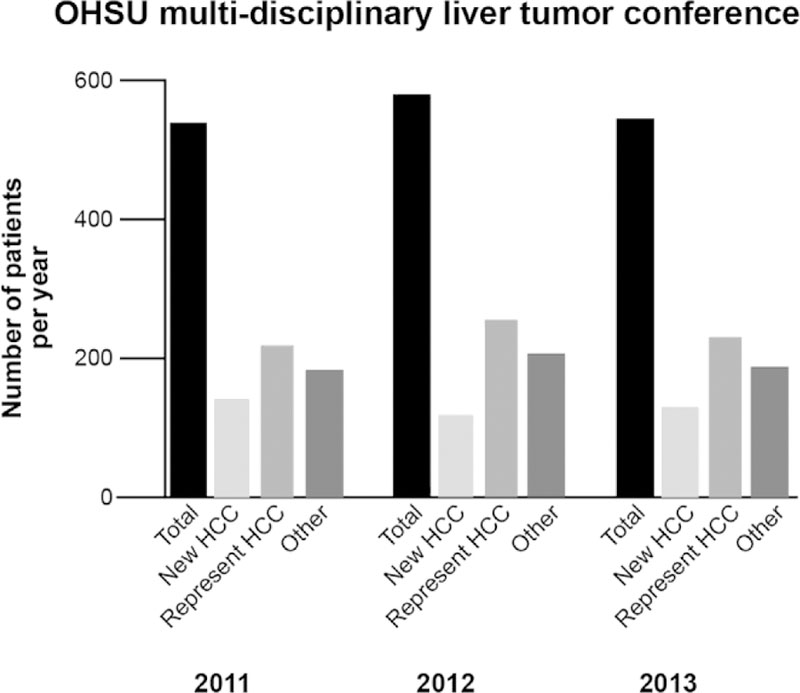
Example of one Liver MDT group (Oregon Health and Science University [OHSU]); case number over 3 years.
Likewise, hospital revenue for patients with HCC managed by an MDT is not difficult to capture, but does not tell us what we really want to know—how does the MDT specifically increase revenue for the institution? However, Table 1 provides us with a glimpse of what these patients mean financially for the institution. Table 1 shows sequential patients with HCC who presented initially to the Oregon Health and Science University MDT from September 2010 to June 2012, and focuses on the number of visits and gross revenue for 1 year after each patient’s initial presentation. Patients who received a liver transplantation were excluded from this analysis, but add significantly to the gross revenue if included. Thus, each of these patients on average generated $89,763 for the first year of management. Certainly, this data will differ between institutions, management styles, and insurance plans. In comparison, a recent Canadian study33 estimated that the 5-year net cost for caring for a patient with HCC in Ontario was $79,509. Although not specific for the MDT effort itself, these data clearly show such patients bring very significant revenue to the institution and thus indirectly support the notion that the MDT is worthwhile. Unfortunately, without more specific data it may be difficult to convince institutional leaders to strongly support liver MDTs, especially when most already are ongoing in absence of such support.
Table 1.
Gross Hospital Revenue and Visits by Type for Patients With HCC Treated Through the Oregon Health and Science University Liver MDT
| Total financials | Inpatient | Observation | Day patient | Emergency | Outpatient | Total |
|---|---|---|---|---|---|---|
| Unique patients | 92 | 37 | 143 | 27 | 231 | 240 |
| Cases/visits | 132 | 46 | 378 | 35 | 1797 | 2697 |
| Per unique patient gross revenue | 89,763 | |||||
| Total gross patient revenue | 21,543,168 |
NOTE. The data include consecutive patients with HCC who presented for the first time from September 2010 to June 2012 to the Oregon Health and Science University Liver MDT. Financial and visit data were collected beginning at the time of MDT presentation and ending 1 year from that time. All patients receiving liver transplantation during this time were excluded from the analysis.
Research
As the complexity of HCC management increases, so too does the complexity of understanding the impact of therapies on outcomes. There are many studies that investigate the effects of particular individual treatments for HCC, but there are little data on what happens in practice, during which patients often receive multiple or different treatments over time. A research question that arises from this is, “How do different combinations of treatments affect patient outcomes?” For example, for a patient who receives resection for HCC, followed by chemoembolization for recurrent disease, followed by treatment with sorafenib, ascribing the survival benefit for any particular treatment is difficult.
Because the MDT is the entity that presides over the entire management of the patient with HCC, it is the ideal setting for observational research of patient outcomes. In such a case, patient data must be collected; however, finding the resources for this can be problematic. Challenges for research lie in convincing MDTs to commit to collecting data on patients in a way that allows easy pooling of data between centers. A possible solution would be a bioinformatics tool that can do the following: (1) interface with the electronic medical record to bring clinical data efficiently into focus for the MDT; (2) create a clinical report for use in communicating with referring and treating providers; (3) provide a platform for billing for the MDT service; and (4) store the clinical data in a uniform way in a database from which robust outcome data could be generated. Such a tool would be used in real time in the MDT, recording the data that already routinely is discussed. If multiple centers used such a tool, pooled data would be collected automatically and complex outcome research would be possible.
Conclusions
Studies show that patients with HCC who receive care from an MDT have better outcomes and receive appropriate care more quickly and more often than patients who are not treated by MDTs.22,25,34 However, MDTs are underused in the United States, and patients being treated for HCC may not be receiving ideal care. The treatment of patients with HCC is complex because both the diseased organ and the cancer must be taken into account, requiring a variety of specialists working in unison. The current array of treatments for HCC also is complex, and no longer corresponds neatly to existing staging systems. An MDT is the ideal modality to manage patients with HCC because this approach may assimilate the varied facets of the management of this disease more easily. Patients with HCC who are treated under an MDT are more likely to receive individually tailored treatment in a timely fashion. The development of a successful MDT requires team dedication; utilization of recommendations in this article may help enable a successful MDT to improve the care of patients with HCC.
Acknowledgments
Funding
Supported by BlueMomentum, a division of the KnowledgePoint360 Group, who provided writing, editorial, and graphics support for the development of this manuscript; which was funded by Onyx Pharmaceuticals, Inc, and Bayer Healthcare.
Abbreviations used in this paper:
- BCLC
Barcelona Clinic Liver Cancer
- HCC
hepatocellular carcinoma
- MDT
multidisciplinary team
- OLT
orthotopic liver transplantation
- vMDT
virtual multidisciplinary team
Footnotes
Conflicts of interest
These authors disclose the following: Angel Alsina has served on the speakers bureau for Bayer, Onyx, and Novartis Pharmaceuticals; Catherine Frenette has served on the speakers bureau for Bayer and Onyx Pharmaceuticals; and Lorenzo Rossaro and Marty Sellers have served on the speakers bureau and advisory boards for Bayer and Onyx Pharmaceuticals. The remaining author discloses no conflicts.
References
- 1.Fennell ML, Das IP, Clauser S, et al. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr 2010;2010:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mitchell P, Wynia M, Golden R, et al. Core principles and values of effective team-based health care. Discussion paper Washington, DC: Institute of Medicine, 2012. Available at: http://www.iom.edu/tbc . Accessed October 20, 2013. [Google Scholar]
- 3.Murray KF, Carithers RL Jr. AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology 2005; 41:1407–1432. [DOI] [PubMed] [Google Scholar]
- 4.Fattovich G, Stroffolini T, Zagni I, et al. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 2004; 127:S35–S50. [DOI] [PubMed] [Google Scholar]
- 5.Colombo M, Raoul JL, Lencioni R, et al. Multidisciplinary strategies to improve treatment outcomes in hepatocellular carcinoma: a European perspective. Eur J Gastroenterol Hepatol 2013;25:639–651. [DOI] [PubMed] [Google Scholar]
- 6.Guy J, Kelley RK, Roberts J, et al. Multidisciplinary management of hepatocellular carcinoma. Clin Gastroenterol Hepatol 2012; 10:354–362. [DOI] [PubMed] [Google Scholar]
- 7.Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin 2005;55:74–108. [DOI] [PubMed] [Google Scholar]
- 8.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. [DOI] [PubMed] [Google Scholar]
- 9.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007; 132:2557–2576. [DOI] [PubMed] [Google Scholar]
- 10.NCCN Clinical Practice Guidelines in Oncology. Hepatobiliary cancers 2013. Available at: http://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf . AccessedO ctober 20, 2013. [DOI] [PMC free article] [PubMed]
- 11.Davis GL, Alter MJ, El-Serag H, et al. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology 2010;138:513–521. e511–e516. [DOI] [PubMed] [Google Scholar]
- 12.Onofrey S, Church D, Kludt P, et al. Hepatitis C virus infection among adolescents and young adults – Massachusetts, 2002–2009. MMWR Morb Mort Wkly Rep 2011;60:537–541. [PubMed] [Google Scholar]
- 13.Lee YS, Evans A, Kim D, et al. Prevalence of fatty liver disease: a community-based autopsy study. Gastroenterology 2012; 142(Suppl 1):S-1021–S-1022. [Google Scholar]
- 14.Vos MB, Welsh J. Prevalence of suspected NAFLD is increasing among U.S. adolescents. Gastroenterology 2012;142(Suppl 1):S–925. [Google Scholar]
- 15.Rahman RN, Ibdah JA. Nonalcoholic fatty liver disease without cirrhosis is an emergent and independent risk factor of hepatocellular carcinoma. Hepatology 2012;56:241A. [Google Scholar]
- 16.Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 1999; 19:329–338. [DOI] [PubMed] [Google Scholar]
- 18.Abou-Alfa G, Colombo M. Shaping the future management of hepatocellular carcinoma. Semin Liver Dis 2013;33(Suppl 1):S20–S23. [DOI] [PubMed] [Google Scholar]
- 19.Chirikov VV, Mullins CD, Hanna N, et al. Multispecialist care and mortality in hepatocellular carcinoma. Am J Clin Oncol 2013. September 21 Epub ahead of print. [DOI] [PubMed]
- 20.Chang TT, Sawhney R, Monto A, et al. Implementation of a multidisciplinary treatment team for hepatocellular cancer at a Veterans Affairs Medical Center improves survival. PB (Oxford) 2008;10:405–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gish RG, Lencioni R, Di Bisceglie AM, et al. Role of the multidisciplinary team in the diagnosis and treatment of hepatocellular carcinoma. Expert Rev Gastroenterol Hepatol 2012; 6:173–185. [DOI] [PubMed] [Google Scholar]
- 22.Cohen GS, Black M. Multidisciplinary management of hepatocellular carcinoma: a model for therapy. J Multidiscip Healthc 2013;6:189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shah SA, Smith JK, Li Y, et al. Underutilization of therapy for hepatocellular carcinoma in the Medicare population. Cancer 2011;117:1019–1026. [DOI] [PubMed] [Google Scholar]
- 24.Davila JA, Duan Z, McGlynn KA, et al. Utilization and outcomes of palliative therapy for hepatocellular carcinoma: a population-based study in the United States. J Clin Gastroenterol 2012; 46:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stark J, Fok B, Frenette C, et al. Multidisciplinary specialty evaluation results in higher rates of treatment for hepatocellular carcinoma International Liver Cancer Association; P117, Berlin, Germany, 2012. [Google Scholar]
- 26.Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 2011; 61:212–236. [DOI] [PubMed] [Google Scholar]
- 27.Haward RA. The Calman-Hine report: a personal retrospective on the UK’s first comprehensive policy on cancer services. Lancet Oncol 2006;7:336–346. [DOI] [PubMed] [Google Scholar]
- 28.Munro AJ, Swartzman S. What is a virtual multidisciplinary team (vMDT)? Br J Cancer 2013;108:2433–2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vazirani S. Nurse practitioners and creating a multidisciplinary care team reduce length of stay and costs at academic medical center Agency for Healthcare Research and Quality, 2000. Available at: http://innovations.ahrq.gov/content.aspx?id¼2609. Accessed October 22, 2013. [Google Scholar]
- 30.Cowan MJ, Shapiro M, Hays RD, et al. The effect of a multi-disciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nurs Adm 2006;36:79–85. [DOI] [PubMed] [Google Scholar]
- 31.Ettner SL, Kotlerman J, Afifi A, et al. An alternative approach to reducing the costs of patient care? A controlled trial of the multi-disciplinary doctor-nurse practitioner (MDNP) model. Med Decis Making 2006;26:9–17. [DOI] [PubMed] [Google Scholar]
- 32.Vazirani S, Hays RD, Shapiro MF, et al. Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care 2005; 14:71–77. [PubMed] [Google Scholar]
- 33.Thein HH, Isaranuwatchai W, Campitelli MA, et al. Health care costs associated with hepatocellular carcinoma: a population-based study. Hepatology 2013;58:1375–1384. [DOI] [PubMed] [Google Scholar]
- 34.Burak KW, Kneteman NM. An evidence-based multidisciplinary approach to the management of hepatocellular carcinoma (HCC): the Alberta HCC algorithm. Can J Gastroenterol 2010; 24:643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]