Abstract
Despite attention on overlap and distinction between generalized anxiety disorder (GAD), social anxiety disorder (SAD), and major depressive disorder (MDD), interpersonal specificity (distinct, prototypical interpersonal features) between the disorders has been understudied. There is emerging evidence for such specificity (e.g., Erickson et al., 2016), but most studies relied on self-report, and not all studies controlled for shared variance between the disorders, complicating interpretation of findings. The present study extended the literature by examining unique interpersonal correlates of GAD, SAD, and MDD symptoms on self- and informant-report, and how self-informant agreement (both mean-level and correlation) in perception of interpersonal affiliation, dominance, and distress varied as a function of the symptoms. 369 college-aged participants (43% with clinical-level symptoms for at least one of the disorders (GAD, SAD, MDD), 57% non-disordered) and up to three of their significant others rated participants’ interpersonal problems (interpersonal behaviors that were difficult to engage in or engaged in excessively). We found evidence for exploitable tendencies in GAD, socially avoidant and nonassertive tendencies in SAD, and coldness in MDD based on self-report, but not on informant-report. Although self-other correlation was positive across outcomes, participants endorsed higher affiliation and interpersonal distress and lower dominance relative to informants. GAD, SAD, and MDD symptoms showed distinct moderating effects on these self-informant discrepancies. GAD symptoms predicted over-endorsing affiliation, SAD predicted under-endorsing dominance and affiliation, and MDD predicted no discrepancies in affiliation and dominance. The results speak to potential differentiation of the disorders based on distinct patterns of self-other discrepancy in interpersonal perceptions.
Keywords: Generalized anxiety disorder, Social anxiety disorder, Major depressive disorder, Interpersonal circumplex, Multi-method
1. Introduction
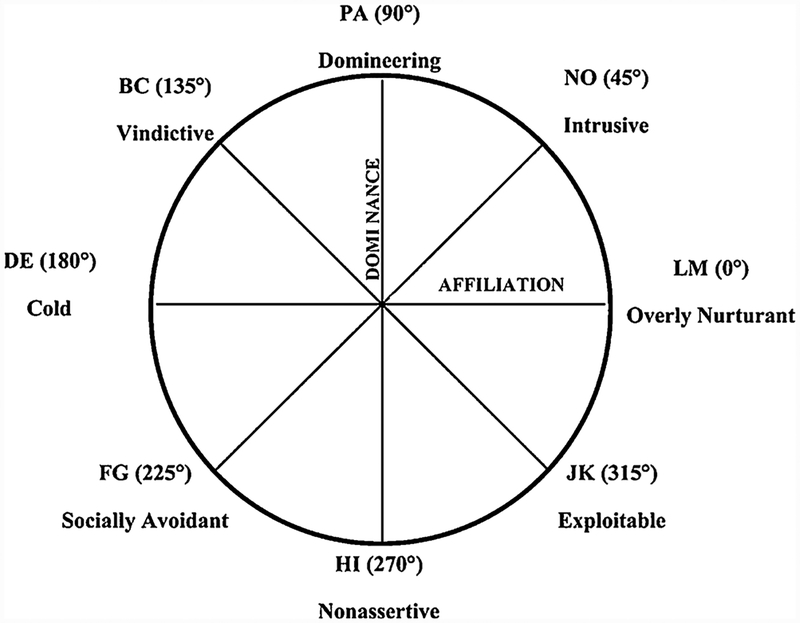
Generalized anxiety disorder (GAD), social anxiety disorder (SAD), and major depressive disorder (MDD) exhibit high comorbidity both concurrently and sequentially (e.g., Jacobson & Newman, 2017; Kessler et al., 2008). As a result, the overlap and distinction between the disorders has been of long-standing interest. One relatively understudied topic is interpersonal specificity, or distinct interpersonal problem features, between GAD, SAD, and MDD. Each disorder has been linked to interpersonal dysfunction such as marital discord, relationship maladjustment, and low social functioning (e.g., Barrera & Norton, 2009; Whisman, Sheldon, & Goering, 2000). However, emerging evidence on interpersonal problem tendencies in the disorders suggests some specificity (e.g., Erickson et al, 2016). Many prior studies utilized the interpersonal circumplex (IPC; Wiggins & Broughton, 1985), a theoretical framework for evaluating interpersonal problem features. The IPC assesses the full range of interpersonal problems based on two orthogonal dimensions, dominance-submission and affiliation-hostility, and includes eight octants that represent different blends of the two axes (Fig. 1).
Fig. 1.
The Interpersonal Circumplex.
Note. The two-letter labels (e.g., BC, NO) do not have substantive meaning, but they serve as meta-labels for octants in the interpersonal circumplex across different dimensions/surfaces of interpersonal functioning (e.g., traits, strengths, problems).
Using the IPC, interpersonal problems can be studied at the level of the two axes (dominance, affiliation), quadrants (dominant, submissive, affiliative, and hostile), as well as octants. Such octants include domineering (dominant; authoritarian, trying to change, control, or manipulate others), intrusive (affiliative-dominant; inserting oneself in other people’s business, attention-seeking), overly-nurturant (affiliative; too generous, putting others’ needs ahead of one’s own), exploitable (affiliative-submissive; easily taken advantage of, too gullible), vindictive (hostile-dominant; self-serving, vengeful toward others), nonassertive (submissive; difficulty letting others know what you want), socially-avoidant (hostile-submissive; difficulty meeting new people, difficulty socializing with others), and cold (hostile; keeping others at a distance, difficulty showing affection). Studying interpersonal problems at the level of octants allows for a more fine-grained analysis of interpersonal problems than axes or quadrants. For instance, the socially avoidant, nonassertive, and exploitable octants indicate hostile-submissive, “pure” submissive, and affiliative-submissive problems respectively whereas the submissive quadrant subsumes those different subtypes of submissiveness without differentiating them.
Prior studies based on the IPC showed that although GAD patients reported diverse interpersonal problems, a majority endorsed affiliative and submissive types of problems (Przeworski et al., 2011; Salzer et al., 2008). When compared to controls, GAD analogues also endorsed greater affiliative and submissive, but not hostile or dominant types of interpersonal problems (Eng & Heimberg, 2006). Pathological worry, the core symptom of GAD, was also associated with exploitable (affiliative-submissive) interpersonal problems when controlling for depression and social anxiety in undergraduate and clinical samples (Erickson et al., 2016). Also, treatment-seeking patients with pure or comorbid GAD reported higher affiliation and lower dominance relative to patients with PTSD (Uhmann, Beesdo-Baum, Becker, & Hoyer, 2010). Affiliation and submission in GAD have been theoretically linked to the function of worry and its maintenance. Newman, Llera, Erickson, Przeworski, and Castonguay (2013) proposed that contrast avoidance, prevention of a sudden large shift in negative emotions, may underlie pathological worry and interpersonal problems in GAD. Worry has been shown to heighten negative emotions and thus, reduce any further sharp increase in negative emotions in response to a stressor (e.g., Llera & Newman, 2014). A similar mechanism may give rise to affiliative and submissive behaviors in GAD such that those behaviors are employed to prevent hostility from others and the expected increase in negative emotions. Affiliation problems in GAD may also reflect beliefs that worrying means caring (Erickson et al., 2016). Those with GAD may worry to anticipate others’ needs and overly engage in affiliation and submission to secure others’ love and approval.
Social anxiety, on the other hand, has been most closely linked with submissive problem tendencies. Compared to controls, socially phobic groups endorsed higher submissiveness (e.g., Kachin, Newman, & Pincus, 2001). Those with SAD were also more nonassertive (submissive) and socially avoidant (hostile-submissive) than controls and depressed individuals without SAD (Alden & Phillips, 1990). Similarly, social anxiety predicted lack of assertion when controlling for depression in a clinical analogue sample (Davila & Beck, 2002). In addition, submissive cognitions correlated more strongly with social anxiety than generalized anxiety in undergraduate samples (Weeks, Rodebaugh, Heimberg, Norton, & Jakatdar, 2009). Evolutionary theories (e.g., Gilbert, 2001) propose that socially anxious individuals may hold low expectations of gaining dominance and choose to submit and avoid to preempt conflicts with dominant group members. Submission has been also viewed as a safety behavior to avoid anticipated negative social outcomes (e.g., Alden & Taylor, 2004).
Depression has been associated with hostile-submissive tendencies. Both depression and anhedonia predicted interpersonal profiles of being cold in undergraduate samples (Wright et al., 2012). When controlling for social anxiety, depressive symptoms also uniquely predicted under-reliance on others (lack of turning to others for social support), which is akin to coldness, in a clinical analogue sample (Davila & Beck, 2002). In student and clinical samples, depression positively correlated with self-reported submissive behaviors (e.g., Allan & Gilbert, 1997). A depression-submission link has been also supported in animal models (Malatynska & Knapp, 2005). It is posited that depressed individuals seek reassurance excessively to assuage their sense of guilt and low self-worth, but then they doubt authenticity of positive feedback, causing eventual rejection by others (e.g., Coyne, 1976; Hames, Hagan, & Joiner, 2013). Self-criticism and neediness (similar to reassurance-seeking) predicted submissiveness, with self-criticism also predicting hostility (Zuroff, Moskowitz, & Côté, 1999). Evolutionary theories (e.g., social competition theory; Gilbert, 2000) posit that depression reflects activation of a defensive psychobiological system to avoid potentially dangerous conflicts with superior rivals. In line with this theory, partner dominance and perceived inferiority predicted more submissive behaviors in depressed participants (Zuroff, Fournier, & Moskowitz, 2007).
Interestingly, several studies also showed that GAD, SAD, and MDD involved interpersonal heterogeneity, or pathoplasticity. Pathoplasticity refers to a mutually influencing, but non-etiological relationship between psychopathology and personality (Widiger & Smith, 2008). Such studies found support for pathoplasticity by identifying interpersonal subgroups within clinical or clinical analogue samples of GAD (Przeworski et al., 2011; Salzer et al., 2008), SAD (Cain, Pincus, & Grosse Holtforth, 2010; Kachin et al., 2001), and MDD (Cain et al., 2012; Dawood, Thomas, Wright, & Hopwood, 2013; Simon, Cain, Wallner Samstag, Meehan, & Muran, 2015). At the same time, some of these studies also found a central, unifying interpersonal problem tendency within each disorder based on a metric that quantifies interpersonal prototypicality, or the degree to which the given problem tendency is representative or coherent in the disorder’s interpersonal profile (i.e., R2; Gurtman, 1994). For instance, both German (Salzer et al., 2008) and U.S. samples of GAD patients (Przeworski et al., 2011) showed an exploitable (affiliative-submissive) problem tendency as a whole, with R2 values ranging from .69 (just below the cut-off of .70 for prototypicality) to .93. One SAD sample showed a prototypically non-assertive (submissive) problem tendency (R2 = .85; Cain et al., 2010) whereas another study found weaker evidence for a socially avoidant (hostile-submissive) problem tendency (R2 = .68) in patients with generalized social phobia (Kachin et al., 2001). Results for MDD were mixed, but in line with an overall hostile problem tendency. One sample exhibited low prototypicality (R2 = .32; Cain et al., 2012) whereas another found a prototypically socially avoidant (hostile-submissive) problem tendency (R2 = .92; Simon et al., 2015) and the other, a prototypically vindictive (hostile-dominant) problem tendency (R2 = .77; Dawood et al., 2013). These results suggest that each disorder might be characterized by an overarching interpersonal tendency while also subsuming interpersonal subgroups. Specifically, GAD individuals exhibited high affiliation and low dominance, SAD, low dominance, and MDD, low affiliation problems.
The reviewed literature indicates potentially distinct interpersonal problems between GAD, SAD, and MDD, but there is a need for further research. First, only two studies (Davila & Beck, 2002; Erickson et al., 2016) considered comorbidity between the disorders. Even in these studies, Davila and Beck (2002) focused on SAD and depression, and Erickson et al. (2016) examined effects of trait worry instead of GAD. Therefore, no study has yet examined unique interpersonal correlates of GAD, SAD, and MDD simultaneously. Such research would help to clarify past findings by informing which of the previously identified patterns was specific to each disorder. In addition, all studies except two (Eng & Heimberg, 2006; Erickson et al., 2016) solely relied on self-report. However, the transactional nature of social relationships necessitates inclusion of informant-report. In fact, greater self-other agreement in interpersonal perception predicted better relationship outcomes (e.g., Neff & Karney, 2005). Self- and informant-report of interpersonal characteristics also typically show very little shared variance (e.g., Clifton, Turkheimer, & Oltmanns, 2005), and informant-report provides greater or incremental validity over self-report in predicting interpersonal behaviors (meta-analysis; Connelly & Ones, 2010).
Furthermore, existing evidence suggests that there might be systematic patterns in how GAD, SAD, and MDD affect self-other discrepancy in interpersonal problem perceptions. For instance, in treatment-seeking patients of mixed anxiety and depression and clinical analogues of GAD (i.e., individuals with subclinical to clinical levels of GAD symptoms), trait worry and GAD status (relative to healthy controls) predicted more affiliation problems in self-report, but hostile impact (Erickson et al., 2016) and submission problems in informant-report (Eng & Heimberg, 2006). GAD analogues also under- or over-estimated their hostile impact on first-time interactants, and those who underestimated it were especially disliked by their interaction partners (Erickson & Newman, 2007). Social anxiety predicted submissive tendencies on both self- and informant-report in a clinical sample (e.g., Erickson et al., 2016). At the same time, in undergraduate and clinical analogue samples, social anxiety predicted underestimation of one’s warmth (Oakman, Gifford, & Chlebowsky, 2003) and likeability relative to ratings by an observer or a first-time interactant (e.g., Christensen, Stein, & Means-Christensen, 2003). The literature paints a different picture for MDD, where depressed patients showed accurate assessment of their interpersonal impact on others (e.g., Lewinsohn, Mischel, Chaplin, & Barton, 1980). In addition, all three disorders were associated with greater self-rated interpersonal distress relative to in-formant-reports in clinical analogue (Eng & Heimberg, 2006) and community samples (Rodebaugh et al., 2014).
The present study was the first one to examine unique interpersonal problem tendencies in GAD, SAD, and MDD relative to each other and to incorporate multiple informant-reports for most of the sample. We aimed to address whether interpersonal problem tendencies of GAD, SAD, and MDD based on self-report generalized to informant-report, and whether the disorders involved self-other discrepancy in distinct dimensions of interpersonal problems. For example, the literature suggests that self-other discrepancy on affiliation problems might occur in opposite directions in GAD (overestimating one’s affiliation relative to others’ perceptions) compared to SAD (underestimating one’s affiliation relative to others’ perceptions), whereas there would be less discrepancy in MDD. Methodological improvements over past studies included controlling for the shared variance between the disorders, using both self- and informant-report, and recruiting multiple informants. Using multiple informants has been shown to enhance predictive validity of informant-report for targets’ interpersonal behaviors (Connelly & Ones, 2010). In addition, to examine maladaptive interpersonal functioning associated with GAD, SAD, and MDD, we used the well-validated and widely used interpersonal circumplex (IPC) measure of interpersonal problems (Inventory of Interpersonal Problems-Short Circumplex; Soldz, Budman, Demby, & Merry, 1995). We computed confidence intervals for IPC parameters using a novel bootstrapping approach (Zimmermann & Wright, 2015) to improve on prior studies, most of which used IPC parameters descriptively (e.g., Przeworski et al., 2011).
Another unique aspect of the study was to quantitatively examine self-informant discrepancy as a function of GAD, SAD, and MDD symptoms. Past studies (e.g., Eng & Heimberg, 2006) only ran separate analyses of self- and informant-reports and descriptively compared results. By explicitly modeling self-informant discrepancy, we were able to test self-other discrepancies associated with each disorder with greater precision. Using the Truth and Bias Model (West & Kenny, 2011), two forms of self-informant discrepancy were examined: mean difference (over- or underestimation of one’s interpersonal problems relative to others’ perceptions) and correlation (low correlation suggesting deficits in ability to track how one presents to others). We assessed self-other discrepancy on multiple interpersonal problem indices including dominance, affiliation, and interpersonal distress.
Hypotheses were derived based on prior evidence and theories on maladaptive interpersonal patterns in GAD, SAD, and MDD. We predicted that on self-report, GAD symptoms would predict prototypical exploitable (affiliative-submissive) problem tendencies controlling for SAD and MDD symptoms whereas SAD symptoms would predict prototypical nonassertive (submissive) problem tendencies, and MDD symptoms, prototypical socially avoidant (hostile-submissive) problem tendencies. These patterns were expected to be partially replicated on informant-report, with GAD symptoms no longer predicting exploitable tendencies, but SAD symptoms predicting prototypical nonassertive tendencies and MDD symptoms predicting prototypical socially avoidant tendencies. We expected that for the mean-level difference between self- and informant-report, higher GAD symptoms would predict overestimating one’s affiliation whereas higher SAD symptoms would predict underestimating one’s affiliation, and MDD symptoms would not predict either over- or underestimation. All symptoms were expected to predict greater self-reported interpersonal distress relative to informant-report. Hypotheses on self-other correlation were exploratory. In past studies, GAD (Zainal & Newman, 2018) predicted intact or superior theory of mind, the capacity to decode and reason about others’ mental states and social cues, compared to healthy controls, but SAD predicted impairments (Hezel & McNally, 2014). MDD showed mixed results (e.g., Washburn, Wilson, Roes, Rnic, & Harkness, 2016). Thus, we predicted that higher SAD and potentially MDD symptoms would decrease self-informant correlations.
2. Methods
2.1. Participants
369 participants (78% female, 22% male) were recruited from the Psychology department subject pool at a large state university. They visited the lab in person, provided informed consent, and completed online questionnaires. Participants received course credits for their participation. Age ranged from 18 to 27 (M = 18.72, SD = 1.16). The sample included 77% White, 9% Asian, 6% Hispanic/Latina/o, 5% African American, and 3% Other (e.g., Multiracial) and exhibited a wide range of MDD, GAD, and SAD symptoms. Scores on the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) ranged from 0 to 44 (possible range 0–63) with the mean of 10.15 (SD = 8.49). Scores on the Generalized Anxiety Disorder Questionnaire-IV (GAD-Q-IV; Newman et al., 2002) ranged from 0 to 13 (possible range 0–13) with the mean of 4.86 (SD = 3.97). On the Social Phobia Diagnostic Questionnaire (SPDQ; Newman, Kachin, Zuellig, Constantino, & Cashman-McGrath, 2003), the range was from 0 to 27 (possible range 0–27) with the mean of 8.26 (SD = 5.79). To ensure clinical relevance of findings, participants were initially randomly sampled from the subject pool, and those who met diagnostic criteria on the self-report measures (GAD-Q-IV and SPDQ) or who met a diagnostic cutoff (BDI-II) were additionally recruited to oversample clinical populations. This led to a sample of 158 people (42.82%) who met clinical levels of one or more of the 3 disorders and 211 (57.18%) who were non-disordered. 94 (25.47%) participants met GAD criteria, 104 (28.18%) met SAD criteria, and 55 (14.90%) met clinical levels of MDD. Of these, 31 (8.4%) had GAD only, 46 (12.47%) had SAD only, and 8 (2.17%) had MDD only. In terms of comorbidity 26 (7.05%) had GAD and SAD, 15 (4.07%) GAD and MDD, 10 (2.71%) SAD and MDD, and 22 (5.96%) GAD, MDD, and SAD.
Participants nominated three people who they believed knew them well to complete an online questionnaire on their interpersonal problems. 94% had at least one informant who completed the survey. Of those, 19% had one informant, 33% had two informants, and 48% had three informants. A total of 796 informants (71% female, 29% male) provided data. Participants sent online survey links directly to their informants. Informants provided implied consent by completing online questionnaires. They did not receive any compensation and participated on a voluntary basis. Mean age of informants was 25.16 (SD = 12.86). Informants were friends (55.7%), family members (32.7%), romantic partners (9%), and the remaining 2.6% were “others” (e.g., coworkers). Participants and informants had known each other for 9.04 years on average (SD = 7.71). Both rated their relationship to be very close on average on a 9-point Likert scale ranging from 0 (Not at all) to 8 (Very much), participant: M = 7.10, SD = .90; informant: M = 7.36, SD = 1.09. Participant- and informant-rated relationship closeness were positively correlated, r(783) = .43, p < .001.
2.2. Measures
2.2.1. Generalized anxiety disorder questionnaire IV (GAD-Q-IV; Newman et al, 2002)
The GAD-Q-IV is a 14-item self-report diagnostic measure for GAD based on the DSM-IV/5 criteria. The first four yes-no questions assess excessiveness and uncontrollability of worry. The number of most frequent worry topics is also assessed. If participants endorse excessive and uncontrollable worries for more days than not for the past six months, they complete yes-no questions assessing somatic symptoms (e.g., “restlessness or feeling keyed up or on edge”) and rate interference and distress caused by worry and somatic symptoms on a 0 (“None”) to 8 (“Very Severe”) Likert scale. The measure has shown high internal consistency (α = .81 in the current sample), retest reliability, convergent and divergent validity. It can be scored categorically or continuously. We used the DSM-based categorical scoring (i.e., matching participants’ responses to the DSM-IV/5 criteria for GAD) to determine participants’ GAD status. Past validation studies showed good sensitivity (.89–.96) and specificity (.67–.82) for this approach (Moore, Anderson, Barnes, Haigh, & Fresco, 2013; Newman et al., 2002). In our primary analyses, we used GAD symptom scores obtained from continuous scoring.
2.2.2. Beck depression inventory-II (BDI-II: Beck et al, 1996)
The BDI-II includes 21 items assessing presence and severity of MDD symptoms. Items are rated on a 0 to 3 scale, and ratings are summed to yield a total score. The measure has shown high internal consistency (α = .91 in the current sample) and 1-week retest reliability (r = .93; Beck et al., 1996), as well as convergent and divergent validity. A score of 19 or higher indicates moderate to severe depression (Beck et al., 1996). We used this cutoff to identify clinical cases of MDD in the sample. This cutoff previously showed good sensitivity (.86–.87) and specificity (.79–.93) (Homaifar et al., 2009; Pietsch et al., 2012). Dimensional scores were used in primary analyses.
2.2.3. Social phobia diagnostic questionnaire (SPDQ; Newman et al, 2003)
The SPDQ is a 29-item self-report measure on symptoms of SAD based on the DSM-IV/5 criteria. The measure includes yes-no items (e.g., “Do you try to avoid social situations?”) and 5-point Likert scale items on fear and avoidance of various social situations (e.g., parties) as well as distress and interference from social anxiety. The measure showed high internal consistency (α = .94 in the current sample), 2-week retest reliability, and convergent and discriminant validity. It can be scored categorically (requiring meeting the full DSM criteria) or continuously. Categorical scoring was used to determine participants’ SAD status. This scoring method showed good specificity (.95), but relatively low sensitivity (.57) (Newman et al., 2003). Therefore, the number of SAD cases we detected in the present sample was likely a conservative estimate. For our primary analyses, we used continuous scoring to obtain dimensional SAD symptom scores.
2.2.4. Inventory of interpersonal problems-short circumplex (IIP-SC; Soldz et al, 1995)
Participants and informants completed the IIP-SC to rate participants’ interpersonal problems. The IIP-SC includes 32 items that assess interpersonal problems based on eight octants of the interpersonal circumplex (PA = domineering (e.g., “I try to control other people too much”), BC = vindictive (e.g., “It is hard for me to feel good about another person’s happiness”), DE = cold (e.g., “It is hard for me to feel close to other people”), FG = socially avoidant (e.g., “It is hard for me to socialize with other people”), HI = nonassertive (e.g., “It is hard for me to be firm when I need to be”), JK = exploitable (e.g., “I let other people take advantage of me too much”), LM = overly nurturant (e.g., “I try to please other people too much”), and NO = intrusive (e.g., “I want to be noticed too much”)). Each octant scale includes 4 items rated on a 5-point Likert scale from “not at all” to “extremely.” Participants made ratings for interpersonal behaviors that they found difficult to do (i.e., “It is hard for me to…”) or engaged in “too much.” Similar to other studies (e.g., Eng & Heimberg, 2006), the informant-version was created by changing the first person pronoun to third person pronouns (i.e., “It is hard for her/him to…”, “She/he …”). The measure showed good retest reliability (r = .83) and internal consistency (α = .65 to .88 for self-report, α = .69 to .90 for informants in the current sample). The IIP-SC has been shown to discriminate between different personality traits at both normative (e.g., the Five Factor personality traits; Nysaeter, Langvik, Berthelsen, & Nordvik, 2009) and pathological levels (DSM-5 personality traits; Wright et al., 2012).
2.3. Planned analyses
2.3.1. Structural summary method (SSM; Gurtman, 1994)
The SSM was used to analyze data from the IIP-SC. The SSM yielded four parameters in addition to dominance and affiliation: elevation, amplitude, angular displacement, and R2. Elevation is an average score across the octants and represents general interpersonal distress. Pathological personality traits (e.g., detachment, psychoticism) showed elevation of .18 or higher (Wright et al., 2012) whereas normative personality traits (e.g., positive emotionality) showed elevation lower than zero (Hopwood et al, 2013). Amplitude quantifies the degree of specificity within an interpersonal profile. A high value indicates a distinctive theme (e.g., peaking in coldness relative to other interpersonal tendencies) whereas a low value suggests lack of a specific theme. The cutoff values of |.15| for elevation and .15 for amplitude have been proposed as indicating markedly high (.15) or low (−.15) interpersonal distress and a meaningfully distinctive interpersonal theme (Wright et al., 2012). In a review of prior SSM studies, elevation ranged from 0 to |.46|, and amplitude ranged from .01 to .43 (Zimmermann & Wright, 2015). The 50th percentiles (|.11| for elevation, .16 for amplitude) roughly corresponded to the suggested cutoffs, providing support for validity of the cutoffs. Angular displacement indicates a predominant theme of an interpersonal profile (e.g., interpersonal problem tendency) by a location on the circumplex (e.g., 90° = Domineering). R2 is a goodness-of-fit statistic that quantifies how well the given profile corresponds to the expected pattern of correlations. R2 > .8 indicates a good fit, and > .7 indicates an acceptable fit. R2 is an index for interpersonal prototypicality. If the profile is too complex to be summarized by the SSM parameters (i.e. R2 < .7), amplitude and angular displacement are not interpretable.
The SSM has been applied to analyzing interpersonal profiles of individuals, groups, and constructs. We used the SSM to identify interpersonal profiles of GAD, SAD, and MDD symptoms on self- and averaged informant-report. To focus on the unique variance of disorders, we regressed each symptom on the other two and used the residualized symptom scores to obtain the SSM statistics for each symptom. The R-squared statistic ranged from .31 to .43 for the variance accounted for in each symptom by the other two symptoms. This was consistent with the well-documented comorbidity between the disorders (e.g, Kessler et al., 2008), but also showed that there was meaningful variance left to predict in each disorder even when accounting for the other two disorder symptoms. 95% percentile bootstrap confidence intervals (CIs) were computed for each SSM parameter using R syntax (Zimmermann & Wright, 2015). A prior simulation study showed that CIs for amplitude and angular displacement were affected by the sample size and parameter magnitude (Zimmermann & Wright, 2015). Thus, we used the R syntax to obtain probability estimates (p) for the probability that the CIs for amplitude and angular displacement were accurate. According to Zimmermann and Wright (2015), the CIs for amplitude and angular displacement should not be interpreted when p < .5 due to the high likelihood that the CI estimates are unreliable. CIs with p between .5 and .95 should be interpreted with caution due to a potential bias. CIs with p greater than .95 can be interpreted with confidence. Simulations demonstrated accurate CIs for elevation, dominance, and affiliation with a sample size of at least 50 (Zimmermann & Wright, 2015). Because the current sample met this requirement, CIs for the three parameters were interpreted with confidence.
2.3.2. Truth and bias model (West & Kenny, 2011)
The Truth and Bias Model was used to analyze the data from the IIP-SC and examine the degree to which participants’ perceptions of their dominance, affiliation, and interpersonal distress (elevation) deviated from informants’ perceptions. Intra-class correlations between informants ranged from .10 (95% CI = [−.18, .31]) for interpersonal distress to .61 (95% CI = [.50, .70]) for dominance and affiliation. We ran the following multi-level models to account for the nesting of informants within participants.
| (1) |
| (2) |
| (3) |
Pij is a participant’s self-report of the outcome variables (dominance, affiliation, and interpersonal distress). Iij is an informant-report of the variables. It is crucial to note that both self- and informant-report were centered by subtracting the grand mean of informant-report. This led to b0j representing the directional bias, the mean-level difference between self- and informant-report. A positive intercept indicated that participants endorsed interpersonal characteristics at a higher level relative to informants, and a negative intercept indicated endorsement at a lower level. The coefficient b1j represented accuracy, or correlation between self- and informant-report. A positive coefficient indicated that participants had corresponding views with informants. A negative coefficient indicated opposing views. Eij was a random error.
Both directional bias (b0j) and accuracy (b1j) were modeled as random effects, allowed to vary across participants. Symptom scores were included as predictors of between-person variability in directional bias and accuracy. GADi, SADi, and MDDi each represented a participant’s GAD, SAD, and MDD symptoms respectively. Symptoms were centered on their respective grand means. β00 was the Level 2 intercept indicating average directional bias across participants. β01, β02, and β03 represented the unique effects of each disorder’s symptoms on the directional bias, controlling for the others. A positive coefficient meant that a given disorder’s symptoms uniquely increased tendency toward overestimation relative to informant-report. A negative coefficient meant that a disorder’s symptoms uniquely increased a tendency toward underestimation relative to informant-report. u0j reflected individual variation in directional bias. In Eq. (3), β10 represented the Level 2 slope for average self-perception accuracy, or self-informant correspondence across participants. β11, β12, and β13 indicated unique moderating effects of each disorder’s symptoms on self-informant correspondence. A positive coefficient indicated that a disorder’s symptoms enhanced self-informant correspondence. A negative coefficient meant that the symptoms lowered the correspondence. u1j was individual variation in self-informant correspondence.
Multilevel analyses were conducted using R packages, lme4 (Bates, Mächler, Bolker, & Walker, 2015) and ImerTest (Kuznetsova, Brockhoff, & Christensen, 2015). We reported unstandardized regression coefficients along with 95% percentile bootstrap confidence intervals. Cohen’s f2 was calculated as a measure of effect size following Selya, Rose, Dierker, Hedeker, and Mermelstein (2012). Multicollinearity was not present (tolerance > .5, variance inflation factor < 2). Bivariate correlations between symptom variables ranged from .49 to .62 (ps < .05).
3. Results
3.1. Interpersonal profiles of GAD, SAD, and MDD symptoms
3.1.1. Self-report
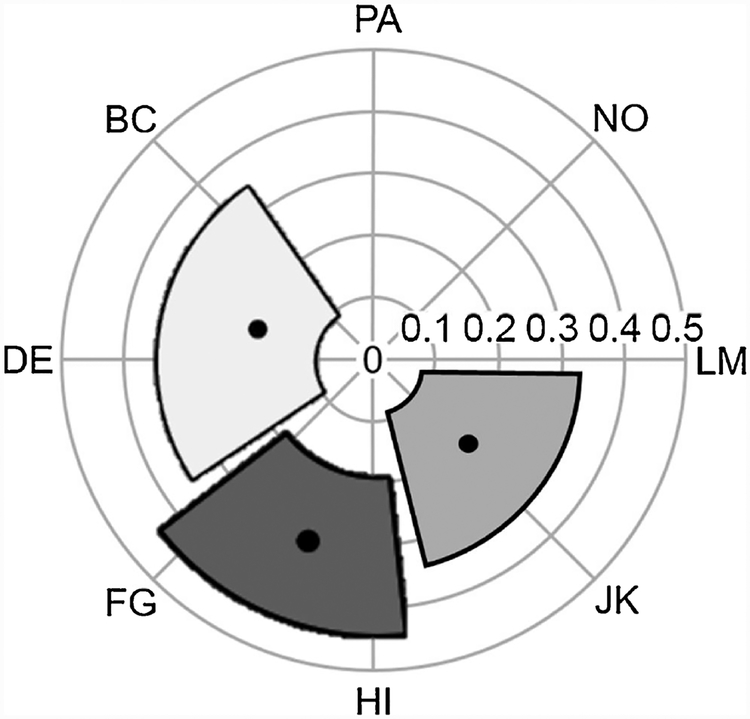
Structural summary method statistics and 95% CIs are summarized in Table 1. When controlling for their shared variance, GAD, SAD, and MDD symptoms each presented prototypical interpersonal problem profiles (R2 > .7) on self-report. Amplitude values indicated that each disorder’s symptoms were associated with specific interpersonal problems. Based on angular displacement, GAD symptoms predicted exploitable tendencies. SAD symptoms predicted socially avoidant and nonassertive tendencies, and MDD symptoms predicted cold tendencies. Non-overlapping CIs for angular displacement showed that GAD, SAD, and MDD had interpersonal problem profiles that were significantly distinct from each other (Fig. 2).
Table 1.
Structural Summary Method Parameters for the Interpersonal Profiles of Generalized Anxiety, Social Anxiety, and Depression.
| Affiliation | Dominance | e | A | δ | R2 | p | |
|---|---|---|---|---|---|---|---|
| Self-reported Interpersonal Problems (IIP-SC Self) | |||||||
| GAD | .16 | −.14 | .24 | .21 | 318° | .80 | .57 |
| [.04, .28] | [−.28, −.01] | [.07, .41] | [.09, .36] | [285°, 356°] | |||
| SAD | −.10 | −.32 | .27 | .33 | 252° | .96 | .97 |
| [−.24, .06] | [−.45, −.15] | [.10, .45] | [.20, .47] | [221°, 281°] | |||
| MDD | −.21 | .06 | −.06 | .22 | 164° | .96 | .73 |
| [−.36, −.07] | [−.11, .25] | [−.26, .13] | [.10, .39] | [121°, 214°] | |||
| Informant-reported Interpersonal Problems (IIP-SC Other) | |||||||
| GAD | .07 | −.08 | −.04 | .11 | 314° | .57 | .12 |
| [−.04, .21] | [−.21, .07] | [−.18, .12] | [.02, .27] | [217°, 78°] | |||
| SAD | −.08 | −.13 | .19 | .15 | 236° | .64 | .24 |
| [−.22, .05] | [−.28, .04] | [.05, .32] | [.05, .30] | [156°, 291°] | |||
| MDD | −.16 | .11 | −.01 | .19 | 146° | .68 | .28 |
| [−.27, −.04] | [−.04, .24] | [−.16, .14] | [.08, .33] | [108°, 196°] | |||
Note. e = Elevation; A = Amplitude; δ = Angular displacement; R2 = Goodness of fit; p = probability that the CIs for the amplitude and angular displacement are accurate; GAD = Generalized Anxiety Disorder Questionnaire-IV scores; SAD = Social Phobia Diagnostic Questionnaire scores; MDD = Beck Depression Inventory-II scores; IIP-SC = Inventory of Interpersonal Problems - Short Circumplex.
Fig. 2.
Interpersonal Profiles of Generalized Anxiety, Social Anxiety, and Depression based on Self-report IIP-SC.
Note. Amplitude (distance from the center) and angular displacement (angle) and bootstrapped 95% confidence intervals for the parameters are portrayed for symptoms of major depressive disorder (off-white), social anxiety disorder (dark gray), and generalized anxiety disorder (lighter gray). IIP-SC = Inventory of Interpersonal Problems – Short Circumplex; PA = Domineering; BC = Vindictive; DE = Cold; FG = Socially-avoidant; HI = Nonassertive; JK = Exploitable; LM = Overly-nurturant; NO = Intrusive. Amplitude exceeding .15 on any specific profile is considered to indicate a meaningfully distinctive interpersonal theme.
In line with results on angular displacement, higher GAD symptoms predicted more affiliation and submission problems. Higher SAD symptoms predicted more submission problems, and higher MDD symptoms predicted more hostility problems. Based on non-overlapping CIs, GAD symptoms predicted higher affiliative problem tendencies than MDD symptoms, and SAD symptoms predicted higher submissive tendencies than MDD symptoms. Based on elevation, higher GAD and SAD symptoms predicted significantly elevated interpersonal distress, but MDD symptoms did not.1
3.1.2. Informant-report
On informant-report, symptoms did not show prototypical interpersonal profiles (R2 < .7). Therefore, amplitude and angular displacement were not interpretable. Based on affiliation and dominance scores, higher MDD symptoms predicted significantly lower affiliation or more hostile problems. GAD and SAD symptoms did not predict significant elevations on either dimension. Nonetheless, non-over-lapping 95% CIs showed that MDD symptoms were associated with significantly lower affiliative tendencies (greater hostility) than GAD symptoms. In addition, only SAD symptoms predicted elevated interpersonal distress on informant-report.
3.2. Effects of GAD, SAD, and MDD symptoms on bias and accuracy in self-perception
Table 2 presents fixed effects from multilevel Truth and Bias Model analyses testing directional bias (mean-level difference between self-and informant-report) and accuracy (self-informant correlation). Directional bias was significant across outcomes. For dominance, directional bias was negative, indicating that participants on average endorsed dominance at a lower level relative to informants’ perceptions. Higher SAD symptoms uniquely heightened this tendency when controlling for the effects of GAD and MDD symptoms. Directional bias for affiliation was positive. Participants on average endorsed affiliation at a higher level relative to informants’ ratings. Controlling for the effects of the other symptoms, higher GAD symptoms increased this tendency whereas higher SAD symptoms predicted under-estimating one’s affiliation. There was no significant self-informant discrepancy for MDD on affiliation or dominance when controlling for the other symptoms. Directional bias was also positive for interpersonal distress. Participants endorsed greater distress relative to informants. Higher GAD, SAD, and MDD symptoms heightened this tendency even when controlling for each other’s effects. Self-informant correlation was positive across outcomes. There was no significant moderation of the self-informant correlation by disorder symptoms.2
Table 2.
Directional Bias and Accuracy of Self-Reported Dominance, Affiliation, and Interpersonal Distress in Relation to Informant-report.
| Dominance | Affiliation | Interpersonal distress | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | f2 | β | SE | 95% CI | f2 | β | SE | 95% CI | f2 | |
| Directional biasa | −.13** | .02 | −.16, −.09 | .12** | .02 | .08, .16 | .34** | .02 | .30, .38 | |||
| Accuracy | .30** | .04 | .22, .37 | .13 | .39** | .05 | .31, .49 | .12 | .12* | .04 | .05, .19 | .02 |
| Effect of participants’ generalized anxiety disorder symptoms | ||||||||||||
| Directional bias | −.004 | .006 | −.02, .01 | .003 | .03** | .01 | .02, .04 | .05 | .03** | .007 | .02, .05 | .02 |
| Accuracy | −.01 | .01 | −.04, .01 | .003 | .02 | .02 | −.01, .05 | .003 | −.005 | .01 | −.03, .02 | .001 |
| Effect of participants’ social anxiety disorder symptoms | ||||||||||||
| Directional bias | −.03** | .004 | −.04, −.02 | .10 | −.01* | .004 | −.02, −.001 | .03 | .03** | .005 | .02, .04 | .07 |
| Accuracy | −.01 | .01 | −.03, .01 | .003 | .01 | .01 | −.01, .03 | .003 | −.006 | .008 | −.02, .01 | .001 |
| Effect of participants’ major depressive disorder symptoms | ||||||||||||
| Directional bias | −.001 | .003 | −.01, .004 | .004 | −.001 | .003 | −.01, .005 | .001 | .02** | .003 | .01, .03 | .03 |
| Accuracy | .005 | .006 | −.01, .02 | .003 | −.01 | .01 | −.02, .004 | .003 | .001 | .005 | −.01, .01 | .001 |
Note. Directional bias represents an intercept, or a mean-level difference between self- and informant-report. Accuracy represents a regression coefficient of informant-report predicting self-report. Effect of each symptom indicates moderation of directional bias and accuracy by the symptom. All moderating terms were included simultaneously, f2 = Cohen’s f2.
p < .05.
p < .001.
Cohen’s f2 cannot be computed for the intercept (directional bias).
4. Discussion
The current study was the first one to examine interpersonal prototypicality of full GAD, SAD, and MDD symptoms in the same sample based on self- and multiple informant-reports and using confidence intervals to empirically determine prototypicality. When controlling for the other two disorders’ symptoms, GAD, SAD, and MDD symptoms predicted distinct interpersonal tendencies, largely consistent with hypotheses. GAD was characterized by exploitable (affiliative-submissive) problems, SAD by nonassertive (submissive) and socially avoidant (hostile-submissive) problems, and MDD by cold (hostile) problems. Contrary to our hypothesis, MDD was not associated with socially avoidant problems. This suggests that past findings on a depression-submission link might have been due to effects of comorbid conditions such as social anxiety. Our GAD and SAD findings were consistent with Erickson et al. (2016) findings for individuals with some GAD and SAD symptoms. In Erickson et al. (2016), depression was inconsistently associated with cold tendencies, but we found support for the depression-coldness association. Given the paucity of research in this area, it is meaningful that we replicated a similar pattern of interpersonal prototypicality of the disorders. Results suggest that interpersonal specificity observed for discrete symptoms (e.g., worry) may generalize to disorders (e.g., GAD).
Our findings may appear to contradict prior findings on pathoplasticity, or interpersonal heterogeneity, in GAD, SAD, and MDD. However, it is important to note that even in some of the prior studies, there was evidence for diagnosis-level prototypicality although interpersonal subgroups featured higher prototypicality (e.g., Cain et al., 2010; Simon et al, 2015). Therefore, each disorder might be characterized by an overarching interpersonal theme, but also include heterogeneous subgroups. For instance, GAD patients may endorse an affiliative-submissive style on average, but individual patients can deviate from this average tendency.
Importantly, interpersonal prototypicality evidenced on self-report for each disorder was not observed on informant-report. This suggests two possibilities. Informants might have simultaneously endorsed various interpersonal problems for an individual with a particular diagnosis (e.g., endorsing both cold and affiliative problems for someone with depression). Alternatively, informants might have reported specific problems for individuals, but the types of problems varied within a diagnostic group (e.g., one depressed individual characterized as cold, but another characterized as affiliative). This contrasts with a prior finding that worry and social anxiety (but not depression) showed prototypical interpersonal profiles on informant-report (Erickson et al., 2016). The difference might be due to the use of multiple informants (at least for most of the sample (76%)) in the current study as opposed to a single informant. Using multiple informants enhances predictive validity relative to a single informant (Connelly & Ones, 2010). The present results indicate greater consistency in how individuals with GAD, SAD, and MDD perceived themselves interpersonally than how they were perceived by others.
In addition, when results on self- and informant-report were compared, there were only a few consistent patterns. MDD symptoms predicted greater hostility relative to GAD symptoms on both reports. However, whereas GAD symptoms predicted affiliation and submission, and SAD symptoms predicted submission on self-report, neither significantly predicted affiliation or submission on informant-report. This is likely related to low prototypicality observed on informant-report. Informants’ endorsement of various problems (e.g., both hostile and affiliative) for participants with high GAD or SAD symptoms would have led to an overall null association between the symptoms and affiliation/dominance. In addition, although worry predicted affiliation on self-report, but hostile impact on informant-report in a prior study (Erickson et al., 2016), we did not find that GAD symptoms predicted hostility on informant-report. However, GAD symptoms still predicted a tendency to over-endorse affiliation on self-report relative to informant-report. This subtle difference in results might be due to using distinct interpersonal measures (i.e., impact vs. interpersonal problems). Nonetheless, both past and current studies showed that GAD symptoms’ association with affiliation problems was not supported on informant-report.
We also found that GAD, SAD, and MDD symptoms were associated with distinct patterns in self-informant discrepancy, specifically mean-level differences between self- and informant-report. Relative to informants’ perceptions, participants on average endorsed affiliation at a higher level and dominance at a lower level, consistent with past findings in married couples (e.g., Smith & Williams, 2016). MDD symptoms did not significantly moderate the self-other discrepancy for dominance or affiliation, in line with prior findings of depressive realism (e.g., Lewinsohn et al., 1980). However, as hypothesized, GAD symptoms predicted heightened tendency to over-endorse affiliation relative to informants’ perceptions whereas higher SAD symptoms predicted a tendency to under-endorse affiliation relative to informants’ perceptions. There was also an unexpected finding where higher SAD symptoms increased a tendency to under-endorse dominance relative to informant-ratings. This might have been due to the nature of the participant-informant relationship. Socially anxious individuals may behave in a less submissive manner around their family or friends. As a result, significant others serving as informants might have rated participants’ dominance more highly than expected. It is also possible that this discrepancy reflects a true bias as this was the first study to quantitatively examine the discrepancy between self- and informant-reports on interpersonal variables for individuals with SAD symptoms.
Interestingly, for GAD and SAD, evidence for self-other discrepancy emerged in their self-reported domains of interpersonal prototypicality. Thus, the disorders may involve prototypical self-perception biases as well as interpersonal problems. This finding has meaningful clinical implications because self-reported prototypical interpersonal problems predicted a worse prognosis for each disorder. For instance, self-reported affiliative problems at baseline predicted worse outcomes in psychodynamic therapy for GAD (Crits-Christoph et al., 2004) and higher anxiety at pre and post-treatment in cognitive behavioral therapy (CBT) for GAD (Newman, Jacobson, Erickson, & Fisher, 2017). In the case of social anxiety, avoidant personality disorder patients with greater hostility and emotional detachment failed to benefit from CBT skills training whereas those with warm, submissive problems did (Alden & Capreol, 1993). In addition, SAD patients with nonassertive problems showed worse outcomes in outpatient therapy than those with exploitable problems (Cain et al., 2010). Results on MDD were more diffuse. In group CBT, greater problems with being cold predicted drop-outs whereas greater problems with being submissive or affiliative predicted worse outcomes at post-treatment (McEvoy, Burgess, & Nathan, 2013). Thus, self-reported prototypical interpersonal problems might be involved in the maintenance of symptoms, especially in GAD and SAD.
The present findings suggest that those self-reported problems may contribute to symptom maintenance because they reflect and reinforce inaccurate perceptions of one’s interpersonal impact on others. One implication of this is that therapists need to assess distortions in clients’ interpersonal self-perceptions and address those beliefs (e.g., GAD clients mistaking the impact of their interpersonal behaviors as affiliative when it is not). For instance, therapists can facilitate clients’ selfmonitoring of cognitive distortions in interpersonal contexts and help them to identify and restructure the distortions (e.g., a GAD client restructuring her fallacy of fairness that others should always reciprocate her affiliative behaviors and understanding how such belief can lead to having a hostile rather than affiliative impact on others). The therapist-client relationship can also serve as a safe context in which a client explores biases in interpersonal perceptions and modifies them through corrective experiences. Therapists can also help clients to change their behaviors to have more desired impact on others. Clients can discuss specific interpersonal situations with therapists where their needs were not met (i.e., clients’ behaviors did not have an intended impact) and engage in role-playing and communication training to acquire more effective interpersonal behaviors to increase their chances of having the intended impact on others. An integrative treatment for GAD, which augmented CBT with interventions for interpersonal and emotional processing difficulties, used a similar approach and showed good outcomes (Newman et al., 2011).
The current study examined two forms of self-informant agreement using the Truth and Bias Model (West & Kenny, 2011): directional bias (mean difference between self- and informant-report), and accuracy (self-informant correlation). It is noteworthy that GAD, SAD, and MDD symptoms only significantly moderated directional bias, but not accuracy. This suggests that factors underlying moderation of directional bias may be irrelevant to accuracy (West & Kenny, 2011). In a past study (Ready & Clark, 2002), a mixed psychiatric sample also showed significant mean-level differences in self- and other-rated personality traits and interpersonal problems, but self-other correlation was comparable to that of nonclinical samples. Perhaps, GAD, SAD, and MDD symptoms are associated with self-schemas that lead to either over- or underestimation of one’s interpersonal traits, but do not alter individuals’ ability to track how they are perceived by others.
It is important to note that we treated informant-report as the relative “truths” to which self-report was compared. However, given that informant-report is subject to its own biases, our findings should be interpreted with caution. In a previous study, individuals who described themselves as paranoid were perceived as cold by peers whereas those who described themselves as angry and hostile were perceived as paranoid (Clifton, Turkheimer, & Oltmanns, 2004). This illustrates that informants do not have full access to participants’ subjective motives behind observed behaviors. Linking this to the present findings, individuals with GAD symptoms may intend affiliative behaviors, but fail to have such impact on others (Erickson et al., 2016). As a result, they may not experience the expected affiliation in return and misattribute it to others’ failure to reciprocate. Such experience would reinforce the self-view of being exploitable (overly accommodating). Similarly, individuals with SAD symptoms may feel they are more distant and submissive in social situations than they appear to others and appraise their behaviors as such.
Furthermore, the truth value of informant-report likely varied across outcomes. We assessed dominance and affiliation based on concrete behaviors (e.g., “open up to people too much”), but interpersonal distress based on subjective sense of severity. Inter-rater reliability between informants indicated higher agreement in rating dominance and affiliation than interpersonal distress. This is consistent with meta-analytic evidence that informant-report performed better in assessing observable than unobservable interpersonal features (Connelly & Ones, 2010). Therefore, the self-informant mean-level difference on interpersonal distress may reflect informants’ limited access to participants’ internal experiences. Accordingly, significant moderation of the mean-level difference in interpersonal distress may suggest that individuals with higher GAD, SAD, and MDD symptoms experienced greater subjective distress, but the distress was not apparent to their informants.
The current study had several limitations including the use of a non-treatment seeking sample. On one hand, we oversampled individuals meeting the clinical criteria for each disorder to ensure clinical relevance of the findings. Scores on self-report symptom measures also showed a wide range, covering severe symptom levels. Nonetheless, the current results warrant replication to see whether they generalize to treatment-seeking samples. Another limitation is using one interpersonal measure focused on interpersonal problems (IIP-SC). The measure has been widely used to examine interpersonal tendencies in GAD, SAD, and MDD (e.g., Kachin et al., 2001). Nonetheless, future studies can extend current findings by assessing interpersonal specificity of GAD, SAD, and MDD on multiple interpersonal measures (e.g., traits, strengths).
Our findings are also contextualized within the specific relationship participants had with informants. Participants nominated people whom they considered close to them (e.g., friends, family) as informants. The benefits of this approach include higher validity of informant-report compared to relying on first-time interactants (Connelly & Ones, 2010) and an opportunity to assess self-other discrepancy in close relationships. Nonetheless, these results warrant replication using other types of informants (e.g., first-time interactants). In addition, it would be important to examine how GAD, SAD, and MDD symptoms moderate individuals’ perceptions of others. Such information can shed light on interpersonal dynamics in each disorder. For instance, in a prior study, GAD analogues perceived confederates in a first-encounter interaction as more hostile, attacking, ignoring, and controlling than non-anxious controls (Erickson & Pincus, 2005). Higher social anxiety also predicted perceiving first-time interactants as less likeable or dependable (Christensen et al., 2003). Based on the present findings, it might be the case that individuals with GAD engage in affiliative behaviors (regardless of the behaviors’ true impact) to appease perceived hostility in others, and those with SAD feel more hostile and submissive toward others whom they perceive to be unlikable or untrustworthy. These hypotheses need further testing to elucidate the nature of interpersonal dysfunction in the disorders.
To summarize, the present findings extended prior evidence for interpersonal prototypicality and specificity between GAD, SAD, and MDD based on self-report by including informant-report and examining self-informant agreement as a function of the disorders. Interpersonal prototypicality was evidenced in self-report, but not in informant-report. The disorders also involved distinct patterns of self-informant discrepancy. Results suggest that interpersonal prototypicality of the disorders is more driven by biased self-views than objective interpersonal behaviors. This differentiates interpersonal prototypicality of GAD, SAD, and MDD from that of personality disorders, in which observable behaviors also exhibit prototypicality. Our findings suggest that it would be beneficial for therapists to assess and address distortions in client’s interpersonal self-schemas when treating GAD, SAD, and MDD.
Supplementary Material
Footnotes
Declarations of interest
None.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi: https://doi.org/10.1016/j.janxdis.2019.04.005.
Bivariate correlations of both unresidualized and residualized symptom scores (GAD, SAD, MDD) with interpersonal variables (octant scores, dominance and affiliation scores) are presented in an online supplemental table. When diagnostic overlap was not controlled for, the disorders presented less prototypical or more heterogeneous self-reported interpersonal problems than when we controlled for the diagnostic overlap. Nonetheless, regardless of whether we controlled for diagnostic overlap (i.e., residualizing symptom scores), GAD symptoms were positively correlated with affiliation, and SAD symptoms were negatively correlated with dominance. Unresidualized GAD and MDD symptom scores were also negatively correlated with dominance, but the correlations were no longer significant after we residualized the scores. These results were consistent with our conclusion that GAD symptoms were uniquely associated with affiliation-related interpersonal problems whereas SAD symptoms were uniquely associated with submission-related interpersonal problems.
Given that the moderation of the self-informant correlation by symptoms was not significant, we suspected that the symptoms’ moderating terms for the slope (self-informant correlation) might have functioned as a suppressor variable, spuriously increasing the predictive validity of the symptoms’ moderating terms for the intercept (directional bias). We reran the Truth and Bias Model analyses without including the symptoms’ moderating terms for the slope, and results were consistent with what we reported here. This ruled out the possibility that the significant moderation of the directional bias by symptoms was due to suppression effects.
References
- Alden LE, & Capreol MJ (1993). Avoidant personality disorder: Interpersonal problems as predictors of treatment response. Behavior Therapy, 24(3), 357–376. 10.1016/S0005-7894(05)80211-4. [DOI] [Google Scholar]
- Alden LE, & Phillips N (1990). An interpersonal analysis of social anxiety and depression. Cognitive Therapy and Research, 14(5), 499–512. 10.1007/BF01172970. [DOI] [Google Scholar]
- Alden LE, & Taylor CT (2004). Interpersonal processes in social phobia. Clinical Psychology Review, 24(7), 857–882. https://doi.Org/10.1016/j.cpr.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Allan S, & Gilbert P (1997). Submissive behaviour and psychopathology. British Journal of Clinical Psychology, 36(4), 467–488. https://doi.Org/10.llll/j.2044-8260.1997.tbOl255.x. [DOI] [PubMed] [Google Scholar]
- Barrera TL, & Norton PJ (2009). Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. Journal of Anxiety Disorders, 23(8), 1086–1090. https://doi.org/l0.1016/j.janxdis.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker B, & Walker S (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, TX: Psychological Corporationb9. [Google Scholar]
- Cain NM, Pincus AL, & Grosse Holtforth M (2010). Interpersonal subtypes in social phobia: Diagnostic and treatment implications. Journal of Personality Assessment, 92(6), 514–527. 10.1080/00223891.2010.513704. [DOI] [PubMed] [Google Scholar]
- Cain NM, Ansell EB, Wright AG, Hopwood CJ, Thomas KM, Pinto A, et al. (2012). Interpersonal pathoplasticity in the course of major depression. Journal of Consulting and Clinical Psychology, 80(1), 78 10.1037/a0026433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen PN, Stein MB, & Means-Christensen A (2003). Social anxiety and interpersonal perception: A social relations model analysis. Behaviour Research and Therapy, 41(11), 1355–1371. 10.1016/S0005-7967(03)00064-0. [DOI] [PubMed] [Google Scholar]
- Clifton A, Turkheimer E, & Oltmanns TF (2004). Contrasting perspectives on personality problems: Descriptions from the self and others. Personality and Individual Differences, 36(7), 1499–1514. https://doi.Org/10.1016/j.paid.2003.06.002. [Google Scholar]
- Clifton A, Turkheimer E, & Oltmanns TF (2005). Self-and peer perspectives on pathological personality traits and interpersonal problems. Psychological Assessment, 17(2), 123 https://doi.Org/10.1037/1040-3590.17.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly BS, & Ones DS (2010). An other perspective on personality: Meta-analytic integration of observers’ accuracy and predictive validity. Psychological Bulletin, 136(6), 1092–1122. 10.1037/a0021212. [DOI] [PubMed] [Google Scholar]
- Coyne JC (1976). Toward an interactional description of depression. Psychiatry: Journal for the Study of Interpersonal Processes, 39(1), 28–40. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MBC, Losardo D, Narducci J, Schamberger M, & Gallop R (2004). Who benefits from brief psychodynamic therapy for generalized anxiety disorder? Canadian Journal of Psychoanalysis, 12(2), 301–324. [Google Scholar]
- Davila J, & Beck JG (2002). Is social anxiety associated with impairment in close relationships? A preliminary investigation. Behavior Therapy, 33(3), 427–446. https://doi.org/l0.1016/S0005-7894(02)80037-5. [Google Scholar]
- Dawood S, Thomas KM, Wright AG, & Hopwood CJ (2013). Heterogeneity of interpersonal problems among depressed young adults: Associations with substance abuse and pathological personality traits. Journal of Personality Assessment, 95(5), 513–522. 10.1080/00223891.2013.781031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng W, & Heimberg RG (2006). Interpersonal correlates of generalized anxiety disorder: Self versus other perception. Journal of Anxiety Disorders, 20(3), 380–387. https://doi.Org/10.1016/j.janxdis.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Erickson TM, & Newman MG (2007). Interpersonal and emotional processes in generalized anxiety disorder analogues during social interaction tasks. Behavior Therapy, 38(4), 364–377. https://doi.Org/10.1016/j.beth.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Erickson TM, & Pincus AL (2005). Using structural analysis of social behavior (SASB) measures of self- and social perception to give interpersonal meaning to symptoms: Anxiety as an exemplar. Assessment, 12(3), 243–254. 10.1177/1073191105276653. [DOI] [PubMed] [Google Scholar]
- Erickson TM, Newman MG, Siebert EC, Carlile JA, Scarsella GM, & Abelson JL (2016). Does worrying mean caring too much? Interpersonal prototypicality of dimensional worry controlling for social anxiety and depressive symptoms. Behavior Therapy, 47(1), 14–28. https://doi.Org/10.1016/j.beth.2015.08.003. [DOI] [PubMed] [Google Scholar]
- Gilbert P (2000). Varieties of submissive behavior as forms of social defense: Their evolution and role in depression In Sloman L, & Gilbert P(Eds.). Subordination and defeat: An evolutionary approach to mood disorders and their therapy (pp. 3–45). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Gilbert P (2001). Evolution and social anxiety. The role of attraction, social competition, and social hierarchies. The Psychiatric Clinics of North America, 24(4), 723–751. 10.1016/S0193-953X(05)70260-4. [DOI] [PubMed] [Google Scholar]
- Gurtman MB (1994). The circumplex as a tool for studying normal and abnormal personality: A methodological primer In Strack S, & Lorr M (Eds.). Differentiating normal and abnormal personality (pp. 243–263). New York, NY: Springer Publishing Co. [Google Scholar]
- Hames JL, Hagan CR, & Joiner TE (2013). Interpersonal processes in depression. Annual Review of Clinical Psychology, 9, 355–377. 10.1146/annurev-clinpsy-050212-185553. [DOI] [PubMed] [Google Scholar]
- Hezel DM, & McNally RJ (2014). Theory of mind impairments in social anxiety disorder. Behavior Therapy, 45(4), 530–540. https://doi.Org/10.1016/j.beth.2014.02.010. [DOI] [PubMed] [Google Scholar]
- Homaifar BY, Brenner LA, Gutierrez PM, Harwood JF, Thompson C, Filley CM, et al. (2009). Sensitivity and specificity of the beck depression inventory-II in persons with traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 90(4), 652–656. https://doi.Org/10.1016/j.apmr.2008.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Burt SA, Keel PK, Neale MC, Boker SM, & Klump KL (2013). Interpersonal problems associated with multidimensional personality questionnaire traits in women during the transition to adulthood. Assessment, 20(1), 60–67. 10.1177/1073191111425854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NC, & Newman MG (2017). Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychological Bulletin, 143(11), 1155–1200. https://doi.Org/10.1037/bul0000111. [DOI] [PubMed] [Google Scholar]
- Kachin KE, Newman MG, & Pincus AL (2001). An interpersonal problem approach to the division of social phobia subtypes. Behavior Therapy, 32(3), 479–501. 10.1016/S0005-7894(01)80032-0. [DOI] [Google Scholar]
- Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, & Yonkers KA (2008). Co-morbid major depression and generalized anxiety disorders in the national comorbidity survey follow-up. Psychological Medicine, 38(3), 365–374. 10.1017/S0033291707002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2015). ImerTest: Tests in linear mixed effects models: R package version 2.0-29. Retrieved from http://CRAN.R-project.org/package=ImerTest.
- Lewinsohn PM, Mischel W, Chaplin W, & Barton R (1980). Social competence and depression: The role of illusory self-perceptions. Journal of Abnormal Psychology, 89(2), 203–212. https://doi.Org/10.1037/0021-843X.89.2.203. [DOI] [PubMed] [Google Scholar]
- Llera SJ, & Newman MG (2014). Rethinking the role of worry in generalized anxiety disorder: Evidence supporting a model of emotional contrast avoidance. Behavior Therapy, 45(3), 283–299. https://doi.Org/10.1016/j.beth.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Malatynska E, & Knapp RJ (2005). Dominant-submissive behavior as models of mania and depression. Neuroscience & Biobehavioral Reviews, 29(4), 715–737. 10.1016/j.neubiorev.2005.03.014. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Burgess MM, & Nathan P (2013). The relationship between interpersonal problems, negative cognitions, and outcomes from cognitive behavioral group therapy for depression. Journal of Affective Disorders, 150(2), 266–275. 10.1016/j.jad.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Moore MT, Anderson NL, Barnes JM, Haigh EA, & Fresco DM (2013). Using the GAD-Q-IV to identify generalized anxiety disorder in psychiatric treatment seeking and primary care medical samples. Journal of Anxiety Disorders, 28(1), 25–30. 10.1016/j.janxdis.2013.10.009. [DOI] [PubMed] [Google Scholar]
- Neff LA, & Karney BR (2005). To know you is to love you: The implications of global adoration and specific accuracy for marital relationships. Journal of Personality and Social Psychology, 88(3), 480 https://doi.Org/10.1037/0022-3514.88.3.480. [DOI] [PubMed] [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Przeworski A, Erickson T, et al. (2002). Preliminary reliability and validity of the generalized anxiety disorder questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy, 33(2), 215–233. 10.1016/S0005-7894(02)80026-0. [DOI] [Google Scholar]
- Newman MG, Kachin KE, Zuellig AR, Constantino MJ, & Cashman-McGrath L (2003). The social phobia diagnostic questionnaire: Preliminary validation of a new self-report diagnostic measure of social phobia. Psychological Medicine, 33(4), 623–635. 10.1017/S0033291703007669. [DOI] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell J, Szkodny LE, et al. (2011). A randomized controlled trial of cognitive-behavioral therapy for generalized anxiety disorder with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology, 79(2), 171–181. 10.1037/a0022489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Llera SJ, Erickson TM, Przeworski A, & Castonguay LG (2013). Worry and generalized anxiety disorder: A review and theoretical synthesis of research on nature, etiology, and treatment. Annual Review of Clinical Psychology, 9(1), 275–297. 10.1146/annurev-clinpsy-050212-185544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Jacobson NC, Erickson TM, & Fisher AJ (2017). Interpersonal problems predict differential response to cognitive versus behavioral treatment in a randomized controlled trial. Behavior Therapy, 48(1), 56–68. 10.1016/j.beth.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nysaeter TE, Langvik E, Berthelsen M, & Nordvik H (2009). Interpersonal problems and personality traits: The relation between IIP-64C and NEO-FFI. Nordic Psychology, 61(3), 82 https://doi.Org/10.1027/1901-2276.61.3.82. [Google Scholar]
- Oakman J, Gifford S, & Chlebowsky N (2003). A multilevel analysis of the interpersonal behavior of socially anxious people. Journal of Personality, 71(3), 397–434. 10.1111/1467-6494.7103006. [DOI] [PubMed] [Google Scholar]
- Pietsch K, Hoyler A, Frühe B, Kruse J, Schulte-Korne G, & Allgaier AK (2012). Early detection of major depression in paediatric care: Validity of the beck depression inventory-second edition (BDI-II) and the beck depression inventory-fast screen for medical patients (BDI-FS). Psychotherapie, Psychosomatik, Medizinische Psychologie, 62(11), 418–424. 10.1055/s-0032-1314869. [DOI] [PubMed] [Google Scholar]
- Przeworski A, Newman MG, Pincus AL, Kasoff MB, Yamasaki AS, Castonguay LG, et al. (2011). Interpersonal pathoplasticity in individuals with generalized anxiety disorder. Journal of Abnormal Psychology, 120(2), 286–298. 10.1037/a0023334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ready RE, & Clark LA (2002). Correspondence of psychiatric patient and informant ratings of personality traits, temperament, and interpersonal problems. Psychological Assessment, 14(1), 39–49. https://doi.Org/10.1037/1040-3590.14.l.39. [PubMed] [Google Scholar]
- Rodebaugh TL, Lim MH, Fernandez KC, Langer JK, Weisman JS, Tonge N, et al. (2014). Self and friend’s differing views of social anxiety disorder’s effects on friendships. Journal of Abnormal Psychology, 123(4), 715–724. 10.1037/abn0000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzer S, Pincus AL, Hoyer J, Kreische R, Leichsenring F, & Leibing E (2008). Interpersonal subtypes within generalized anxiety disorder. Journal of Personality Assessment, 90(3), 292–299. 10.1080/00223890701885076. [DOI] [PubMed] [Google Scholar]
- Selya AS, Rose JS, Dierker LC, Hedeker D, & Mermelstein RJ (2012). A practical guide to calculating Cohen’s f2, a measure of local effect size, from PROC MIXED. Frontiers in Psychology, 3, 111 10.3389/fpsyg.2012.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon S, Cain NM, Wallner Samstag L, Meehan KB, & Muran JC (2015). Assessing interpersonal subtypes in depression. Journal of Personality Assessment, 97(4), 364–373. 10.1080/00223891.2015.1011330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TW, & Williams PG (2016). Assessment of social traits in married couples: Self-reports versus spouse ratings around the interpersonal circumplex. Psychological Assessment, 28(6), 726 10.1037/pas0000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldz S, Budman S, Demby A, & Merry J (1995). A short form of the inventory of interpersonal problems circumples scales. Assessment, 2(1), 53–63. 10.1177/1073191195002001006. [DOI] [Google Scholar]
- Uhmann S, Beesdo-Baum K, Becker ES, & Hoyer J (2010). Specificity of interpersonal problems in generalized anxiety disorder versus other anxiety disorders and depression. Journal of Nervous and Mental Disease, 198(11), 846–851. 10.1097/NMD.ObOl3e3181f98063. [DOI] [PubMed] [Google Scholar]
- Washburn D, Wilson G, Roes M, Rnic K, & Harkness KL (2016). Theory of mind in social anxiety disorder, depression, and comorbid conditions. Journal of Anxiety Disorders, 37, 71–77. https://doi.Org/10.1016/j.janxdis.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Rodebaugh TL, Heimberg RG, Norton PJ, & Jakatdar TA (2009). “To avoid evaluation, withdraw”: Fears of evaluation and depressive cognitions lead to social anxiety and submissive withdrawal. Cognitive Therapy and Research, 33(4), 375–389. 10.1007/sl0608-008-9203-0. [DOI] [Google Scholar]
- West TV, & Kenny DA (2011). The truth and bias model of judgment. Psychological Review, 118(2), 357 10.1037/a0022936. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Sheldon CT, & Goering P (2000). Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology, 109(4), 803–808. https://doi.Org/10.1037/0021-843X.109.4.803. [DOI] [PubMed] [Google Scholar]
- Widiger TA, & Smith GT (2008). Personality and psychopathology In Oliver JP, Robins RW, & Pervin LA (Eds.). Handbook of personality psychology: Theory and research (pp. 743–769). (3rd ed.). New York: Guilford Press. [Google Scholar]
- Wiggins JS, & Broughton R (1985). The interpersonal circle: A structural model for the integration of personality research In Hogan R, & Jones WH (Vol. Eds.), Perspectives in personality: Vol. 1, (pp. 1–47). Greenwich, CT: JAI Press. [Google Scholar]
- Wright AG, Pincus AL, Hopwood CJ, Thomas KM, Markon KE, & Krueger RF (2012). An interpersonal analysis of pathological personality traits in DSM-5. Assessment, 19(3), 263–275. 10.1177/1073191112446657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainal NH, & Newman MG (2018). Worry amplifies theory-of-mind reasoning for negatively valenced social stimuli in generalized anxiety disorder. Journal of Affective Disorders, 227, 824–833. https://doi.Org/10.1016/j.jad.2017.11.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann J, & Wright AG (2017). Beyond description in interpersonal construct validation methodological advances in the circumplex structural summary approach. Assessment, 24(1), 3–23. 10.1177/1073191115621795. [DOI] [PubMed] [Google Scholar]
- Zuroff DC, Moskowitz D, & Côté S (1999). Dependency, self-criticism, interpersonal behaviour and affect: Evolutionary perspectives. British Journal of Clinical Psychology, 38(3), 231–250. 10.1348/014466599162827. [DOI] [PubMed] [Google Scholar]
- Zuroff DC, Fournier MA, & Moskowitz DS (2007). Depression, perceived inferiority, and interpersonal behavior: Evidence for the involuntary defeat strategy. Journal of Social and Clinical Psychology, 26(7), 751–778. 10.1521/jscp.2007.26.7.751. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.