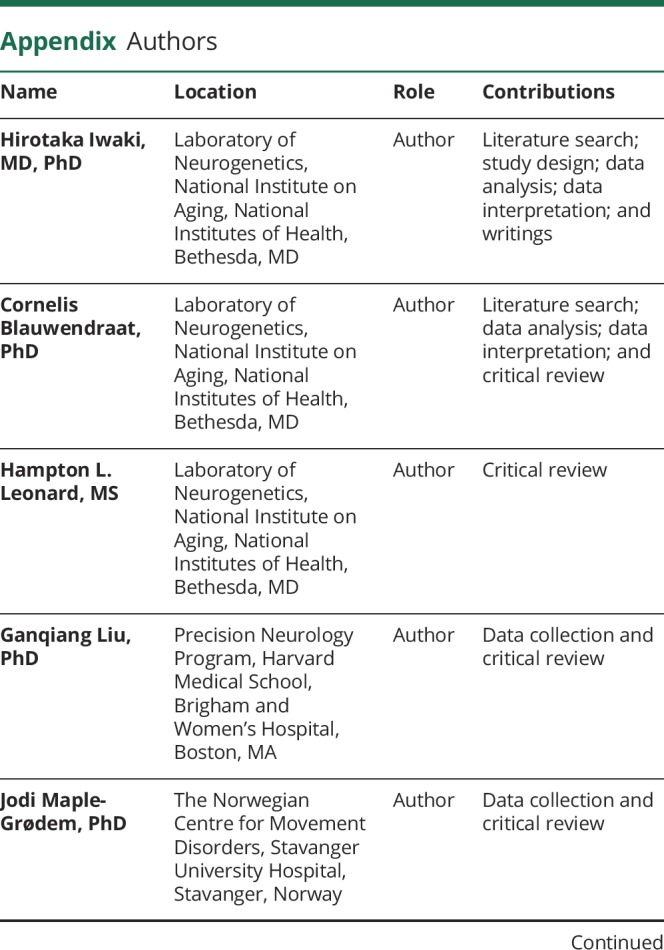
Hirotaka Iwaki
Hirotaka Iwaki, MD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Cornelis Blauwendraat
Cornelis Blauwendraat, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Hampton L Leonard
Hampton L Leonard, MS
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Ganqiang Liu
Ganqiang Liu, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Jodi Maple-Grødem
Jodi Maple-Grødem, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
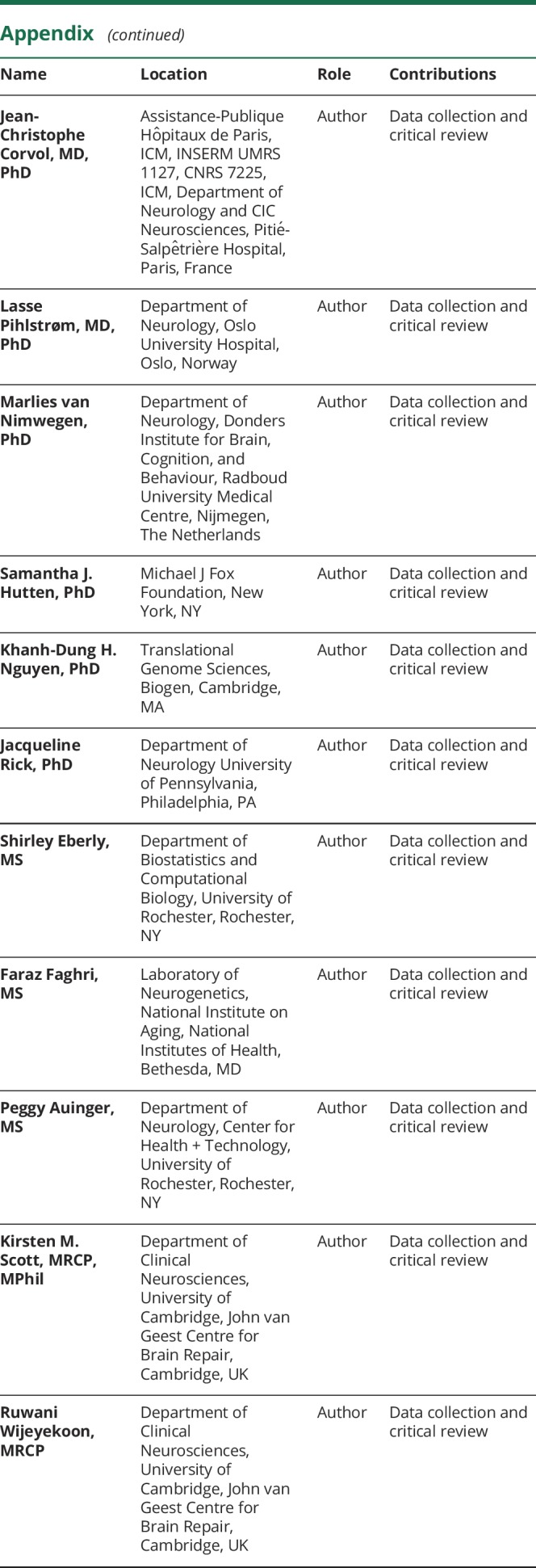
Jean-Christophe Corvol
Jean-Christophe Corvol, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Lasse Pihlstrøm
Lasse Pihlstrøm, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Marlies van Nimwegen
Marlies van Nimwegen, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Samantha J Hutten
Samantha J Hutten, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Khanh-Dung H Nguyen
Khanh-Dung H Nguyen, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Jacqueline Rick
Jacqueline Rick, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Shirley Eberly
Shirley Eberly, MS
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Faraz Faghri
Faraz Faghri, MS
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Peggy Auinger
Peggy Auinger, MS
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Kirsten M Scott
Kirsten M Scott, MRCP, MPhil
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Ruwani Wijeyekoon
Ruwani Wijeyekoon, MRCP
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
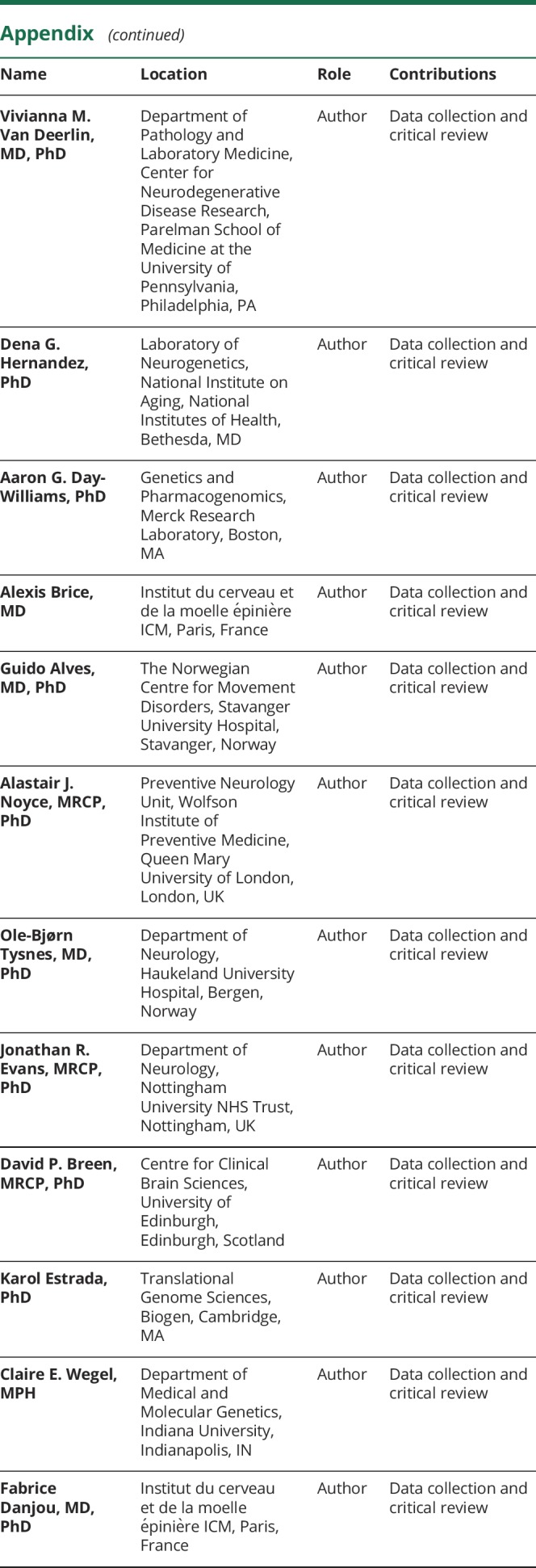
Vivianna M Van Deerlin
Vivianna M Van Deerlin, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Dena G Hernandez
Dena G Hernandez, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Aaron G Day-Williams
Aaron G Day-Williams, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Alexis Brice
Alexis Brice, MD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Guido Alves
Guido Alves, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
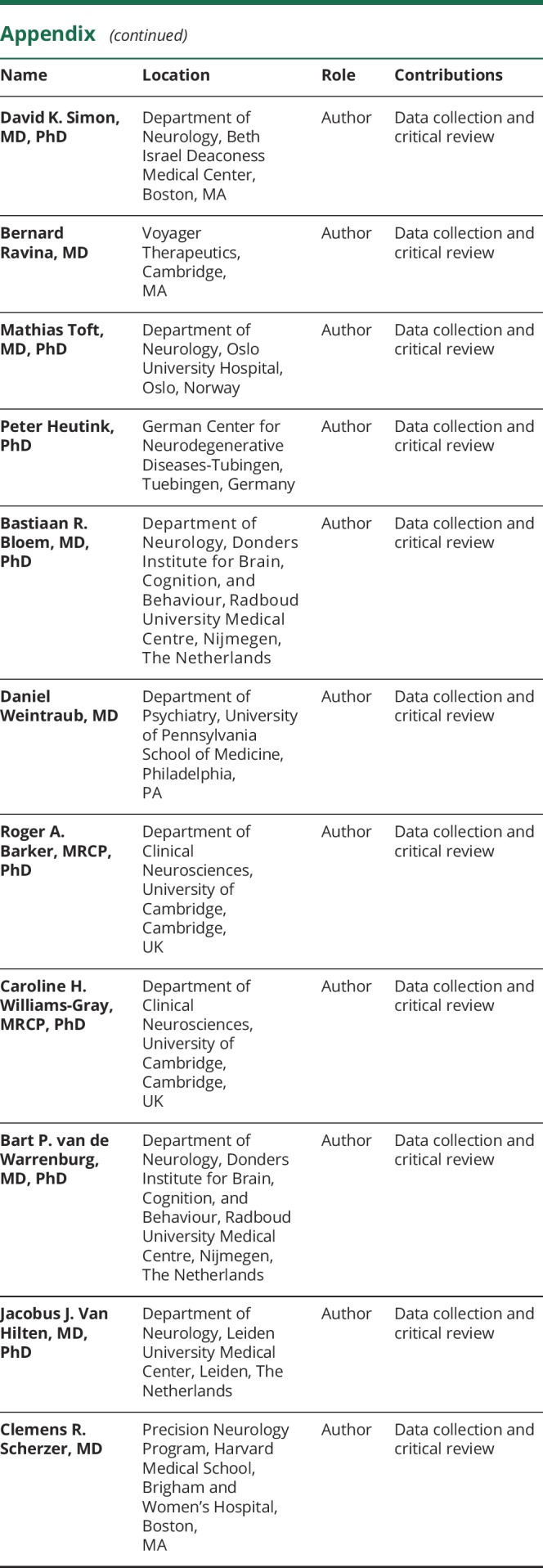
Alastair J Noyce
Alastair J Noyce, MRCP, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Ole-Bjørn Tysnes
Ole-Bjørn Tysnes, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Jonathan R Evans
Jonathan R Evans, MRCP, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
David P Breen
David P Breen, MRCP, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Karol Estrada
Karol Estrada, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Claire E Wegel
Claire E Wegel, MPH
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Fabrice Danjou
Fabrice Danjou, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
David K Simon
David K Simon, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Bernard Ravina
Bernard Ravina, MD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Mathias Toft
Mathias Toft, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Peter Heutink
Peter Heutink, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Bastiaan R Bloem
Bastiaan R Bloem, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Daniel Weintraub
Daniel Weintraub, MD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Roger A Barker
Roger A Barker, MRCP, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Caroline H Williams-Gray
Caroline H Williams-Gray, MRCP, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Bart P van de Warrenburg
Bart P van de Warrenburg, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Jacobus J Van Hilten
Jacobus J Van Hilten, MD, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Clemens R Scherzer
Clemens R Scherzer, MD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Andrew B Singleton
Andrew B Singleton, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,
Mike A Nalls
Mike A Nalls, PhD
1From the Laboratory of Neurogenetics (H.I., C.B., H.L.L., F.F., D.G.H., A.B.S., M.A.N.), National Institute on Aging, National Institutes of Health, Bethesda; Data Tecnica International (H.I., M.A.N.), Glen Echo, MD; Precision Neurology Program (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Neurogenomics Laboratory (G.L., C.R.S.), Harvard Medical School, Brigham and Women's Hospital; Ann Romney Center for Neurologic Diseases (G.L., C.R.S.), Brigham and Women's Hospital, Boston, MA; The Norwegian Centre for Movement Disorders (J.M.-G., G.A.), Stavanger University Hospital; Department of Chemistry (J.M.-G., G.A.), Bioscience and Environmental Engineering, University of Stavanger, Norway; Assistance-Publique Hôpitaux de Paris (J.-C.C.), ICM, INSERM UMRS 1127, CNRS 7225, ICM, Department of Neurology and CIC Neurosciences, Pitié-Salpêtrière Hospital, Paris, France; Department of Neurology (L.P., M.T.), Oslo University Hospital, Norway; Department of Neurology (M.N., B.R.B., B.P.W.), Donders Institute for Brain, Cognition, and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; Michael J Fox Foundation (S.J.H.), New York; Translational Genome Sciences (K.-D.H.N, K.E.), Biogen, Cambridge, MA; Department of Neurology University of Pennsylvania (J.R.), Philadelphia, PA; Department of Biostatistics and Computational Biology (S.E.), University of Rochester, NY; Department of Computer Science (F.F.), University of Illinois Urbana-Champaign; Department of Neurology (P.A.), Center for Health + Technology, University of Rochester, NY; Department of Clinical Neurosciences (K.M.S., R.W.), University of Cambridge, John van Geest Centre for Brain Repair, UK; Department of Pathology and Laboratory Medicine (V.M.V.D.), Center for Neurodegenerative Disease Research, Parelman School of Medicine at the University of Pennsylvania, Philadelphia; Genetics and Pharmacogenomics (A.G.D.-W.), Merck Research Laboratory, Boston, MA; Statistical Genetics (A.G.D.-W.), Biogen, Cambridge, MA; Institut du cerveau et de la moelle épinière ICM (A.B., F.D.); Sorbonne Université SU (A.B.); INSERM UMR1127 (A.B.), Paris, France; Department of Neurology (G.A.), Stavanger University Hospital, Norway; Preventive Neurology Unit (A.J.N.), Wolfson Institute of Preventive Medicine, Queen Mary University of London; Department of Molecular Neuroscience (A.J.N.), UCL Institute of Neurology, London, UK; Department of Neurology (O.-B.T.), Haukeland University Hospital; University of Bergen (O.-B.T.), Bergen, Norway; Department of Neurology (J.R.E.), Nottingham University NHS Trust, UK; Centre for Clinical Brain Sciences (D.P.B.), University of Edinburgh; Anne Rowling Regenerative Neurology Clinic (D.P.B.), University of Edinburgh; Usher Institute of Population Health Sciences and Informatics (D.P.B.), University of Edinburgh, Scotland; Department of Medical and Molecular Genetics (C.E.W.), Indiana University, Indianapolis; Department of Neurology (D.K.S.), Beth Israel Deaconess Medical Center; Harvard Medical School (D.K.S.), Boston; Voyager Therapeutics (B.R.), Cambridge, MA; Department of Neurology (B.R.), University of Rochester School of Medicine, NY; Institute of Clinical Medicine (M.T.), University of Oslo, Norway; German Center for Neurodegenerative Diseases-Tubingen (P.H.); HIH Tuebingen (P.H.), Germany; Department of Psychiatry (D.W.), University of Pennsylvania School of Medicine; Department of Veterans Affairs (D.W.), Philadelphia, PA; and Department of Clinical Neurosciences (R.A.B., C.H.W.-G.), University of Cambridge, UK; Department of Neurology (J.J.V.H.), Leiden University Medical Center, The Netherlands.
1,✉