Abstract
Background
Recent research has suggested that increases in mortality among middle-aged US Whites are being driven by suicides and poisonings from alcohol and drug use. Increases in these ‘despair’ deaths have been argued to reflect a cohort-based epidemic of pain and distress among middle-aged US Whites.
Methods
We examine trends in all-cause and cause-specific mortality rates among younger and middle-aged US White men and women between 1980 and 2014, using official US mortality data. We estimate trends in cause-specific mortality from suicides, alcohol-related deaths, drug-related deaths, ‘metabolic diseases’ (i.e. deaths from heart diseases, diabetes, obesity and/or hypertension), and residual deaths from extrinsic causes (i.e. causes external to the body). We examine variation in mortality trends by gender, age and cause of death, and decompose trends into period- and cohort-based variation.
Results
Trends in middle-aged US White mortality vary considerably by cause and gender. The relative contribution to overall mortality rates from drug-related deaths has increased dramatically since the early 1990s, but the contributions from suicide and alcohol-related deaths have remained stable. Rising mortality from drug-related deaths exhibit strong period-based patterns. Declines in deaths from metabolic diseases have slowed for middle-aged White men and have stalled for middle-aged White women, and exhibit strong cohort-based patterns.
Conclusions
We find little empirical support for the pain- and distress-based explanations for rising mortality in the US White population. Instead, recent mortality increases among younger and middle-aged US White men and women have likely been shaped by the US opiate epidemic and an expanding obesogenic environment.
Keywords: USA, midlife mortality, obesogenic, opiates, despair deaths, mortality trends
Introduction
Reports of increasing mortality among young and middle-aged White Americans have alarmed researchers and have raised serious challenges for US health policy.1–8 Evidence suggests that mortality increases have been disproportionately driven by deaths from chronic liver disease, suicide and drug overdoses,1–3 which some suggest are ‘likely symptoms of the same underlying epidemic’.2 Specifically, mortality trends among middle-aged White Americans are thought to reflect rising distress, economic insecurities and chronic pain in this population.1–8 Distress- and pain-based narratives have also been covered widely in media outlets and have prompted discussions over the possible social problems and economic challenges shaping mortality risk in White America.9–13
In this study, we use official US mortality data to examine cause-specific mortality trends among younger-aged (25–34 years) and middle-aged (35–54 years) US White men and women between 1980 and 2014. We examine trends in White men’s and women’s mortality separately, by the specific causes of death said to be most responsible for rising mortality among middle-aged White Americans: suicides, alcohol-related deaths and drug-related deaths.1–3 We also examine recent trends in mortality rates from ‘metabolic diseases’ (i.e. deaths from obesity, heart disease, diabetes and/or hypertension), as some researchers hypothesize that an expanding obesogenic environment in the USA might elevate mortality risk from these causes of death.14,15 Finally, we analyse mortality trends in residual deaths from extrinsic causes, with particular attention to infectious diseases and other HIV-related deaths.16 Results from our analyses do not support the contention that recent trends in US White mortality have been driven by a ‘lost generation’ suffering an ‘epidemic of pain’ or rising distress.2
Methods
Counts of death among US White women and men aged 25–54 for years 1980–2014 were obtained from the National Center for Health Statistics (NCHS) Mortality Multiple Cause-of-Death public use records.17 Annual estimates of mid-year population for US White women and men aged 25–54 for years 1990–14 were obtained from the Centers for Disease Control and Prevention (CDC) Bridged-Race Population Estimates, 1990–2014.18 Annual estimates of mid-year population for US White women and men aged 25–54 for years 1980–89 were obtained from the US Census Bureau’s Vintage Quarterly Population Estimates.19 We combined these data sources to calculate annual age-specific mortality rates for US White men and women aged 25–54 for years 1980–2014.
We examined annual trends in White men’s and women’s all-cause age-specific mortality rates and separately by suicides, alcohol-related deaths, drug-related deaths, metabolic diseases and residual deaths from extrinsic causes (see Supplementary data for cause-of-death coding, available at IJE online). We estimated single-year age-specific mortality rates by fitting Poisson rate models separately to three age groups (25–34, 35–44, 45–54) and separately for men and women (see Supplementary material for a detailed description of our analytic approach). Additionally, we fitted age-period-cohort (APC) models using the intrinsic estimator (IE) to White men’s and women’s mortality rates separately by deaths from suicides, alcohol use, drug use and metabolic diseases (see Supplementary material for a broader discussion about the use of APC methods). We used APC models to examine if cohort-based variation in the extrinsic causes of death exhibit generational patterns consistent with Case and Deaton’s ‘lost generation’ hypothesis.2 This hypothesis posits that cohorts of middle-aged Whites are experiencing greater mortality increases from suicides, alcohol use and drug-related deaths than are other cohorts. Additionally, we fitted APC models to examine if the period-based variation in drug-related mortality coincides with the timing of the Food and Drug Administration (FDA) approval of oxycodone-based painkillers such as Oxycontin, which was first introduced in 1996 and aggressively marketed thereafter.20–27 Finally, we also explored whether cohort-based variation in metabolic disease mortality is consistent with the hypothesis that duration of exposure to the US obesogenic environment has elevated metabolic disease mortality risk for recent US birth cohorts.15,16
Results
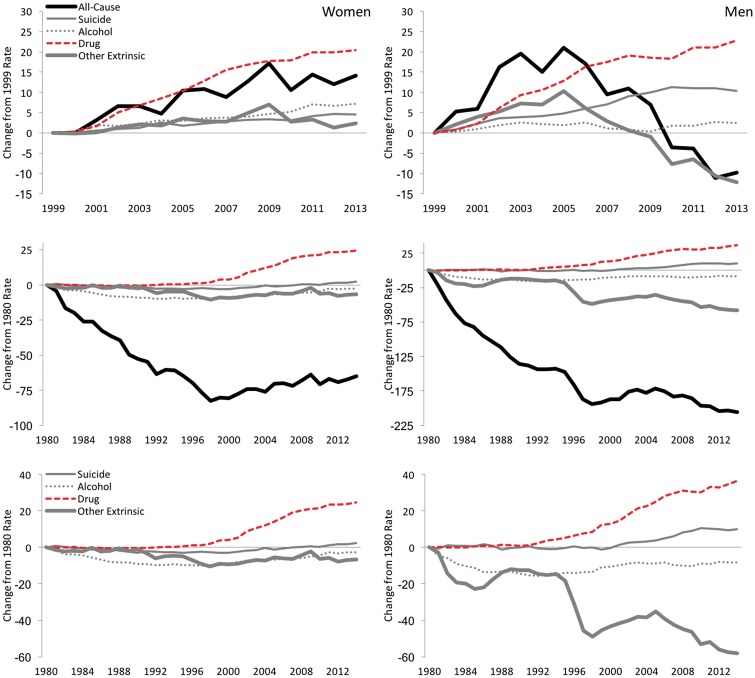
In the top row of Figure 1, we plot absolute changes in age-standardized all-cause and cause-specific mortality rates among US White women (left) and White men (right) aged 45–54 between 1999 and 2013. These graphs are provided to replicate Case and Deaton’s 2015 analyses that focused on recent trends in middle-aged White mortality (1999–2013), and which emphasized rising mortality risk from extrinsic causes of death related to health behaviours (e.g. heavy alcohol consumption).2 We separate trends by gender to highlight the fact that increases in all-cause mortality during this time occurred only among White women, with increases among White men observed only through 2005 followed by rapid decreases.28 We also include trends from other extrinsic causes of death not highlighted by Case and Deaton, to observe how trends in these residual causes of death tracked with trends in all-cause mortality.
Figure 1.
Absolute changes in US White women’s (left) and men’s (right) age-standardized mortality rates, ages 45–54. Top row: 1999–2013. Middle and bottom rows: 1980–2014. Mortality rates are per 100 000 person-years.
In the second row of Figure 1, we plot absolute changes in mortality rates among middle-aged White men and women between 1980 and 2014, to more accurately observe the time at which mortality rates from these causes of death first increased. Middle-aged US White men’s and women’s all-cause mortality rates dropped considerably across the 1980s and 1990s, but mortality reversals noted by Case and Deaton2 can be observed to begin around 1998. What we do not observe, however, in either White women’s mortality or White men’s mortality, are sizeable increases in mortality from either suicides or alcohol-related deaths during this time. These trends are more easily observed in the third row of Figure 1, in which we re-plot the mortality trends without all-cause mortality in order to more clearly see the cause-specific mortality trends on a finer scale. Here, we see that rising all-cause mortality among middle-aged White men between 1998 and 2005 cannot be attributed to changes in suicides, as suicide rates did not increase substantially until the late 2000s, when White men’s all-cause mortality rates were decreasing. Nor can the increases in White men’s mortality be attributed to alcohol abuse, as we observe no substantive increases in White men’s alcohol-related mortality at any time. The increases in middle-aged White men’s all-cause mortality appear to correspond most with the striking increases in drug-related deaths and the variable trend in residual deaths from extrinsic causes. The latter partly reflect trends in HIV/AIDS-related mortality, as we observe a pronounced drop in residual deaths in the mid-1990s that corresponds with the introduction and widespread adoption of antiretroviral treatments (ART) in 199629,30 (see Supplementary material for trend analyses of HIV/AIDS-related deaths among middle-aged White men). Overall, we observe dramatic mortality decreases in residual deaths between 1996 and 1998, followed by large increases between 1998 and 2005, and then steady decreases thereafter. We also see that increases in mortality from drug-related deaths are much larger than the increases suggested by trend analyses limited to years 1999–2013. Specifically, the absolute change in drug-related mortality rates for White men aged 45–54 between 1999 and 2013 is about 22.8 deaths per 100 000, whereas the absolute change between 1980 and 2014 is about 36.5 deaths per 100 000. The results show that increases in White men’s drug-related mortality began in the early 1990s, with an accelerated increase beginning in the late 1990s.
Among middle-aged White women we observe trends similar to those among White men, save the dramatic variation in residual deaths from extrinsic causes. Specifically, we observe rapid increases in drug-related mortality that begin in the late 1990s, whereas we observe only relatively minor mortality increases from both suicide and alcohol use. Although mortality rates rise slightly from these causes of death between the late 1990s and the 2010s, mortality increases in residual deaths from extrinsic causes were comparable to increases in both suicide and alcohol-related deaths.
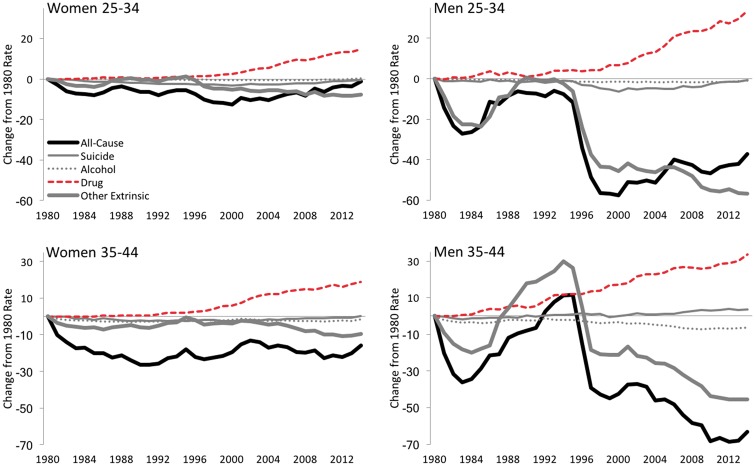
In Figure 2, we plot absolute changes in US White men’s and women’s mortality rates between 1980 and 2014 for ages 25–34 and 35–44. We provide these results to contrast White men’s and women’s mortality trends in these age groups with those trends observed among the middle-aged group (ages 45–54 years). Four findings are especially noteworthy. First, we observe mortality increases from drug-related deaths among these younger age groups, which are very similar to the increases observed among White men and women aged 45–54. Second, mortalities from suicide and alcohol use exhibit no significant trends, but for a small rise in suicide among White men aged 35–44 corresponding to the timing of the great recession (i.e. 2007–09) and a steady decline in alcohol-related deaths among men aged 35–44. Third, all-cause mortality rates among young adult White men and women (ages 25–34) have been increasing since 1999 and appear to be largely driven by rising mortality from drug-related deaths. And fourth, deaths from residual extrinsic causes appear to be the overwhelming driver of recent trends in all-cause mortality rates among both White men and women aged 35–44.
Figure 2.
Absolute Changes in US White women’s (left) and men’s (right) age-standardized mortality rates, ages 35–44 (bottom) and 25–34 (top), 1980–2014. Mortality rates are per 100 000 person-years.
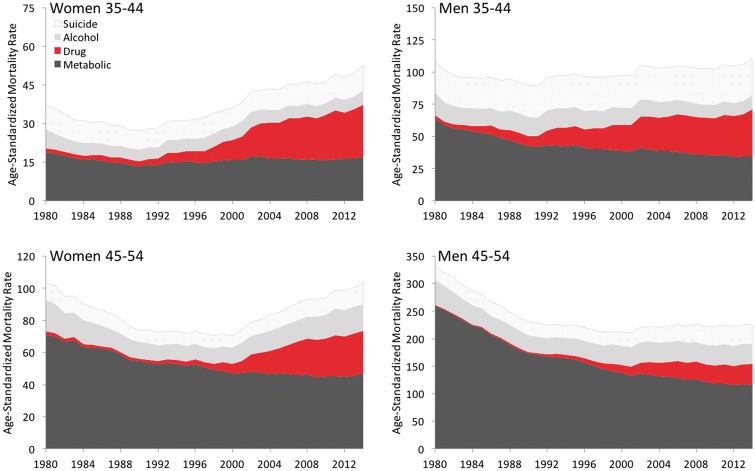
In Figure 3, we plot the combined age-specific mortality rates from drug-related deaths, alcohol-related deaths, suicide and metabolic diseases among middle-aged White men and women in order to observe trends in these causes’ contributions to overall mortality levels. Here, we observe no substantive increases in the relative mortality contribution from either suicide or alcohol use among middle-aged US White men or women. In contrast, we observe large increases in the relative mortality contributions from drug-related deaths for both White men and White women in both age groups. Finally, we observe that the relative mortality contribution from metabolic diseases has dropped considerably for White men and women, but the pace of the reductions in metabolic disease mortality has slowed for middle-aged White men and has stalled for middle-aged White women.
Figure 3.
Combined mortality rates for US White women (left) and men (right) aged 45–54 (bottom) and 35–44 (top), from drug-related deaths, alcohol-related deaths, suicides and metabolic diseases, 1980–2014. Mortality rates are per 100 000 person-years.
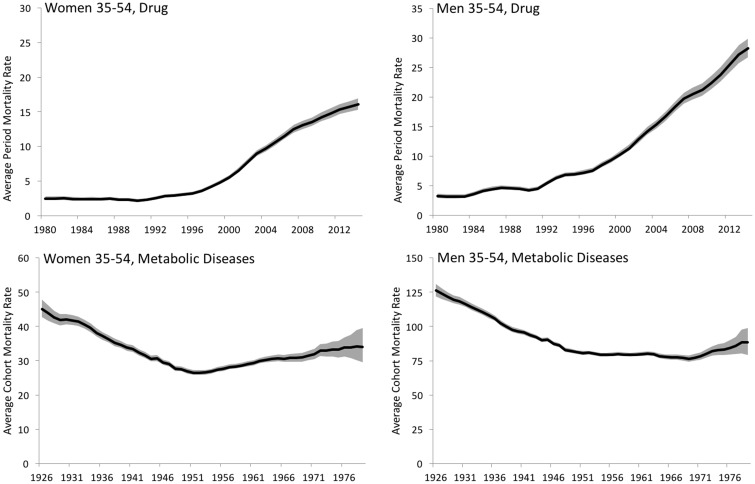
In the top row of Figure 4, we graph 3-year moving average mortality rates from drug-related deaths among White men and women aged 35–54 between 1980 and 2014. The mortality rates are estimated from age-period-cohort (APC) models and are plotted at the mean age (44.1 for women and 44.0 for men) and mean birth cohort (1954.3 for women and 1954.5 for men) in order to show only period-based variation in drug-related mortality. Results indicate striking period-based increases in drug-related mortality for both White men and women. We observe increases among White men to begin in the early 1990s and to rapidly increase in the late 1990s. For White women, the period-based increases in drug-related deaths are observed to begin in the late 1990s, but the increases are smaller than those for White men. In contrast, cohort-based variation in drug-related mortality is estimated to be significantly smaller than period-based variation among White men, and is nearly absent among White women (results available upon request).
Figure 4.
Period-based variation in drug-related mortality and cohort-based variation in metabolic disease mortality among White women and men (right), ages 35–54, 1980–2014. Estimates are 3-year moving averages, and gray areas indicate upper and lower bounds of the 95% confidence interval. Estimates are mortality rates per 100 000 person-years.
In the bottom row of Figure 4, we graph 3-year moving average mortality rates from metabolic diseases among White men and women aged 35–54 across cohorts born 1926 through 1979. The mortality rates are estimated from APC models and are plotted at the mean ages and mean time periods (1998.4 for women and 1998.5 for men) in order to show only cohort-based variation in metabolic disease mortality. Results indicate strong cohort-based decreases in metabolic disease mortality for US White men and women born between the 1920s and 1950s. These findings are consistent with existing evidence suggesting large cohort decreases in US heart disease mortality for US adults born between the late 19th century and mid 20th century.31,32 Beginning with US White men and women born in the 1950s, however, we observe steady cohort-based increases in metabolic disease mortality risk. These cohort-based increases are driving the slowing declines in overall metabolic disease mortality among US White men and women, as estimates from the APC models suggest period-based reductions in metabolic disease mortality occurred during the 1990s, 2000s and 2010s (results available upon request).
Discussion
Recent analyses of US middle-aged White mortality have reported rising mortality rates that are largely attributed to increases in deaths from suicides, chronic liver diseases and drug use.1–5 These results imply that an epidemic of pain and distress might be driving recent mortality trends among middle-aged White Americans.2 However, these results were derived from analyses that combined men’s and women’s mortality rates and pooled different causes of death. When we analyse trends in cause-specific mortality rates for US White men and women separately, we find little evidence to support the pain- and distress-based narratives forwarded by Case and Deaton and popularized in the media.2,9–13 Instead, our analyses contribute four important conclusions that are relevant to both public health policy and future mortality research.
First, we find sizeable gender differences in mortality trends among the US White population for both all-cause and cause-specific mortality. As others have noted, middle-aged White men and women experienced very different trends in all-cause mortality during the 2000s and 2010s.28,33 These differences complicate previous research findings and undermine existing explanations, since we would expect to observe similar trends among White men and women had the all-cause mortality increases been driven by the ‘same underlying epidemic’.2 Importantly, we find gender differences in mortality trends by extrinsic causes of death as well, which suggest significant gender differences in the phenomena behind the cause-specific mortality trends. For instance, deaths from residual extrinsic causes greatly affected recent mortality trends among middle-aged White men (most likely from HIV/AIDS-related deaths), whereas deaths from these residual causes only slightly influenced recent mortality trends among middle-aged White women. Although the increases in White men’s and women’s mortality from drug-related deaths are similar in many respects, we observe gender differences in their onset, levels and ages most affected. With these gender differences in mind, health policy makers and mortality researchers must seriously consider the gender processes associated with mortality risk, to understand and address recent trends in US mortality.
Second, although others have combined drug-related deaths, suicides and alcohol-related deaths, we observe very different mortality trends for these specific causes. For instance, among younger and middle-aged White men, drug-related deaths began to increase in the 1990s, whereas substantive increases in suicide rates did not occur until the late 2000s, and no substantive increases in alcohol-related mortality were observed. Further, the relative contributions to overall mortality rates from drug-related deaths increased remarkably across the 1990s, 2000s and into the 2010s, whereas the relative contributions from both suicide and alcohol-related deaths remained stable across these times. As such, recent US mortality trends from these three causes of death are quite different from one another, suggesting that the trends likely do not share the same underlying cause(s).
Third, the rising mortality from drug-related deaths among US White men and women is not confined to mid-life ages. Consistent with others’ reports, we observe increasing mortality from drug use among US White men and women in their 20 s, 30 s, 40 s and 50 s.21,22,25,27 Moreover, the mortality increases from drug-related deaths among White men and women in their 20 s and 30 s are driving increases in overall mortality rates at these ages. As such, we find strong evidence suggesting that increases in US drug-related mortality reflect a period-based epidemic, affecting multiple cohorts of Americans during recent years. The onset and pace of US mortality increases from drug-related deaths are inconsistent with the idea that the increases reflect rising incidence of pain among middle-aged White Americans.2 Instead, rising mortality rates from drug-related deaths appear to coincide with the rising availability, over-prescription and misuse of opioid-based painkillers (e.g. Oxycontin) among US medical practitioners, coupled with related increases in heroin use.20–27
Fourth, we find that reductions in mortality related to metabolic diseases have slowed among middle-aged White men and have stalled among middle-aged White women. Moreover, the mortality trends exhibit very strong birth cohort patterns, whereby the mortality risks from metabolic diseases are higher for more recently born US Whites. These findings are consistent with previous researchers’ warnings that US mortality levels could soon be affected by an expanding US obesogenic environment.14 Indeed, we find that without these cohort-based increases in metabolic disease mortality risk, the recent increases in middle-aged US White women’s overall mortality rates likely would not have occurred. Recognizing that metabolic disease risk is likely increasing across birth cohorts should be a high-priority for US public health policy.
To conclude, we acknowledge that recent reports of rising mortality among US White men and women have alarmed researchers and pose serious challenges to US health policy.1–4 However, existing research and media reports have pushed narratives that explain the trends in terms of rising incidence of chronic pain, increasing despair and economic deterioration in White America.9–13 Such narratives have been fuelled by findings from research that analysed US White mortality rates in a select age group (45–54 years) during a narrow period of time (1999–2013), and that combined men’s and women’s deaths from vastly different causes.2 The analyses produced erroneous results that suggested mortality rates have increased for both middle-aged US White men and women, and that three causes of deaths–suicide, alcohol use, and drug use–were responsible for the trend. We find little empirical support for these narratives.
We do not doubt that times of economic insecurity can have severe consequences for a population’s health–indeed, White men’s suicide rates track closely with the timing of economic recessions–nor do we doubt that pain and distress can pose serious health problems. However, taken together, our findings suggest that it is unlikely that recent trends in US White men’s and women’s mortality rates have been driven by an epidemic of pain and rising distress. Instead, the recent trends appear to be strongly associated with three other US epidemics: (i) the opiate epidemic has driven drug-related mortality among both younger- and middle-aged US men and women; (ii) the ‘obesity epidemic’ likely has increasingly shaped metabolic disease mortality risk among recent cohorts of US White men and women; and (iii) lagged effects of the HIV/AIDS epidemic continued to shape middle-aged White men’s extrinsic mortality from the 1990s through the 2000s. The recent trends in US mortality suggest an increasing need to combat the health consequences of both an expanding obesogenic environment in the USA and a rampant opiate epidemic. While some recent developments are encouraging, such as the CDC’s recently published guidelines for prescribing opiates,34 more action is likely needed to reverse trends in opiate-related deaths and rising metabolic disease risk in the US population.
Supplementary Data
Supplementary data are available at IJE online
Conflict of interest: None declared.
Key Messages
Recent cause-specific mortality trends among US White men and women are inconsistent with existing explanations for rising mortality among middle-aged White Americans.
Younger- and middle-aged US White mortality has likely been shaped by the US opiate epidemic and an expanding obesogenic environment.
Trends in younger- and middle-aged US White men’s mortality from extrinsic causes of death have also been shaped by the US HIV/AIDS epidemic.
Supplementary Material
References
- 1. Kochanek KD, Arias E, Bastian BA. The Effect of Changes in Selected Age-specific Causes of Death on Non-Hispanic White Life Expectancy Between 2000 and 2014. Atlanta, GA: National Center for Health Statistics, 2016. [PubMed] [Google Scholar]
- 2. Case A, Deaton A. Rising morbidity and mortality in midlife among White non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015;112:15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Meara E, Skinner J. Losing ground at midlife in America. Proc Natl Acad Sci U S A 2015;11249:15006–07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Center for Health Statistics. Quarterly Provisional Estimates for Selected Causes of Death: United States, 2014–Quarter 4, 2015. National Vital Statistics System, Vital Statistics Rapid Release Program. Atlanta, GA: National Center for Health Statistics, 2016. [Google Scholar]
- 5. Arias E. Changes in Life Expectancy by Race and Hispanic Origin in the United States, 2013–2014. NCHS data brief, no 244. Hyattsville, MD: National Center for Health Statistics, 2016. [PubMed] [Google Scholar]
- 6. Woolf SH, Aron L. . US Health in International Perspective:: Shorter Lives, Poorer Health. Washington, DC: National Academies Press, 2013. [PubMed] [Google Scholar]
- 7. Montez JK, Zajacova A. Why is life expectancy declining among low-educated women in the United States? Am J Public Health 2014;104:e5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff 2012;31:1803–13. [DOI] [PubMed] [Google Scholar]
- 9. Krugman P. Despair, American style. New York Times 2015, Nov 9;Sect A:23. [Google Scholar]
- 10. Cassidy J. Why did the death rates rise among middle-aged White Americans? New Yorker 2015, Nov 9. [Google Scholar]
- 11. Douthat R. The dying of the Whites. New York Times 2015, Nov 9;Sect SR:11. [Google Scholar]
- 12. Tavernise S. First rise in US death rates in years surprises experts. New York Times 2016, June 1;Sect A:10. [Google Scholar]
- 13. Saslow E. ‘We don’t know why it came to this.’ As White women between 25 and 55 die at spiking rates, a close look at one tragedy. Washington Post 2016, April 8;Part 1. [Google Scholar]
- 14. Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J. A potential decline in life expectancy in the United States in the 21st century . N Engl J Med 2005; 352:1138–45. [DOI] [PubMed] [Google Scholar]
- 15. Reither EN, Olshansky SJ, Yang Y. New forecasting methodology indicates more disease and earlier mortality ahead for today’s younger Americans. Health Aff 2011;30:1562–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Carnes BA, Holden LR, Olshansky SJ, Witten MT, Siegel JS. Mortality partitions and their relevance to research on senescence. Biogerontology 2006;7:183–98. [DOI] [PubMed] [Google Scholar]
- 17. NCHS. Mortality Multiple Cause-of-death. Atlanta, GA: National Vital Statistics System, National Center for Health Statistics, 1968. [Google Scholar]
- 18. Bridged-Race Population Estimates, 1990–2014. Atlanta, GA: CDC Wonder, US Department of Health & Human Services, 2014. [Google Scholar]
- 19. Quarterly Population Estimates, 1980 to 1990. Suitland, MD: United States Census Bureau, 1990. [Google Scholar]
- 20. Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy. Am J Public Health 2009;99:221–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Calcaterra S, Glanz J, Binswanger IA. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug Alcohol Depend 2013;131:263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hedegaard H, Chen LH, Warner M. Drug-poisoning Deaths Involving Heroin: United States, 2000–2013. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2015. [Google Scholar]
- 23. Quinones S. Dreamland: The True Tale of America’s Opiate Epidemic. New York, NY: Bloomsbury Press, 2015. [Google Scholar]
- 24. Rudd RA, Paulozzi LJ, Bauer MJ, et al. Increases in heroin overdose deaths—28 States, 2010 to 2012. MMWR Morb Mortal Wkly Rep 2014;63:849–54. [PMC free article] [PubMed] [Google Scholar]
- 25. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. Am J Transplant 2016;16:1323–27. [DOI] [PubMed] [Google Scholar]
- 26. Manchikanti L, Helm S II, Fellows B, et al. Opioid epidemic in the United States. Pain Physician 2012;15(Suppl 3):ES9–38. [PubMed] [Google Scholar]
- 27. Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry 2014;71:821–26. [DOI] [PubMed] [Google Scholar]
- 28. Gelman A, Auerbach J. Age-aggregation bias in mortality trends. Proc Natl Acad Sci U S A 2016;113:E816–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boyd MA. Improvements in antiretroviral therapy outcomes over calendar time. Curr Opin HIV AIDS 2009;4:194–99. [DOI] [PubMed] [Google Scholar]
- 30. Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet 2008;372:293–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Masters RK, Hummer RA, Powers DA, Beck A, Lin SF, Finch BK. Long-term trends in adult mortality for US Blacks and Whites: An examination of period-and cohort-based changes. Demography 2014;51:2047–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yang Y. Trends in US adult chronic disease mortality, 1960–1999: Age, period, and cohort variations. Demography 2008;45:387–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Masters RK, Tilstra AM, Simon DH. Mortality from suicide, chronic liver disease, and drug poisonings among middle-aged US men and women, 1980–2013. Biodemogr Soc Biol 2017;63:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 2016;315:1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.