Abstract
A case of multiple myeloma with testicular involvement is rare. We report a 72-year-old male with testicular infiltration as extramedullary disease of IgD λ-type multiple myeloma. The patient received systemic treatment, which included high orchiectomy, anticancer chemotherapy, and radiation therapy for bone metastasis. Eight months after the initial diagnosis, he remains alive.
The testis is a rare location for extramedullary disease of multiple myeloma. Testicular involvement of multiple myeloma indicates a poor prognosis. The particular treatment strategy for extramedullary disease in multiple myeloma remains unclear. Testicular involvement of multiple myeloma is reviewed and discussed in this paper.
Introduction
Multiple myeloma is a cancer of plasma cells. Testicular involvement in the course of multiple myeloma is rare and indicates a poor prognosis. In this paper, we report a patient with a case of testicular infiltration of multiple myeloma. The testis is a rare site for the localization of multiple myeloma. The particular treatment strategy for extramedullary disease in multiple myeloma remains unclear. Therefore, it is important to describe case reports of multiple myeloma with testicular involvement.
Presentation of the case
A 72-year-old Japanese man experienced chest pain and was referred to the department of internal medicine at our hospital in September 2018. His hemoglobin level was 10.1 g/dL (normal, 14.0–18.0 g/dL), and calcium level and renal function were normal. His total protein was 8.8 g/dL (normal, 6.1–8.0 g/dL), albumin was 3.4 g/dL (normal, 3.7–5.2 g/dL), and β2-microgloblin was 4.7 mg/L (normal, 1.0–1.9 mg/L). His serum immunoglobulin D (IgD) level was 8.810 mg/dL (normal, <9.0 mg/dL). The levels of the other immunoglobulin classes were as follows: IgG, <398.1 mg/dL (normal, 870–1700 mg/dL); IgA, <15.8 mg/dL (normal, 110–410 mg/dL); and IgM, 9.0 mg/dL (normal, 33–190 mg/dL). Serum protein electrophoresis showed M-protein in the gamma-zone. Immunoelectrophoresis revealed IgD λ-type M-protein and Bence Jones protein λ-type M-protein in the serum, and Bence Jones protein λ-type M-protein in the urine. Bone marrow aspiration showed 60% plasma cell infiltration. Computed tomography showed osteolytic lesions in multiple ribs and vertebrae. Therefore, he was diagnosed as having IgD λ-type multiple myeloma. Bortezomib and Dexamethasone were commenced for treatment.
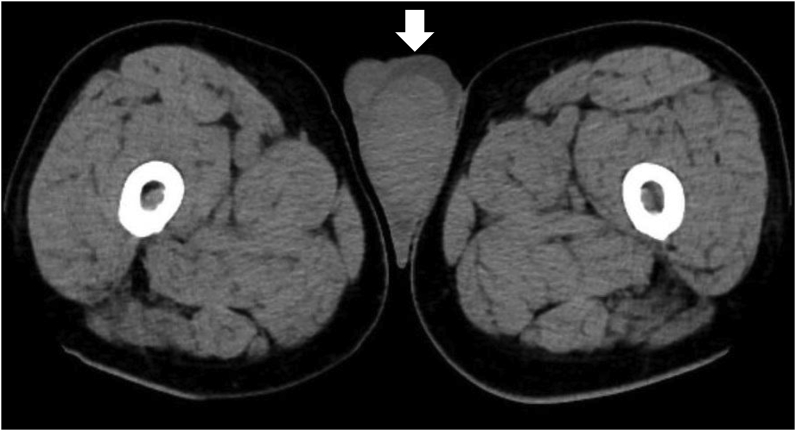
At the initial diagnosis, he also had unpainful left testicular swelling. He was referred to our department of urology. The levels of germ cell tumor markers (e.g., alpha-fetoprotein, beta-human chorionic gonadotropin, and lactate dehydrogenase) were normal. Ultrasonography examination showed an enlarged left testis with low echoic areas. Computer tomography image demonstrated an enlarged left testis and hydrocele (Fig. 1). He underwent left high orchiectomy in November 2018.
Fig. 1.
Computer tomography image demonstrated an enlarged left testis and hydrocele (arrow).
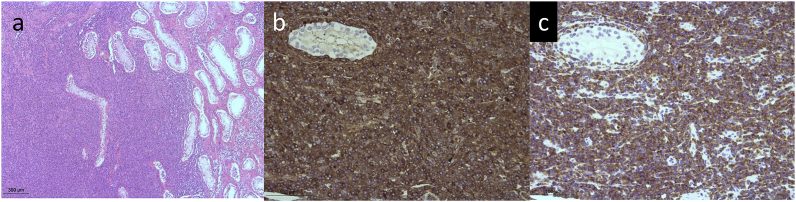
The macroscopic specimen was a grossly enlarged testis (65 mm × 50 mm × 50 mm) in which white nodular tumor components had replaced most of the normal testicular tissue (Fig. 2). Pathological specimen revealed myeloma cell infiltration in the testis and spermatic cord (Fig. 3a). Immunohistochemistry staining showed the specimen was positive for IgD (Fig. 3b) and for light chain λ (Fig. 3c). Therefore, he was diagnosed has having IgD λ-type myeloma cell infiltration in the left testis.
Fig. 2.
The macroscopic specimen is a grossly enlarged testis (65 mm × 50 mm × 50 mm). White nodular tumor components have replaced the normal testicular tissue.
Fig. 3.
Histopathological analyses. (a) The pathological specimen shows myeloma cell infiltration in the testis (hematoxylin and eosin stain). Immunohistochemistry staining is positive for (b) IgD and (c) light chain λ.
He had flaccid paraplegia because of metastases to thoracic vertebrae T5, T8, and T9. He underwent radiation therapy to these metastases. He was administered four cycles of Bortezomib and Dexamethasone, until he experienced a Bortezomib-induced peripheral nerve disorder. Melphalan and Prednisone were initiated in March 2019 for the second line anticancer chemotherapy. Eight months after the initial diagnosis, he remains alive.
Discussion
Multiple myeloma is the second most common hematologic malignancy,1 and represents 10%–15% of all hematological neoplasms.2 Multiple myeloma is the malignant production and proliferation of the monoclonal body of plasma cells. Neoplastic plasma cells multiply in the bone marrow. Extramedullary disease in multiple myeloma is a plasma cell neoplasm that occurs outside of the bone marrow. The most common sites of extramedullary disease in multiple myeloma are parenchymous organs such as the liver and kidneys1, however, testicular involvement in the course of multiple myeloma is rare.3,4
At the initial diagnosis, our patient had testicular involvement as extramedullary disease in multiple myeloma. However, there was secondary testicular involvement in multiple myeloma at the time of the multiple myeloma relapse. Wei et al.5 reported a patient who had a late relapse of multiple myeloma with testicular plasmacytoma at 3 years after autologous hematopoietic stem-cell transplantation for a previous diagnosis of multiple myeloma. Rosenberg et al.3 reported their experience with a case of testicular plasmacytoma without evidence of a relapse of multiple myeloma of the bone marrow in a patient who had been diagnosed with multiple myeloma 9 years earlier.
The testes provide a sanctuary site for hematologic malignancy because of the testicular blood barrier. Therefore, hematologic malignant cells may remain in the testes, even after systemic anticancer chemotherapy for a previous hematologic malignancy such as multiple myeloma. Urologist and hematologists or oncologists should pay attention to physical examination findings such as testicular swelling and nodules when following up patients with a history of hematologic malignancy. High orchiectomy is needed for surgical therapy and a pathologic diagnosis.
Sevcikova et al.1 found longer overall survival in patients with multiple myeloma without extramedullary disease than in patients with extramedullary disease. The prognosis of patients with testicular involvement of multiple myeloma is believed to be poor. However, in our investigations, we found no published prospective studies of a specific treatment for extramedullary disease with multiple myeloma.
Proteasome inhibitor-based regimens (e.g., Bortezomib therapy) have recently been used to treat testicular involvement of multiple myeloma after high orchiectomy.3,4 Reporting cases of testicular involvement of multiple myeloma is essential for understanding the condition and for treating multiple myeloma with extramedullary disease with testicular involvement.
Conclusion
Testicular involvement as extramedullary disease of multiple myeloma is rare and indicates a poor prognosis. The testes provide a sanctuary site for hematologic malignancy because of the testicular blood barrier. Urologists have to consider conducting a physical examination of the testes when following up with patients who have a history of hematologic malignancies such as multiple myeloma.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
No funding was provided for this case report.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.100971.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Savcikova S., Minarik J., Stork M., Jelinek T., Pour L., Hajek R. Extramedullary disease in multiple myeloma — controversies and future directions. Blood Rev. 2019 doi: 10.1016/j.blre.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Gerecke C., Fuhrmann S., Strifler S., Schmidt-Hieber M., Einsele H., Knop S. The diagnosis and treatment of multiple myeloma. Dtsch Arzteblatt Int. 2016 doi: 10.3238/arztebl.2016.0470. https://doi.10.3238/arztebl.2016.0470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenberg S., Shapur N., Gofrit O., Or R. Plasmacytoma of the testis in a patient with previous multiple myeloma: is the testis a santuary site? J Clin Oncol. 2010 doi: 10.1200/JCO.2009.27.6519. https://doi.10.1200/JCO.2009.27.6519 [DOI] [PubMed] [Google Scholar]
- 4.Hwang Y.Y., Chim C.S., Shek T.W. Multiple myeloma with testicular involvement. J Clin Oncol. 2008 doi: 10.1200/JCO.2007.15.1316. https://doi.10.1200/JCO.2007.15.1316 [DOI] [PubMed] [Google Scholar]
- 5.Wei Z.L., Pac C.M., Jiang Y.Z., Yan-Dai, Huanguang L.Q., Huang D.P. Late relapse of multiple myeloma with testicular plasmacytoma after autologous hematopoietic stem cell transplantation: a case report and review of the literature. Ann Clin Lab Sci. 2018;48:120–125. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.