Abstract
Objective:
Although adult hoarding disorder is relatively common and often debilitating, few studies have examined the phenomenology of pediatric hoarding. We examined the clinical phenomenology and response to cognitive-behavioral therapy (CBT) treatment in youths with a diagnosis of obsessive-compulsive disorder (OCD) with and without hoarding symptoms. Age was tested as a moderator across analyses, given prior findings that the impact of hoarding symptoms may not become apparent until adolescence.
Method:
Youths (N = 215; aged 7–17 years) with OCD pursuing evaluation and/or treatment at a university-based specialty clinic participated in the current study. Presence of hoarding symptoms was assessed as part of a larger battery. Data from a subset of youths (n = 134) who received CBT were included in treatment response analyses.
Results:
Youths with hoarding symptoms did not differ from those without hoarding symptoms with respect to overall OCD symptom severity and impairment. Youths with hoarding met criteria for more concurrent diagnoses, including greater rates of internalizing and both internalizing/externalizing, but not externalizing-only, disorders. Youths with and without hoarding symptoms did not significantly differ in rate of response to CBT. Age did not moderate any of these relationships, suggesting that the presence of hoarding symptoms was not associated with greater impairments across the clinical presentation of OCD or its response to treatment by age.
Conclusion:
We found no evidence that hoarding is associated with greater OCD severity or poorer treatment response in affected youth. Theoretical and clinical implications of these findings, including future directions for research on testing developmental models of hoarding across the lifespan, are discussed.
Keywords: pediatric, OCD, hoarding
Compulsive hoarding is defined as the excessive acquisition and inability to discard possessions of little value.1 Increasingly, hoarding is recognized as a mental health problem that is both relatively common and debilitating. Clinically significant hoarding behaviors affect between 1.5%2 and 4%3,4 of adults. The condition is associated with significant functional impairment,5 and poses considerable public health risk due to its chronicity and potential public safety concerns.6,7
Although hoarding behaviors are well studied in adults,8–12 these symptoms predominantly onset prior to adulthood (between ages 11 and 15 on average13), with an estimated 2% of adolescents exhibiting clinical levels of hoarding.14 There is relatively scant literature on child/adolescent manifestations or developmental trajectories of hoarding. Thus, there is a clear need to better understand the phenomenology and treatment of hoarding in youth. Such work may provide targets for treating the condition during the pediatric period, which in turn may improve individuals’ functioning across the lifespan.
Unlike the common presentation of hoarding without co-occurring OCD in adults,15 few youths report hoarding symptoms in the absence of other OCD symptoms,16 and up to 30% of youths with OCD diagnoses report hoarding symptoms.17 As hoarding rarely presents in the absence of OCD in youths, studying pediatric hoarding in the context of OCD may be informative. A handful of studies have examined associated features of pediatric hoarding, finding that youths with OCD diagnoses and hoarding symptoms reported earlier age of OCD onset,18 more severe current19 and lifetime18 OCD, and higher rates of internalizing disorder comorbidity.17,18,20 Moreover, a recent meta-analysis suggests hoarding symptoms are predictive of poorer treatment response in both youths and adults with OCD21; however, findings for youths appear to be driven by a naturalistic follow-up study of youths treated with pharmacotherapy.19 In contrast, the single empirical investigation that examined the relationship between specific pediatric OCD symptoms and cognitive-behavioral therapy (CBT) response found no difference in response between youths with and without hoarding symptoms.22
Although the above-described studies provide preliminary information about the phenomenology of hoarding in youth, they also raise questions about the role of development in the expression of hoarding and its sequelae. Hoarding is correlated with earlier OCD onset in youth19 and tends to worsen with age in adulthood,23 suggesting that age may play an important role in hoarding phenomenology. To our knowledge, no study to date has assessed the potential influence of age in the relationship between hoarding symptoms and OCD characteristics in youth. Thus, a primary goal of the present study was to test age as a putative moderator of hoarding symptom presence in pediatric OCD, its clinical correlates, and CBT response. Our aims were two-fold. First, to benchmark against the extant pediatric literature,18 we sought to characterize the hoarding phenotype in youths with OCD in a large, well-characterized sample of youths with primary OCD. Second, we explicitly examined age as a moderator of the relationship between presence of hoarding symptoms in pediatric OCD and three sets of outcomes: (1) clinical variables (OCD severity and impairment); (2) diagnostic comorbidity; and (3) treatment response to CBT. We hypothesized that age would moderate the relationship between hoarding symptoms and clinical outcomes such that, compared to the group without hoarding symptoms, youths with hoarding symptoms would evidence greater impairments in clinical outcome and treatment response with increasing age. This hypothesis was based on adult findings that hoarding is treatment resistant21 and becomes more problematic across the lifespan.23 It was also based on theoretical proposals for a developmentally sensitive model of hoarding in youth.24
METHOD
Participants
Participating youths included 215 children and adolescents presenting for diagnostic assessment at a university-based research clinic specializing in the treatment of OCD and anxiety disorders. All parents provided consent and youths provided assent to participate in a research assessment battery that had been approved by the university’s institutional review board. A subsample (n = 134) of the original 215 youths consented to participate in and were randomly assigned to receive CBT in one of three randomized clinical trials25–27; their data were used for treatment response analyses (Aim 3). This subsample did not significantly differ from youths who received an assessment but did not receive CBT on age [t (213) = −0.33, p =.74], gender [χ2 (1) = 0.04,p =.85], baseline OCD severity [t (213) = 0.87,p =.39], or proportion of youths who presented with hoarding symptoms [χ2 (1) = 1.47, p =.69].
Measures
Anxiety Disorders Interview Schedule for Children, Version IV.
The Anxiety Disorders Interview Schedule for Children, Version IV (ADIS) is a semi-structured diagnostic interview that assesses the major DSM-IV internalizing and externalizing disorders and that has demonstrated strong psychometric properties.29,30 The ADIS was used to determine primary OCD diagnosis and to assess for other comorbid diagnoses.
Children’s Yale—Brown Obsessive-Compulsive Scale.
The Children’s Yale—Brown Obsessive Compulsive Scale (CYBOCS)31 is a clinician-rated dimensional measure of OCD severity that includes a symptom checklist and total severity score. The severity score is derived from ratings for time spent on, resistance to, and control over symptoms, and interference and distress associated with symptoms. The CYBOCS has sound psychometric properties31,32 and is the gold-standard dimensional, clinician-rated measure of youth OCD severity. The CYBOCS checklist was used to code for the presence or absence of the hoarding symptom cluster, which has previously been empirically derived.33,34 Youths who endorsed either hoarding obsessions (fear of losing things; other hoarding/saving obsessions) and/or hoarding compulsions (difficulty throwing things away, saving bits of paper, string, etc.; other hoarding/saving compulsions) on the CYBOCS checklist were rated as meeting for the hoarding cluster.33,34 The hoarding cluster was then used to divide the sample into groups of youths who did versus did not evidence hoarding symptoms; this was the primary predictor across analyses. The CYBOCS total score was used in this study to assess whether the presence of hoarding symptoms was associated with worse symptom severity at baseline, as well as to assess symptom severity change following CBT. In this sample, Cronbach’s α for the CYBOCS total severity score was 0.87.
Children’s Obsessive Compulsive Impact Scale-Revised.
The Children’s Obsessive Compulsive Impact Scale-Revised (COIS-R)35 is a 27-item youth- and parent-report questionnaire that assesses OCD-specific functional impairment across home, school, and social domains of functioning. The COIS-R was used in this study to assess whether the presence of hoarding symptoms was related to worse functional impairment by youth and parent. Cronbach’s α for the COIS-R was 0.75 for parent report and 0.80 for child report.
Clinical Global Impressions-Improvement.
The Clinical Global Impressions-Improvement (CGI-I)36 is a clinician-rated measure of improvement that is commonly used to indicate treatment response in clinical trials. A CGI-I score of 1 (“much improved”) or 2 (“very much improved”) was used as the primary measure of CBT treatment response.
Procedure
Youth seeking assessment and/or treatment for OCD completed an initial research diagnostic evaluation and assessment battery, from which the measures in this study were drawn. The ADIS-IV and CYBOCS were conducted with both youth and parent by doctoral-level psychologists or doctoral students in clinical psychology; all doctoral students were trained and supervised by doctoral-level psychologists, with weekly supervision and case consensus. Parents and youths completed the COIS-R. Eligible youths were then offered participation in one of three randomized controlled trials.25–27 A subset of youths (n = 134) consented to participate in and were randomly assigned to receive 12 sessions of manualized CBT37 in one of these three treatment trials25–27; their data were used for the CBT treatment response analyses.
Statistical Analyses
The hoarding symptom cluster on the CYBOCS was previously derived by Stewart et al.33,34 Cluster assignment was dichotomous (yes/no); if youths met criteria for any current symptom in the hoarding cluster as rated by clinician, they were included in the hoarding symptoms group. Presence/absence of hoarding symptoms was the primary predictor in analyses except where otherwise specified. Descriptive statistics, including frequencies, means, and χ2 were used to characterize the sample (Table 1).
TABLE 1.
Demographic and Clinical Characteristics for Full Sample and by Group
| Total | Hoarding | No Hoarding | |
|---|---|---|---|
| Characteristic | Sample (N=215) | Symptoms (n=92) | Symptoms (n=123) |
| Age, y | 12.25 (2.75) | 12.15 (2.80) | 12.33 (2.72) |
| Sex, % female* | 43% | 51% | 37% |
| Minority status, % minority | 26% | 26% | 26% |
| Psychotropic medication use, % | 13% | 11% | 15% |
| CYBOCSa total severity score | 24.89 (4.33) | 25.43 (3.93) | 24.49 (4.58) |
| COIS-Rb Child total score | 25.12 (26.28) | 27.08 (27.09) | 23.63 (25.66) |
| COIS-Rb Parent total score | 28.46 (24.72) | 28.91 (25.84) | 28.11 (23.93) |
| Comorbid diagnoses, %c | |||
| Anxiety disorders | 47% | 65% | 33% |
| Depressive disorders | 9% | 12% | 7% |
| ADHD | 12% | 10% | 13% |
| Oppositional defiant disorder | 5% | 7% | 3% |
| Conduct disorder | 1% | 1% | 0% |
| Tourette/chronic tic disorder | 9% | 10% | 8% |
Note: ADHD = attention-deficit/hyperactivity disorder.
CYBOCS = Children’s Yale-Brown Obsessive Compulsive Scale.31
COIS-R = Children’s Obsessive Compulsive Impact Scale-Revised.35
Anxiety disorders include generalized anxiety, separation anxiety, and social phobia; depressive disorders include major depressive disorder and dysthymia; attention-deficit/hyperactivity disorder includes inattentive, hyperactive, and combined subtypes; Tourette/chronic tic disorder includes Tourette’s disorder and chronic vocal and motor tic disorders.
p < .05
In addition to characterizing the hoarding phenotype across demographic and other clinical characteristics, we aimed to test age continuously as a putative moderator between the presence of hoarding symptoms and outcomes of interest. Specifically, we tested whether age moderated the relationship between the presence of hoarding symptoms and other clinical variables (Aim 1: OCD severity and impairment), diagnostic comorbidity (Aim 2: total number of comorbid diagnosis; internalizing and/or externalizing comorbidity), and treatment (Aim 3: treatment response; OCD severity reduction). Across aims, analysis of covariance was used for continuous outcomes, and binomial and multinomial logistic regression was used for categorical outcomes (including treatment response on the CGI-I). All models included group (hoarding versus no hoarding symptoms), age (continuous), and a group × age interaction. We decided a priori that if the interaction term was not significant, it would be dropped from models, and that (in the absence of significant interaction) if age was not a significant predictor, age would also be dropped from models, to explore the potential significance of group on outcome excluding nonsignificant terms. For the analysis of covariance testing CBT response on the CYBOCS total severity score from pre- to posttreatment, time was included as a repeated-measures factor.
RESULTS
Sample Characterization
Youths were 7 to 17 years of age (mean = 12.25, SD = 2.75), 57% female, and identified as 74% white, 11% Hispanic, 4% Asian, 1% African American, 1% American Indian, and 9% mixed. All youths were diagnosed with primary OCD, and 14% were on psychotropic medications. Additional demographic and clinical information for the total sample and by hoarding group are presented in Table 1.
Of the total sample, 43% of youths reported current hoarding symptoms: 8% reported hoarding obsessions, 9% reported hoarding compulsions, and 26% reported both hoarding obsessions and compulsions. Youths with versus without hoarding symptoms did not significantly differ in regard to age [t (213) = 0.45, p =.65], minority status [χ2 (1) = 0.00, p =.99], or psychotropic medications [χ2 (1) = 0.95, p =.33]. Although approximately half (51%) of girls reported hoarding symptoms, only 37% of boys reported hoarding [χ2 (1) = 4.52, p =.03]. All youths (100%) in the hoarding group met for OCD symptoms (eg, washing/cleaning; checking, symmetry, etc) on the CYBOCS symptom checklist.
OCD Severity and Impairment
In regard to OCD severity (CYBOCS total score), there was not a significant group × age interaction (F1,211 = 0.57, p =.44), nor were there significant main effects of group (F1,211 = 0.15, p =.70) or age [F1,211 = 3.43, p =.07]. When age and the interaction term were removed from the model, the effect of group remained nonsignificant (F1,213 = 2.53, p =.11), such that OCD severity did not differ between youths with (mean = 25.43, SD = 3.93) versus without (mean = 24.49, SD = 4.58) hoarding symptoms. For youth-reported OCD-related impairment (COIS-R child report), there was no significant group × age interaction (F1,211 = 0.99, p =.32), nor were there significant main effects of group (F1,211 = 0.56, p =.46) or age (F1,211 = 2.68, p =.12). When age and the interaction term were removed from the model, the effect of group remained nonsignificant (F1,213 = 0.86, p =.35), such that youth-rated OCD-related impairment did not differ between youths with (mean = 27.08, SD = 27.06) and without (mean = 23.63, SD = 25.66) hoarding symptoms. In parallel, for parent-reported OCD-related impairment (COIS-R parent report), there was no significant group × age interaction (F1,211 = 1.22, p =.27), or significant main effects of group (F1,211 = 1.04, p =.31) or age (F1,211 = 2.68, p =.10). When age and the interaction term were removed from the model, the effect of group remained nonsignificant (F1,213 = 0.05, p =.82) such that parentrated OCD-related impairment did not differ between youths with (mean = 28.91, SD = 25.84) and without (mean = 28.11, SD = 23.93) hoarding symptoms.
Comorbid Diagnoses
There was a significant main effect of group on the total number of internalizing (anxiety, depression) and externalizing (ADHD, oppositional defiant disorder, conduct disorder) diagnoses, but no main effect of age (F1,211 = 1.05, p =.31), and no group × age interaction (F1,211 = 0.001, p =.98). When age and the interaction term were removed from the model, youths with hoarding symptoms had a greater total number of comorbid diagnoses (mean = 1.5, SD = 1.32) than those without hoarding symptoms (mean = 0.78, SD = 0.93; F1,213 = 21.98, p <.001).
Youth were also split into those with (internalizing, externalizing, both internalizing and externalizing) and without comorbid diagnoses. Age was not a significant predictor (p values ranged from .23 to .74) and there was no significant group × age interaction (p values ranged from .0 to .82) for any comorbid diagnostic category. When age and the interaction were removed from the model, youths with hoarding symptoms compared to those without hoarding symptoms were more likely to have concurrent internalizing disorders (odds ratio [OR] = 4.89, SE = 0.43, p <.001, 95% CI = 2.12—11.25) and both internalizing and externalizing disorders (OR = 3.20, SE = 0.86, p =.02, 95% CI = 1.74—9.94), but not externalizing disorders only (OR= 1.71, SE = 0.86,p =.80,95% CI = −0.05 to 5.39).
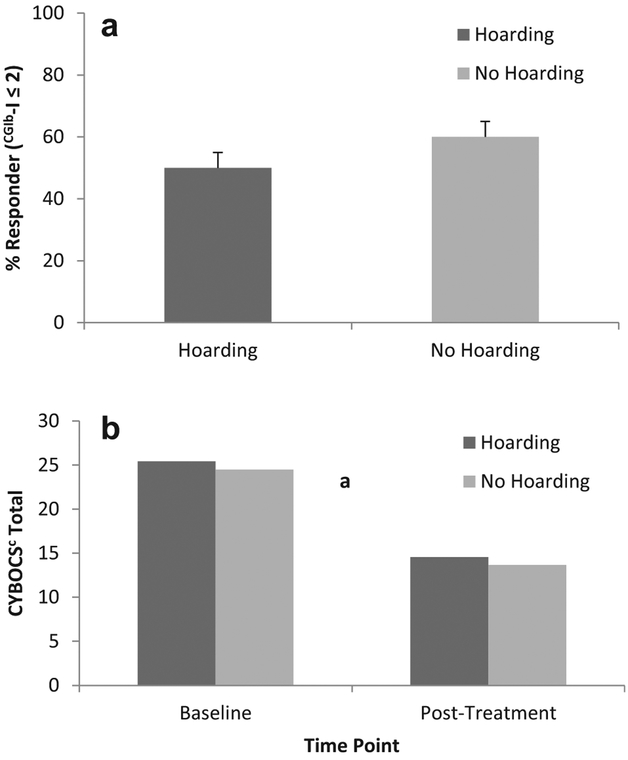
Treatment Response and Symptom Reduction Following CBT
With respect to treatment response (CGI-I), there was no significant group × age interaction (OR = 0.82, SE = 0.13, p =.14, 95% CI = 0.64—1.06), nor were there significant main effects of group (OR = 17.50, SE = 1.66, p =.08, 95% CI = 0.68—8.22) or age (OR = 1.03, SE =.10, p =.80, 95% CI = 0.84—1.25). When age and the interaction term were removed from the model, the effect of group remained nonsignificant (OR = 1.52, SE = 0.36, p =.25; 95% CI = 0.75—3.07) (Figure 1a), such that youths with and without hoarding symptoms did not significantly differ in rates of treatment response (50% versus 60%). Similarly, in regard to change in CYBOCS severity from pre- to posttreatment, there was no significant group × age interaction (F1,130 = 1.67, p =.16), nor were there significant main effects of group (F1,130 = 2.28, p =.08) or age (F1,130 = 0.82, p =.37). When age and the interaction term were removed from the model, the effect of group remained nonsignificant (F1,130 = 0.20, p =.66) (Figure 1b), with comparable reduction in CYBOCS score between youths with (mean difference = 10.24, SD = 7.63) and without (mean difference = 10.90, SD = 8.59) hoarding symptoms.
FIGURE 1.
Treatment Response and Symptom Reduction After Receipt of Cognitive-Behavioral Therapy (CBT) in Youths With and Without Hoarding Symptoms
aIndicates significant reduction in both groups from pre- to post-CBT(p <.05), although the hoarding symptom group did not differ from the no hoarding symptom group at either pre- or posttreatment.
bCGI-I = Clinical Global Impressions-Improvement.36
cChildren’s Yale-Brown Obsessive Compulsive Scale.31
DISCUSSION
Hoarding is increasingly recognized as a chronic, impairing condition with public health implications5,38; yet, little is known about its manifestations in pediatric populations. We examined the clinical phenomenology and response to CBT treatment in youths with primary OCD who did versus did not report hoarding symptoms, and explicitly examined the potential moderating role of youth age. We hypothesized that, as youth age increased, hoarding symptoms would be associated with more severe OCD symptoms, impairment, and comorbidity profiles, as well as poorer treatment response.
Broadly, our findings did not support our developmental hypothesis: across all analyses, age did not moderate the relationship between the presence of hoarding symptoms and clinical or treatment outcome variables. These results provide initial support for the observation that adolescents with OCD and hoarding symptoms do not appear to have more severe OCD symptoms, impairment, or comorbidity profiles than children with OCD and hoarding. These data are in contrast to findings from the adult literature that suggest that adult hoarders tend to have more functional impairment and worse diagnostic profiles as they age.39 Interestingly, adult hoarders tend to report symptom onset during the pediatric period,13,23,39 although there is some evidence to suggest that the mean age of clutter and difficulty discarding (~ 16 years) may precede acquisition symptoms (~18 years40). This is not surprising, as youths often do not have the financial resources or control over their living space that might allow for excessive acquisition. Thus, it may be possible that our age range (7—17 years) precluded our ability to detect the adverse effects of hoarding during the transition to adulthood. Future investigations of hoarding might explore the moderating role of age from childhood through adulthood to identify the developmental window at which hoarding symptoms worsen and result in more substantial impairments, as well as the role of parents or other caretakers in accommodating hoarding (or refusal to do so).
Our hypotheses were partially supported with respect to comparing OCD-affected youths with and without hoarding symptoms. In contrast to some prior findings with youth,18,19 we did not find group differences in OCD severity or youth- or parent-reported OCD-related impairment. However, consistent with other research17,18,20 and as hypothesized, we found group differences in comorbidity profiles, such that youths with hoarding symptoms had a greater number of comorbid diagnoses and, particularly, concurrent internalizing and both internalizing and externalizing disorders, than those without hoarding symptoms. Thus, although impairment may not differ between youths who report hoarding compared to those who do not, their co-occurring psychopathology may complicate their clinical presentation and shape their subsequent treatment plan.
Finally, in contrast to our hypotheses and prior findings in adults,21 and consistent with a prior, smaller investigation in youths,22 in this sample we did not find statistically significant group differences between youths with and without hoarding symptoms in treatment response or OCD symptom severity reduction following CBT. This finding is generally consistent with our other results. If replicated, these findings may suggest that the adult hoarding literature may not accurately reflect the presentation, age-related impairment, or treatment response for youths with hoarding symptoms. In the context of the adult literature, our findings may suggest that the impairment-related sequelae of hoarding may not become evident until adulthood; it would therefore follow that hoarding may not result in worse treatment outcome until adulthood either. Nonetheless, we are encouraged by these findings as, clinically, they provide initial support for the notion that the presence of hoarding symptoms might not negatively influence CBT response in youths with OCD.
This investigation is not without its limitations. First, as with prior investigations,17,18 the way in which the sample was ascertained and our measurement of hoarding symptoms may not fully reflect the population of youths with hoarding. Youths were recruited prior to DSM-5 for primary OCD (which, at the time, included hoarding symptoms). In addition, we used a diagnostic tool (ADIS-IV)28 in which hoarding symptoms are conceptualized as part of an OCD diagnosis. Thus, we are unable to explore whether youths in our sample would have met criteria for a hoarding disorder diagnosis in addition to OCD, or whether they would only have met criteria for subclinical hoarding symptoms. For some participants, it is possible that the symptoms classified in the DSM-IV-TR OCD (or on the ADIS-IV) would have been fully accounted for by a hoarding disorder diagnosis in DSM-5 or on the newer version of the ADIS created to reflect the DSM-5. Next, we dichotomized youths into those who did versus did not endorse hoarding symptoms on the CYBOCS. Although such categorization to identify symptom type has been validated in youths,33,34 it likely does not fully capture the clinical presentation or severity of hoarding symptoms. Categorization of youths into groups of those who do versus do not endorse hoarding symptoms may not generalize to youths who present with hoarding disorder or subclinical hoarding symptoms in the absence of OCD symptoms. Thus, the present findings are limited to conceptualization of hoarding symptoms as acquired on the CYBOCS symptom checklist, and may not generalize to youths with hoarding disorder or those with hoarding symptoms not directly assessed by the CYBOCS symptom checklist. Future investigations might use recently published measures that are specifically designed to assess hoarding behaviors in youths41 and assess both diagnostic categorization and hoarding-specific severity and impairment. In addition, a lack of statistically significant differences between groups does not confirm a true lack of difference between groups; we look forward to future replication studies in youths with primary OCD and those with primary hoarding disorder. Finally, the current sample was primarily of white ethnicity, which may limit our ability to generalize these findings to minority youths.
In summary, 43% of our sample reported hoarding symptoms, and all youths in the hoarding group also reported symptoms from at least one other OCD cluster. These data suggest that, particularly during the pediatric period, hoarding should be assessed as part of standard OCD symptom assessment and vice versa. Moreover, this study provides preliminary support for the notion that the findings from the adult hoarding literature may not necessarily be applied to youths with OCD and hoarding symptoms. In contrast to the adult literature, which has found that hoarding symptoms are associated with a worse clinical picture as adults age, our findings provide initial support that youths with hoarding symptoms do not have worse OCD severity, impairment, or treatment outcome, although they may have greater rates of diagnostic comorbidity. Future work might seek to understand the progression of hoarding from childhood through adulthood in both cross-sectional and longitudinal investigations, with an eye toward identifying sensitive developmental windows in which hoarding begins to be associated with greater impairment and less favorable treatment outcome.
Acknowledgments
Support for work on this manuscript was provided as follows: Dr. Rozenman received research support from the UCLA Clinical Translational Science Institute (UL1TR000124), the UCLA Friends of Semel Research Scholar Program, and the International OCD Foundation (IOCDF); Dr. McGuire received support from the Tourette Syndrome Association (TSA); Dr. Wu received support from the UCLA T32 in Psychobiological Sciences; Dr. Ricketts received support from the National Institute of Mental Health (NIMH; K23MH113884) and TSA; Dr. Peris received support from NIMH (R01MH110476 and K23MH085058); Dr. Chang received support from NIMH (R34MH109601); and Dr. Piacentini received support from NIMH (R01 MH081864), IOCDF, and TSA.
All authors meet all four JAACAP authorship criteria, including conception and design of study or analysis and interpretation of data; article drafts and revisions critical to intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
The authors would like to acknowledge and thank the youths and families who participated in this research.
Disclosure: Dr. Peris has received grant support from NIMH and royalties from Oxford University Press, including for manuals for the CBT described in this study. Dr. O’Neill has received grant support from NIMH. Dr. Bergman has received royalties from Oxford University Press, including for manuals for the CBT described in this study. Dr. Chang has received grant support from NIMH and royalties from Oxford University Press, including for manuals for the CBT described in this study. Dr. Piacentini has received grant support from NIMH. He has received royalties from Oxford University Press, including for manuals for the CBT described in this study, Guilford Press, and the American Psychological Association. He has served on the speakers’ bureau for the TSA. Drs. Rozenman, McGuire, Wu, and Ricketts report no biomedical financial interests or potential conflicts of interest.
REFERENCES
- 1.Steketee G, Frost R. Compulsive hoarding: current status of the research. Clin Psychol Rev. 2003;23:905–927. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 3.Mueller A, Mitchell JE, Crosby RD, Glaesmer H, de Zwaan M. The prevalence of compulsive hoarding and its association with compulsive buying in a German population-based sample. Behav Res Ther. 2009;47:705–709. [DOI] [PubMed] [Google Scholar]
- 4.Samuels J, Bienvenu O, Grados M. Prevalence and correlates of hoarding behavior in a community-based sample. Behav Res Ther. 2008;46:836–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burton CL, Arnold PD, Soreni N. Three reasons why studying hoarding in children and adolescents is important. J Can Acad Child Adolesc Psychiatry. 2015;24:128–130. [PMC free article] [PubMed] [Google Scholar]
- 6.Frost RO, Steketee G, Williams LF,Mood Warren R, personality disorder symptoms and disability in obsessive compulsive hoarders: a comparison with clinical and nonclinical controls. Behav Res Ther. 2000;38:1071–1081. [DOI] [PubMed] [Google Scholar]
- 7.McGuire JF, Kaercher L, Park JM, Storch EA. Hoarding in the community: a code enforcement and social service perspective. J Soc Serv Res. 2013;39:335–344. [Google Scholar]
- 8.Kress VE, Stargell NA, Zoldan CA, Paylo MJ. Hoarding disorder: diagnosis, assessment, and treatment. J Couns Dev. 2016;94:83–90. [Google Scholar]
- 9.Ong C, Pang S, Sagayadevan V, Chong SA, Subramaniam M. Functioning and quality of life in hoarding: a systematic review. J Anxiety Disord. 2015;32:17–30. [DOI] [PubMed] [Google Scholar]
- 10.Thew GR, Salkovskis PM. Hoarding among older people: an evaluative review. Cogn Behav Ther. 2016;9:e32. [Google Scholar]
- 11.Tolin DF, Frost RO, Steketee G, Muroff J. Cognitive behavioral therapy for hoarding disorder: a meta-analysis. Depress Anxiety. 2015;32:158–166. [DOI] [PubMed] [Google Scholar]
- 12.Williams M, Viscusi JA. Hoarding disorder and a systematic review of treatment with cognitive behavioral therapy. Cogn Behav Ther. 2016;45:93–110. [DOI] [PubMed] [Google Scholar]
- 13.Tolin DF, Meunier SA, Frost RO, Steketee G. Course of compulsive hoarding and its relationship to life events. Depress Anxiety. 2010;27:829–838. [DOI] [PubMed] [Google Scholar]
- 14.Ivanov VZ, Mataix-Cols D, Serlachius E, et al. Prevalence, comorbidity and heritability of hoarding symptoms in adolescence: a population based twin study in 15-year olds. PLoS One. 2013;8:e69140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mataix-Cols D, Frost RO, Pertusa A, et al. Hoarding disorder: a new diagnosis for DSM- V? Depress Anxiety. 2010;27:556–572. [DOI] [PubMed] [Google Scholar]
- 16.Storch E, Rahman O, Park J. Compulsive hoarding in children. J Clin Psychology. 2011Available at:http://onlinelibrary.wiley.com/doi/10.1002/jclp.20794/full. Accessed April 6, 2016. [DOI] [PubMed] [Google Scholar]
- 17.Storch E, Lack C, Merlo L. Clinical features of children and adolescents with obsessive-compulsive disorder and hoarding symptoms. Comp Psychiatry. 2007;48:313–318. [DOI] [PubMed] [Google Scholar]
- 18.Samuels J, Grados MA, Riddle MA, et al. Hoarding in children and adolescents with obsessive-compulsive disorder. J Obsessive Compuls Relat Disord. 2014;3:325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masi G, Millepiedi S, Perugi G, et al. A naturalistic exploratory study of the impact of demographic, phenotypic and comorbid features in pediatric obsessive-compulsive disorder. Psychopathology. 2010;43:69–78. [DOI] [PubMed] [Google Scholar]
- 20.Mataix-Cols D, Nakatani E, Micali N, Heyman I. structure of obsessive-compulsive symptoms in pediatric OCD. J Am Acad Child Adolesc Psychiatry. 2008;47:773–778. [DOI] [PubMed] [Google Scholar]
- 21.Bloch MH, Bartley CA, Zipperer L, et al. Meta-analysis: hoarding symptoms associated with poor treatment outcome in obsessive-compulsive disorder. Mol Psychiatry. 2014;19: 1025–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Storch EA, Merlo LJ, Larson MJ, et al. Symptom dimensions and cognitive-behavioural therapy outcome for pediatric obsessive-compulsive disorder. Acta Psychiatr Scand. 2008;117:67–75. [DOI] [PubMed] [Google Scholar]
- 23.Dozier ME, Porter B, Ayers CR. Age of onset and progression of hoarding symptoms in older adults with hoarding disorder. Aging Ment Health. 2016;20:736–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park JM, McGuire JF, Storch EA. Compulsive Hoarding in Children. New York: Oxford University Press; 2014. [Google Scholar]
- 25.O’Neill J, Piacentini J, Chang S, et al. Glutamate in pediatric obsessive-compulsive disorder and response to cognitive-behavioral therapy: randomized clinical trial. Neuropsychopharmacology. 2017;42:2414–2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peris TS, Rozenman MS, Sugar CA, McCracken JT, Piacentini J. Targeted family intervention for complex cases of pediatric obsessive-compulsive disorder: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2017;56:1034–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piacentini J, Bergman RL, Chang S, et al. Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2011;50: 1149–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silverman W, Albano A. The Anxiety Disorders Interview Schedule for Children for DSM-IV: (Child and Parent Versions). San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 29.Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Am Acad Child Adolesc Psychiatry. 2001;40:937–944. [DOI] [PubMed] [Google Scholar]
- 30.Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Clin Child Adolesc Psychol. 2002;31: 335–342. [DOI] [PubMed] [Google Scholar]
- 31.Scahill L, Riddle MA, McSwiggin-Hardin M, et al. Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36: 844–852. [DOI] [PubMed] [Google Scholar]
- 32.Storch EA, Murphy TK, Geffken GR, et al. Psychometric evaluation of the Children’s Yale-Brown Obsessive-Compulsive Scale. Psychiatry Res. 2004;129:91–98. [DOI] [PubMed] [Google Scholar]
- 33.Stewart SE, Rosario MC, Brown TA, et al. Principal components analysis of obsessive-compulsive disorder symptoms in children and adolescents. Biol Psychiatry. 2007;61: 285–291. [DOI] [PubMed] [Google Scholar]
- 34.Stewart SE, Rosario MC, Baer L, et al. Four-factor structure of obsessive-compulsive disorder symptoms in children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry. 2008;47:763–772. [DOI] [PubMed] [Google Scholar]
- 35.Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M. Functional impairment in childhood OCD: development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale—Revised (COIS-R). J Clin child Adolesc Psychol. 2007;36: 645–653. [DOI] [PubMed] [Google Scholar]
- 36.Guy W, editor ECDEU Assessment Manual for Psychopharmacology Rockville, MD: US Department of Heath, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration; 1976. [Google Scholar]
- 37.Piacentini J, Langley A, Roblek T. Cognitive-Behavioral Treatment of Childhood OCD:It’s Only a False Alarm: Therapist Guide. New York: Oxford University Press; 2007. [Google Scholar]
- 38.Frost R, Tolin D, Steketee G. Excessive acquisition in hoarding. J Anxiety Disord. 2009; 23:632–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ayers C, Saxena S. Age at onset and clinical features oflate life compulsive hoarding. Int J Anxiety Disorders. 2010. Available at:http://onlinelibrary.wiley.com/doi/10.1002/gps.2310/abstract. Accessed April 6, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grisham J, Frost R, Steketee G. Age of onset of compulsive hoarding. J Anxiety Disorders. 2006;20:675–686. [DOI] [PubMed] [Google Scholar]
- 41.Storch EA, Muroff J, Lewin AB, et al. Development and preliminary psychometric evaluation of the Children’s Saving Inventory. Child Psychiatry Hum Dev. 2011;42: 166–182. [DOI] [PubMed] [Google Scholar]