Abstract
Background
Self-diagnosis is the process of diagnosing or identifying a medical condition in oneself. Artificially intelligent digital platforms for self-diagnosis are becoming widely available and are used by the general public; however, little is known about the body of knowledge surrounding this technology.
Objective
The objectives of this scoping review were to (1) systematically map the extent and nature of the literature and topic areas pertaining to digital platforms that use computerized algorithms to provide users with a list of potential diagnoses and (2) identify key knowledge gaps.
Methods
The following databases were searched: PubMed (Medline), Scopus, Association for Computing Machinery Digital Library, Institute of Electrical and Electronics Engineers, Google Scholar, Open Grey, and ProQuest Dissertations and Theses. The search strategy was developed and refined with the assistance of a librarian and consisted of 3 main concepts: (1) self-diagnosis; (2) digital platforms; and (3) public or patients. The search generated 2536 articles from which 217 were duplicates. Following the Tricco et al 2018 checklist, 2 researchers screened the titles and abstracts (n=2316) and full texts (n=104), independently. A total of 19 articles were included for review, and data were retrieved following a data-charting form that was pretested by the research team.
Results
The included articles were mainly conducted in the United States (n=10) or the United Kingdom (n=4). Among the articles, topic areas included accuracy or correspondence with a doctor’s diagnosis (n=6), commentaries (n=2), regulation (n=3), sociological (n=2), user experience (n=2), theoretical (n=1), privacy and security (n=1), ethical (n=1), and design (n=1). Individuals who do not have access to health care and perceive to have a stigmatizing condition are more likely to use this technology. The accuracy of this technology varied substantially based on the disease examined and platform used. Women and those with higher education were more likely to choose the right diagnosis out of the potential list of diagnoses. Regulation of this technology is lacking in most parts of the world; however, they are currently under development.
Conclusions
There are prominent research gaps in the literature surrounding the use of artificially intelligent self-diagnosing digital platforms. Given the variety of digital platforms and the wide array of diseases they cover, measuring accuracy is cumbersome. More research is needed to understand the user experience and inform regulations.
Keywords: diagnosis, artificial intelligence, symptom checkers, diagnostic self evaluation, self-care
Introduction
Background
Researching health information on the internet has become common practice by the general public [1-3]. Those who do not have access to health care services are more likely to use the internet for health information [4]. In some cases, browsing the internet for health information can have certain benefits such as improving health outcomes by increasing the availability of information, providing social support, and improving self-efficacy [5,6]. However, potential negative consequences still exist; the information may not be reliable, and the individual seeking information may have low health literacy [6]. For example, an individual may not be able to critically analyze the health information and assess the applicability of the information to their case, which could result in detrimental effects on their health [6]. Therefore, health information widely circulated on the internet should be interpreted with caution [7].
Significant technological advances have resulted in the rise of more sophisticated digital health platforms, which could potentially mitigate this issue, especially those involving artificial intelligence (AI). Interest in AI appears to be relatively recent; however, the term dates back to the 1950s and is described as the theory and development of computer systems that can perform tasks that would normally require human intelligence [8,9]. Notably, AI has become incorporated in computerized diagnostic decision support systems, which were initially developed for health professionals. These platforms have now become readily available to the general public and are known as self-diagnosing apps or symptom checkers, which include the Mayo Clinic symptom checker, Babylon Health, the Ada health app, and the K Health app. On the basis of the medical information and symptoms provided by an individual, these digital platforms perform 2 main functions: (1) provide individuals with a list of potential diagnoses and (2) assist with triage [10]. While the accuracy of symptom checkers is still under question [11,12], this technology has been gaining traction globally [13,14] owing to its potential in addressing the lack of access to primary care providers (PCPs) and unnecessary medical visits—prominent issues in Canada and most parts of the world [15-18].
Objectives
Although accuracy is important to consider, it is of equal importance to understand the overall body of knowledge that surrounds this technology, including legal and ethical implications and user experiences. In light of this, it is imperative to systematically map the literature available on artificially intelligent self-diagnosing digital platforms to identify the areas of research pertaining to this topic and to outline the key gaps in knowledge. This information can support the growing interest in leveraging AI technology in health care systems. As such, this scoping review aimed to answer the following question: What is known about the use of artificially intelligent self-diagnosing digital platforms by the general public and what are the main knowledge gaps in the literature?
Methods
Eligibility Criteria
In this review, self-diagnosing digital platforms were defined as platforms that utilize algorithms to provide a list of potential diagnoses to the user based on the medical information and symptoms provided. Although this scoping review does not entail quality assessment, it follows a sound methodological approach to map out the results in a concise manner for knowledge users. This scoping review follows the 2018 checklist developed by Tricco et al [19] for reporting scoping reviews. Ethics approval was not required.
The 3 main overarching concepts that guided this search were (1) self-diagnosis; (2) digital platforms; and (3) public or patients. Given the relatively new emergence of this technology and its use by the general public, the search was not limited by a publication date. Articles that were included in the review were those that (1) pertained to the use of self-diagnosing digital platforms by the lay public or patients and (2) were written in English or French. Exclusion criteria were articles that (1) focused on the use of self-diagnosing AI technology by health professionals; (2) described the back-end development of a self-diagnosing platform (eg, neural networks and architecture); (3) focused on digital health platforms that provide general health information, advice for disease management or triage; (4) focused on a tool that entails a validated questionnaire rather than an algorithm; and/or (5) examined test kits or digital platforms requiring an image upload. To allow for a wide array of results to be included, quantitative, qualitative, and mixed-methods studies or reports were eligible for inclusion.
Information Sources and Search
This scoping review systematically searched citation databases and the gray literature for relevant published and unpublished articles. The citation databases included PubMed (Medline), Scopus, Association for Computing Machinery Digital Library, Institute of Electrical and Electronics Engineers, and Google Scholar. To supplement the gray literature retrieved through Google Scholar [20], OpenGrey and ProQuest Dissertations and Theses were also searched. The final search strategy for each data source was defined and refined with the assistance of a librarian (Rebecca Hutchinson, University of Waterloo) and was finalized on November 19, 2018. The final search strategy for PubMed (Medline) can be found in Multimedia Appendix 1. The final search results were exported into RefWorks for screening.
Selection of Sources of Evidence
Once duplicates were removed in RefWorks, the screening process was conducted independently by 2 researchers (SA and RHL). The decision tree in Figure 1 was used as a guide to screen titles and abstracts (or executive summaries for reports and commentaries). Articles that were extracted from the title and abstract screening stage were read in their entirety (full-text review). For the full-text screening step, 2 researchers (SA and RHL) screened the same 30 articles to assess inter-rater reliability. Any uncertainty and disagreements were discussed and resolved through consensus. Following full-text review, the reference lists of eligible articles were systematically screened. Similarly, for any review paper screened at the full-text review stage, references were screened for potentially relevant articles meeting the inclusion criteria.
Figure 1.
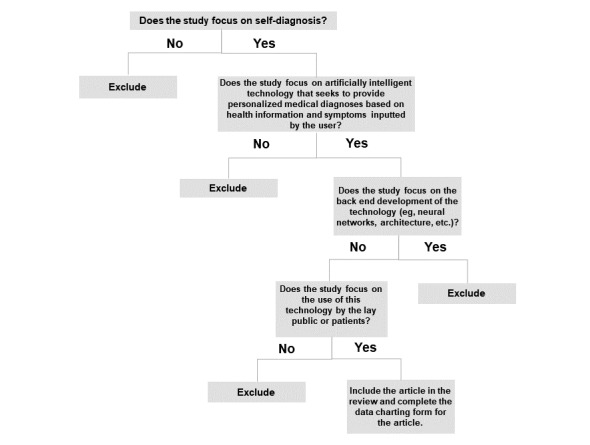
Decision tree for assessing article eligibility.
Data Charting Process
Once the final number of articles was determined, a scan through these articles allowed the research team to gain a high-level understanding of the topics of interest in which self-diagnosing digital platforms were being examined (eg, accuracy and regulatory concerns). This allowed for the development of a data-charting form that captured all the relevant information, irrespective of the article type (eg, clinical trial or a qualitative study on user experience). The data-charting form was pretested with the same 5 articles to assess consistency. No changes were made to the form following this exercise.
Data Extraction
The variables collected through the data-charting form included the following: country, year of publication, main objective, the main area of study (eg, clinical, legal, and ethical), study design, data sources used (if any), target population (if any), sample size and sample characteristics (if any), methods/statistical analyses (if applicable), main findings, and study limitations (if applicable).
Synthesis of Results
Scoping reviews provide knowledge users with a concise overview on the literature available on a given topic of interest [21]. Given the heterogeneity of the studies included in this review, studies were grouped based on a specific area of study. A concept map was used to illustrate the breadth of studies surrounding self-diagnosing AI technology. Tables were used to provide an overview on the types of articles found in the literature and the data extracted from each article. A thematic synthesis was used to outline the knowledge gaps in the literature and other key considerations.
Results
Selection of Sources of Evidence
Figure 2 depicts the flow chart, which illustrates the selection process at each screening step. Our search identified a total of 2536 from which 217 were duplicates. In addition, 2 researchers independently screened the titles and abstracts of 2316 articles from which 2229 were excluded based on relevance and eligibility criteria. A total of 104 full-text articles were retrieved and assessed for eligibility. Of these, 76 articles were excluded for the following reasons: described the back-end development of the digital platform or the algorithm, examined the use of digitized questionnaires rather than algorithm-based digital platforms, the digital platform required the input of health professionals, provided the risk of disease, monitored symptoms, technology designed for health professionals, not in scope, and did not provide enough data or information. We excluded 12 additional articles because we were unable to retrieve them. Through reference screening of the included articles, we identified 17 potentially relevant articles from which 3 articles were included in the review. A total of 19 articles were considered eligible for this review. Inter-rater reliability was assessed at the full-text stage which resulted in a score of 0.82, an almost perfect agreement score, between the 2 reviewers (SA and RHL) [22,23].
Figure 2.
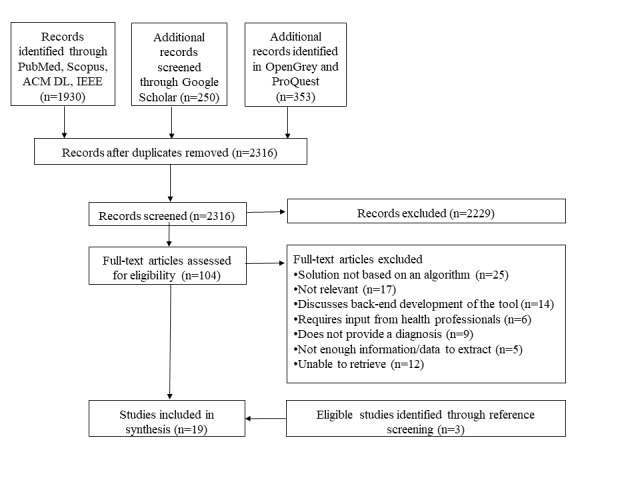
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of included articles. ACM DL: Association for Computing Machinery Digital Library; IEEE: Institute of Electrical and Electronics Engineers.
Characteristics of Sources of Evidence
The concept map in Figure 3 provides an illustrative overview of the main topic areas surrounding the use of artificially intelligent self-diagnosing digital platforms by the general public. The articles were mainly conducted in the United States (n=10) or the United Kingdom (n=4). In total, 2 of the articles were commentaries and the rest focused on the following areas: accuracy or correspondence with a doctor’s diagnosis, regulation, sociological perspectives, experience, theory, privacy and security, ethics, and design. The concept map also outlines the main themes that emerged from the articles and the health conditions examined.
Figure 3.

Concept map of the literature surrounding the use of artificially intelligent self-diagnosing digital platforms by the general public. DCM: degenerative cervical myelopathy; ENT: ear, nose, and throat; FDA: Food and Drug Administration; HIPAA: Health Insurance Portability and Accountability Act; NHS: National Health Service.
Results of Individual Sources of Evidence
Multimedia Appendix 2 provides an overview of all included articles and outlines the following variables: the article type, topic area examined, main objective, and main findings [24-42].
Synthesis of Results
Table 1 provides additional information on studies that entailed participant recruitment to answer their research question. These articles tended to focus on accuracy of the digital platform or user experience.
Table 1.
Synthesis of results of studies with participants.
| First author, year, reference, country | Sample size (n) | Target population | Data collection | Digital platforms used | Methods |
| Bisson, 2014 [26], United States | 572 | Individuals with knee pain | Primary data collection from patients and electronic medical records (EMRs) | A Web-based program developed by the research team | Sensitivity and specificity of the program’s ability to provide a correct diagnosis for knee pain was tested, out of a possible 21 conditions in which the algorithm was trained to diagnose |
| Bisson, 2016 [27], United States | 328 | Individuals with knee pain | Primary data collection from patients and EMRs | A Web-based program developed by the research team | Sensitivity and specificity were calculated |
| Copeland, 2018 [29], United States | 13 | Users who tested the protocol (specifics not provided) | Primary data collection using the System Usability Scale and the Usability Metric for User Experience | Prototype developed by the research team | Descriptive statistics |
| Farmer, 2011 [32], United Kingdom | 61 | Patients coming in to the Ear, Nose, Throat surgeon’s office | Primary data collected from patients over 1 month | Boots WebMD Symptom | Not provided |
| Hageman, 2014 [33], United States | 86 | Patients coming in to an outpatient hand and upper extremity surgeon’s office | Primary data collection from patients and physicians | WebMD Symptom Checker | The Pearson chi-square test was used to determine the level of correspondence of the provided diagnosis by the diagnostic application and the final diagnosis of the physician |
| Lanseng, 2007 [36], Norway | 160 | Individuals between the ages of 18 and 65 years | Primary data collection using the Technology Readiness Survey (TRI) | N/Aa | A survey with an internet‐based medical self‐diagnosis application as the focal technology was conducted; The research hypotheses were tested by completing a scenario and then following-up with a questionnaire |
| Luger, 2014 [37], United States | 79 | Older adults (aged 50 years or older) | Primary data collection of think-aloud protocols | WebMD Symptom Checker | Participants received one of 2 vignettes that depicted symptoms of illness. Participants talked out loud about their thoughts and actions while attempting to diagnose the symptoms with and without the help of common internet tools (Google and WebMD’s Symptom Checker); Think-aloud content of participants was then compared with those who were accurate in their diagnosis versus those who were not. |
| Powley, 2016 [40], United Kingdom | 34 | Consecutive patients with newly presenting clinically apparent synovitis or a new onset of symptoms consistent with inflammatory arthritis | Primary data collection from patients | National Health Service (NHS) and WebMD Symptom Checkers | Patients were asked questions about their internet use in relation to their presenting symptoms. Subsequently, they completed the NHS and the WebMD symptom checkers and their answers as well as outcomes were recorded. |
aNot applicable.
Discussion
Summary of Evidence and Knowledge Gaps
In this scoping review, 19 articles were included that examined artificially intelligent self-diagnosing digital platforms from various perspectives. Despite the popularity and accessibility of self-diagnosing AI technology by the public, it is noteworthy that research examining the accuracy of these platforms is limited. As such, it is unclear whether these platforms hinder or improve the health of users. Although some argue that the use of this technology may cause an individual to delay seeking care, it is important to recognize that delayed diagnoses are prevalent even without the use of this technology [40,42,43]. Many factors contribute to a delayed diagnosis with the top-ranked issues being poor communication between secondary and primary care, a mismatch between patients’ medical needs and health care supply, and a lack of access or use of health services [42,44]. For example, Behrbalk et al found that the average time delay from initiation of symptoms to the diagnosis of cervical spondylotic myelopathy (CSM) was 2.2 (SD 2.3) years [43]. Although symptom checkers can potentially address delayed diagnoses, a review showed that this technology was suboptimal in diagnosing CSM [30].
Moreover, these platforms generally provide a list of potential diagnoses rather than a single diagnosis. In this case, the user must decide which condition describes their current state best. The likelihood of a user to accurately choose the right diagnosis is associated with the sociodemographic profile/variables of a user, such as education and gender [33]. For example, women and those with higher education were more likely to choose the correct diagnosis [33]. Therefore, although having a timely diagnosis is important, it may be counterproductive if the user considers the wrong treatment options owing to a misdiagnosis. Moreover, the patient may still require a visit to a PCP to receive treatment or a prescription. Issues may arise if patients already have a diagnosis in mind when visiting their PCP as it could translate into disagreements regarding their condition.
This scoping review suggests that there are prominent knowledge gaps in the literature; as such, a systematic review may not be worthwhile on this topic. Rather, concerted efforts are needed in producing research in this area related to accuracy, user experience, regulation, doctor-patient relationship, PCP perspectives, and ethics. Specifically, extensive research is needed in evaluating the accuracy of this technology while accounting for the fact that some platforms are designed for a wide area of conditions and others are specialized—as such, these platforms need to be evaluated accordingly. It is also important to distinguish the difference between accuracy and correspondence with a PCP’s diagnosis as PCPs may misdiagnose or miss a diagnosis [45-47]. Importantly, when developing self-diagnosing AI digital platforms, it is important to test them on users with a wide range of backgrounds and level of experience with technology. This will ensure that a high proportion of users will end up choosing the right diagnosis.
Along with the importance of accuracy in self-diagnosing applications, there also needs to be guidance on how these platforms should be regulated. Although regulations related to self-diagnosing AI technologies should focus on patient safety as well as privacy and security, they should not hinder innovation in this area; rather, they should allow innovative advancements that are safe and improve access to timely diagnosis. Overall, more knowledge is needed on how different types of users interact with this technology and how its use can impact the PCP-patient relationship. There is also a need for clarity on data management shared by users. Ethical concerns surrounding the digital economy is a main area of concern, and there is currently a debate surrounding the trade-offs pertaining to the use of these platforms.
Limitations
Some limitations of this scoping review warrant mention. Artificially intelligent self-diagnosing platforms that require individuals to upload an image or a scan were excluded from the review. Test kits or platforms that would require the user to perform medical tests were also excluded. Our scoping review’s focus was on platforms that required the least amount of effort from the user (ie, simply entering their symptoms into the platform to obtain potential diagnoses). It is also possible that some potentially relevant articles were missed because they could not be retrieved. To counteract this limitation, the authors systematically reviewed the references of relevant articles and held multiple meetings to assess consistency and to discuss any discrepancies in the screening process.
Conclusions
Given self-diagnosing AI technology’s potential, it is worth understanding how it can be leveraged by health care systems to reduce costs and unnecessary medical visits. This scoping review aimed to map the literature surrounding the use of artificially intelligent self-diagnosing platforms. Given the direct-to-consumer approach of these platforms, it is worrisome that only a few studies have focused on the use of this technology. It is important that future research and resources are directed to understanding the accuracy and regulation of self-diagnosing AI digital platforms. These regulations may take different forms such as creating an application library which includes a list of platforms that have been deemed safe and provide highly accurate diagnoses from a credible health agency or organization. It should be noted that patient engagement is necessary in the development of these platforms to ensure that they allow a high proportion of individuals—irrespective of gender and education—to choose the right diagnosis. Importantly, user experience is crucial to consider as the public may be skeptical of this technology.
Acknowledgments
The authors thank Rebecca Hutchinson, librarian at the University of Waterloo, for assisting in creating the search strategy. This study was funded by the Canadian Institutes of Health Research. The funder had no role in study design, study selection, data synthesis, decision to publish, or preparation of the manuscript.
Abbreviations
- AI
artificial intelligence
- CSM
cervical spondylotic myelopathy
- PCP
primary care provider
Search strategy for PubMed (Medline).
Overview of included studies related to self-diagnosing artificial intelligence digital platforms.
Footnotes
Authors' Contributions: SA conceived and designed the review. RHL, BND, AC, and SE participated in the conception of the study. SA, RHL, and BND carried out the review. All authors read and improved the final manuscript.
Conflicts of Interest: None declared.
References
- 1.Statistics Canada. [2019-04-06]. 2009 Canadian Internet use survey https://www150.statcan.gc.ca/n1/daily-quotidien/100510/dq100510a-eng.htm .
- 2.Beck F, Richard JB, Nguyen-Thanh V, Montagni I, Parizot I, Renahy E. Use of the internet as a health information resource among French young adults: results from a nationally representative survey. J Med Internet Res. 2014;16(5):e128. doi: 10.2196/jmir.2934. http://www.jmir.org/2014/5/e128/ v16i5e128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pew Research Centre. [2019-04-06]. Health Online 2013 https://www.pewinternet.org/2013/01/15/health-online-2013/
- 4.Amante DJ, Hogan TP, Pagoto SL, English TM, Lapane KL. Access to care and use of the internet to search for health information: results from the US National Health Interview Survey. J Med Internet Res. 2015;17(4):e106. doi: 10.2196/jmir.4126. http://www.jmir.org/2015/4/e106/ v17i4e106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ybarra ML, Suman M. Help seeking behavior and the internet: a national survey. Int J Med Inform. 2006 Jan;75(1):29–41. doi: 10.1016/j.ijmedinf.2005.07.029.S1386-5056(05)00147-4 [DOI] [PubMed] [Google Scholar]
- 6.Tonsaker T, Bartlett G, Trpkov C. Health information on the internet: gold mine or minefield? Can Fam Physician. 2014 May;60(5):407–8. http://www.cfp.ca/cgi/pmidlookup?view=long&pmid=24828994 .60/5/407 [PMC free article] [PubMed] [Google Scholar]
- 7.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67. doi: 10.1186/1472-6947-12-67. http://www.biomedcentral.com/1472-6947/12/67 .1472-6947-12-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turing A. Computing machinery and intelligence. Mind. 1950;49:433–460. https://www.csee.umbc.edu/courses/471/papers/turing.pdf . [Google Scholar]
- 9.Senate Canada Standing Senate Committee on Social Affairs, Science and Technology. 2017. [2019-04-06]. Challenge ahead: Integrating Robotics, Artificial Intelligence and 3D Printing Technologies into Canada?s Healthcare Systems https://sencanada.ca/content/sen/committee/421/SOCI/reports/RoboticsAI3DFinal_Web_e.pdf .
- 10.Semigran HL, Linder JA, Gidengil C, Mehrotra A. Evaluation of symptom checkers for self diagnosis and triage: audit study. Br Med J. 2015;351:h3480. doi: 10.1136/bmj.h3480. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=26157077 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fraser H, Coiera E, Wong D. Safety of patient-facing digital symptom checkers. Lancet. 2018 Dec 24;392(10161):2263–2264. doi: 10.1016/S0140-6736(18)32819-8.S0140-6736(18)32819-8 [DOI] [PubMed] [Google Scholar]
- 12.Millenson ML, Baldwin JL, Zipperer L, Singh H. Beyond Dr Google: the evidence on consumer-facing digital tools for diagnosis. Diagnosis (Berl) 2018 Dec 25;5(3):95–105. doi: 10.1515/dx-2018-0009./j/dx.ahead-of-print/dx-2018-0009/dx-2018-0009.xml [DOI] [PubMed] [Google Scholar]
- 13.Business Insider. 2018. [2019-04-06]. An AI startup that claimed it can beat doctors in an exam is putting $100 million into creating 500 new jobs https://www.businessinsider.com/babylon-health-invests-100-million-500-new-jobs-ai-research-2018-9 .
- 14.Digital Health. 2018. [2019-04-06]. Babylon goes to Canada with Telus Health partnership https://www.digitalhealth.net/2018/09/babylon-canadian-partnership/
- 15.Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, Nagpal S, Saini V, Srivastava D, Chalmers K, Korenstein D. Evidence for overuse of medical services around the world. Lancet. 2017 Dec 08;390(10090):156–168. doi: 10.1016/S0140-6736(16)32585-5. http://europepmc.org/abstract/MED/28077234 .S0140-6736(16)32585-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. 2016 update on medical overuse: a systematic review. JAMA Intern Med. 2016 Dec 01;176(11):1687–92. doi: 10.1001/jamainternmed.2016.5381. http://europepmc.org/abstract/MED/27654002 .2553296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canadian Institute of Health Information. 2017. [2019-04-06]. Unnecessary Care in Canada https://www.cihi.ca/sites/default/files/document/choosing-wisely-baseline-report-en-web.pdf .
- 18.Organisation for Economic Co-operation and Development. 2019. [2019-04-06]. Health Care Quality Indicators http://www.oecd.org/health/health-systems/oecdhealthcarequalityindicatorsproject.htm .
- 19.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018 Oct 02;169(7):467–73. doi: 10.7326/M18-0850.2700389 [DOI] [PubMed] [Google Scholar]
- 20.Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of Google Scholar in evidence reviews and its applicability to grey literature searching. PLoS One. 2015;10(9):e0138237. doi: 10.1371/journal.pone.0138237. http://dx.plos.org/10.1371/journal.pone.0138237 .PONE-D-15-27398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Canadian Institutes of Health Research. 2016. [2019-04-06]. A Guide to Knowledge Synthesis http://www.cihr-irsc.gc.ca/e/29418.html .
- 22.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22(3):276–82. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3900052&tool=pmcentrez&rendertype=abstract . [PMC free article] [PubMed] [Google Scholar]
- 23.Wongpakaran N, Wongpakaran T, Wedding D, Gwet KL. A comparison of Cohen's kappa and Gwet's AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol. 2013;13:61. doi: 10.1186/1471-2288-13-61. http://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-61 .1471-2288-13-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bauer M, Glenn T, Monteith S, Bauer R, Whybrow PC, Geddes J. Ethical perspectives on recommending digital technology for patients with mental illness. Int J Bipolar Disord. 2017 Dec;5(1):6. doi: 10.1186/s40345-017-0073-9. http://europepmc.org/abstract/MED/28155206 .10.1186/s40345-017-0073-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weldegebrial T. Marshall University, Department of Health Informatics. 2016. [2019-04-06]. Regulations for eHealth & mHealth Apps before Deployment https://www.researchgate.net/publication/318887422_Regulations_for_eHealth_mHealth_Apps_before_Deployment .
- 26.Bisson LJ, Komm JT, Bernas GA, Fineberg MS, Marzo JM, Rauh MA, Smolinski RJ, Wind WM. Accuracy of a computer-based diagnostic program for ambulatory patients with knee pain. Am J Sports Med. 2014 Oct;42(10):2371–6. doi: 10.1177/0363546514541654.0363546514541654 [DOI] [PubMed] [Google Scholar]
- 27.Bisson LJ, Komm JT, Bernas GA, Fineberg MS, Marzo JM, Rauh MA, Smolinski RJ, Wind WM. How accurate are patients at diagnosing the cause of their knee pain with the help of a web-based symptom checker? Orthop J Sports Med. 2016 Feb;4(2):2325967116630286. doi: 10.1177/2325967116630286. http://europepmc.org/abstract/MED/26962542 .10.1177_2325967116630286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boulos MNK, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP. Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform. 2014;5(3):229. doi: 10.5210/ojphi.v5i3.4814. http://europepmc.org/abstract/MED/24683442 .ojphi-05-e229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Copeland C, Morreale P, Li J. m-Health application Interface design for symptom checking. 10th International Conference on e-Health; July 17-19, 2018; Madrid, Spain. 2018. http://tinyurl.com/y5jotoby . [Google Scholar]
- 30.Davies BM, Munro CF, Kotter MR. A novel insight into the challenges of diagnosing degenerative cervical myelopathy using web-based symptom checkers. J Med Internet Res. 2019 Jan 11;21(1):e10868. doi: 10.2196/10868. http://www.jmir.org/2019/1/e10868/ v21i1e10868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flaherty JL. Digital diagnosis: privacy and the regulation of mobile phone health applications. Am J Law Med. 2014;40(4):416–41. [PubMed] [Google Scholar]
- 32.Farmer SE, Bernardotto M, Singh V. How good is internet self-diagnosis of ENT symptoms using Boots WebMD symptom checker? Clin Otolaryngol. 2011 Oct;36(5):517–8. doi: 10.1111/j.1749-4486.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- 33.Hageman MG, Anderson J, Blok R, Bossen JK, Ring D. Internet self-diagnosis in hand surgery. Hand (N Y) 2015 Sep;10(3):565–9. doi: 10.1007/s11552-014-9707-x. http://europepmc.org/abstract/MED/26330798 .9707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jutel A, Lupton D. Digitizing diagnosis: a review of mobile applications in the diagnostic process. Diagnosis (Berl) 2015 Jun 01;2(2):89–96. doi: 10.1515/dx-2014-0068./j/dx.2015.2.issue-2/dx-2014-0068/dx-2014-0068.xml [DOI] [PubMed] [Google Scholar]
- 35.Kao C, Liebovitz DM. Consumer mobile health apps: current state, barriers, and future directions. PM R. 2017 May;9(5S):S106–15. doi: 10.1016/j.pmrj.2017.02.018.S1934-1482(17)30382-9 [DOI] [PubMed] [Google Scholar]
- 36.Lanseng E, Andreassen T. Electronic healthcare: a study of people's readiness and attitude toward performing self‐diagnosis. Int J of Service Industry Mgmt. 2007 Aug 14;18(4):394–417. doi: 10.1108/09564230710778155. [DOI] [Google Scholar]
- 37.Luger TM, Houston TK, Suls J. Older adult experience of online diagnosis: results from a scenario-based think-aloud protocol. J Med Internet Res. 2014 Jan 16;16(1):e16. doi: 10.2196/jmir.2924. http://www.jmir.org/2014/1/e16/ v16i1e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lupton D, Jutel A. 'It's like having a physician in your pocket!' A critical analysis of self-diagnosis smartphone apps. Soc Sci Med. 2015 May;133:128–35. doi: 10.1016/j.socscimed.2015.04.004.S0277-9536(15)00224-5 [DOI] [PubMed] [Google Scholar]
- 39.Morita T, Rahman A, Hasegawa T, Ozaki A, Tanimoto T. The potential possibility of symptom checker. Int J Health Policy Manag. 2017 Dec 05;6(10):615–6. doi: 10.15171/ijhpm.2017.41. http://europepmc.org/abstract/MED/28949479 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Powley L, McIlroy G, Simons G, Raza K. Are online symptoms checkers useful for patients with inflammatory arthritis? BMC Musculoskelet Disord. 2016 Dec 24;17(1):362. doi: 10.1186/s12891-016-1189-2. https://www.biomedcentral.com/1471-2474/17/362 .10.1186/s12891-016-1189-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ryan A, Wilson S. Internet healthcare: do self-diagnosis sites do more harm than good? Expert Opin Drug Saf. 2008 May;7(3):227–9. doi: 10.1517/14740338.7.3.227. [DOI] [PubMed] [Google Scholar]
- 42.Tudor Car L, Papachristou N, Bull A, Majeed A, Gallagher J, El-Khatib M, Aylin P, Rudan I, Atun R, Car J, Vincent C. Clinician-identified problems and solutions for delayed diagnosis in primary care: a PRIORITIZE study. BMC Fam Pract. 2016 Dec 09;17:131. doi: 10.1186/s12875-016-0530-z. https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-016-0530-z .10.1186/s12875-016-0530-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Behrbalk E, Salame K, Regev GJ, Keynan O, Boszczyk B, Lidar Z. Delayed diagnosis of cervical spondylotic myelopathy by primary care physicians. Neurosurg Focus. 2013 Jul;35(1):E1. doi: 10.3171/2013.3.FOCUS1374. [DOI] [PubMed] [Google Scholar]
- 44.Aboueid S, Meyer SB. Factors affecting access and use of preventive and weight management care: A public health lens. Healthc Manage Forum. 2019 Apr 03;:840470418824345. doi: 10.1177/0840470418824345. [DOI] [PubMed] [Google Scholar]
- 45.Singh H, Schiff GD, Graber ML, Onakpoya I, Thompson MJ. The global burden of diagnostic errors in primary care. BMJ Qual Saf. 2017 Jun;26(6):484–94. doi: 10.1136/bmjqs-2016-005401. http://qualitysafety.bmj.com/cgi/pmidlookup?view=long&pmid=27530239 .bmjqs-2016-005401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Panesar SS, deSilva D, Carson-Stevens A, Cresswell KM, Salvilla SA, Slight SP, Javad S, Netuveli G, Larizgoitia I, Donaldson LJ, Bates DW, Sheikh A. How safe is primary care? A systematic review. BMJ Qual Saf. 2016 Dec;25(7):544–53. doi: 10.1136/bmjqs-2015-004178.bmjqs-2015-004178 [DOI] [PubMed] [Google Scholar]
- 47.Nurek M, Kostopoulou O, Delaney BC, Esmail A. Reducing diagnostic errors in primary care. A systematic meta-review of computerized diagnostic decision support systems by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015 Sep;21 Suppl:8–13. doi: 10.3109/13814788.2015.1043123. http://europepmc.org/abstract/MED/26339829 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy for PubMed (Medline).
Overview of included studies related to self-diagnosing artificial intelligence digital platforms.


