Abstract
Purpose
Activated leukocyte cell adhesion molecule (ALCAM), a member of the immunoglobulin superfamily, is highly expressed on dendritic cells. ALCAM and its receptor CD6 are co-stimulatory molecules in the immunological synapse; their interaction is required for T cell activation. While atopic dermatitis (AD) is recognized as a T helper 2 (Th2)-mediated allergic disease, the role of ALCAM in its pathogenesis is unclear.
Methods
ALCAM levels were measured in the serum of AD patients and AD-induced murine model by ovalbumin treatment. We next investigated transepidermal water loss, clinical score, Th2-immune responses, skin barrier gene expression and T-cell activation using wild-type (WT) and ALCAM deficiency mice. An oxazolone-induced AD-like model was also established and analyzed using WT- and ALCAM-deficient mice.
Results
We found that serum ALCAM levels were elevated in pediatric AD patients as well as WT AD mice, whereas Th2-type cytokine production and AD symptoms were suppressed in ALCAM-deficient mice. In addition, CD4+ effector T-cell counts in murine skin and skin-draining lymph nodes were lower in ALCAM-deficient mice than in their WT counterparts. ALCAM deficiency was also linked to higher expression of skin barrier genes and number of lamellar bodies.
Conclusions
These findings indicate that ALCAM may contribute to AD pathogenesis by meditating a Th2-dominant immune response and disrupting the barrier function of the skin.
Keywords: ALCAM, CD166, atopic dermatitis, type 2 helper T cells, skin barrier
INTRODUCTION
Atopic dermatitis (AD) is a common inflammatory cutaneous disorder1 caused by complex interactions among environmental factors, changes in skin barrier function, and immune system.2,3 AD is a risk factor that can predispose an individual to allergic diseases such as asthma or rhinitis4,5 since disruption of the skin barrier in AD patients can lead to allergen sensitization, which can, in turn, induce allergic esophageal inflammation or food anaphylaxis.6,7
A number of studies have suggested that an imbalance in T helper (Th) 1/Th2 cells and skin barrier dysfunction contribute to AD pathogenesis.8 Defective skin barrier causes unregulated activation of proteases in the epidermis, leading to the production of Th2-type immune-inducing factors. AD is dominantly mediated by Th2 cells9,10 and is associated with increased immunoglobulin (Ig) E and the production of Th2 cytokines, such as interleukin (IL)-4 and IL-13 in AD lesions.11,12,13 Moreover, there is growing recognition that AD is not only associated with Th2 immune response, but that Th17 and Th22 inflammatory responses are also involved.14,15,16 Activated T cells are recruited to the skin in acute and chronic cutaneous inflammatory diseases.17 CD4+ T cells are key factors in allergic inflammatory diseases. Several studies have shown that inhibition of CD4+ T-cell activation inhibited Th1, Th2 and Th17 cell differentiation with capsiate treatment.18 These immune responses require specific signals for T-cell activation that engage receptor systems on T cells and dendritic cells (DCs). The initial interaction involves contact between T-cell receptor and the antigenic peptide bound to major histocompatibility complex class II on the DC surface,19 followed by adhesion and expression of co-stimulatory molecules on T cells (CD28, cytotoxic T-lymphocyte-associated protein-4 and CD6) and DCs (CD80/B7.1 and CD86/B7.2).20
Activated leukocyte cell adhesion molecule (ALCAM) is a transmembrane protein of the Ig superfamily21,22 that is expressed on a variety of cell types. CD6 is highly expressed on T cells and binds to ALCAM on DCs.23 Crosslinking of CD6 and ALCAM contributes to both early and later stages of T-cell proliferation,24 suggesting that the CD6-ALCAM interaction is necessary for maximum antigen-specific T-cell activation. Indeed, blocking this interaction with an antibody suppressed IL-2 production.25 Lymphocyte function-associated antigen 1 (LFA-1) and intercellular adhesion molecule (ICAM)-3 are also involved in effector T-cell function26; although this is similar to those of LFA-1 and ICAM-3 localized in the synapse, CD6-ALCAM accumulation at this site occurs independently of these adhesion molecules.23 Another study reported that the engagement of CD6 with ALCAM at the synapse provided the co-stimulatory signal for activation of γδ T cells in response to cell-associated non-peptide antigens in a way that was similar to activation of αβ T cells by peptide antigen-loaded DCs, which involved immunological synapse stabilization.27 It is thus likely that the CD6-ALCAM interaction affects diverse subsets of T cells.
Prior studies demonstrated that ALCAM contributes to ovalbumin (OVA)-induced allergic asthma and food allergy by stimulating T-cell activation and proliferation.28,29 Although ALCAM is associated with hypersensitivity and T cell activation in the initiation of immune responses, its function in AD has not yet been demonstrated. Therefore, the present study examined the role of ALCAM in AD pathogenesis using an OVA-induced AD-like allergic skin inflammation mouse model and compared ALCAM-deficient and wild-type (WT) mice in terms of molecular and histological changes.
MATERIALS AND METHODS
Subjects
ALCAM levels were measured in the serum of children who visited the allergy clinic at Severance Children's Hospital for AD or for a general health checkup between June 2010 and November 2014. Children with AD fulfilled the revised Hanifin and Rajka criteria30 and were subdivided into the following 3 groups according to disease severity based on the SCORing AD (SCORAD) index:31,32 mild (SCORAD index ≤ 25), moderate (25 < SCORAD index ≤ 50) and severe (SCORAD index > 50). They had no symptoms of other allergic diseases such as asthma or allergic rhinitis. Healthy controls had no history of AD or other allergic diseases such as asthma, allergic rhinitis, or inflammatory disease. At the first visit, blood samples were obtained from all subjects. Eosinophil count was determined using a hematological analyzer (NE-8000; Sysmex, Kobe, Japan), and IgE level was measured with the CAP assay (Pharmacia, Uppsala, Sweden). The study protocol was approved by the Institutional Review Board (IRB) of Severance Hospital, and written informed consent was obtained from subjects or their parents (IRB No. 4-2004-0036).
Skin biopsy samples were obtained from 1 healthy control and 1 AD patient who were diagnosed according to the criteria of Hanifin and Rajka.33 This study was approved by the IRB of Yonsei University Health System, Severance Hospital (No. 4-2013-0624), and informed consent was obtained from all subjects before they participated in the study. This study protocol was performed in accordance with the ethical guidelines of the Korean Bioethics and Safety Act.
Mice
C57BL/6 (B6) mice were purchased from Orient Bio (Sungnam, Korea). ALCAM-deficient mice on the B6 genetic background were purchased from Jackson Laboratory (Bar Harbor, ME, USA). Mice were maintained under pathogen-free conditions with controlled humidity and temperature. Animal experiments in this study were carried out in accordance with the Laboratory Animals Welfare Act, the Guide for the Care and Use of Laboratory Animals and the Guidelines and Policies for Rodent experiment provided by the Institutional Animal Care and Use Committee (IACUC) and were approved by the IACUC of the Yonsei University Health System (reference No.2014-0282).
Induction of AD
The OVA-induced AD model was established as previously described.34 Mice were anesthetized, and their back skin was shaved and tape-stripped 5 times with cellophane tapes (Nichiban, Tokyo, Japan). For epicutaneous (EC) sensitization, 100 μg OVA (grade V; Sigma-Aldrich, St. Louis, MO, USA) in 100 μL of normal saline was placed on a 1×1 cm2-patch of sterilized gauze attached to the dorsal skin with Tegaderm (1,624W; 3M Health Care, Maplewood, MN, USA). Mice were thus subjected to a total of three 1-week EC sensitizations with a 2-week interval between individual sensitization periods. Transepidermal water loss (TEWL; Delfin, Kuopio, Finland) and clinical score were assessed during the experimental period.
To induce oxazolone (OXA)-AD-like model, the dorsal skin of mice was sensitized with 50 μL of 3% OXA (Sigma-Aldrich) at day 0. After 5 days, the ear was challenged by 20 μL of 0.6% OXA every other day until day 13. TEWL, clinical score and ear thickness (Mitutoyo, Kanagawa, Japan) were measured during the experimental periods. On day 14, mice were sacrificed to collect the skin biopsy specimen and blood.
The clinical severity of skin lesions was scored according to the macroscopic diagnostic criteria that were used for the NC/Nga mouse. The severity of dermatitis was evaluated once a week, just before each elicitation. The development of 1) erythema/hemorrhage, 2) scarring/dryness, 3) edema and 4) excoriation/erosion was scored as 0 (none), 1 (mild), 2 (moderate) and 3 (severe). The average of the individual scores was taken as the clinical score.35
Quantitative real-time polymerase chain reaction (PCR)
AD skin lesion samples were obtained after the last sensitization to assess messenger RNA (mRNA) expression levels. Total RNA was isolated with TRIzol reagent (Invitrogen, Carlsbad, CA, USA), and 2 μg were used to synthesize complementary DNA using superscript II reverse transcriptase (Invitrogen). Quantitative real-time PCR was performed on an Applied biosystem (Foster City, CA, USA) and target gene levels were quantified with AccuPower Greenstar qPCR PreMix (Bioneer, Daejeon, Korea) according to the manufacturer's instructions. Forward and reverse primers for target gene amplification were synthesized by Integrated DNA Technologies (Coralville, IA, USA). The primer details are shown in Table 1. Target gene mRNA levels were quantified relative to that of β-actin.
Table 1. Sequences of the primers used for quantitative real-time polymerase chain reaction.
| Gene | Direction | Sequence |
|---|---|---|
| ALCAM | Forward | 5′-TGG TAC ACT GTC AAC TCA GCA-3′ |
| Reverse | 5′-ACC CAT CGG GCT TTT CAT ATT TC-3′ | |
| IL-4 | Forward | 5′-GGT CTC AAC CCC CAG CTA GT-3′ |
| Reverse | 5′-GCC GAT GAT CTC TCT CAA GTG AT-3′ | |
| IL-5 | Forward | 5′-CTC TGT TGA CAA GCA ATG AGA CG-3′ |
| Reverse | 5′-TCT TCA GTA TGT CTA GCC CCT G-3′ | |
| IL-13 | Forward | 5′-CCT GGC TCT TGC TTG CCT T-3′ |
| Reverse | 5′-GGT CTT GTG TGA TGT TGC TCA-3′ | |
| Filaggrin | Forward | 5′-CAC TGA GCA AAG AAG AGC TGA A-3′ |
| Reverse | 5′-CGA TGT CTT GGT CAT CTG GA-3′ | |
| Loricrin | Forward | 5′-TCC TTC CCT CAC TCA TCT TCC-3′ |
| Reverse | 5′-CTC CTC CAC CAG AGG TCT TT-3′ | |
| Involucrin | Forward | 5′-CTC CTG TGA GTT TGT TTG GTC T-3′ |
| Reverse | 5′-GGA TGT GGA GTT GGT TGC TT-3′ | |
| β-actin | Forward | 5′-GGC TGT ATT CCC CTC CAT CG-3′ |
| Reverse | 5′-CCA GTT GGT AAC AAT GCC ATG T-3′ |
Enzyme-linked immunosorbent assay (ELISA)
Mice were bled by cardiac puncture and serum was collected by centrifugation and stored at −70°C until use. Serum levels of total IgE were quantified with a specific ELISA kit (BD Biosciences, San Diego, CA, USA) according to the manufacturer's protocol. ALCAM levels in mouse skin homogenate were quantified by ELISA (R&D Systems, Minneapolis, MN, USA) according to manufacturer instructions.
Hematoxylin and eosin (H&E) staining
Dorsal skin was fixed in 10% buffered formalin, and samples were embedded in paraffin and cut into sections at a thickness of 4 μm that were mounted onto slides and stained with H&E. Histological changes were scored (0−4) according to the degree of inflammation, immune cell infiltration, edema and epithelial hyperplasia by visualization under a light microscope (BX40; Olympus, Center Valley, PA, USA).35
Electron microscopy
Skin samples were pre-fixed in Karnovsky's fixative solution (2% glutaraldehyde-paraformaldehyde in 0.1 M phosphate buffer, pH 7.4) for 7 days, then rinsed with phosphate-buffer saline and pre-fixed with 1% osmium tetroxide. Samples were dehydrated in a graded series of ethanol, then infiltrated with propylene oxide and embedded using the Ply/Bed 812 kit (Polysciences, Warrington, PA, USA). Thin sections (70 nm) were cut and stained with 7% uranyl acetate and lead citrate and observed under a JEM-1011 transmission electron microscope (JEOL, Tokyo, Japan). Images were obtained with a Mega View III camera (Olympus, Tokyo, Japan).
Flow cytometry
Cell suspensions were isolated from the skin and skin draining lymph nodes (LNs) of mice. To collect whole skin cells, skin was detached from the body and incubated for 1 hour in Roswell Park Memorial Institute (RPMI) 1640 medium (Hyclone, Logan, UT, USA) containing 1 mg/mL dispase II (Sigma-Aldrich). The samples were cut into small pieces and incubated for 1.5 hours in RPMI 1640 medium containing 10% fetal bovine serum (FBS), 0.8 mg/mL collagenase type II (Worthington Biochemical, Lakewood, NJ, USA), and 50 μg/mL DNase I (Roche, Freehold, NJ, USA).36 The LNs were cut into small pieces and digested in collagenase type II (0.5 mg/mL; Worthington Biochemical) or DNase I (Roche; 0.02 mg/mL) at 37°C for 45 minutes. Digested skin draining LNs and skin were passed through a 40-µm cell strainer (BD Biosciences). Red blood cells were lysed using ammonium chloride-potassium lysing buffer, and the remaining cells were washed and resuspended in phosphate-buffered saline (PBS) containing 5% FBS.
Single-cell suspensions were then stained with antibodies for flow cytometry. The following antibodies were used: CD3 (17A2), CD4 (GK1.5), CD44 (IM7), CD62L (MEL-14) and isotype controls (rat IgG) (eBioscience, San Diego, CA, USA). Fixable Viability Dye (eBioscience) was used to exclude dead cells. Stained cells were analyzed by flow cytometry using an LSR II (BD Biosciences), and data were analyzed with Flow Jo software (Tree Star, Ashland, OR, USA).
Statistical analysis
Continuous data were tested for normality using the Kolmogorov-Smirnov test or Shapiro-Wilk test and reported accordingly as the mean ± standard error of the mean. The Student's t-test and 1-way analysis of variance were used to evaluate differences between continuous variables. Categorical data are presented as counts and percentages, and the χ2 test was used for comparisons. Correlations between ALCAM level and SCORAD index were evaluated by Pearson correlation analysis. Statistical analyses were performed with SPSS v.20 software (SPSS Inc., Chicago, IL, USA). Differences were deemed significant at P < 0.05.
RESULTS
ALCAM levels are altered in serum from human AD and OVA-induced AD model
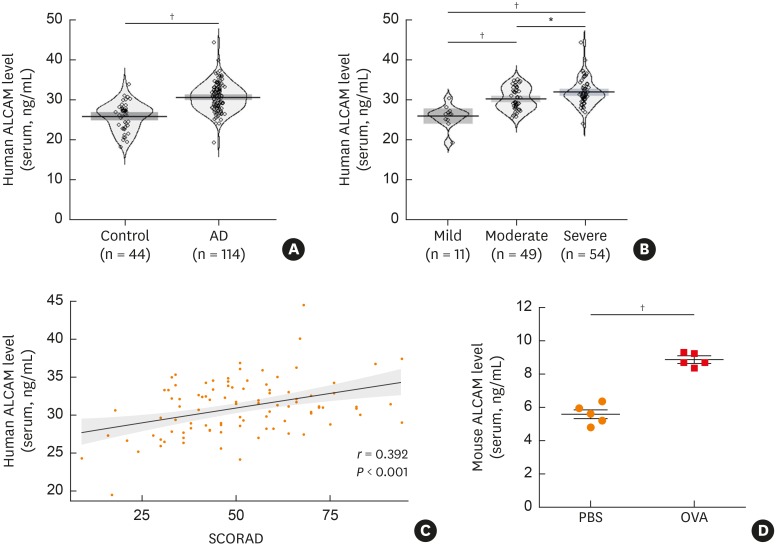
The clinical characteristics of the study subjects are summarized in Table 2. The AD group was significantly younger in age and included more males than the control group. Serum total eosinophil count and IgE level were higher in the AD group than in healthy controls, and the former also showed elevated serum ALCAM levels (26 ± 3.4 ng/mL vs. 30.8 ± 3.5 ng/mL, P < 0.001) (Fig. 1A) even after adjusting for age and sex (β = 3.68, P < 0.001). Moreover, ALCAM levels in children with AD tended to increase with AD severity (Fig. 1B), as evidenced by the positive correlation with the SCORAD score (r = 0.392, P < 0.001) (Fig. 1C).
Table 2. Characteristics of the study population.
| Characteristics | Control (n = 44) | Atopic dermatitis (n = 114) |
|---|---|---|
| Age (yr) | 8.9 ± 2.7 | 4.0 ± 4.0† |
| Sex (male) | 24 (54.5) | 89 (78.1)* |
| Blood eosinophils (/µL) | 183.7 ± 148.5 | 870.6 ± 767† |
| Total immunoglobulin E (IU/mL) | 45.7 ± 33.2 | 1,036.1 ± 1,262.2† |
Values represent mean ± standard deviation or number (%).
*P < 0.05; †P < 0.001 vs. healthy control (Student's t-test).
Fig. 1. ALCAM expression in pediatric AD patients and OVA-induced AD mice. (A-C) ALCAM level was measured by ELISA in serum samples from healthy controls (n = 44) and AD patients (n = 114). Pirate plots show the distribution of ALCAM levels for each group; horizontal lines represent means and boxes represent 95% confidence intervals. (A) ALCAM level in human serum. (B) Increase in serum ALCAM level as a function of AD severity increases. (C) Correlation between serum ALCAM level and AD SCORAD index. (D) Serum ALCAM abundance was assessed by ELISA.
The data represent mean ± standard error of the mean.
ALCAM, activated leukocyte cell adhesion molecule; AD, atopic dermatitis; OVA, ovalbumin; PBS, phosphate-buffered saline; SCORAD, SCORing atopic dermatitis; ELISA, enzyme-linked immunosorbent assay.
*P < 0.05; †P < 0.001 by t-test (n = 5–10 mice/group).
To examine whether development of OVA-sensitized AD can regulate the levels of ALCAM in WT mice. OVA-sensitized mice showed increased serum ALCAM level (Fig. 1D) compared to PBS mice.
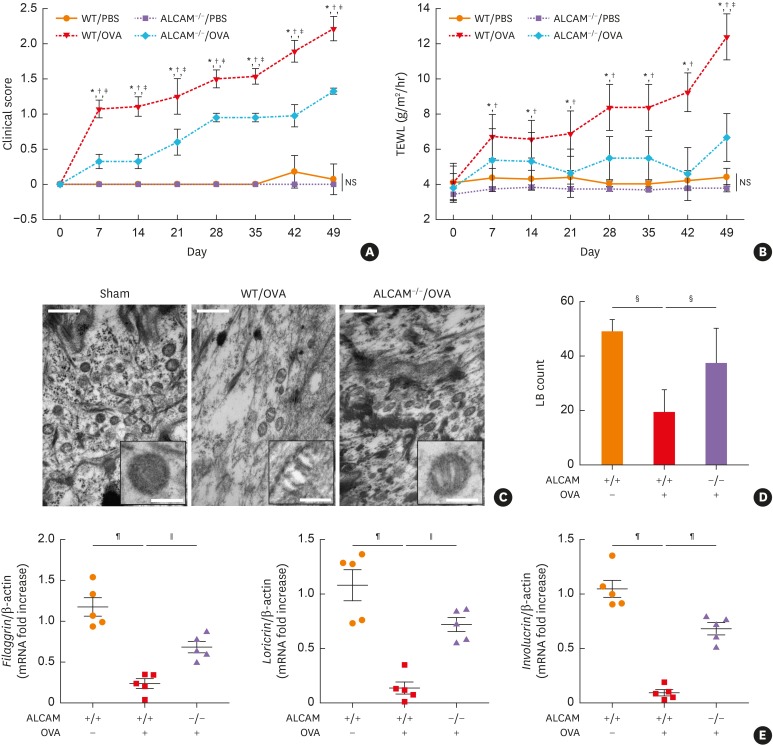
ALCAM deficiency alleviates skin barrier disturbance
One of the common features of AD is an impaired skin barrier. In this AD model, clinical score and TEWL level, which shows the abnormal skin barrier function, was significantly increased from day 7 in WT/OVA mice (Fig. 2A and B). However, ALCAM−/−/OVA mice had markedly decreased clinical score and TEWL compared to WT mice (Fig. 2A and B). We next examined lamellar body (LB) morphology and permeability barrier gene expression in ALCAM−/− and WT mice. LB is a unique organelle that delivers lipids to the stratum corneum. Failure of LB secretion was previously reported as a feature of AD.16,37 Electron microscopy demonstrated the empty and abnormal-shape of LBs in the epidermis of WT/OVA, whereas ALCAM−/−/OVA LBs showed normal density and shape (Fig. 2C, insert C). In addition, ALCAM−/−/OVA showed higher LB count than WT/OVA (Fig. 2D). Quantitative real-time PCR analysis revealed that the levels of skin barrier genes including filaggrin, loricrin and involucrin were downregulated in WT/OVA, an effect that was mitigated by ALCAM-deficient mice (Fig. 2E). These findings suggest that ALCAM regulates the skin barrier function in AD.
Fig. 2. ALCAM attenuates skin barrier disruption induced by epicutaneous OVA sensitization. (A) Time course of clinical score and (B) TEWL. (C) Electron micrographs of osmium tetroxide-postfixed skins show LBs in SG (×50,000, Scale bar = 0.5 μm; Insert C). (Left) Normal shaped LBs are present in sham mouse epidermis. (Middle) WT/OVA mouse epidermis shows severely abnormal LBs, (Right) Whereas LBs in ALCAM−/− mice display less abnormality (×120,000, Scale bar = 0.2 μm). (D) Bar graph represents the number of LBs in SG. (E) The mRNA expression of skin barrier genes (filaggrin, loricrin and involucrin).
The data represent mean ± standard error of the mean.
ALCAM, activated leukocyte cell adhesion molecule; TEWL, transepidermal water loss; OVA, ovalbumin; PBS, phosphate-buffered saline; NS, not significant; WT, wild-type; LB, lamellar body; mRNA, messenger RNA; SG, stratum granulosum.
*P < 0.05 (WT/PBS vs. WT/OVA); †P < 0.05 (ALCAM−/−/PBS vs. ALCAM−/−/OVA); ‡P < 0.05 (WT/OVA vs. ALCAM−/−/OVA); §P < 0.05; ∥P < 0.01; ¶P < 0.001 (n = 5–7 mice/group).
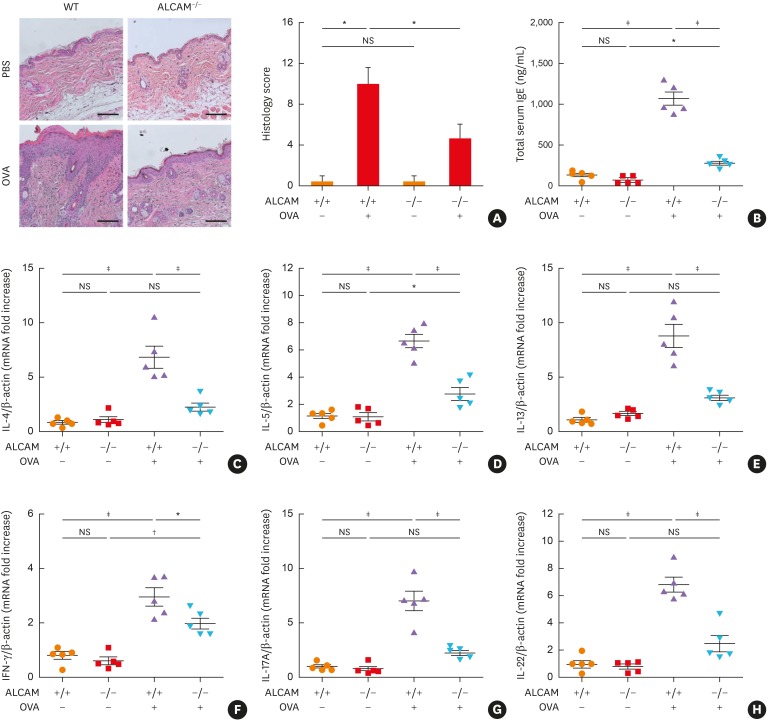
ALCAM deficiency suppresses Th-2 inflammation
To investigate the contribution of ALCAM to Th2 inflammation, ALCAM−/− and WT mice were epicutaneously sensitized with OVA, and their inflammatory responses were compared. Infiltration of inflammatory cells and histological score were significantly increased in WT mice compared to those in ALCAM−/− mice following the EC OVA treatments (Fig. 3A). Moreover, WT/OVA mice manifest significantly increased total IgE accumulation (Fig. 3B) and heightened IL-4, IL-5, IL-13, interferon (IFN)-γ, IL-17A and IL-22 mRNA expression (Fig. 3C-H) compared with ALCAM−/−/OVA mice.
Fig. 3. ALCAM deficiency attenuates T helper-dominant skin inflammation induced by epicutaneous OVA sensitization. (A) Mouse skin biopsy specimen stained with hematoxylin and eosin (×200, Scale bar = 50 μm) and scored according to histological features. (B) Serum levels of total IgE measured by enzyme-linked immunosorbent assay. (C-H) Skin mRNA levels were assessed by quantitative real-time polymerase chain reaction; (C) IL-4, (D) IL-5, (E) IL-13, (F) IFN-γ, (G) IL-17A and (H) IL-22.
The data represent mean ± standard error of the mean.
ALCAM, activated leukocyte cell adhesion molecule; NS, not significant; OVA, ovalbumin; PBS, phosphate-buffered saline; WT, wild-type; IgE, immunoglobulin E; IL, interleukin; IFN, interferon; mRNA, messenger RNA.
*P < 0.05; †P < 0.01; ‡P < 0.001 (n = 5–7 mice/group).
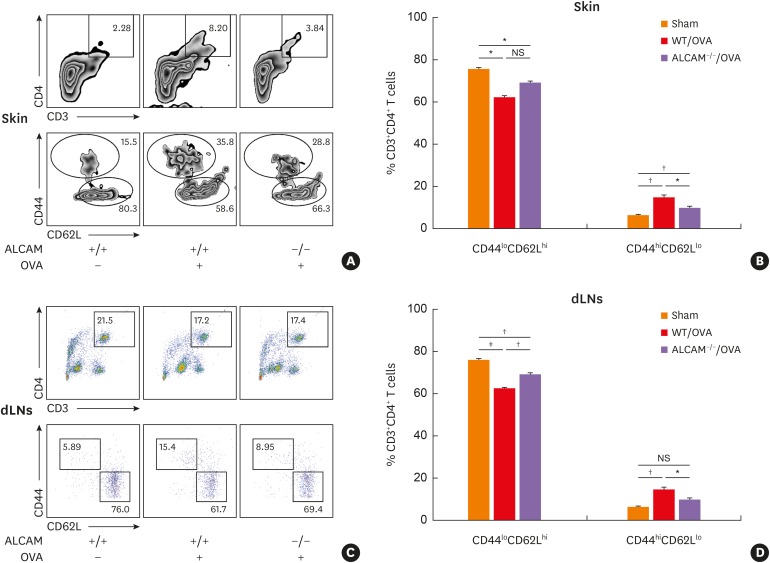
ALCAM deficiency suppresses CD4 T cell activation
Next, we investigated whether ALCAM deficiency affects Th2 cell activation in skin and skin-draining LNs by flow cytometry. After OVA sensitization, a lower accumulation of CD3+CD4+ T cells was detected in skin lesions (Fig. 4A) and skin draining LNs (Fig. 4C) of ALCAM-deficient mice than in those of WT mice. T cells were categorized as CD44loCD62Lhi (naïve), and CD44hiCD62Llo (effector memory).38 Interestingly, ALCAM-deficient mice had a reduced population of CD44hiCD62Llo cells in both skin and skin draining LNs relative to WT counterparts (Fig. 4A-D). These findings indicate that ALCAM mediates Th2-dominant inflammation via activation of CD4+ T cells in the skin and skin-draining LNs.
Fig. 4. ALCAM deficiency suppresses CD4+ T cell activation. Cells from the (A and B) skin and (C and D) skin draining -LN(dLN)s were harvested and stained for CD3, CD4, CD44 and CD62L. Cells were gated on CD3+CD4+ cells and then on CD44 and CD62L. Naïve cells are identified as CD44loCD62Lhi and effector cells as CD4hiCD62Llo. Representative dot plots are presented. Graphs represent percentage of (B) CD3+CD4+CD44loCD62Lhi in skin and (D) CD3+CD4+CD4hiCD62Llo in dLNs.
The data represent mean ± standard error of the mean.
ALCAM, activated leukocyte cell adhesion molecule; WT, wild-type; NS, not significant; OVA, ovalbumin; dLN, skin-draining lymph node.
*P < 0.05; †P < 0.01; ‡P < 0.001(n = 5–7 mice/group).
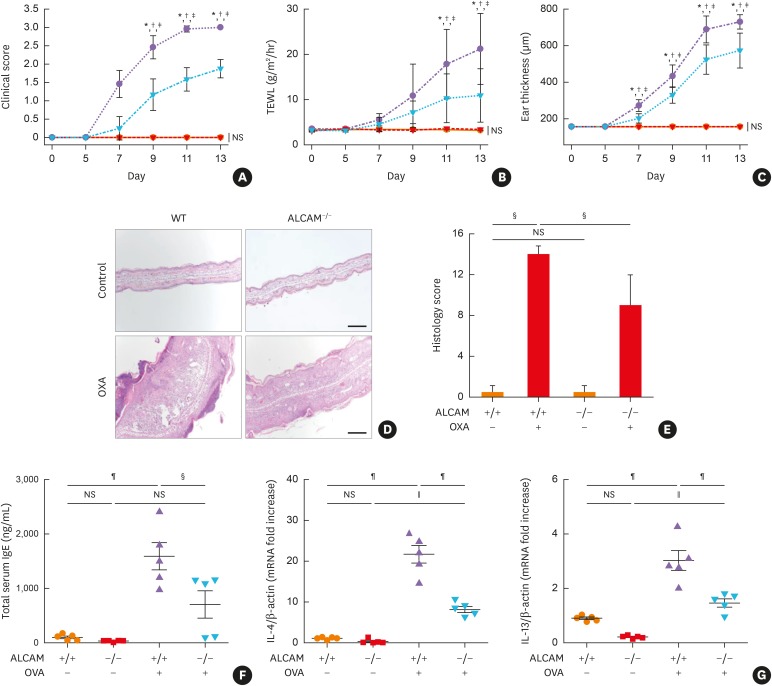
ALCAM deficiency suppresses skin inflammation and barrier disruption in the OXA- induced AD-like model
To further define the roles of ALCAM in allergic skin disease, we utilized AD-like mouse model that employed the OXA which could provoke an immune response. In these experiments, WT and ALCAM−/− mice were sensitized to and challenged with OXA, and the responses were evaluated. After OXA sensitization and challenge, WT mice manifest significantly increased clinical sore, TEWL and ear thickness compared to ALCAM−/− mice (Fig. 5A-C). Histological evaluations demonstrated enhanced epidermal thickness and epidermis inflammatory cell infiltration in comparisons of WT and ALCAM−/− mice (Fig. 5D and E). Next, we examined the total serum IgE level and tissue Th2 cytokines production. OXA-induced AD like WT mice showed increased total IgE accumulation (Fig. 5F) and heightened mRNA expression of IL-4 and IL-13 (Fig. 5G) compared to ALCAM−/− mice.
Fig. 5. ALCAM deficiency attenuates murine AD-like skin lesion induced by repeated OXA application. (A-C) AD severity was assessed by (A) clinical score, (B) TEWL and (C) ear thickness. (D) Mouse ear skin biopsy specimen stained with hematoxylin and eosin (×100, bar = 200 μm) and (E) scored according to histological features. (F) Total IgE level in serum, as determined by enzyme-linked immunosorbent assay. The mRNA expression of (G) IL-4 and IL-13 in skin lesions.
Data represent mean ± standard error of the mean.
ALCAM, activated leukocyte cell adhesion molecule; OXA, oxazolone; AD, atopic dermatitis; mRNA, messenger RNA; NS, not significant; WT, wild-type; TEWL, transepidermal water loss; IgE, immunoglobulin E; IL, interleukin, PBS, phosphate-buffered saline.
*P < 0.05 (WT/PBS vs. WT/OXA); †P < 0.05 (ALCAM−/−/PBS vs. ALCAM−/−/OXA); ‡P < 0.05 (WT/OXA vs. ALCAM−/−/OXA); §P < 0.05; ∥P < 0.01; ¶P < 0.001 (n = 4–6 mice/group).
The noted effects of ALCAM were not specific for allergens-induced inflammation because similar changes were noted in comparisons of skin tissues from ALCAM−/− and WT mice challenged with OXA.
DISCUSSION
In the present study, we addressed the involvement of ALCAM in AD pathogenesis using a murine model of OVA-induced AD. In our AD model, ALCAM levels were increased in serum relative to those in control mice. The serum ALCAM level was also more increased in AD patients that that in healthy controls; and was positively correlated with disease severity. Equivalent tendency of ALCAM alteration was described in our previous studies for allergic asthma and food allergy.28,29 Although alterations in ALCAM level have been described in various human cancers,21,24,39 alterations of ALCAM level in allergic disease has only recently been described, which is the first report providing evidence for the involvement of ALCAM in human AD.
Despite the repeated OVA exposure, ALCAM-deficient mice showed attenuated inflammatory responses and reduced production of Th2-type cytokines. We also observed a smaller population of CD3+CD4+ CD44hiCD62Llo T cells in the skin and skin-draining LNs of ALCAM-deficient AD mice. These results provide evidence that ALCAM is involved in AD pathogenesis.
A recent study showed that ALCAM is structurally similar to receptors for advanced glycation end products and can interact with S100B to activate nuclear factor κB signaling in delayed-type hypersensitivity diseases.40,41 Although ALCAM may be associated with other inflammatory signaling pathways, our findings provide evidence that ALCAM–CD6 interactions contribute to both early and later stages of DC-induced T-cell activation and proliferation. It has also been reported that ALCAM–CD6 modulates the activation of the mitogen-activated protein kinase, extracellular signal-regulated kinase 1/2, p38 and c-Jun N-terminal kinase cascades,24 which further supports our conclusion that ALCAM contributes to the immune response.
As confirmed by our data, mouse models of AD induced by EC sensitization are characterized by epidermal thickening, CD4+ T cell infiltration, and up-regulation of the Th2 cytokines, IL-4, IL-5 and IL-13.34 Th2 cytokines regulate skin homeostasis via the signal transducer and activator of transcription-6.42,43,44 Th2 inflammation also impairs the epidermal barrier, skin permeability, and cutaneous innate response.45 In AD mice, skin lesions showed reduced levels of skin barrier genes, filaggrin, loricrin, and involucrin and fewer lamellar bodies in the WT background than in the absence of ALCAM. Moreover, TEWL was less increased in ALCAM-deficient mice indicating the association of ALCAM with perturbation of the skin barrier. Hence, ALCAM may indirectly undermine the skin barrier function via modulation of the Th2 immune response.
In a psoriasis model, there is evidence that ALCAM affects T cell activation via Th17 cells.46 In the present study, ALCAM-deficient mice showed reduced expression of not only Th2 type cytokines but also IFN-γ, IL-17A and IL-22. As AD is a heterogeneous disease involving Th1, Th2 and Th17 cells, the role of ALCAM in the activation of various types of helper T cells and whether ALCAM expression levels differ in Th1, Th17 or Th2-dominated diseases need to be further elucidated.
In conclusion, the results presented here demonstrate that ALCAM can regulate Th2-type cytokine production and CD4+ T cell activation in AD-like skin lesions. In addition, our observations from clinical specimens suggest that ALCAM contributes to skin barrier dysfunction. These findings indicate that ALCAM mediates Th2-dominant immunological responses in AD pathogenesis and can be a potential target for disease treatment.
ACKNOWLEDGMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI17C0104) and by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2016R1D1A1B03933309) and the Ministry of Science, ICT & Future Planning (NRF-2017R1A2B2004043 and NRF-2018R1A5A2025079).
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
References
- 1.Yanaba K, Kamata M, Asano Y, Tada Y, Sugaya M, Kadono T, et al. CD19 expression in B cells regulates atopic dermatitis in a mouse model. Am J Pathol. 2013;182:2214–2222. doi: 10.1016/j.ajpath.2013.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Cesare A, Di Meglio P, Nestle FO. A role for Th17 cells in the immunopathogenesis of atopic dermatitis? J Invest Dermatol. 2008;128:2569–2571. doi: 10.1038/jid.2008.283. [DOI] [PubMed] [Google Scholar]
- 3.Peng W, Novak N. Pathogenesis of atopic dermatitis. Clin Exp Allergy. 2015;45:566–574. doi: 10.1111/cea.12495. [DOI] [PubMed] [Google Scholar]
- 4.Pyun BY. Natural history and risk factors of atopic dermatitis in children. Allergy Asthma Immunol Res. 2015;7:101–105. doi: 10.4168/aair.2015.7.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han DK, Kim MK, Yoo JE, Choi SY, Kwon BC, Sohn MH, et al. Food sensitization in infants and young children with atopic dermatitis. Yonsei Med J. 2004;45:803–809. doi: 10.3349/ymj.2004.45.5.803. [DOI] [PubMed] [Google Scholar]
- 6.Venturelli N, Lexmond WS, Ohsaki A, Nurko S, Karasuyama H, Fiebiger E, et al. Allergic skin sensitization promotes eosinophilic esophagitis through the IL-33-basophil axis in mice. J Allergy Clin Immunol. 2016;138:1367–1380.e5. doi: 10.1016/j.jaci.2016.02.034. [DOI] [PubMed] [Google Scholar]
- 7.Galand C, Leyva-Castillo JM, Yoon J, Han A, Lee MS, McKenzie AN, et al. IL-33 promotes food anaphylaxis in epicutaneously sensitized mice by targeting mast cells. J Allergy Clin Immunol. 2016;138:1356–1366. doi: 10.1016/j.jaci.2016.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhingra N, Gulati N, Guttman-Yassky E. Mechanisms of contact sensitization offer insights into the role of barrier defects vs. intrinsic immune abnormalities as drivers of atopic dermatitis. J Invest Dermatol. 2013;133:2311–2314. doi: 10.1038/jid.2013.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung DY, Boguniewicz M, Howell MD, Nomura I, Hamid QA. New insights into atopic dermatitis. J Clin Invest. 2004;113:651–657. doi: 10.1172/JCI21060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mamessier E, Magnan A. Cytokines in atopic diseases: revisiting the Th2 dogma. Eur J Dermatol. 2006;16:103–113. [PubMed] [Google Scholar]
- 11.Heeringa JJ, Fieten KB, Bruins FM, van Hoffen E, Knol EF, Pasmans SG, et al. Treatment for moderate to severe atopic dermatitis in alpine and moderate maritime climates differentially affects helper T cells and memory B cells in children. Clin Exp Allergy. 2018;48:679–690. doi: 10.1111/cea.13136. [DOI] [PubMed] [Google Scholar]
- 12.Hennino A, Vocanson M, Toussaint Y, Rodet K, Benetière J, Schmitt AM, et al. Skin-infiltrating CD8+ T cells initiate atopic dermatitis lesions. J Immunol. 2007;178:5571–5577. doi: 10.4049/jimmunol.178.9.5571. [DOI] [PubMed] [Google Scholar]
- 13.van der Heijden FL, Wierenga EA, Bos JD, Kapsenberg ML. High frequency of IL-4-producing CD4+ allergen-specific T lymphocytes in atopic dermatitis lesional skin. J Invest Dermatol. 1991;97:389–394. doi: 10.1111/1523-1747.ep12480966. [DOI] [PubMed] [Google Scholar]
- 14.Otsuka A, Nomura T, Rerknimitr P, Seidel JA, Honda T, Kabashima K. The interplay between genetic and environmental factors in the pathogenesis of atopic dermatitis. Immunol Rev. 2017;278:246–262. doi: 10.1111/imr.12545. [DOI] [PubMed] [Google Scholar]
- 15.Vandeghinste N, Klattig J, Jagerschmidt C, Lavazais S, Marsais F, Haas JD, et al. Neutralization of IL-17C reduces skin inflammation in mouse models of psoriasis and atopic dermatitis. J Invest Dermatol. 2018;138:1555–1563. doi: 10.1016/j.jid.2018.01.036. [DOI] [PubMed] [Google Scholar]
- 16.Heo WI, Lee KE, Hong JY, Kim MN, Oh MS, Kim YS, et al. The role of interleukin-17 in mouse models of atopic dermatitis and contact dermatitis. Clin Exp Dermatol. 2015;40:665–671. doi: 10.1111/ced.12567. [DOI] [PubMed] [Google Scholar]
- 17.Fuhlbrigge RC, King SL, Sackstein R, Kupper TS. CD43 is a ligand for E-selectin on CLA+ human T cells. Blood. 2006;107:1421–1426. doi: 10.1182/blood-2005-05-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee JH, Lee YS, Lee EJ, Lee JH, Kim TY. Capsiate inhibits DNFB-induced atopic dermatitis in NC/Nga mice through mast cell and CD4+ T-cell inactivation. J Invest Dermatol. 2015;135:1977–1985. doi: 10.1038/jid.2015.117. [DOI] [PubMed] [Google Scholar]
- 19.Fesenkova VI, Kurchenko AI, Castellani ML, Conti P, Anogeianaki A, Caraffa A, et al. Expression of co-stimulatory molecules on langerhans cells in lesional epidermis of human atopic dermatitis. Immunopharmacol Immunotoxicol. 2007;29:487–498. doi: 10.1080/08923970701675101. [DOI] [PubMed] [Google Scholar]
- 20.Gutcher I, Becher B. APC-derived cytokines and T cell polarization in autoimmune inflammation. J Clin Invest. 2007;117:1119–1127. doi: 10.1172/JCI31720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donizy P, Zietek M, Halon A, Leskiewicz M, Kozyra C, Matkowski R. Prognostic significance of ALCAM (CD166/MEMD) expression in cutaneous melanoma patients. Diagn Pathol. 2015;10:86. doi: 10.1186/s13000-015-0331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swart GW. Activated leukocyte cell adhesion molecule (CD166/ALCAM): developmental and mechanistic aspects of cell clustering and cell migration. Eur J Cell Biol. 2002;81:313–321. doi: 10.1078/0171-9335-00256. [DOI] [PubMed] [Google Scholar]
- 23.Zimmerman AW, Joosten B, Torensma R, Parnes JR, van Leeuwen FN, Figdor CG. Long-term engagement of CD6 and ALCAM is essential for T-cell proliferation induced by dendritic cells. Blood. 2006;107:3212–3220. doi: 10.1182/blood-2005-09-3881. [DOI] [PubMed] [Google Scholar]
- 24.Weidle UH, Eggle D, Klostermann S, Swart GW. ALCAM/CD166: cancer-related issues. Cancer Genomics Proteomics. 2010;7:231–243. [PubMed] [Google Scholar]
- 25.Hassan NJ, Simmonds SJ, Clarkson NG, Hanrahan S, Puklavec MJ, Bomb M, et al. CD6 regulates T-cell responses through activation-dependent recruitment of the positive regulator SLP-76. Mol Cell Biol. 2006;26:6727–6738. doi: 10.1128/MCB.00688-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Islam SA, Luster AD. T cell homing to epithelial barriers in allergic disease. Nat Med. 2012;18:705–715. doi: 10.1038/nm.2760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kato Y, Tanaka Y, Hayashi M, Okawa K, Minato N. Involvement of CD166 in the activation of human gamma delta T cells by tumor cells sensitized with nonpeptide antigens. J Immunol. 2006;177:877–884. doi: 10.4049/jimmunol.177.2.877. [DOI] [PubMed] [Google Scholar]
- 28.Kim MN, Hong JY, Shim DH, Sol IS, Kim YS, Lee JH, et al. Activated leukocyte cell adhesion molecule stimulates the T-cell response in allergic asthma. Am J Respir Crit Care Med. 2018;197:994–1008. doi: 10.1164/rccm.201703-0532OC. [DOI] [PubMed] [Google Scholar]
- 29.Kim YS, Kim MN, Lee KE, Hong JY, Oh MS, Kim SY, et al. Activated leucocyte cell adhesion molecule (ALCAM/CD166) regulates T cell responses in a murine model of food allergy. Clin Exp Immunol. 2018;192:151–164. doi: 10.1111/cei.13104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol. 2003;49:1088–1095. doi: 10.1016/s0190-9622(03)02539-8. [DOI] [PubMed] [Google Scholar]
- 31.Severity scoring of atopic dermatitis: the SCORAD index. Consensus report of the European task force on atopic dermatitis. Dermatology. 1993;186:23–31. doi: 10.1159/000247298. [DOI] [PubMed] [Google Scholar]
- 32.Oranje AP, Glazenburg EJ, Wolkerstorfer A, de Waard-van der Spek FB. Practical issues on interpretation of scoring atopic dermatitis: the SCORAD index, objective SCORAD and the three-item severity score. Br J Dermatol. 2007;157:645–648. doi: 10.1111/j.1365-2133.2007.08112.x. [DOI] [PubMed] [Google Scholar]
- 33.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1980;92:44–47. [Google Scholar]
- 34.Jin H, He R, Oyoshi M, Geha RS. Animal models of atopic dermatitis. J Invest Dermatol. 2009;129:31–40. doi: 10.1038/jid.2008.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moniaga CS, Jeong SK, Egawa G, Nakajima S, Hara-Chikuma M, Jeon JE, et al. Protease activity enhances production of thymic stromal lymphopoietin and basophil accumulation in flaky tail mice. Am J Pathol. 2013;182:841–851. doi: 10.1016/j.ajpath.2012.11.039. [DOI] [PubMed] [Google Scholar]
- 36.Almeida FF, Tenno M, Brzostek J, Li JL, Allies G, Hoeffel G, et al. Identification of a novel lymphoid population in the murine epidermis. Sci Rep. 2015;5:12554. doi: 10.1038/srep12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elias PM, Hatano Y, Williams ML. Basis for the barrier abnormality in atopic dermatitis: outside-inside-outside pathogenic mechanisms. J Allergy Clin Immunol. 2008;121:1337–1343. doi: 10.1016/j.jaci.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krishnan L, Gurnani K, Dicaire CJ, van Faassen H, Zafer A, Kirschning CJ, et al. Rapid clonal expansion and prolonged maintenance of memory CD8+ T cells of the effector (CD44highCD62Llow) and central (CD44highCD62Lhigh) phenotype by an archaeosome adjuvant independent of TLR2. J Immunol. 2007;178:2396–2406. doi: 10.4049/jimmunol.178.4.2396. [DOI] [PubMed] [Google Scholar]
- 39.van Kempen LC, van den Oord JJ, van Muijen GN, Weidle UH, Bloemers HP, Swart GW. Activated leukocyte cell adhesion molecule/CD166, a marker of tumor progression in primary malignant melanoma of the skin. Am J Pathol. 2000;156:769–774. doi: 10.1016/S0002-9440(10)64943-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.von Bauer R, Oikonomou D, Sulaj A, Mohammed S, Hotz-Wagenblatt A, Gröne HJ, et al. CD166/ALCAM mediates proinflammatory effects of S100B in delayed type hypersensitivity. J Immunol. 2013;191:369–377. doi: 10.4049/jimmunol.1201864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ibáñez A, Sarrias MR, Farnós M, Gimferrer I, Serra-Pagès C, Vives J, et al. Mitogen-activated protein kinase pathway activation by the CD6 lymphocyte surface receptor. J Immunol. 2006;177:1152–1159. doi: 10.4049/jimmunol.177.2.1152. [DOI] [PubMed] [Google Scholar]
- 42.Kim BE, Leung DY, Boguniewicz M, Howell MD. Loricrin and involucrin expression is down-regulated by Th2 cytokines through STAT-6. Clin Immunol. 2008;126:332–337. doi: 10.1016/j.clim.2007.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sehra S, Yao Y, Howell MD, Nguyen ET, Kansas GS, Leung DY, et al. IL-4 regulates skin homeostasis and the predisposition toward allergic skin inflammation. J Immunol. 2010;184:3186–3190. doi: 10.4049/jimmunol.0901860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elias PM, Wakefield JS. Mechanisms of abnormal lamellar body secretion and the dysfunctional skin barrier in patients with atopic dermatitis. J Allergy Clin Immunol. 2014;134:781–791.e1. doi: 10.1016/j.jaci.2014.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hönzke S, Wallmeyer L, Ostrowski A, Radbruch M, Mundhenk L, Schäfer-Korting M, et al. Influence of Th2 cytokines on the cornified envelope, tight junction proteins, and ß-defensins in filaggrin-deficient skin equivalents. J Invest Dermatol. 2016;136:631–639. doi: 10.1016/j.jid.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 46.Bughani U, Saha A, Kuriakose A, Nair R, Sadashivarao RB, Venkataraman R, et al. T cell activation and differentiation is modulated by a CD6 domain 1 antibody Itolizumab. PLoS ONE. 2017;12:e0180088. doi: 10.1371/journal.pone.0180088. [DOI] [PMC free article] [PubMed] [Google Scholar]